Introduction
Helminthiasis are among the most prevalent infections in the world and the leading cause of morbidity, particularly in the developing world [1]. Literary billions of people harbor at least one species of parasitic worm [2]. Outside the developing world, 20th century brought dramatic reductions in the prevalence of infections as a result of improvements in living standards and specific control programmes. In the developing world inadequate water supply, absence of correct sanitation and overcrowded living conditions combined with the lack of access to correct healthcare and low level of education make the poor particularly susceptible to infection and disease, including soil transmitted helminthiasis (STH) [3]. Today it is estimated that approximately one third of the almost three billion people that live below poverty line in developing regions of the Sub-Saharan Africa, Asia and the Americas are infected with one or more helminths [4]. The most common helminthiasis are those caused by infection with intestinal helminthes including ascariasis, trichuriasis and hookworm [5].
School age children are one of the groups that are at higher risk of intestinal parasitic infection. The adverse effects of intestinal parasites among children are diverse and alarming. Intestinal parasitic infections have detrimental effects on long term survival, appetite, growth and general physical fitness, school attendance and cognitive performance [6, 7].Various studies have shown the negative influence of intestinal parasitic infections on the anthropometric indices on school age children [8]. The main conditions and risk factors known to favor the transmission of intestinal helminthic infections exist in Kashmir Division but limited information has been documented in this area on the epidemiology of these parasites. This study was therefore conducted to provide data on the incidence, intensity and host morbidity of intestinal helminthic infections in Budgam District, one of the major districts of Jammu & Kashmir State.
Material and Method
This cross sectional study was conducted among 500 school children between May and November 2009, in Sumbal of Budgam District in Kashmir Province. Budgam is located in the 75º E longitude and 34º N latitude of Jammu & Kashmir State. The villages of this district have many streams and ponds that might predispose children to waterborne diseases both during swimming or playing. The great majority of the population is involved in cattle ranching and farming. Houses are predominantly made of mud, concrete or a combination of wood and mud. Less than 35% of these homes have a latrine inside while others are using makeshift latrines outside their homes or even are defecating in the open. Among the ten schools located in this district, seven were selected for this study. A series of meetings were held with various Public School authorities to explain the use, purpose and methodology of this study and that they could withdraw from this study at any time, if they desire. Also written or oral consent was obtained from the parents of the children included in this study. Inclusion criteria were: (a) To be a resident on the study area over the last 24 months and (b) Willing and able to give informed consent to study protocol. Individuals were excluded if they attended school outside of study area or had received antihelminth treatment within the last 24 hours.
Parasitological Data
Participants were instructed to deposit one fecal sample into each container provided and to return the container immediately to one of the several collection points. Fecal samples returned later than 24 hours after the date of distribution were not accepted and new containers were issued. The research was conducted at junior and elementary school level. At the time of survey (May to November 2009) school attendance was of 1700 students. 430 school children were chosen to participate in the study and the sample size (n) was estimated using statistical formula p (1-p) z2/d2 at a confidence interval of 95% and an error margin of 5% [9]. This gave a sample size of 318 as significant.
Questionnaire survey
A pre-tested questionnaire based on known local risk factors including information such as age, family size, source and storage conditions of drinking water, existence of latrines in their homes, hand washing after defecation, drinking water directly from river Jhelum and “yes or no” choice questions for common signs and symptoms of parasitic infections during the past month was developed. At the time of the interview, interviewers also inspected whether the fingernails of the students were trimmed.
Samples were collected from collection points, emulsified in 10% formalin solution and transported to Microbiology Department of SKIMS Medical College. Formol-ether concentration technique, which is considered to be the most sensitive for intestinal helminthes, was done for examination of the stool. The samples were processed using Kato-Katz thick smear technique and microscopically examined for parasites [10]. Data was analysed by using SPSS 11 version statistical software. The results were expressed as rates and proportions. Chi square test of statistical significance was applied to study the association between prevalence of intestinal parasites and the demographic factors. P value <0.05 was considered as significant [11]
Results
To select the sample children, the students were first stratified according to their educational level (grade 1 to grade 7). A quota was then allocated for each grade and each class room. Finally, the sample children were selected using systematic random sampling techniques by using class rosters as the sample frame. A total of 430 school children aged 3 to 14 years were selected for the study, out of which 34 either did not provide the proper stool sample or complete information thus were excluded from the study. Among the remaining 396 (92%), 216 were males and 180 were females. The mean age of children was 9.5. Five species of intestinal helminthes were identified with an overall prevalence of 58.1% (230 out of 396). There was no discrepancy in the stool examination results between the test and the quality control tests [12].
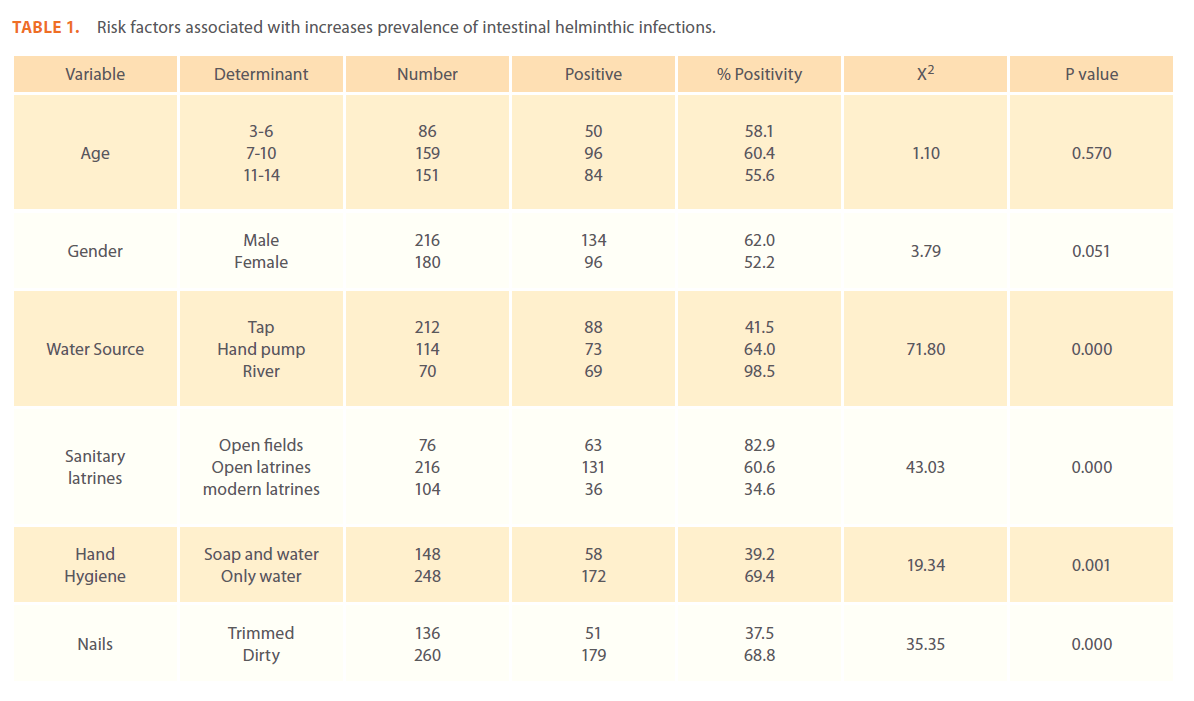
The predominant parasite detected was Ascaris lumbricoides (54.9%) followed by Trichuris trichuria (32.5%), Taenia saginata (9.1%), Enterobius vermacularis (2.6%) and Hymenolepis nana (2.05%). 25% of the students were suffering from infestation with more than one parasite. Since the population is mostly muslin and pigs are not seen in this area no case of infestation with Taenia solium was seen. Similarly not a single case of hookworm was seen due to an unfavourable soil content of Kashmir province for hookworms [13]. The differences in prevalence rates between male, female and different age groups were statistically insignificant (P>0.05). Water source, defecation site and personal hygiene were statistically significant (P<0.05) risk factors in predicting the presence of an intestinal helminthic infection. (Table 1).
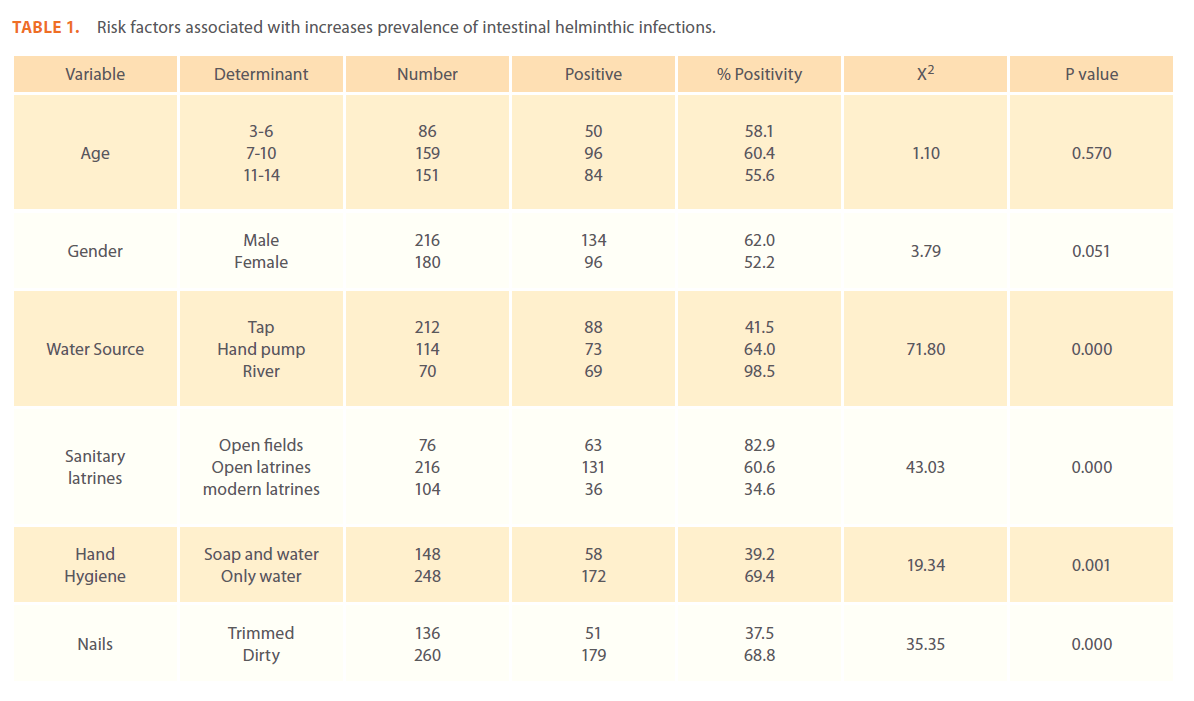
Table 1: Risk factors associated with increases prevalence of intestinal helminthic infections.
Discussion
The main purpose of the study was to show that not much has changed regarding helminthic infections in our country and they continue to be a serious contributor to disease and an important problem from a public health point of view as has been validated by similar studies done in other parts of India [14]. Concomitant multiple parasitic infections were found to be the rule and not the exception in our study population, which is in accordance with what has been found by others [15].
The results of our investigation very clearly demonstrate a very high prevalence of intestinal helminth parasites among school children in Sumbal, Jammu & Kashmir State, India. This might give a general view of the problem of intestinal helminth infection in school children throughout the entire Kashmir province since very similar environmental conditions abound elsewhere. Although India governmental intervention programs have been initiated in many states, in the case of the Kashmir province due to current socio-political unrest, treatment campaigns remain dismal. Ascariasis was found to be the commonest infestation in our study and has been reported in the other parts of Kashmir provinces occupied by Pakistan [16]. A previous study on tribal children of Gurez area of Kashmir has also shown a higher prevalence of ascariasis [17]. These results have attracted the attention of researchers who conducted detailed separate studies only on Ascaris lumbricoides [18]. A. lumbricoides is a soil transmitted parasite and its embryonated ova are very resistant to cold and dry climate. The great majority of infestations occur when children are playing on the soil and do not wash their hands before eating. Ascariasis is considered to be responsible for 20% of acute pancreatitis in Kashmir valley with an overall mortality of 3% [19].
Based on the univariate analysis done, the most striking observation from this study was the strong association between socioeconomic status and prevalence and intensity of infection with geohelminths. Risk factors that are statistically significant associated with helminth infection included open defecation , source of drinking water, untrimmed nails and hand hygiene after defecation. The prevalence of intestinal helminths was significantly higher among children with untrimmed nails. The families using river Jhelum as drinking water source showed a drastic parasitic infestation with all the 70 children being infected. Hand washing after defecation had a protective effect against helminthic infection.
Based on our findings, it is evident that the incidence of intestinal helminthic infections is relatively high in our study area, with very heavy parasite loads. Our study also demonstrated that poor hand washing post defecation and incorrect nail trimming significantly contribute to intestinal helminthic infections morbidity. These are also indicators of low socioeconomic status of a community [20], highlighting the need to educate members of the community, especially those in rural areas, on the methods of preventing the transmission and spread of these human intestinal helminthic infections. In rural Bangladesh, a health intervention study previously found that the combination of periodic anti-helminthic treatment and hygiene education was a cost-effective method to control helminthic parasitic infection [21]. Based on this study and on previous ones, similar methods can be adopted in these communities in a way to reduce intestinal helminthic infections morbidity.
As recommended by WHO, “In areas where prevalence of mild to moderate underweight children is greater than 25% and where parasites are known to be widespread, high priority should be given to deworming,” [10]. We recommend that sustainable efforts on deworming, of our State inhabitants, should be started and continued in order to offer a worm-free environment that could promote physical and cognitive development in the children and thus would gives support to the economic development of our state.
211
References
- Muller R(2002) Worms and human diseases. 2nd Ed. Wallingford: CABI Publishing; p1-2.
- Anderson RM, My RM (1991) Infectious diseases of humans: Dynamics and Control. New York: Oxford University Press. pp 433-606
- Nilanth DS, Simon B, Peter Holezetal (2003) Soil transmitted helminthic infections: Updating the global picture. Disease Control Priorities Project EHO. paper 12.
- Hotez PJ, Molyneux DH, Fenwick A, Kumaresan J, Ehrlich Sach S, Sachs JD, Savioli L (2007) Control of neglected tropical diseases. N. Engl J Med 375: 1018- 1027.
- Hotez PJ, Brindley PJ, Bethony JM, King CH, Pearce EJ, Jacobson J (2008) Helminthic Infections: the great neglected tropical diseases. J Clin Invest. 118: 1311-1321.
- GirumTadesse (2005) The prevalence of intestinal helminthes infections and associated risk factors among school children in Babiletown, Eastern Ethiopia. Etiop. J. Health Dev.19:140-147.
- Nokes C, Bundy DA (1993) Compliance and absenteeism in school children. Implications for helminth control. Trans R Soc Trop Med Hyg. 87:148-152.
- Quinhui – Cota L, Valenica MF, Crompton DW, Phillips S, Hagen Petal (2004) Prevalence and intensity of intestinal parasitic infections in relation to nutritional status in Mexican school children. Trans R Soci Trop Med Hyg. 98: 653-659.
- Daniel WW (1995) Biostatistics - a foundation for analysis in the health science. 6th Ed. New York. John Willey & Sons Inc. New York. USA. P.155.
- World Health Organization (1991) Basic Laboratory methods in medical Parasitology Geneva. WHO, Geneva, Switzerland. p 32.
- Statistical Package for Social Scientists (SPSS) Version 11 (2001) SPSS Inc, Chicago, USA
- Cheesbrough, M.(2000). District Laboratory practice in Tropical Countries. Cambridge University Press, pp: 209-211
- By Hotez PJ, Nilanthi de Silva, Brooker S and Jeffrey Bethony (2003) Soil transmitted helminth infections: The nature, causes and burden of the condition. Working Paper No. 3, Disease Control Priorities Project. Bethesda, Maryland: Fogarty International Center, National Institutes of Health.
- LathaRagunathan, Senthil Kumar Kalivaradhan, SasikalaRamadass, MuruganandamNagaraj, Karthikeyan Ramesh J (2010) Helminthic Infections in School Children in Puducherry, South India MicrobiolImmunol Infect 43(3):228–23
- Ezeamama AE, Mc Garvey ST, Acosta LP, Zierler S, Manola BL et al.(2008) The synergistic effect of concomitant Schistosomiasis, Hookworm, and Trichuria infections on children’s anemia burden. PloSNegl Trop Dis. 2: 245.
- Ahmad Khan, Sultana A, Khan AM, Rashid H, Najm SA (2004) Study of prevalence, distribution and risk factors of intestinal helminthic infestation in District Bagh, Azad Kashmir. Pakistan armed forces med journal.12: 243-248.
- Wani SA, Ahmad F, Zargar SA, Amin A, Dar ZA, Dar PA (2010) Intestinal Helminthiasis in children of Gurez valley of Jammu and Kashmir State, India. Clin. Epidemiology. 2: 91-94.
- Crompton DWT (1998). The prevalence of ascariasis. Parasitology today. 4: 162-169.
- Okwa OO (2007) Tropical parasitic diseases and women. Annals African Med. 6: 157-163.
- Mascie-TaylorCG, Alam M, Montanri RM, Karim R, Ahmad T, Karim E, Akhter S (1999) A study of cost effectiveness of selective health interventions for the control of intestinal parasites in rural Bangadesh. J Parasitol. 85: 6-11.