Keywords
GERD, Bronchial asthma, FSSG scale, Los Angeles grading
Introduction
Gastro-esophageal reflux disease (GERD) is defined as a condition which develops when the reflux of stomach contents causes troublesome symptoms and/or complications [1]. Atypical and extra-esophageal manifestations of gastroesophageal reflux disease remain an area of intense research. However, in many areas of extra-esophageal manifestations of GERD, there has been very limited progress in the understanding of the role of GERD in generating extra-esophageal symptoms. Based on the Montreal definition, chest pain is not considered an atypical manifestation of GERD, but rather one of the typical symptoms that may resolve from GERD. The atypical presentations of GERD include chest pain, epigastric pain, and nausea. The extraesophageal manifestations of GERD include dental erosions, hoarseness, globus sensation, sore throat, vocal cord irritation, vocal cord polyps and granulomas, posterior laryngitis, chronic cough, asthma, aspiration, pulmonary fibrosis, recurrent pneumonia, sleep abnormalities, and cardiac angina.
Gastro esophageal reflux (GER) is common in patients with pulmonary disease and is involved in the pathophysiology of exacerbation of bronchial asthma. GER is a potential trigger for supraesophageal manifestations of asthma and COPD [2]. A number of studies [3,4] have demonstrated a GERD prevalence ranging from 15% to 82% using pH monitoring in asthma. Distal esophageal stimulation with acid may cause bronchoconstriction or may increase bronchial reactivity via vagal mechanisms [5]. Thus, potential mechanisms exist for GERD to cause asthma symptoms; however, it is unclear whether or not there is a true causal relationship between reflux episodes and asthma symptoms [6]. It has been proposed that GERD is particularly likely to be an exacerbating factor in the subgroup of patients with “difficult-to-control” asthma. In one study [7] of patients with difficult-to-control asthma, GERD was identified as the most common identifiable exacerbating factor; however, subjects were not receiving inhaled steroids but were maintained on oral steroids, and the diagnosis of GERD was based solely on clinical grounds in a proportion of study patients.
The aim of the present study was to evaluate the prevalence of GERD among bronchial asthma patients in a tertiary care hospital. The impact of GERD on the severity of bronchial asthma was also evaluated.
Materials and Methods
Subjects
The prospective study was done at KLES Dr. Prabhakar Kore Hospital and MRC, Belgaum over a period of 2 years from January 2012 to December 2014. All patients with confirmed cases of bronchial asthma according to Global Initiative for Asthma (GINA) guidelines were included in the study. A total of 60 cases were included in the study by computer generated random sampling method. The grading of bronchial asthma was done according to the GINA guidelines [8]. Patients were excluded if they were having chronic obstructive pulmonary disease, chronic smokers, had previous gastric or oesophageal surgery, scleroderma, with malignancy and immune suppressive therapy, and patients on acid suppressive therapy and ACE inhibitors therapy. Ethical clearance was obtained before conducting the study from the Institutional Review Board.
Methodology
All enrolled patients were given questionnaire which included: Age, gender, cigarette smoking, any other illness, any medication history, any previous surgeries, duration of respiratory disease, and any previous surgery. Then all patients underwent GERD FSSGSCALE (Frequency Scale for Symptoms of GERD) questionnaire [9] (Table 1). The FSSG has been proven to be a useful questionnaire for the assessment of GERD, and it was used to determine the prevalence and symptoms of GERD [10]. This questionnaire is composed of 12 questions, which are scored to indicate the frequency of symptoms as follows: never=0, occasionally=1, sometimes=2, often=3, and always=4. The cut-off score for diagnosis of GERD is defined as 8 points. The unique feature of the FSSG is that the questions cover both acid regurgitationrelated symptoms (questions 1, 4, 6, 7, 9, 10, and 12) and gastric dysmotility-related symptoms (questions 2, 3, 5, 8, and 11).
| Questions |
| 1. Do you get heart burn? |
| 2. Does your stomach feel bloated? |
| 3. Does your stomach ever feel heavy after meals? |
| 4. Do you sometimes sub consciously rub your chest with your hand? |
| 5. Do you ever feel sick after meals? |
| 6. Do you get heart burn after meals? |
| 7. Do you have unusual sensation in the throat? |
| 8. Do you feel full while eating meals? |
| 9. Do something gets stuck while swallow? |
| 10. Do you get bitter coming up in to your throat? |
| 11. Do you burp a lot? |
| 12. Do you get heart burn if you bend over? |
| 13. FSSG* - The frequency of scale for the symptoms of GERD |
Symptom scale : Each question was scored as: Never=0, Occasionally=1, Sometimes=2, Often=3, Always=4. If score >8 then GERD was considered to be POSITIVE.
Table 1: Questions of FSSG*.
The confirmation of GERD was done by using objective evidence with Gastro- Esophageal endoscopy to all GERD positive cases obtained by FSSG SCALE Questionnaire method. Grading of GERD was done with endoscopy report according to Los Angeles classification [11] (Table 2). The severity of oesophagitis was categorized by gastro-oesophageal endoscopy as Grade A to Grade D according to the classification used. Then the severity of GERD was compared with severity of bronchial asthma cases. Those cases which were confirmed by endoscopy were taken as positive for GERD and were taken for the final analysis.
| Grade A-Mucosal break=5mm in length |
| Grade B-Mucosal break>5mm |
| Grade C-Mucosal break continuous betwee>2 mucosal folds |
| Grade D -Mucosal break>75% of esophageal circumference |
Table 2: Los Angeles Grading of GERD.
Statistical analysis
Data are expressed as the mean (SD). Comparison of parameters between two groups was done by Student’s t test. Comparisons among three groups were done by one-way ANOVA with Bonferroni’s multiple comparison tests. Differences in frequency between regurgitation and dysmotility symptoms were assessed by the chi-square test. A p value of less than 0.05 was considered significant.
Results
The baseline characteristics are shown in Table 3. The average age in bronchial asthma patients was 44 ± 4.5 years. The BMI in bronchial asthma patients was 20.4 ± 1.2. The main risk factor for bronchial asthma was allergy as evident by the peripheral blood and sputum eosinophilia. The pulmonary functions done at the baseline showed that average predicted FEV1 was 76 ± 23% (2.1 L ± 2.3 L). The regular treatment given for bronchial asthma patients were inhaled steroids/beta2 agonists, Montelukast, oral theophyllines, if required and oral steroids during exacerbations. Blood peripheral eosinophil count was 6.4 ± 2.6%.
| Frequency of GERD |
Number ( % ) |
| % of GERD |
24 (40%) |
| Age (Years) |
44 ± 4.5 |
| Sex (M/F) |
6:/10 |
| BMI |
20.4 ± 1.2 |
| Smoking pack-years |
7 ± 2 |
| Peripheral eosinophilia, % |
6.4 ± 2.6 |
| Sputum, % |
| Neutrophils |
45 ± 10.5 |
| Eosinophils |
34.2 ± 6.7 |
| Pulmonary Functions |
| FEV1, L |
2.1 ± 2.3 |
| FEV1 % predicted,% |
76 ± 23 |
| FEV1/FVC, % |
67 ± 25 |
Acid regurgitation related symptoms
(Questions -1, 4, 6, 7, 9, 10 and 12) |
32 (53.3%) |
Dysmotility related symptoms
(Questions -2, 3, 5, 8 and 11) |
21 (35%) |
Table 3: Baseline characteristics of patients having Bronchial Asthma.
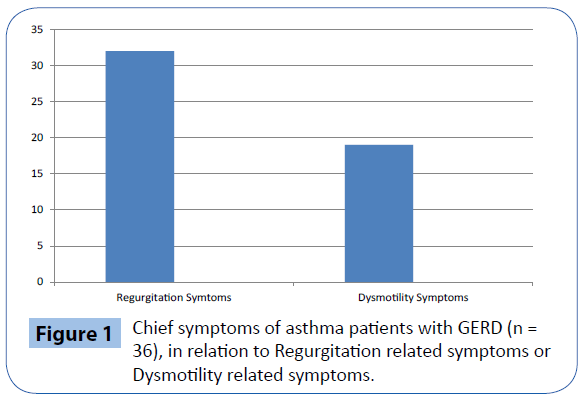
The prevalence of GERD in bronchial asthma patients was 40% (24/60). In FSSG questionnaire, the questions are divided into those covering acid regurgitation-related symptoms (Questions 1, 4, 6, 7, 9, 10, and 12) and those for gastric dysmotility-related symptoms (Questions 2, 3, 5, 8, and 11). The response of the bronchial asthma patients to the various questions in FSSG Questionnaire scale is shown in Table 4. When regurgitationrelated and dysmotility-related symptoms were compared among both the groups, the number of patients showing predominance of regurgitation related symptoms was higher (32 patients, 88.8%) as compared to dysmotility related symptoms (19 patients, 52.7%) (Figure 1).
| Questions of FSSG |
No. |
% |
| 1. Do you get heart burn? |
31 |
51.6 |
| 2. Does your stomach feel bloated? |
19 |
31.6 |
| 3. Does your stomach ever feel heavy after meals? |
23 |
38.3 |
| 4. Do you sometimes sub consciously rub your chest with your hand? |
34 |
56.7 |
| 5. Do you ever feel sick after meals? |
17 |
28.3 |
| 6. Do you get heart burn after meals? |
44 |
73.3 |
| 7. Do you have unusual sensation in the throat? |
38 |
63.3 |
| 8. Do you feel full while eating meals? |
31 |
51.7 |
| 9. Do something gets stuck while swallow? |
32 |
53.3 |
| 10. Do you get bitter coming up in to your throat? |
39 |
65.0 |
| 11. Do you burp a lot? |
21 |
35.0 |
| 12. Do you get heart burn if you bend over? |
37 |
61.7 |
Table 4: Response to the various FSSG Questionnaire.
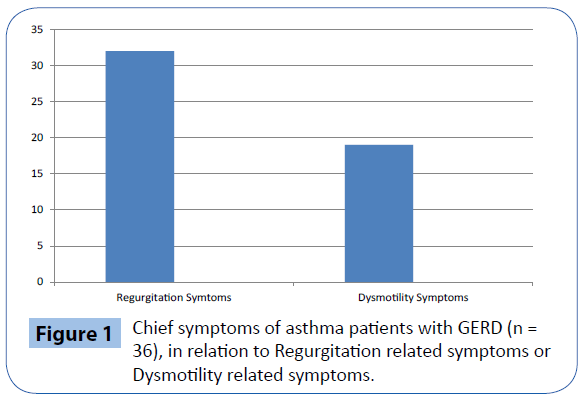
Figure 1: Chief symptoms of asthma patients with GERD (n = 36), in relation to Regurgitation related symptoms or Dysmotility related symptoms.
In the present study, the diagnosis of GERD was made depending upon the upper gastro-endoscopy findings, and all were classified according to Los Angeles classification [11]. It was observed that as the severity of bronchial asthma increased, the severity of GERD also increased (Table 5). This indicates that, in bronchial asthma patients, as the severity of the diseases increases, the severity of the GERD related symptoms also increases. The presence of GERD was not related to BMI in asthma patients. No other risk factors were observed for the presence of GERD in the present study.
| Asthma Grades |
GERD |
Negative |
Total |
| A |
B |
C |
D |
| Intermittent persistent (Grade 1) |
- |
1 |
1 |
- |
10 |
12 |
Mild persistent
(Grade 2) |
2 |
2 |
2 |
1 |
11 |
18 |
Moderate persistent
(Grade 3) |
- |
1 |
2 |
2 |
8 |
13 |
Severe persistent
(Grade 4) |
- |
1 |
3 |
6 |
7 |
17 |
| Total |
2 |
5 |
8 |
9 |
36 |
60 |
Table 5: Comparison between Asthma severity and GERD severity.
All the patients with proven GERD were initiated on PPI therapy as per recommendations for 12 weeks and all these patients showed good control of asthma depending upon the symptoms and pulmonary function tests.
Discussion
In the present study the prevalence of GERD in bronchial asthma patients was observed to be 40%. All the patients were initially evaluated by the FSSG scale for GERD, and were later confirmed by gastro-esophageal endoscopy. The mean age among bronchial asthma patients was 44 ± 4.5 years. From the various studies it has been observed that prevalence of GERD in general population varies from 24% to 80%. In Indian patients the prevalence of GERD in general population varies from 7.6% to 16.2% [12,13]. So the prevalence of GERD observed in bronchial asthma is much higher than the general population in Indian population. The method used for diagnosis of GERD in asthmatic patients varies in different studies; and this may affect the prevalence rates in different studies. In many of the studies only FSSG scale is used for the diagnosis of GERD. However, this prevalence figure is similar to that of other, less severe asthma populations. Field et al. [14] quoted prevalence figures for symptoms of heartburn and regurgitation of 77% and 55% of asthmatics, respectively. Harding et al. [15] retrospectively examined 199 asthmatics, of whom one third were classified as severe, and found 164 subjects (82%) with symptoms of GERD. O’Connell et al. [16] found 72% of consecutive asthma patients had heartburn (136 of 189 patients). Although studies vary in their criteria for diagnosing what level of symptoms is pathologic, symptoms of GERD appear to be more common among asthma populations compared to 35% to 40% reported for the general population [17].
Sontag et al. [9] performed 24-h esophageal pH monitoring in 104 consecutive asthmatic patients, and observed GERD to be 43% in asthma patients. Harding et al. [18] studied 26 asthmatic patients and observed that about 62% of patient had showed abnormal acid exposure. Yet another study by Calabrese et al. [19] also observed high prevalence of GERD (80%) in bronchial asthma patients. Thus present study is comparable to most of the studies published in the literature. Takenaka et al. [20] used FSSG scale and observed that the prevalence of GERD among bronchial asthma patients was 37.4%. Charles et al. [21] used the same FSSG scale in 89 patients and found the prevalence of GERD to be 43%. Harding et al. [22] performed esophageal pH monitoring on 44 patients with asthma, and they observed that 15 patients (34%) had GERD. Calabrese et al. [23] investigated 34 consecutive asthmatic patients with ambulatory esophageal pH monitoring, and they observed the prevalence of GERD to be 80%.
In bronchial asthma patients, the typical symptoms detected by the FSSG were an unusual sensation in the throat and burning sensation in the chest. Another study [24] also reported higher prevalence of regurgitation related symptoms in bronchial asthma patients as compared with COPD patients. Possible mechanisms leading to an unusual sensation in the throat are direct acid reflux or acidic gas reflux. Another mechanism is stimulation of esophageal or laryngeal sensory nerves by gastric acid, because some sensory nerves from these sites terminate in the same region of the central nervous system [25]. Dysmotilityrelated symptoms were less common in asthma patients. A decrease of lower esophageal sphincter pressure is related to the mechanism of GER in both asthma patients, while dysmotility from the esophagus to intestines seemed to contribute to GER symptoms in COPD [25]. All our patients had confirmed cases of GERD with gastro-esophageal endoscopy, thus ruling out functional dyspepsia.
In the present study comparison between bronchial asthma severity and GERD severity was done and it was observed that majority of patients who had Grade D GERD were associated with severe persistent bronchial asthma. Also, it was observed that as the severity grade of asthma increased the severity of GERD also statistically increased. This association was statistically significant (p<0.0001). Yasuo et al. [26] studied GERD in bronchial asthma cases using Los Angeles classification, and it was observed that 5%, 10%, 12.5%,and 12.7% patients had Grade A, Grade B, Grade C, and Grade D GERD respectively. In another study, Ruigomez et al. [27] observed the risk of asthma development following GERD diagnosis. They observed over a 3 years period, 103 cases of bronchial asthma among 17,190 patients of GERD cases. Thus they estimated an incidence of 6 cases of bronchial asthma per 1000 patients of GERD diagnosed. Harding et al. [22] investigated 105 consecutive asthmatic patients with ambulatory esophageal pH monitoring for GERD, and they observed significant association with smoking history in bronchial asthma patients (p<0.0001). Such association was not observed in the present study. Also, no other clear association of GERD with other risk factors including BMI and age group was observed in the present study.
Due to the high prevalence of GERD in bronchial asthma, proper treatment should be initiated at the earliest so that appropriate control of bronchial asthma can be achieved. The goals of treatment include relief of symptoms, healing of esophagitis, prevention of recurrence, and prevention of complications. The principles of treatment include lifestyle modifications and control of gastric acid secretion using drugs or surgical treatment with corrective anti-reflux surgery, if required [28]. Multi-drug therapy may be important in bronchial asthma patients with GERD. The efficacy of proton pump inhibitors may differ between regurgitationrelated symptoms and dysmotility related symptoms in asthma patients with GERD. There is controversy regarding the benefit of PPI use in patients suspected of having reflux-induced asthma. Studies have employed different endpoints regarding efficacy of acid suppressive therapy in this group [29]. Early trials reported improvements in pulmonary symptoms and pulmonary function in patients treated with acid suppressive therapy [30]. In 1994, Meier et al. [31] conducted a double-blind, placebo controlled crossover study which evaluated pulmonary function of asthma patients treated with 20 mg of omeprazole twice a day for six weeks. This study found that 27% patients with reflux had a>20% increase in FEV1. In another study, Sontag et al. [30] evaluated 62 patients with both GER and asthma and divided the group into three treatment arms: control, treatment of reflux with ranitidine 150 mg three times a day, or surgical treatment with Nissen fundoplication. After a two year follow up, 75% of surgical patients had improvement in nocturnal asthma exacerbations, compared to 9.1% and 4.2% of patients on medical therapy and controls, respectively. Additionally, there was a statistically significant improvement in mean asthma symptom score, but no improvement in pulmonary function or reduction in the need for medication between the groups. Littner et al. [32] followed 207 patients with symptomatic reflux, who were treated with either placebo or a proton pump inhibitor twice a day for 24 weeks. The study showed that medical treatment of reflux did not reduce daily asthma symptoms or albuterol use and did not improve pulmonary function in this group of asthmatic patients. Similarly, a recent study conducted by the American Lung Association Asthma Clinical Research Center [33] randomised 412 patients with poor asthma control to either esomeprazole 40 mg twice daily or placebo. After 24 weeks of follow up, the study found no treatment benefit to PPI therapy in asthma control. A Cochrane review of GER treatment for patients with asthma found only minimal improvement of asthma symptoms with reflux therapy [34]. Encouragingly, a recent controlled trial in asthmatics suggested therapeutic benefit with PPIs in the subgroup of asthmatics with both nocturnal respiratory and GER symptoms [35]. Thus, the issue of asthma control by treating reflux in patients who have asthma is not yet clear. Therefore, the current recommendation in patients with asthma (with or without concomitant heartburn or regurgitation) is similar to those in patients with chronic cough and laryngitis, suggesting the initial empiric trial of twice daily PPI’s for 2-3 months [29]. In those responsive to therapy for both heartburn and/or asthma symptoms, PPI’s should be tapered to the minimal dose necessary to control symptoms. In unresponsive patients, testing for reflux, by pH testing and/or impedance-pH monitoring may be needed to measure for continued reflux of acid or non-acid material, which could still be responsible for patients’ asthma exacerbation.
The reported prevalence of clinically silent GERD defined by pH monitoring varies between 29% and 62% . The analysis of cough and its correlation to reflux episodes remains problematic. Patients underreport cough, and the timing of coughs can be misreported. Paterson et al. suggested that combining ambulatory esophageal manometry and pH monitoring may provide an objective measure of the temporal relationship between cough episodes and reflux that is superior to relying on patient reporting. They found that if single coughs and cough bursts were considered; patients reported a mean of 4.4 coughs per study out of 36.9 recorded manometrically (p = 0.001). Recently Leggett et al. [17] has observed that in difficult-to-control asthma, GERD is common, but identification and treatment of GERD do not appear to relate to improvement in asthma control in this population. Thus, it was concluded that while GERD is common in difficult asthma, proactive identification and treatment of GERD using high-dose proton pump inhibitors does not relate to asthma outcome, at least in this population.
There are certain limitations in this study. The present study was done in a tertiary care hospital. Hence the results cannot be generalised at community level. Secondly, the sample size is small. Thirdly, the presence of the silent reflux cannot be ruled out, as we have not done 24-hour pH monitoring of the gastric acid, which is considered as the gold standard technique in the diagnosis of GERD. Lastly, the effect of proton pump inhibitors in GERD in asthma was evaluated only by the clinical symptoms and pulmonary functions. Repeat endoscopy was not performed in any patients.
In conclusion, in the present study, more than one third of adult asthmatic patients had GERD. These patients do not often have typical reflux symptoms such as heartburn or regurgitation. However, the presence of typical reflux symptoms in an asthmatic patient does not seem to guarantee the presence of pathologic acidic esophageal reflux.
9570
References
- Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R; Global Consensus Group (2006) The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 101: 1900-1920.
- Harding SM(2003) Recent clinical investigations examining the association of asthma and gastroesophageal reflux. Am J Med 115 Suppl 3A: 39S-44S.
- Nagel RA, Brown P, Perks WH, Wilson RS, Kerr GD (1988) Ambulatory pH monitoring of gastro-oesophageal reflux in "morning dipper" asthmatics. BMJ 297: 1371-1373.
- Sontag SJ, O’Connell S, Khandelwal T (1990) Most asthmatic patients have gastroesophageal reflux with or without bronchodilator therapy. Gastroenterology99:613-620.
- Herve P, Denjean A, Jian R, Simonneau G, Duroux P (1986) Intraesophageal perfusion of acid increases the bronchomotor response to methacholine and to isocapnic hyperventilation in asthmatic subjects. Am Rev Respir Dis 134: 986-989.
- Richter JE (1999) Asthma and gastroesophageal reflux disease: the truth is difficult to define. Chest 116: 1150-1152.
- Irwin RS, Curley FJ, French CL (1993) Difficult-to-control asthma. Contributing factors and outcome of a systematic management protocol. Chest 103: 1662-1669.
- Global Initiative for Asthma (GINA) (2015) Global strategy for Asthma Management and Prevention. Bethesda, National Institute of Health.
- Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd (1997) Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology 112: 1448-1456.
- Kusano M,Shimoyama Y, Sugimoto S, Kawamura O, Maeda M, et al. (2004) Development and evaluation of FSSG: frequency scale for the symptoms of GERD. J Gastroenterol 39: 888-891.
- Kusano M,Ino K, Yamada T, Kawamura O, Toki M, et al. (1999) Interobserver and intraobserver variation in endoscopic assessment of GERD using the "Los Angeles" classification. GastrointestEndosc 49: 700-704.
- Bhatia SJ, Reddy DN, Ghoshal UC, Jayanthi V, Abraham P, et al. (2011) Epidemiology and symptom profile of gastroesophageal reflux in the Indian population: report of the Indian Society of Gastroenterology Task Force. Indian J Gastroenterol 30: 118-127.
- Sharma PK,Ahuja V, Madan K, Gupta S, Raizada A, et al. (2011) Prevalence, severity, and risk factors of symptomatic gastroesophageal reflux disease among employees of a large hospital in northern India. Indian J Gastroenterol 30: 128-134.
- Field SK, Underwood M, Brant R, Cowie RL (1996) Prevalence of gastroesophageal reflux symptoms in asthma. Chest 109: 316-322.
- Harding SM,Guzzo MR, Richter JE (1999) 24-h esophageal pH testing in asthmatics: respiratory symptom correlation with esophageal acid events. Chest 115: 654-659.
- 1O’Connell, Sontag SJ, Miller T (1990) Asthmatics have a high prevalence of reflux (GER) symptoms regardless of the use of bronchodilators. Gastroenterology 98: A97.
- Leggett JJ, Johnston BT, Mills M, Gamble J, Heaney LG (2005) Prevalence of gastroesophageal reflux in difficult asthma: relationship to asthma outcome. Chest 127: 1227-1231.
- Harding SM, Richter JE (1997) The role of gastroesophageal reflux in chronic cough and asthma. Chest 111: 1389-1402.
- Calabrese C, Fabbri A, Bartolotti M, Cenacchi G, Areni A, et al. (2003) Dilated intercellular spaces as a marker of oesophageal damage. Aliment pharmacolTher 18:525-532.
- Takenaka R (2010)The use of FSSG scale in assessment of GERD in asthma. AllegolImmunopathol 38:20-24.
- Charles A, Adeyeye OO, Ogbera AO (1997) Prevalence of GERD among bronchial asthma patients. Gastroenterol 113: 755-760.
- Canning BJ,Mazzone SB (2003) Reflex mechanisms in gastroesophageal reflux disease and asthma. Am J Med 115 Suppl 3A: 45S-48S.
- Yasuo SH, Kunio D, Setsuo K (2003) High prevalence of GERD with minimal mucosal change in asthmatic patients. Clin J Gastroenterol 116:26-31.
- Ruigómez A, Rodríguez LA, Wallander MA, Johansson S, Thomas M, et al. (2005) Gastroesophageal reflux disease and asthma: a longitudinal study in UK general practice. Chest 128: 85-93.
- Nwokediuko SC(2012) Current trends in the management of gastroesophageal reflux disease: a review. ISRN Gastroenterol 2012: 391631.
- SaritasYuksel E,Vaezi MF (2012) Extraesophageal manifestations of gastroesophageal reflux disease: cough, asthma, laryngitis, chest pain. Swiss Med Wkly 142: w13544.
- Sontag SJ, O'Connell S, Khandelwal S, Greenlee H, Schnell T, et al. (2003) Asthmatics with gastroesophageal reflux: long term results of a randomized trial of medical and surgical antireflux therapies. Am J Gastroenterol 98: 987-999.
- Meier JH, McNally PR, Punja M, Freeman SR, Sudduth RH, et al. (1994) Does omeprazole (Prilosec) improve respiratory function in asthmatics with gastroesophageal reflux? A double-blind, placebo-con- trolled crossover study. Dig Dis Sci 39: 2127-2133.
- Littner MR, Leung FW, Ballard ED, Huang B, Samra NK (2005) Effects of 24 weeks of lansoprazole therapy on asthma symptoms, exacerbations, quality of life, and pulmonary function in adult asthmatic patients with acid reflux symptoms. Chest 128: 1128-1135.
- American Lung Association Asthma Clinical Research Centers, Mastronarde JG, Anthonisen NR, Castro M, Holbrook JT, et al. (2009) Efficacy of esomeprazole for treatment of poorly controlled asthma. N Engl J Med 360: 1487-1499.
- Gibson PG, Powell H, Coughlan J, Wilson AJ, Hensley MJ, et al. ( 2002) Limited (information only) patient education programs for adults with asthma. Cochrane Database Syst Rev 2:CD001005.
- Kiljander TO, Harding SM, Field SK, Stein MR, Nelson HS, et al. (2006) Effects of esomeprazole 40 mg twice daily on asthma: a randomized placebo-controlled trial. Am J RespirCrit Care Med 173: 1091-1097.
- Harding SM,Guzzo MR, Richter JE (2000) The prevalence of gastroesophageal reflux in asthma patients without reflux symptoms. Am J RespirCrit Care Med 162: 34-39.
- Paterson WG, Murat BW (1994) Combined ambulatory esophageal manometry and dual-probe pH-metry in evaluation of patients with chronic unexplained cough. Dig Dis Sci 39: 1117-1125.
- Xu X, Chen Q, Liang S, HanjingLv, Qiu Z (2014) Comparison of gastroesophageal reflux disease Questionnaire and multichannel intraluminal impedance pH monitoring in identifying patients with chronic cough responsive to antireflux therapy. Chest 145:1264-1270.