Chen-Tin Liu1, Yen-Ru Chou2,3,#, Chao-Chia Weng2,4, Chia-Yu Wu4,5, Keng-Liang Ou2,3,6,7*, Han-Yi Cheng2,3,6*
1Department of Dentistry, Sijhih Cathay General Hospital, Taipei 221, Taiwan
2Research Center for Biomedical Devices and Prototyping Production, Taipei Medical University, Taipei 110, Taiwan
3Graduate Institute of Biomedical Materials and Tissue Engineering, College of Oral Medicine, Taipei Medical University, Taipei 110, Taiwan
4School of Dentistry, College of Oral Medicine, Taipei Medical University, Taipei 110, Taiwan
5Division of Oral and Maxillofacial Surgery, Department of Dentistry, Taipei Medical University Hospital, Taipei, Taiwan
6Research Center for Biomedical Implants and Microsurgery Devices, Taipei Medical University, Taipei 110, Taiwan
7Department of Dentistry, Taipei Medical University-Shuang Ho Hospital, Taipei 235, Taiwan
#Co-first author
Corresponding Authors:
Han-Yi Cheng
Department of Dentistry, Taipei Medical University-Shuang Ho Hospital
Taipei 235, TaiwanDepartment of Dentistry
Taipei Medical University-Shuang Ho Hospital, Taipei 235, Taiwan
Tel: 886-2-27361661 ext. 5401 ext. 5100
Fax: 886-2-27395524
E-mail: chytmu@gmail.com
Keng-Liang Ou
Department of Dentistry, Taipei Medical University-Shuang Ho Hospital
Taipei 235, Taiwan
Tel: 886-2-27361661 ext. 5401 ext. 5100
Fax: 886-2-27395524
E-mail: klou@tmu.edu.com
Citation: Chen-Tin L, Yen-Ru C, Chao-Chia W, et al. Research of Oral Remodeling on Mandible with Ameloblastoma Defect: Biomechanical Analysis and Histological Examination. J Biomedical Sci. 2015, 4:1. doi:10.4172/2254-609X.10006
Copyright: © 2015 Chen-Tin L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
3D-reversed model; Ameloblastoma; Histopathological examination
Introduction
Ameloblastomas (ABs) are benign tumors derived from dental embryonic apparatus [1], and account for 1% of all tumors of the mandible. Its main characteristic is slow growth. Although they are histologically benign, they have a high reoccurrence rate after treatment because of their high local invasiveness [2]. The symptoms of ameloblastomas include maxillofacial area swelling, pain, malocclusion, loss of teeth, and misfit of existing dental prosthesis. Non-tender swelling is the most common characteristic of ameloblastomas [3]. This disease is prevalent in individuals aged between 20 to 40 years and has no gender predilection. Reportedly, the tumors that affect mainly the mandible and the maxillary ameloblastomas only account for 1 to 20% of the time [4,5]. There are several histological variants of ameloblastomas, but the follicular variant is the most common.
Finite Element Analysis (FEA) is a useful tool that can be applied to quantify the stress distribution in the mandible and surrounding tissues. This method has been previously used in the study of biomechanical behavior in orthopedic devices, including hip, knee, and spinal implants, under various loading conditions [6-8]. Even as numerous finite element simulations of the mandible have been performed, there has been no research comparing 3-D ameloblastoma models before and after surgery to understand stress fields in various cases of ameloblastoma, both before and after operation [9,10].
To examine the biomechanical behavior of the ameloblastoma model, one must focus on the magnitude and location of the maximum stresses and displacement under physiological loading. Therefore, the aim of this study is to demonstrate the 3-D Finite Element Models (FEMs) reconstructed from in vivo image data to quantify the stress distribution and deformation in the mandible and implant devices before and after clinical surgery and then compare the histopathological examinations to investigate the ABs.
Materials and Methods
In 2010, a patient with no family history of tumors claimed to have painful swelling in his lower jaw after undergoing root canal treatments for his mandibular teeth. He was medically healthy and had no habit of smoking, drinking, or betel nut chewing. Physical examination disclosed an elevated mass in the anterior mandibular labial vestibule and the left buccal vestibule. The mass was non-tender on palpation and had no exudate. The overlying mucosa was intact but color change was noted. There were no deep pockets in the area around the teeth. The lateral facial profile showed obvious protrusions in lower jaw. Other than that, there was no neurological anomaly or enlarged neck lymph nodes that could be palpated.
Panoramic radiographic examinations showed a lesion located in the mandible from the right canine to the left second premolar. The lesion showed “soap bubble” appearance in some areas and unilocular radiolucency in others. Chest radiography did not show any abnormity. The head and neck Computed Tomography (CT) scan revealed general radiolucent lesion in the mandible, and the buccal cortical bone was enlarged and partly perforated by the tumor. An incisional biopsy showed a mass containing both a solid tumor and a cystic lesion in the mandible, which was histologically proved to be an ameloblastoma. The aforementioned patient underwent two marsupialization surgeries in 2011 to shrink the lesion area. The purpose of the marsupialization was to decrease the volume of the ameloblastoma tumor. It proved to be beneficial in subsequent clinical operations. The post-surgery physical and radiographic examination showed the tumor was in remission. The next stage of treatment was wide excision and immediate reconstruction of the mandible.
The surgery was carried out in 2012. The safety margin of excision was 10 mm. The suggested margin was 10 mm to ensure that the ameloblastoma tumor is completely removed. A prebended titanium with the aid of a 3-D printing plate was fixed on the remaining parts of the mandible. Subsequently, the free fibular osteocutaneous flap was harvested and the fibula was osteotomized into segments with the guidance of a surgical stent to perfectly fit the curve of the mandible with straight fibula. The soft tissue defect was reconstructed with a skin paddle.
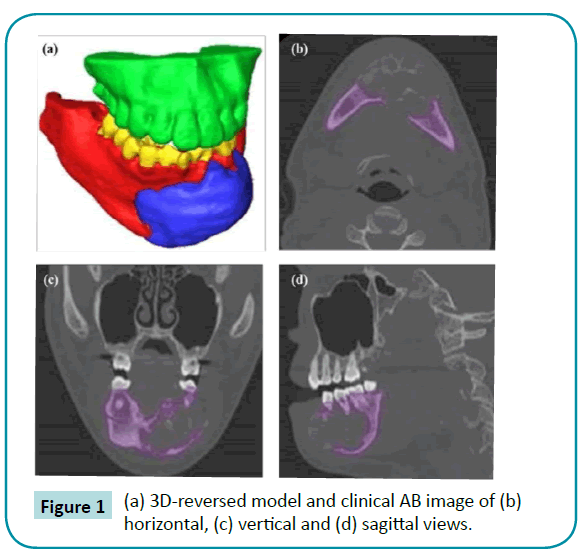
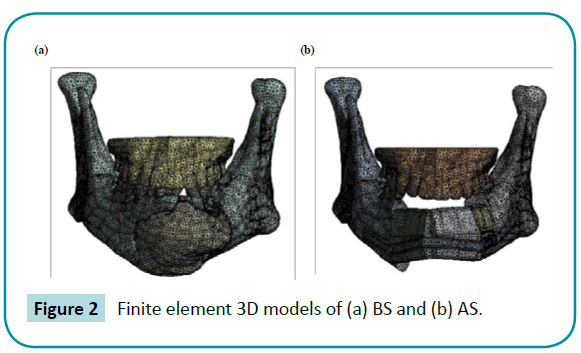
The patient suffering from AB symptoms was enrolled in this study. For the reconstructed model based on the patient’s symptoms, precise computed tomography (CT, slices at 0.625 mm intervals; High Speed CT1, General Electrics, USA) examinations were carried out, using maxilla and mandible geometries as shown in Figure 1. An edge detection algorithm was set up in the program AVIZO 6.2 (Internet Securities, Inc, USA), which is a 3-D image reconstruction and solid modeling program. To obtain accurate results in the finite element method, converging and reinforcing the meshes are important processes, which help the model better represent a real model. Though it takes five times the original convergence process, the new method would have a mesh that is as reliable as the final 3-D model, and consists of approximately 370,000 nodes and 210,000 solid elements. The element adapts a tetrahedral feature with 10 nodes, i.e., each side has a mid-side node and three degrees of freedom, as shown in Figure 2. Finally, the properties of the elements and the muscles of mastication on the temporomandibular joint (TMJ) were adopted [11,12].
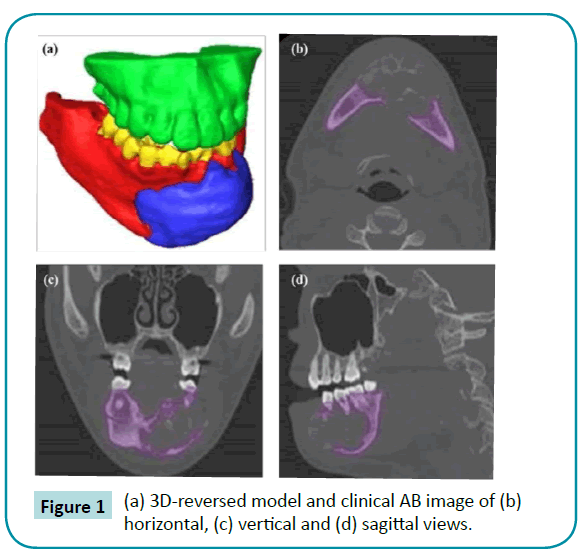
Figure 1: (a) 3D-reversed model and clinical AB image of (b) horizontal, (c) vertical and (d) sagittal views.
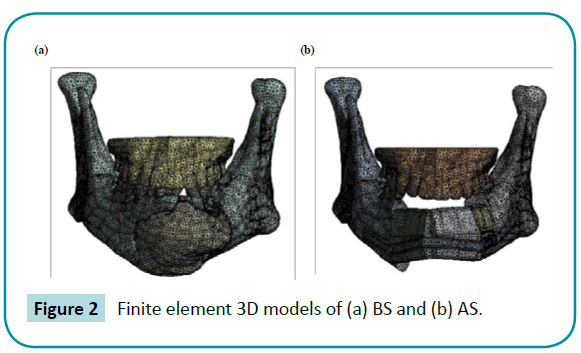
Figure 2: Finite element 3D models of (a) BS and (b) AS.
All the specimens taken from the patient were investigated histopathologically. An excised fragment was fixed in 10% paraformaldehyde, embedded in paraffin wax, and stained with hematoxylin and eosin (HE) stain. Coded specimens were scored under an optical microscope by a pathologist.
Results
This article reports on a 26-year-old man showing symptoms of swelling on the lower jaw after dental treatment. The radiographic examination showed a large radiolucent lesion occupying the mandible. The lesion histologically proved to be an ameloblastoma. The treatment was conducted in two stages. The first stage was marsupialization to reduce the size of the tumor. The second stage was wide excision and reconstruction of the area with a free fibular osteocutaneous. This case applied a 3-D model to facilitate the surgery. Constructing 3-D models of the mandible and the fibula with a 3-D printer and accordingly fabricating the surgical stent significantly reduced the surgical time and helped prevent errors during surgery.
FEA
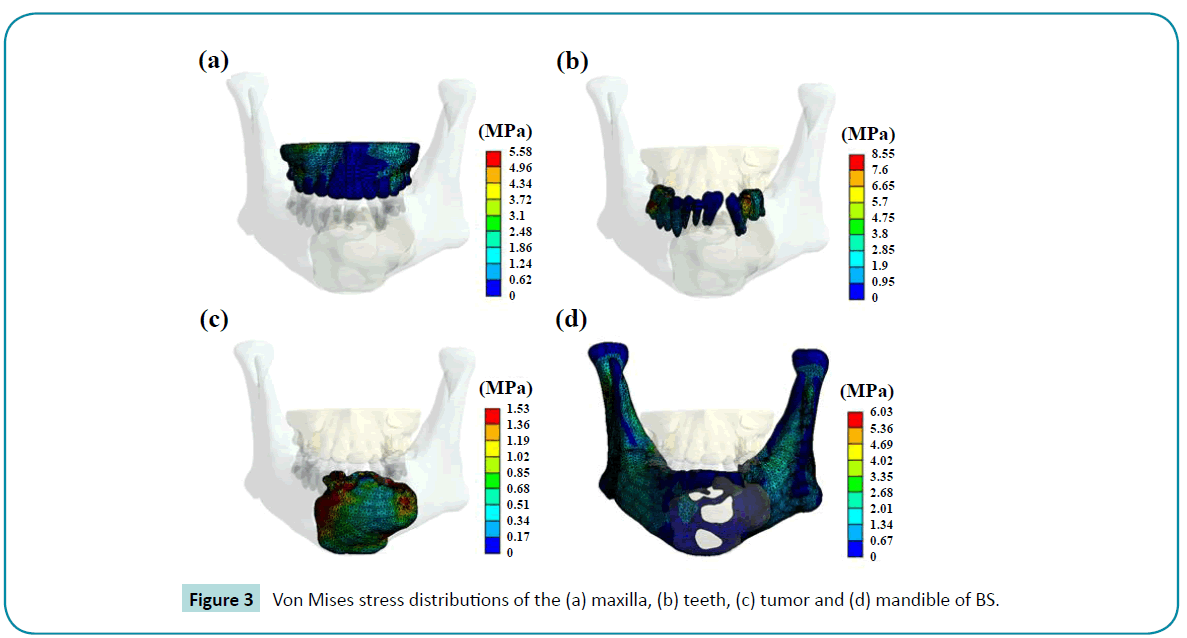
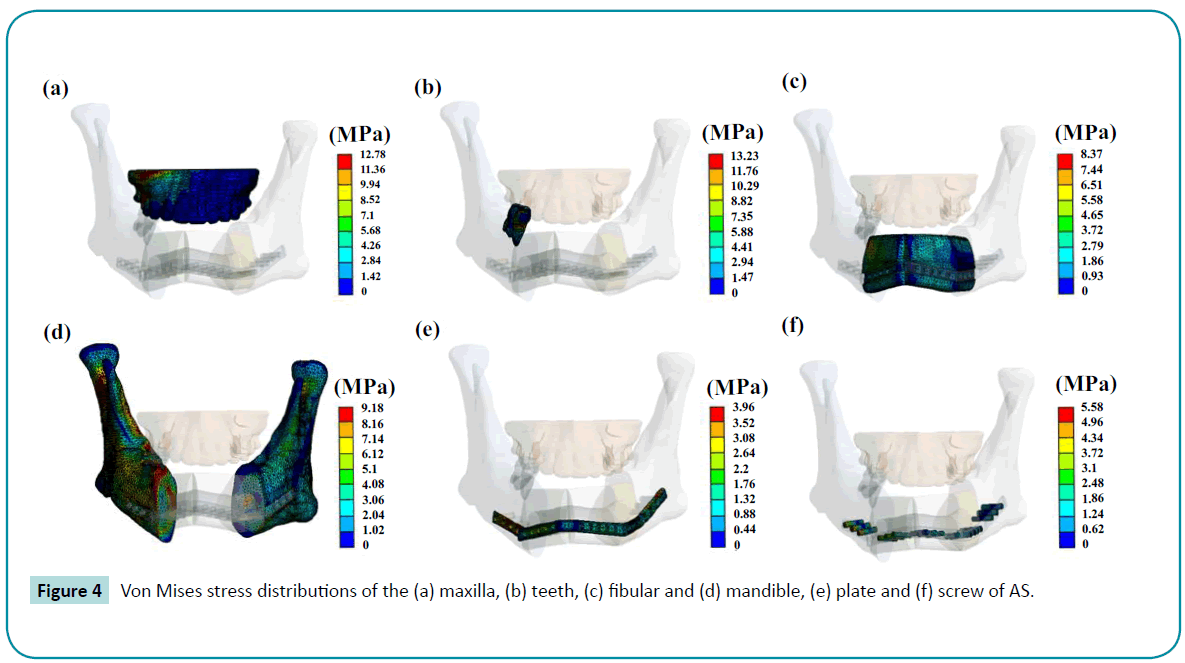
For all of the models, the highest von Mises stress varied from 1.42 MPa to 12.97 MPa (Table 1). The remarkable differences among the trials were the stress increase by approximately 2.42 times in the maxilla and 1.51 times in the mandible. The stress became more uneven in the other regions for the after clinical surgery (AS) group as shown in Figures 3 and 4. AB directly affects stress because it is a kind of soft tissue and it does not have the capability to transfer or support forces. The maximum stresses were usually on the interfaces between elements. The highest stress on the teeth was 54.56% higher in the AS group than those in the before clinical surgery (BS) group. Fibular replacement surgery was demonstrated to increase the stresses in the mandible, maxilla, and teeth. The maximum stress on the plate observed at the right side eighth screw was 5.47 MPa. The maximum von Mises stress on the plates tends to be smaller than that of the screw during jaw movement.
| |
|
Von Mises stress (MPa) |
Deformation (*10-5 mm) |
| BS |
Maxilla |
5.21 |
9.62 |
| Mandible |
5.92 |
345.338 |
| Teeth |
8.49 |
29.89 |
| Tumor |
1.44 |
54.31 |
| AS |
Maxilla |
12.61 |
13.67 |
| Mandible |
8.93 |
696.07 |
| Teeth |
13.13 |
70.58 |
| Fibula |
8.28 |
309.23 |
| Plate |
3.90 |
420.91 |
| Screw |
5.47 |
394.24 |
Table 1: von Mises stresses and deformations in the models.
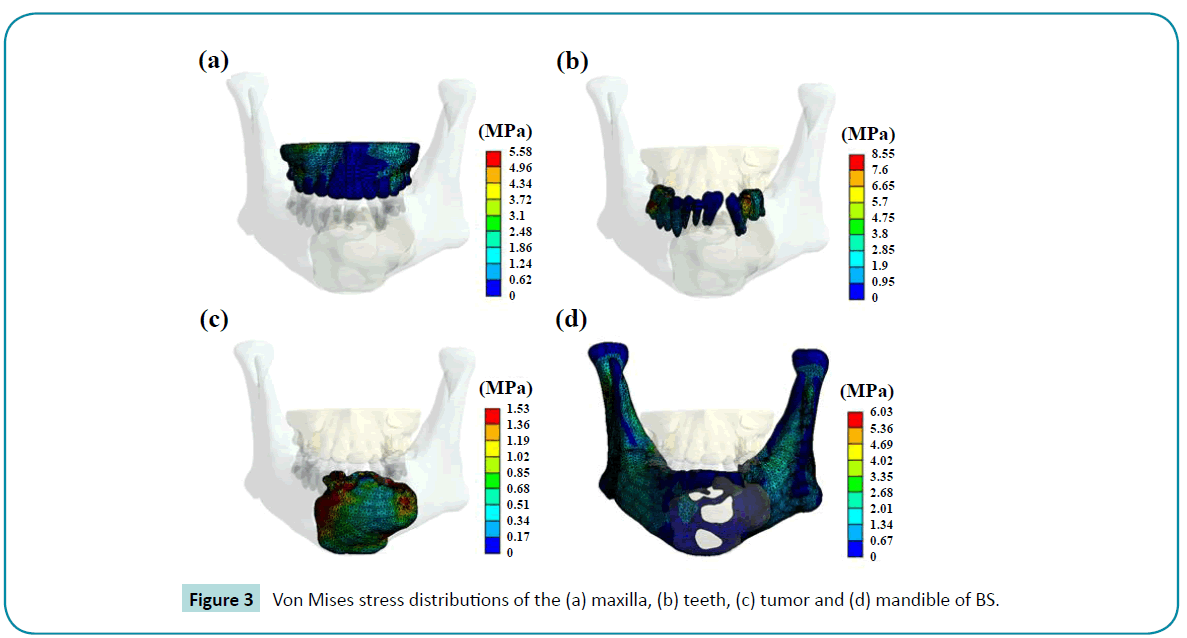
Figure 3: Von Mises stress distributions of the (a) maxilla, (b) teeth, (c) tumor and (d) mandible of BS.
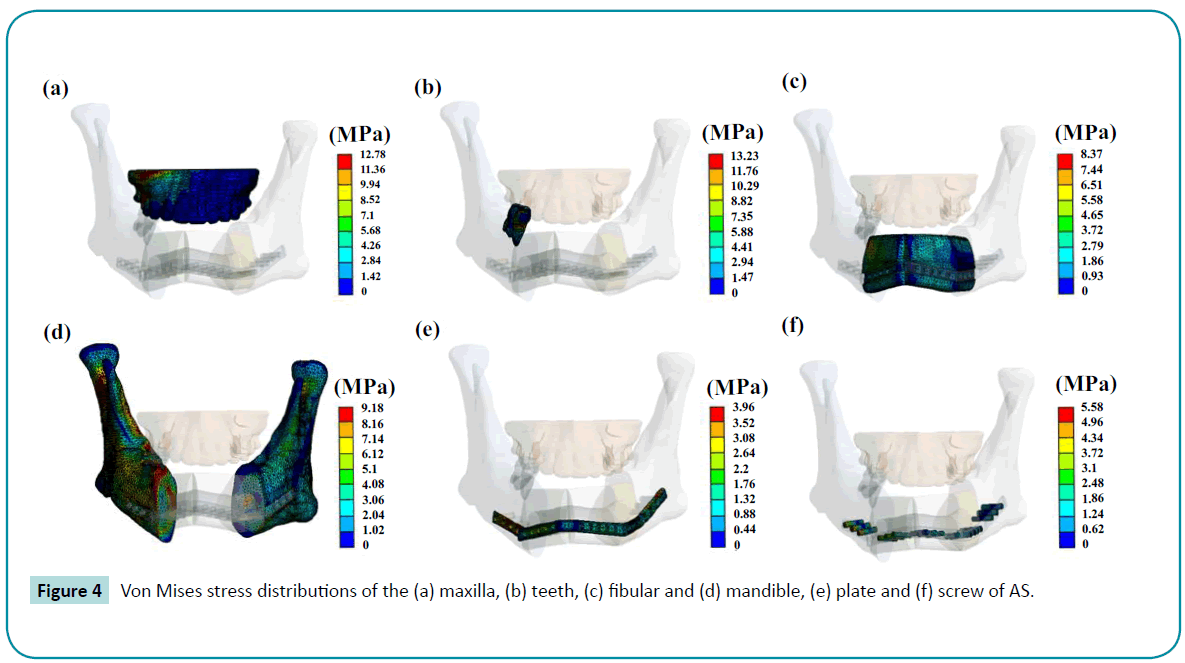
Figure 4: Von Mises stress distributions of the (a) maxilla, (b) teeth, (c) fibular and (d) mandible, (e) plate and (f) screw of AS.
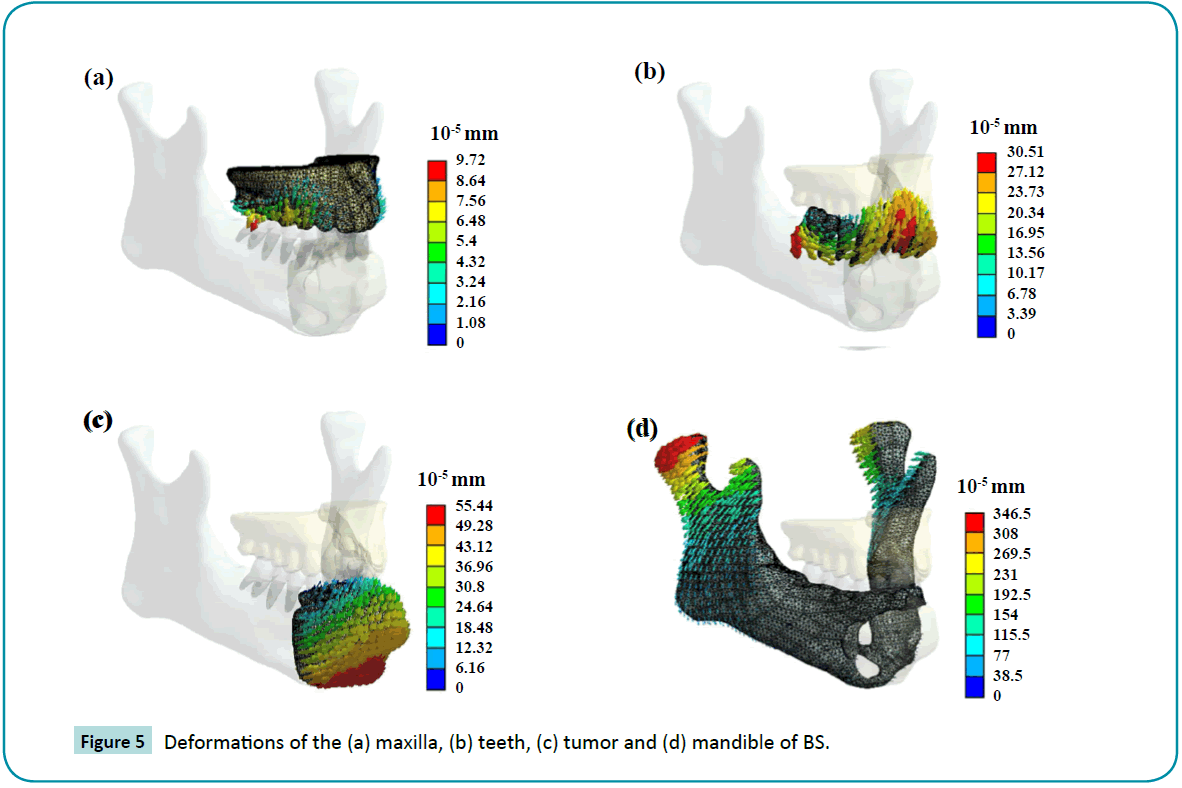
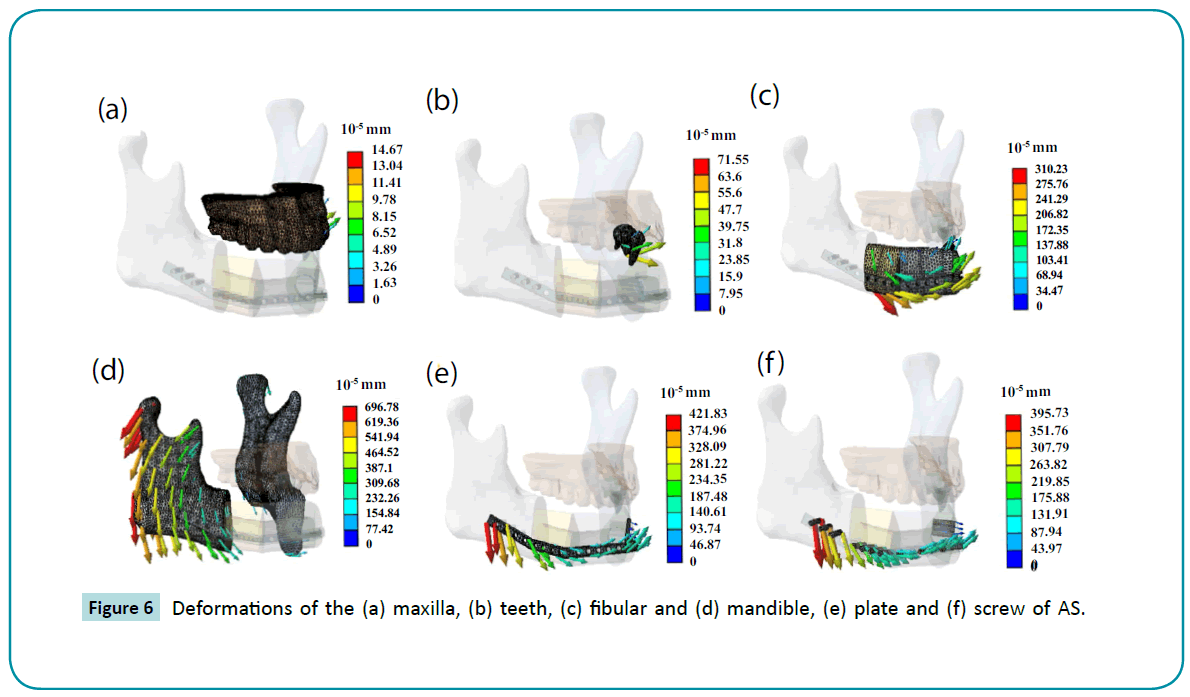
It was found that deformation increases in the AS group, and the maximum deformation rise in the left mandible region and the deformation value increased 2.02 times as shown in Figures 5 and 6. When the jaw moves, it shows significant abnormal deformation in the left fibular and plate. However, the difference between the two groups in the maxilla could not be determined. Within the contact region, the load transfer from the mandible to the teeth and maxilla during usage is established. The deformation increased more than twice after the surgery. There was merely a 5.43E-6 mm deformation in the tumor area. However, the fibular, screws, and plates were replaced. The deformations of these elements were much larger (>3E-3 mm) than the tumor in the BS group. It was observed that maximum stress and deformation occurred at the contact points. The applied stress is the most important factor in long-term success of the operation. Furthermore, the bone response will depend on the applied stress because of overload stress in most cases.
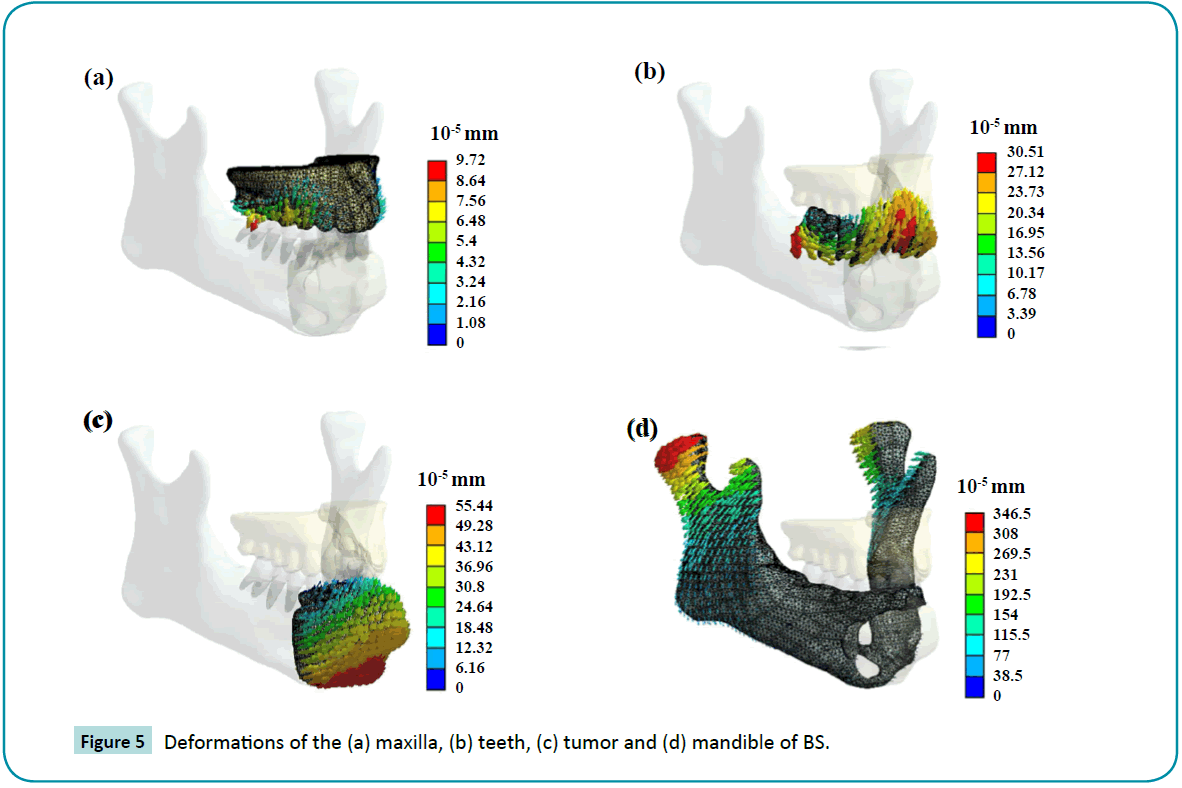
Figure 5: Deformations of the (a) maxilla, (b) teeth, (c) tumor and (d) mandible of BS.
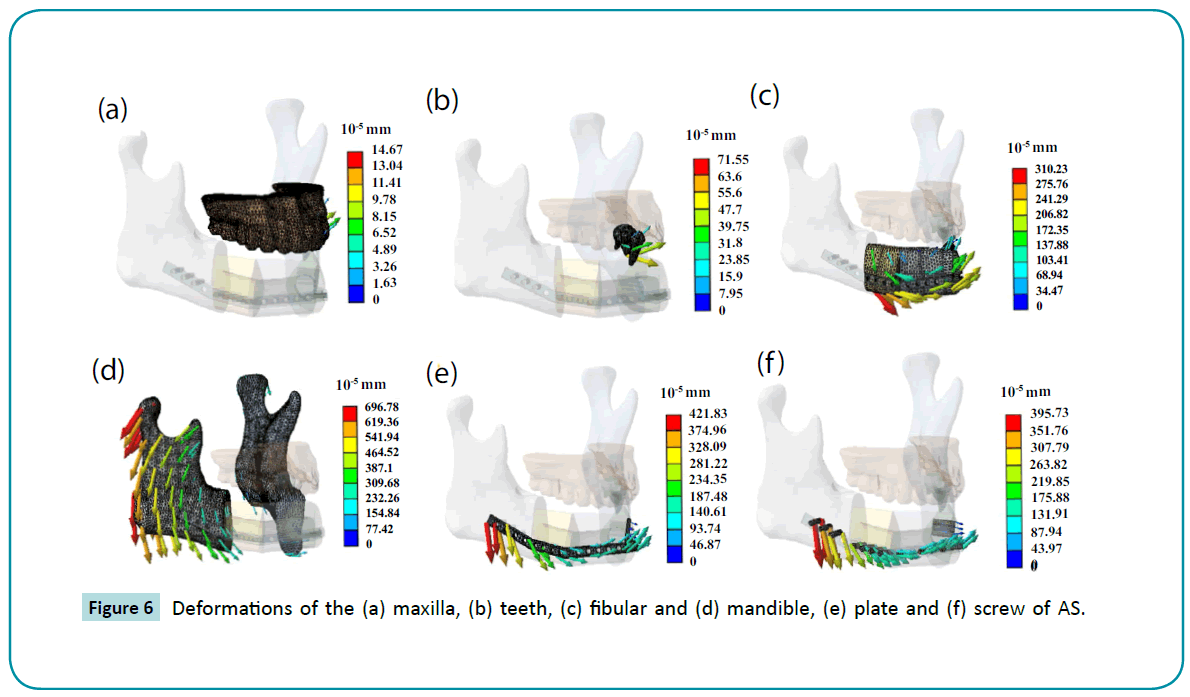
Figure 6: Deformations of the (a) maxilla, (b) teeth, (c) fibular and (d) mandible, (e) plate and (f) screw of AS.
Histological examination
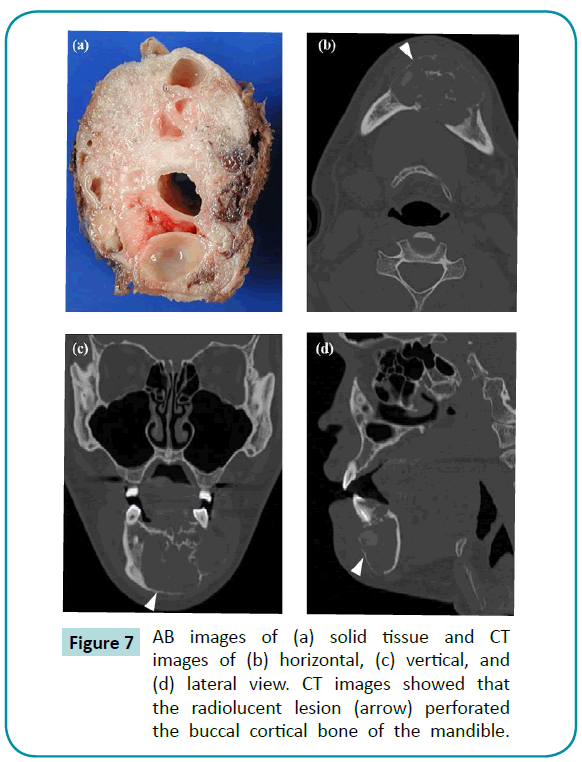
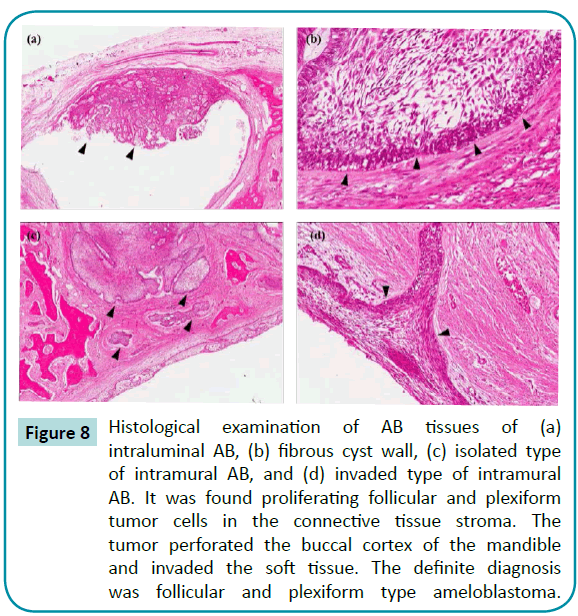
The ABs were examined using clinical tissue imaging and radiography as shown in Figure 7. The ABs in the mandible expanded and interfered with the space of the normal bone tissue. This resulted in the normal bone tissues being dissolved because of overloading stress by ABs. Using Optical Microscopy (OM), AB tissues were divided into four subtypes: fibrous cyst wall, intraluminal AB, isolated type, and invaded type of intramural AB (Figure 8). The intraluminal AB reveal plexiform in the ameloblastoma center and fibrous cyst wall around the epithelium. However, the intramural AB comprised of islands of infiltrating ameloblastoma tissue, where some islands were observed during cystic degenerations. Furthermore, parts of the nodule invade the fibrous cyst wall. Proliferating follicular and plexiform tumor cells were found in the connective tissue stroma. The tumor perforated the buccal bone cortex of the mandible and invaded the soft tissue. The definite diagnosis was follicular and plexiform type ameloblastoma.
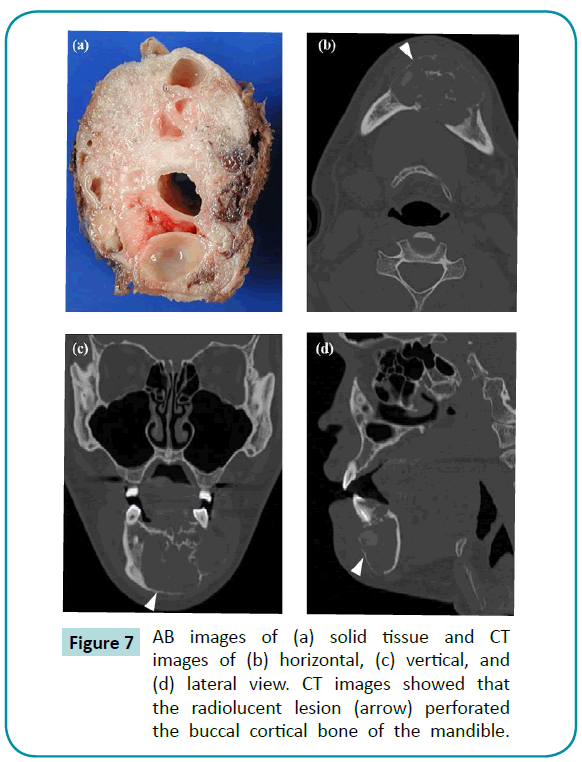
Figure 7: AB images of (a) solid tissue and CT images of (b) horizontal, (c) vertical, and (d) lateral view. CT images showed that the radiolucent lesion (arrow) perforated the buccal cortical bone of the mandible.
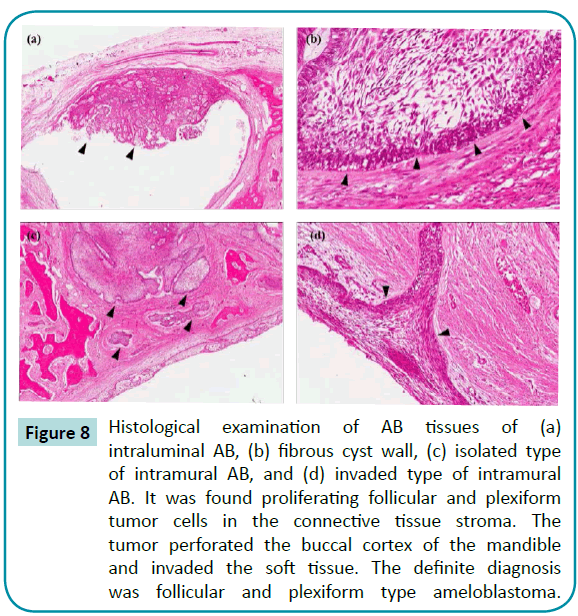
Figure 8: Histological examination of AB tissues of (a) intraluminal AB, (b) fibrous cyst wall, (c) isolated type of intramural AB, and (d) invaded type of intramural AB. It was found proliferating follicular and plexiform tumor cells in the connective tissue stroma. The tumor perforated the buccal cortex of the mandible and invaded the soft tissue. The definite diagnosis was follicular and plexiform type ameloblastoma.
Discussion
In this study, the stresses and deformations increased significantly after surgery, but the patient needed to accept clinical treatment for removing the AB tumor as the histological analysis indicated the tumor was too severe and affected oral functions. However, the results showed that the abnormal stress was concentrated at the interface between the plates. Therefore, we suggested enhancing the strength of materials or designs of screws and plates to prevent them from fracturing. For oral cancers, partial removal of mandibular bone tissue prevents the cancer to extend and damage surrounding tissues [13]. This defect is usually cured using an autograft bone [14,15]. However, many patients cannot tolerate long clinical operation. For the patient in this study, the oral model was reconstructed using computer-aided reverse system and 3-D printing, and the titanium plate was formed before the surgery to shorten valuable clinical operation time.
Various researches have investigated the classifications of AB tissues. The division of AB tissues into four subtypes in the present study is based on Reichart’s report [25]. He conducted a worldwide literature survey of 193 published cases of AB and produced data allowing the presentation of a revised concept of this much-debated lesion. AB is a variant of the solid or multicystic ameloblastoma. It was found that the unilocular pattern is more common than the multilocular, especially in cases associated with tooth impaction. In line with the mean of the “dentigerous” and the “non-dentigerous” ages (16.5 years versus 35.2 years), one 26-year-old volunteer was enrolled in the present study. Similar to this study, Reichart separated AB tissue into four subtypes, such as simple type AB, simple with intralumenal proliferations, simple with both intralumenal and intramural proliferations, and simple with only intramural proliferations.
Finite element is widely used in clinical analysis to evaluate potential cases. It is an effective analysis method with a variety of biomechanical studies for biological applications in dental implantations [16,17]. In the dental field, models have been used to determine stresses in different biological structures, such as TMJ implants, facial skeletons, periodontal ligaments, and dentition [18-20]. Most of these FEA studies have analyzed the biomechanical behavior of individual structures or materials. However, biomechanical models of the human masticatory finite element model are not perfect because they are based on a number of assumptions and simplifications. Many authors have reported studies using finite element method for reconstructing mandibular models, but none of these studies have investigated the ameloblastoma model before and after clinical surgery. The maximum stress occurred at the screw-bone interfaces, especially at the screw, which was closest to the defect region. This is a dangerous sign for clinical practices. However, it was suggested to use larger diameter screw or more than one screw in those places. Nagasao published similar results in 2010 that support our data [21]. However, previous papers reported that screw loosening could develop long-term complications after clinical plate reconstruction of the mandible operation [22,23]. This analysis could provide the solution to prevent screw loosening or fracture.
Three-dimensional models have been used as preoperative treatment planning tools for maxillofacial surgeries, such as temporomandibular joint (TMJ), correction of asymmetric faces, post-tumoral reconstruction, skull defect reconstruction, craniofacial syndromes, orthognathic surgery, and distraction osteogenesis. Additionally, this technique can be used for soft tissue reconstruction and could also be potentially applied in anthropological studies. Therefore, 3-D models have been used for the diagnosis and treatment planning related to complicated maxillofacial tumor, as it can help in clear visualization of the relationships between the disc and condyle in the TMJ. The present study also demonstrates the risks for placing implants in clinical fibular reconstructed mandibles, based on the FEA of stresses and deformations of the screws occurring at the interface between the plates. In the oral model, the maximum von Mises stresses are located in the region around the right side eighth screw and these overloading stresses can potentially initiate implant fatigue failure. Various studies have demonstrated that these regions of the mandible are important functional regions that sustain masticatory loading and these results suggest that the strength of screws can be enhanced. A 3-D FEM can be fabricated based on the data of the CT scan. A simulated surgery on the model is performed, and the suitable screws and plates are prepared beforehand to shorten the duration of the clinical operation. However, efficacy of preoperative versus intraoperative mandibular contouring using rapid prototyping technology was investigated in 2013 [24], and their results revealed no statistical significant differences in conformance, surface-area contact, and best overall match. Our present study provides useful information related to stress distribution and probability of locating areas for ameloblastoma treatment. The limitations of our study are as follows: (1) it adopted uniform muscle forces; (2) viscoelasticity of bone was not taken into account; (3) the number of clinical AB cases was not enough to investigate the statistical analysis. Our results suggest that AB could be cured by the clinical surgery, but may generate an abnormal stress. After surgery, the patient is required to take precautions to minimize overloading stress in the mandible.
Conclusion
Although many finite element studies of ameloblastomas have been published, few have compared the models for BS and AS based on biomimetic geometrical mandible models. The interface between bone tissue and implant during mandibular movement is an important aspect of osseointegration. The intention of this research was to specifically investigate stress distributions and deformations in a mandible with AB, and also to observe AB tissue by radiography and histopathological examinations. The results confirmed that stresses and deformations increased after clinical surgery. Moreover, the clinical relevance of the results is to design an improved structure plate and screw to eliminate the overloading problem at the interface between plates during clinical operation. Using larger diameter screws, special screw threads, thicker plates, or double screw designs in the plate have the potential to solve the present problem. As described above, this information helps in elucidating the behavior of mandibles with ABs.
Acknowledgment
The authors would like to thank the Department of Health, Executive Yuan, Taiwan for financially supporting this research under contract No. MOHW103-TDU-N-211-133001 and No. MOHW103-TD-B-111-01 (Health and welfare surcharge of tobacco products).
6522
References
- Reichart PA, Philipsen HP, Sonner S (1995) Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol 31B: 86-99.
- Bredenkamp JK, Zimmerman MC, Mickel RA (1989) Maxillary ameloblastoma.A potentially lethal neoplasm. Arch Otolaryngol Head Neck Surg 115: 99-104.
- Dunsche A, et al. (2003)Dentigerous cyst versus unicysticameloblastoma – differential diagnosis in routine histology. Journal of Oral Pathology and Medicine 32(8): pp. 486-491.
- Eversole LR, Leider AS, Strub D (1984) Radiographic characteristics of cystogenicameloblastoma. Oral Surg Oral Med Oral Pathol 57: 572-577.
- Pinsolle J, Michelet V, Coustal B, Siberchicot F, Michelet FX (1995) Treatment of ameloblastoma of the jaws. Arch Otolaryngol Head Neck Surg 121: 994-996.
- Morra EA, Greenwald AS (2005) Polymer insert stress in total knee designs during high-flexion activities: a finite element study. J Bone Joint Surg Am 87 Suppl 2: 120-124.
- Goel VK, Panjabi MM, Patwardhan AG, Dooris AP, Serhan H; American Society for Testing and Materials (2006) Test protocols for evaluation of spinal implants. J Bone Joint Surg Am 88 Suppl 2: 103-109.
- Poggie RA, Turgeon TR, Coutts RD (2007) Failure analysis of a ceramic bearing acetabular component. J Bone Joint Surg Am 89: 367-375.
- Beek M, et al. (2001) Three-dimensional Finite Element Analysis of the Cartilaginous Structures in the Human Temporomandibular Joint. Journal of Dental Research 80(10): pp. 1913-1918.
- Koolstra JH, van Eijden TM (2007) Consequences of viscoelastic behavior in the human temporomandibular joint disc. J Dent Res 86: 1198-1202.
- Donzelli PS, Gallo LM, Spilker RL, Palla S (2004) Biphasic finite element simulation of the TMJ disc from in vivo kinematic and geometric measurements. J Biomech 37: 1787-1791.
- Tanaka E, Tanne K, SakudaM (1994) A three-dimensional finite element model of the mandible including the TMJ and its application to stress analysis in the TMJ during clenching. Medical Engineering and Physics 16(4): pp. 316-322.
- Deleyiannis FW, Rogers C, Lee E, Russavage J, Gastman B, et al. (2006) Reconstruction of the lateral mandibulectomy defect: management based on prognosis and location and volume of soft tissue resection. Laryngoscope 116: 2071-2080.
- Kim JH, Rosenthal EL, Ellis T, Wax MK (2005) Radial forearm osteocutaneous free flap in maxillofacial and oromandibular reconstructions. Laryngoscope 115: 1697-1701.
- Militsakh ON, et al. (2004) Use of the 2.0-mm Locking Reconstruction Plate in Primary Oromandibular Reconstruction after Composite Resection. Otolaryngology -- Head and Neck Surgery 131(5): pp. 660-665.
- Cheng, HY, et al.(2013) Stress effect on bone remodeling and osseointegration on dental implant with novel nano/microporous surface functionalization. Journal of Biomedical Materials Research Part A 101A(4): pp. 1158-1164.
- Chu KT, Cheng HY, Pan YN, Chen SY, Ou KL (2013) Enhancement of biomechanical behavior on osseointegration of implant with SLAffinity. J Biomed Mater Res A 101: 1195-1200.
- Cheng HY, et al. (2013) Stress analysis during jaw movement based on vivo computed tomography images from patients with temporomandibular disorders. International Journal of Oral and Maxillofacial Surgery 42(3): pp. 386-392.
- Kashi A, Chowdhury AR, Saha S (2010) Finite element analysis of a TMJ implant. J Dent Res 89: 241-245.
- Wang C, Zhang J, WangX (2009) Multi-Body Contact Finite Element Analysis of Teeth and Orthodontic Devices. Biomedical Engineering and Informatics BMEI '09 2nd International Conference.
- Nagasao T, Miyamoto J, Tamaki T, Kawana H (2010) A comparison of stresses in implantation for grafted and plate-and-screw mandible reconstruction. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 109: 346-356.
- Mariani PB, Kowalski LP, Magrin J (2006) Reconstruction of large defects postmandibulectomy for oral cancer using plates and myocutaneous flaps: a long-term follow-up. International Journal of Oral and Maxillofacial Surgery, 35(5): pp. 427-432.
- Okura M, Isomura ET, Iida S, Kogo M (2005) Long-term outcome and factors influencing bridging plates for mandibular reconstruction. Oral Oncol 41: 791-798.
- Prisman E, Haerle SK, Irish JC, Daly M, Miles B, et al. (2014) Value of preoperative mandibular plating in reconstruction of the mandible. Head Neck 36: 828-833.
- Philipsen HP, Reichart PA (1998) Unicysticameloblastoma. A review of 193 cases from the literature. Oral Oncol 34: 317-325.