Sandeep Kumar Kar*, Dipanwita Das and Chaitali Sen Dasgupta
Department of Cardiac Anaesthesiology, Institute of Post Graduate Medical Education and Research, Kolkata, India
Corresponding Author:
Sandeep Kumar Kar
Department of Cardiac Anaesthesiology
Institute of Post Graduate Medical Education and Research
Kolkata, India
Tel: 919477234900
E-mail: sndpkar@yahoo.co.in
Received date: November 12, 2015; Accepted date: December 10, 2015; Published date: December 17, 2015
Citation: Kar Sk, Recurrent Fibrosarcoma Protuberans of Anterior Chest and Abdominal Wall. A Rare Case Report. Arch Med. 2015, 8:1.
Introduction
Dermatofibrosarcoma Protuberans (DFSP) is a rare soft tissue tumour. It often has a high recurrence rate. Commonly the tumor involves the trunk (42-72%), proximal extremities (16-30%) and the head and neck (10-16%) [1-6]. However, it can metastasize in 1-4% of cases after so many years of development of primary lesion [7]. It is a low to intermediate grade malignancy in 90% cases [7] and rarely progresses to high grade fibrosarcomatous component [8]. The incidence rate is only 0.8 cases per million with slight male predominance [9]. Usually middle aged males suffer more from this tumor as compare to female [10]. Recently the authors have encountered such a case of recurrent DFSP which was treated successfully.
Case Report
A 50 year male presented with a large swelling involving the anterior chest wall and the anterior abdominal wall with occasional pain and local irritation. Patient has a burn injury at his age of 4 years and developed scar tissue over anterior abdominal and chest wall. After few years he noticed a small firm painless swelling over the scar which progressively increased in size and patient developed symptoms of pain for which FNAC followed by excision of mass was done. Histopathology and immunohistochemical staining findings were consistent with the diagnosis of DFSP.
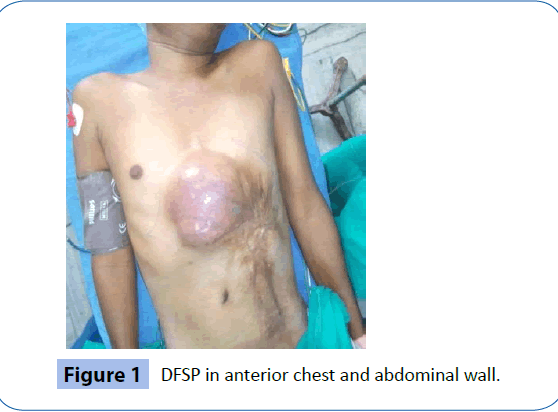
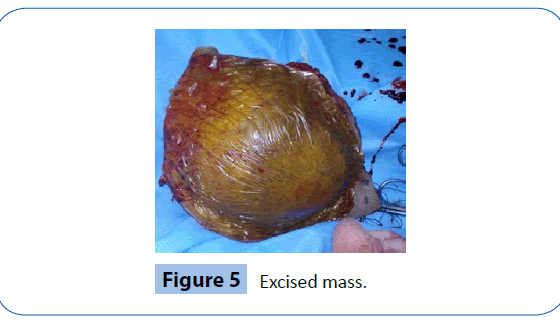
The tumor had reoccurred within 1 year with similar symptoms and with rapid growth to attain a size 11.2 cm × 7.62 cm × 11.18 cm of size protruding from anterior chest and abdominal wall. On examination, the tumor was non tender, firm with well defined margins, a shiny surface with vascular prominence and a previous surgery scar. There was no other abnormality found on clinical examination. CT scan of chest showed an oval shaped heterogeneous contrast enhancing soft tissue mass measuring 11.2 cm × 7.62 cm × 11.18 cm in size, located in the lower presternal and adjacent upper anterior abdominal wall, inseparable from the subcutaneous tissue, skin and rectus muscles of either side. The lesion was seen projecting within the upper abdominal cavity. Histopathology report revealed spindle cell with mild atypia (Figures 1 and 2).
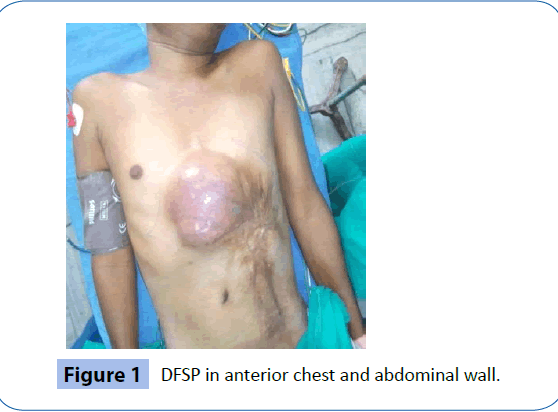
Figure 1: DFSP in anterior chest and abdominal wall.
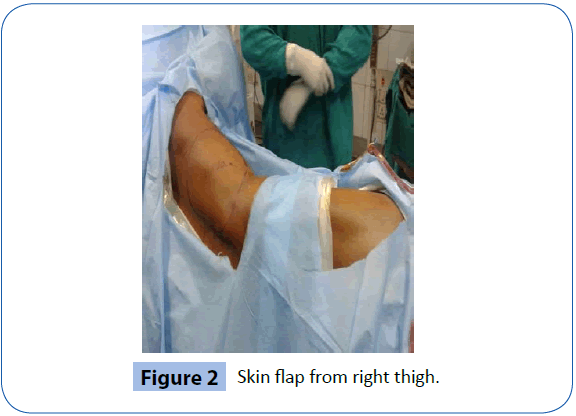
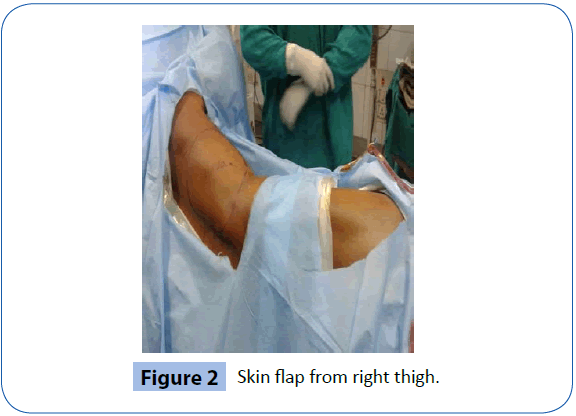
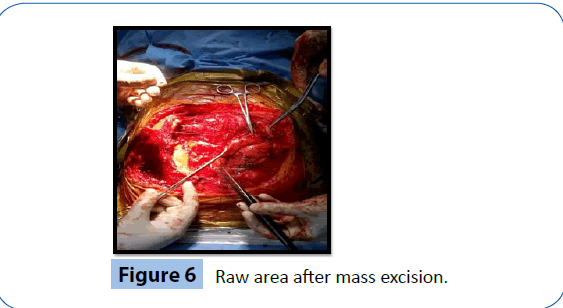
Figure 2: Skin flap from right thigh.
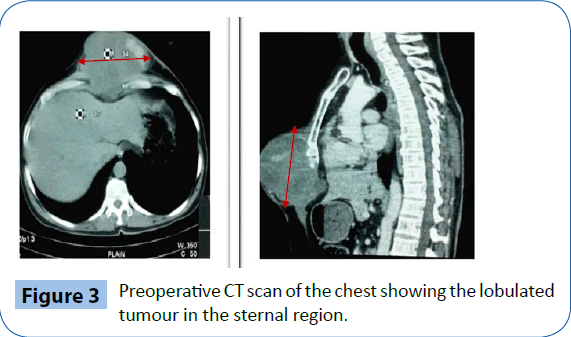
Cells were arranged in whorling pattern. At place Herring bone pattern was appreciated. Mitosis was present (5/10HPF) and features were suggestive of low grade fibrosarcoma (Figures 3 and 4).
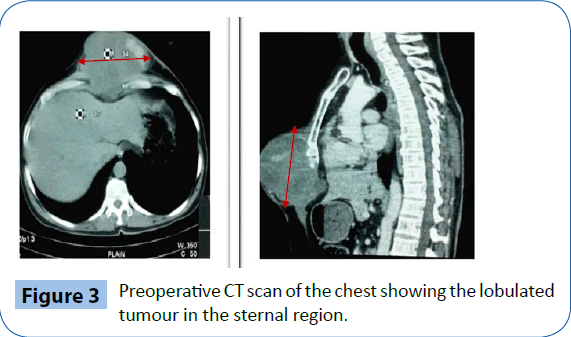
Figure 3: Preoperative CT scan of the chest showing the lobulated tumour in the sternal region.
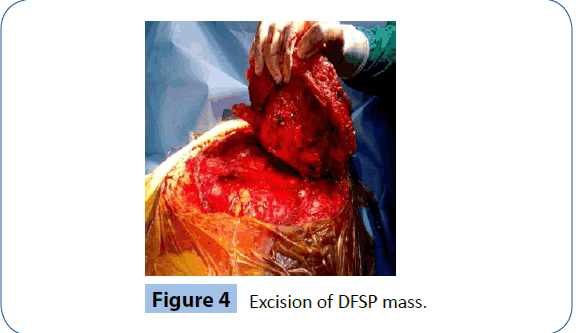
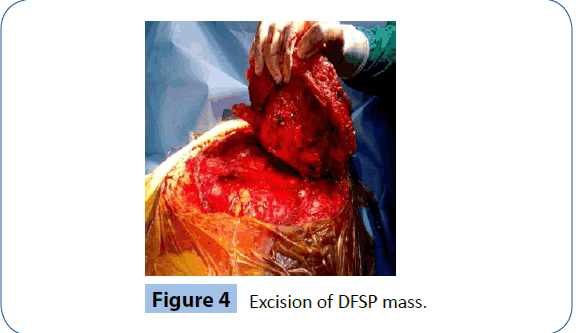
Figure 4: Excision of DFSP mass.
Wide local excision with a 3 cm tumour free margin all around was done (Figure 5). The lower part of sternum and 4 ribs (7th, 8th, 9th, 10th) of each side were resected (Figure 6). During excision there was inadvertent injury to right dome of diaphragm which was repaired successfully. Non absorbable mesh and Right Latissimus dorsi flap were used to repair the defect resulting from the excision.
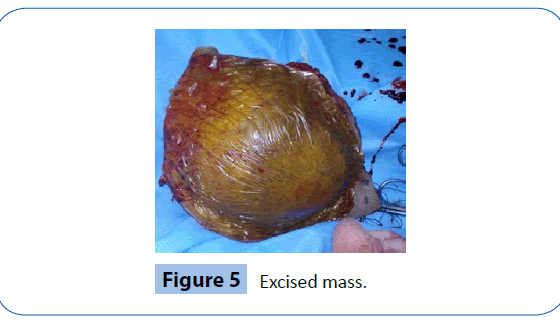
Figure 5: Excised mass.
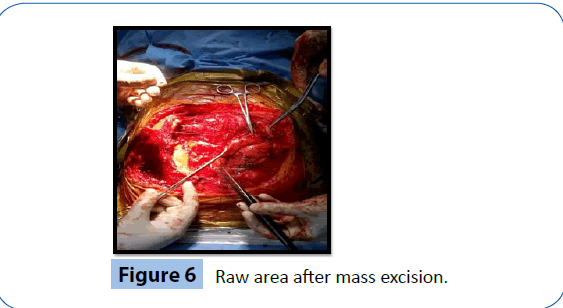
Figure 6: Raw area after mass excision.
A skin flap of 20 cm × 21 cm was taken from right thigh by the plastic surgeon (Figure 2) and the anterior chest and abdominal wall was reconstructed. Biopsy revealed Dermatofibrosarcoma Protuberans with equivocal margin. Immunohistochemical staining was diffusely positive for CD34 and negative for CD117.
Post operative course was uneventful. Postoperative chemotherapy for mitotic activity and radiotherapy for equivocal margin were advised by the oncologist. Patient was discharged on 10th post operative day and advised monthly follow up.
Discussion
Less than 5% of all thoracic tumors is malignant [11] of which 50% is soft tissue fibrosarcoma. DFSP accounts for only 2-6% of all soft tissue sarcomas. Darier and Ferrand first described DFSP as a distinct cutaneous disease and termed as progressive and recurrent dermatofibroma in 1924 [12]. However it was initially published in literature as early as 1890. In 1925 Hoffman coined it as "dermato-fibrosarcoma-protuberans". The origin of DFSP is still controversial (Figure 6). With this defect usually genetic correlation is associated. This occurs due to translocation of chromosomes 17 and 22 or formation of a ring [13]. Primarily the tumor starts with a very small non indurated nodule and patient presents when it slowly increases to large, firm, sometimes tender, multilobulated, blue to red mass as in our case. Due to its local aggressiveness, it can grow into the surrounding fat, fascia, muscle and even bone. In this case, tumor invaded the lower part of sternum and adjacent four ribs bilaterally. So, during mass removal, these bones were excised in this case. Rarely, distant metastasis is seen in such case and it is nearly 4-6%, with the lungs being the common site [14,15]. There was no distant metastasis in this patient. This case was a recurrence of primary tumor.
Literature shows that DFSP has characteristically high and varying recurrence rate ranging 10-80% [16]. Surgery is the gold standard treatment. Excision of mass with 3 cm tumor free margin is the mainstay though histological free margin as local control is emphasized [17]. In this case along with muscle flap, non absorbable mesh was used to reinforce the anterior abdominal and chest wall to avoid post-operative complication of incisional hernia.
Chemotherapy is not always advised but radiotherapy is usually recommended if tumor margin is equivocal. In this case, chemotherapy was advised for mitotic activity of this aggressive tumor and also post operative radiotherapy was recommended as adjuvant therapy to reduce the chance of recurrence when excision biopsy reveals doubtful tumor margins [18].
In the era of minimally invasive surgical practice, a microscopic surgical procedure termed as Mohs surgery is widely popular not only for its high oncological effectiveness, it can also provide maximal tissue salvage. In case of unresectable tumor tyrosin kinase inhibitor (Imatinib) is the treatment of choice. Among all available treatment of such case, primary surgical excision is the gold standard and early resection with tumor free margin plays the pivot role of success in the management of DFSP. It provides advantage of less chance of recurrence and sometime needs no chemotherapy or radiotherapy, thus enhances the positive outcome with good prognosis.
Conclusion
DFSP is a locally invasive tumor with rare incidence of distant metastasis though recurrence rate is high. Early detection and wide primary surgical resection followed by postoperative adjuvant radiotherapy and chemotherapy can successfully prevent recurrence resulting a favorable outcome.
7934
References
- Gloster HM Jr, Harris KR, Roenigk RK (1996) A comparison between Mohs micrographic surgery and wide surgical excision for the treatment of dermatofibrosarcoma protuberans. J Am Acad Dermatol 35: 82-87.
- Criscione VD, Weinstock MA (2007) Descriptive epidemiology of dermatofibrosarcoma protuberans in the United States, 1973 to 2002. J Am Acad Dermatol 56: 968-973.
- Barnes L, Coleman JA Jr, Johnson JT (1984) Dermatofibrosarcoma protuberans of the head and neck. Arch Otolaryngol 110: 398-404.
- Taylor HB, Helwig EB (1962) Dermatofibrosarcoma protuberans. A study of 115 cases. Cancer 15: 717-725.
- Stojadinovic A, Hoos A, Karpoff HM, Leung DH, Antonescu CR, et al. (2001) Soft tissue tumors of the abdominal wall: analysis of disease patterns and treatment. Arch Surg 136: 70-79.
- Fiore M, Miceli R, Mussi C, Lo Vullo S, Mariani L, et al. (2005) Dermatofibrosarcoma protuberans treated at a single institution: a surgical disease with a high cure rate. J Clin Oncol 23: 7669-7675.
- Bowne WB, Antonescu CR, Leung DH, Katz SC, Hawkins WG, et al. (2000) Dermatofibrosarcoma protuberans: A clinicopathologic analysis of patients treated and followed at a single institution. Cancer 88: 2711-2720.
- Mentzel T, Beham A, Katenkamp D, Dei Tos AP, Fletcher CD (1998) Fibrosarcomatous ("high-grade") dermatofibrosarcomaprotuberans:clinicopathologic and immunohistochemical study of a series of 41cases with emphasis on prognostic significance. Am J SurgPathol 22: 576-587.
- McLoughlin PM, Girach M, Wood GA (1992) Dermatofibrosarcoma protuberans of the scalp. Br J Oral Maxillofac Surg 30: 401-403.
- Darier J (1924) Dermatofibromesprogressifsetrecidivantsoufibrosarcomes de la peu. Ann DermatolSyphiligr (Paris) 5: 542-562.
- David EA, Marshall MB (2011) Review of ChestWall Tumors: A Diagnostic, Therapeutic, and Reconstructive Challenge. Semin Plast Surg 25: 16-24.
- Lemm D, Mügge LO, Mentzel T, Höffken K (2009) Current treatment options in dermatofibrosarcoma protuberans. J Cancer Res Clin Oncol 135: 653-665.
- CamaraES, Kasse AN, Sane JC, Bousso A, Thiam B, et al. (2013) Dermatofibrosarcoma. Internet J OrthopSurg 2013 21: 1.
- Lemm D, Mügge LO, Mentzel T, Höffken K (2009) Current treatment options in dermatofibrosarcoma protuberans. J Cancer Res Clin Oncol 135: 653-665.
- Mendenhall WM, Zlotecki RA, Scarborough MT (2004) Dermatofibrosarcomaprotuberans. Cancer 101: 2503-2508.
- Brabant B, Revol M, Vergote T, Servant JM, Banzet P (1993) Dermatofibrosarcomaprotuberans of the chest and the shoulder: wide and deep excisions with immediate reconstruction. Plast Reconstr Surg 92: 459-462.
- Asuquo ME, Umoh MS, Ebughe G (2007) Dermatofibrosarcoma protuberance: case reports. Ann Afr Med 6: 80-83.
- Stivala A, Lombardo GA, Pompili G, Tarico MS, Fraggetta F, et al. (2012) Dermatofibrosarcoma protuberans: Our experience of 59 cases. Oncol Lett 4: 1047-1055.