Keywords
Social networks; Health informatics; Health disparities; Health policies
Introduction
Factors that contribute to health disparities are complex and intertwined, but we know that demographics, socioeconomic status, lack of access to care, and certain risky behaviors contribute strongly to health disparities in rural areas [1-3]. In order to reduce health disparities in rural populations, institutional strategies and approaches that empower residents to seek better health, help change local healthcare practices, and mobilize communities to implement evidence-based public health programs to reduce health disparities across a broad range of health conditions is critical. Furthermore, eliminating health disparities to emerging factors that affect members in rural communities more readily [4-6]. Health care in the future will tout the expanded use of social networks to “crowdsource” an individual’s health plan, where medical treatments and preventive care will be more informed [7-10]. Initiatives such as eHealth may potentially enhance quality of care and may reduce health disparities in rural communities.
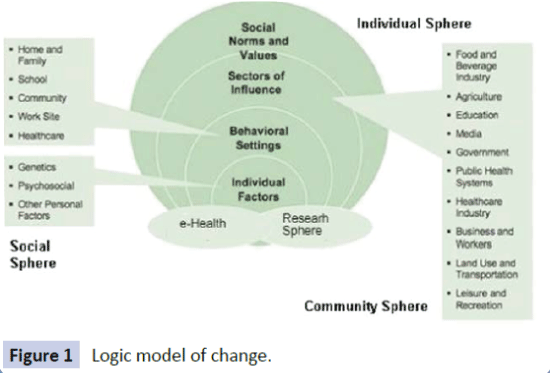
eHealth is an emerging field referring to health services and information delivered or enhanced through the Internet and related technologies. The term “eHealth” characterizes not only a technical development, but also an attitude and a commitment for networked, global thinking, to improve health care locally, regionally, and worldwide by using information and communication technology [11]. We propose that greater collaboration among community partners formed through capacity-building (social sphere) and evidence-based (research sphere) dissemination activities, along with individual social support (individual sphere) is a way to diffuse the necessary information technology to affect health disparities (Figure 1). The integration of these objectives elevates “eHealth” from only having access to information to defining communities and individuals with the access to crucial resources, such as knowledge, skills, and supportive organizational and social structures, to make effective use of e-technology in order to enable social and community objectives. Such an integration of eHealth within communities would require a paradigm shift in thinking about the digital divide, as inequalities relating to information and communication technology are typically associated with access [12,13].
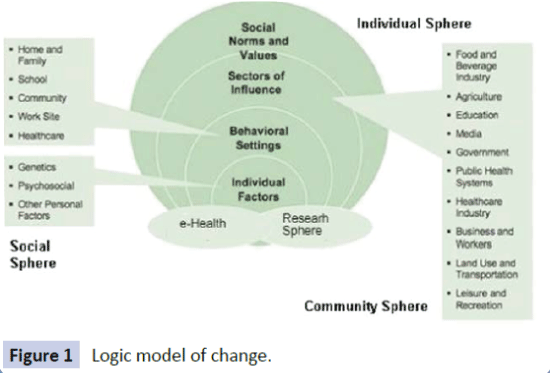
Figure 1: Logic model of change.
In addition to eHealth, social interactions and social support have consistently been beneficial in effectively improving patient health and wellbeing [14]. Social networks channel the diffusion of ideas and practices and are the nexus for the creation of cultural norms and beliefs. Thus, social networks may play a vital role in community-based interventions that depend on the spread of new ideas for their success. We know that when groups of people, particularly individuals who are familiar and interconnected with one another, engage in an activity, such as a health improvement behavior, they are more likely to sustain the collaboration and ultimately, respond positively. Despite this correlation, social media is still the most common methodology for dissemination, not dialogue. Social media transmits the values and norms of the people who built (and continue to build) the sites we use. Thus, it is imperative to understand that these values impact the conversations taking place within these networks. In contrast to the early days of social media, when consumers were focused on publishing to the world and communicating with peers, increased globalization has turned these networks into broadcasting channels. Users will become more passive with time and will increasingly turn to organizations and experts for interesting content. However, despite the trend of social media, the real innovations in health disparities are likely to be facilitated through community discussions.
Social networks play a crucial role in the process of individual participation in collective actions. The goal of social networking within the realm of rural community mobilization should strengthen social capital and community cohesion; contribute to civic empowerment and engagement, and build individual and community capacity. Social networks may also promote a willingness to work alongside pre-established services to create new partnerships. Fulfilling these goals would enhance the community-based participatory capacity of community partners through the identification of resources for community engagement projects and community-based participatory training for research. As a result, health disparities may be reduced. But the question at hand is how to shape social networking to affect health disparities with a “people driven” focus to bring existing networks online in a healthcare context to effect improved health outcomes.
The purpose of this review is to present perspectives associated with informatics strategies that link science to community resources that will improve research quality, enhance community capacity, and improve health outcomes through discussion among healthcare workers and end users. Informatics efforts can provide an avenue to bring researchers and practitioners active in “geo-local” and “virtual” communities together to collaborate in research and real-world projects associated with health disparities [15]. An expected outcome of working with pre-established partnerships is to identify the most effective models for sustaining informatics initiatives both economically and socially while benefiting those most at risk [16-18]. However, unlike social media, these models must be shaped in a way that fosters dialogue and not just fostering the dissemination of information.
Framing the social network challenge
The traditional view of community members as passive recipients of health care services must therefore transform into an enlightened view, where members are seen as smart and capable collaborators [19,20]. Individuals require information as they engage in self-help, self-care, and disease management activities, [18,21-23] but community members must be compelled to speak or discuss this information [24] in order for a systemic dialogue to begin. Online communities can be categorized in terms of virtual groups based off a pre-established community group (a physical grouping) and a virtual network- that is based off the web community [24]. The membership of an online community based upon a physical grouping, e.g. focus group, community council, or neighborhood watch group, is more positively correlated with social bonding gratification and negatively correlated with information-seeking gratification [24]. Self-help activities may include general health education, and life style modification strategies both of which contribute to quality of life [23]. Furthermore, building and sustaining networks of individuals and private entities for community health improvement, which includes establishing and maintaining communication channels, exchanging resources, and coordinating collaborative partnerships beneficial to social support is necessary [18,21,22]. Through interpersonal interactions, community engagement, and forming partnerships and collaborations, we can enhance, grow and strengthen social networking for promoting health throughout the community by means of discussion.
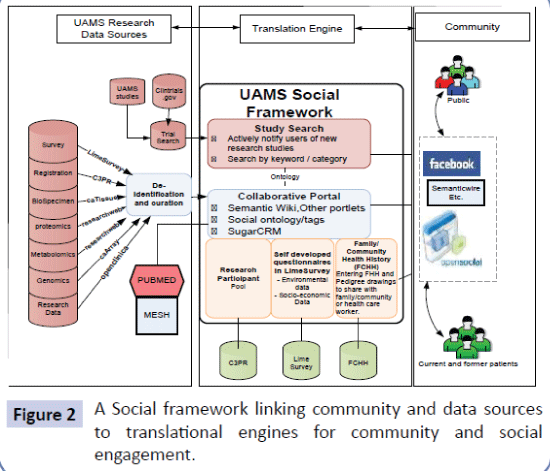
Reducing health disparities requires creativity in maximizing information technology within all segments of the population to empower communities and the individual to make complex health choices, influence the public agenda, advocate for policies and programs, promote positive changes in the socioeconomic and physical environment, improve the delivery of public health and health care services, and encourage social norms that benefit overall health and quality of life. Social media can provide a safe environment for mobilizing people to effect change both at the individual and community levels [23,25]. For example, anti-tobacco advertisements have been found to be effective in enhancing knowledge as well as in transforming to positive attitude of the people about tobacco use [26]. Social media venues have also undergone a significant shift to greater bidirectional or multidirectional communication in recent years to engage diverse communities and youth [23]. Technology venues represent opportunities for health messaging that have yet to be fully utilized, but would require a level of eHealth literacy from community members that already have their own demands and barriers [23,25,27,28] (Figure 2).
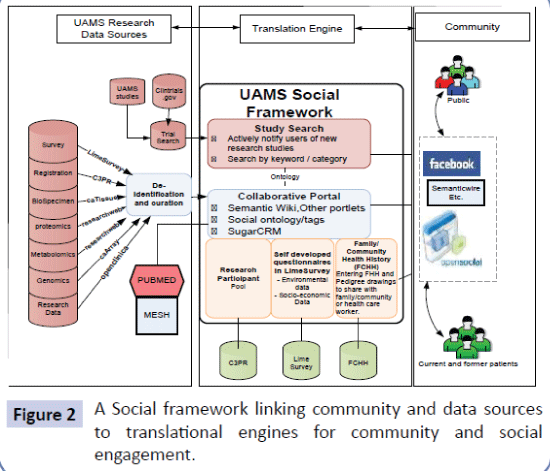
Figure 2: A Social framework linking community and data sources to translational engines for community and social engagement.
Depicted is a social framework in which community members can own the process and the data collected/generated. The left frame is the University of Arkansas for Medical Science’s (UAMS) research informatics infrastructure that currently utilizes caBIG and other open-source technologies. We propose to create a de-identification and entity recognition (e.g. OpenCLAIS) process by which research data might be shared back to the community. Furthermore, publications related to a social tag (i.e. the topic being investigated) could be brought to community members to have one-stop access to all possible information. The middle translation engine serves as a bridge between the research sphere and the community by providing tools and services for the community to start discussion on their own and has several components; 1) searching studies that might be of interest to the community can be searched/accessed after the UAMS’ studies (and ClinicalTrials.gov trials in the area) ontologically curated to provide machine guided matching options; and 2) the collaborative portal is where the community will have access information (i.e. semantic wiki), ask questions (i.e. discussion portlets), start a community ((i.e. social network application programming interface (APIs)), start collecting data (i.e. Limesurvey and Family/community Health History), lead/ maintain the community (i.e. sugarCRM, a customer relationship management system for community management), participate in research pools (i.e. caBIG Central Clinical Participant Registry (C3PR)). To be developed social ontology will allow data from disparate sources to be accessed and understood. The Right Frame is where the community is located. Many current users of social networking sites might be able to access the data/ discussions and/or participate without leaving the environment they are in via social network APIs.
Framing the Informatics Challenge
Health informatics has much to offer to close the gap in health disparities [18,21,22]. Health information systems address the collection, storage analysis, interpretation, and communication of health data. To effect change, social networking should be viewed as a means to advance “eHealth” from an informative database to a holistic workflow that is centered on informatics and two-way dialogue. This concept requires a systemically prepared community with the knowledge, skills, and supportive organizational and social structures to make effective use of e-technology to fulfill the social and community objectives that are in demand by a community.
Consumer Health Informatics supports the development of information management, discovery tools, insurance of health information literacy, as well as re-engineering clinical and research practices in order to fully integrate community members from patients into partners in health care. Community Informatics (CI) has a focus on social capital associated with personal, social, cultural or economic development both within and between communities [29]. The term ‘social media’ is used interchangeably with Web 2.0 to describe sites and applications that allow information sharing and interactive activities among online communities, such as blogs, wikis, content-sharing sites, virtual worlds, and social networking sites [30]. Yet, very little has been published about how social networking might be utilized for health promotion interventions [31].
In contrast, Social informatics (SI) is the study of information and communication tools in a cultural or institutional context. SI introduces information technology in a social context. SI reflects an intriguing social phenomenon that emerges when people use information technology, demonstrated by the ways that people develop trust in virtual teams, and how individuals share the impact of their illness as a means to help others. In this context, social networks provide opportunities to foster opinions, collate information, collect history, and reframe questions as the discussion evolves [32]. The concept of SI can lend to an analysis of data, which can improve current practices. For example, tweets on specified topics may elucidate trends, or [33] gathering data from individuals via social media may be comparable to existent data as well as less labor intensive, leading to new translational research questions [34]. This alternative method could potentially overcome the data collection challenge in cohort and prospective studies [35].
eHealth and Communities - Web-based Information Dissemination
Individual health is influenced by a variety of factors including: family history, genes, personal lifestyle, habits and ultimately social networks. The collective or social health of a community is not simply the sum of the health of its residents, but in reality reflects many of the community's characteristics such as the environment and food systems. With the increase in online social networking, several web site characteristics emerged that contribute to the local communication ecology. Analyses for community websites that address the communication ecology have been documented in the study, Online Neighborhoods Networks (ONN) (info@ networkedneighbourhoods.com). The implementation of both web-based eHealth expansion and the individual’s access to resources facilitates growth. With this expansion of information on how to understand and improve the health of communities, the health of individuals is consequently improved. However, the characteristics found in the study support that websites need not only to be readily available, but actually need to be established and maintained by local residents. In addition, most of the content needs to relate to local issues and community interests. The forums should be open to discussions and contributions from anyone living in the area, or from anyone interested in the area.
The ability of online health interventions to merge internetapplications and health practices has prompted diverse approaches to improve outreach, effectiveness, adoption, implementation, and maintenance of web-based interventions [36]. Due to the added emphasis web-based programs place on literature and gathering resources reflective of communities’ needs, web-based health interventions are able to present information, forecast outcomes, and construct informed future decisions in order for patients to effectively manage their health [37]. Web-based decision support interventions, worksite interventions, and community-based interventions have distinct applications capable of addressing patients’ and communities’ unique needs (Table 1).
| Title |
Description |
Characteristics of Web-Based Health Intervention |
| Community or Research Based Intervention |
How intervention was developed |
| Prosdex |
Prosdex is a web-based support intervention geared toward assisting men deciding to undergo the protestic specific antigen test. |
Research Based Intervention |
Various universities along with the national Prostate Cancer Risk Management Programdeveloped Prosdex. |
| Aminodex |
Aminodex is a web-based support intervention to assist women and their partners in deciding on screening for fetal abnormalities. |
Research Based Intervention |
Health professionals from the University of Cardiff and affiliating universities initiated the development of Aminodex. |
| Bresdex |
Bresdex provides support to patients deciding whether lumpectomy or mastectomy is the best treatment option for combating breast cancer. |
Research Based Intervention |
Health professionals from the University of Cardiff and affiliating universities initiated the development of Bresdex. |
| Health Choice: Food & Fitness |
Teenagers’ obstacles to practicing health habits were translated into a website with various web-tools addressing barriers to eating and exercising. |
Community Based Intervention |
Researchers probed teenagers’ interests relevant to health and exercise to develop the teenage online health intervention. |
| Tompkins County Health |
Webpages addressing teen smoking, dieting, and exercising were developed to support health efforts of Community members and employees within Tompkins County. |
Community Based Intervention |
Community members and employees in Tompkins County along with researchers collaborated to develop the Tompkins County Health Website. |
| Every Block a Village |
Community members in Austin & Chicago developed a website to raise awareness of cultural and social factors preventing community growth and access to health care. Their website is tailored toward providing resources. |
Community Based Intervention |
Community members and organizations worked with researchers to create a website possessing web-tools and literature relevant to communities in Austin, Chicago. |
| Community Vital Signs (CVS) |
CVSis a web-based informatics tool for community members, investigators, and policy makers to share data and display emerging health disparities. |
Research Based Intervention |
San Francisco Department of Public Health initiated CVS. |
| Get Healthy Harlem (GHH) |
GHH allows communities to discuss healthier living through sharing and commenting about events encouraging healthier lifestyles. GHH serves a medium to support and facilitate health habits. |
Community Based Intervention |
GHH was developed in junction with community members, community organizations, public agencies, and researchers. |
Table 1: Community and patient focused web-based health interventions.
Boyd and Ellison [38] define Social Network Sites as ‘web-based services that allow individuals to (1) construct a public or semipublic profile within a bounded system, (2) articulate a list of other users with whom they share a connection, and (3) view and traverse their list of connections and those made by others within the system.
The role of eHealth and informatics can be viewed in the context of addressing serious shortages of qualified health service professionals and in building a stronger health system capacity. In this regard, social networking among trusted individuals might be beneficial to community health, similar to community health workers (CHW) who function as both health navigators and as trusted sources of information. There are a myriad of evaluations of CHWs, and the meta-analyses of these studies reveal significantly increased access to health care, improved asthma symptoms, a decreased use of urgent care, improved blood pressure control, an increase in breast feeding, and a decrease in high-risk sexual behavior [39-42].
The websites in Table 1 can be grouped into those that possess essential features of community-based websites and those that don’t. GetHeathyHarlem and Health Choices: Food and Fitness implement infrastructures necessary to meet the principles described within the study ONN. Both websites incorporated the targeted population from conception, utilized publishing web features, and implemented focus groups reflective of populations’ demographics. Health Choices: Food and Fitness took appropriate measures to ensure that content remained relevant and transparent. GetHeathyHarlem and Health Choices: Food and Fitness describe unique essential features that offer opportunities for users to serve as content managers; in turn, users’ activities and feedback represent a template for further development.
Community Vital Sign (CVS) is a web-based informatics tool for displaying communities’ health in relation to the frequency of emerging health disparities. CVS serves as a community-based web-tool, yet it involves marginal community involvement and operates as a research initiated web-tool. CVS incorporates ONN principles of community engagement in order to achieve its primary goal of serving as an informatics tool for sharing research findings and connecting experts. Researchers, policy makers, stakeholders, and the general public are able to share data through web features depicting the prevalence of local health disparities.
Community-based, organized websites such as EveryBlockaVillage provide the community engaged principles outlined in ONN, but lack significant user-publishing web features. EveryBlockaVilliage captures communities’ interest through assessing their needs and translating them into a community defined website. Resource and web-tool reliance on traditional top-down flow of information as the primary module for sharing and interfacing web-tools, limited user-publishing web-tool functionalities and cooperative community sharing opportunities. EveryBlockaVillage limited sharing features allowed it to serve as an online awareness resource for communities, instead of a community supported social network. ONN concludes that community members are advocates for ensuring that websites maintain fluid changes relative to their appearance and literature. These are traits portrayed precisely in GetHealthyHarlem.
Prosdex, Aminodex, and Bresdex miss the mark. Although these websites attract individuals nation-wide and create web communities around common health conditions, they lacked a unique geographical community. Tompkins County Health intervention is similar to EveryBlockaVillage as it captures the communities’ interests and translates them to into webpages. All of these websites are attempting to address eHealth disparities through different lenses, but there is still no option that satisfies all of the components. In order to better accommodate community health through dialogue and web-based sites, an option needs to be simulated to bridge the gaps in the existing options.
Social Factors and Technology
A healthy lifestyle can be thought of as a broad description of people's behavior in three inter-related dimensions: individuals, individuals within their social environments (e.g. family, peers, community, workplace), and the relation between individuals and their social environment. Interventions to improve health through lifestyle choices can use comprehensive approaches to address health as a social or community (i.e. shared) issue. Social factors relate to changes in the behavior, tastes, and lifestyles of communities. The idea that social factors determine the acceptance of information and technologies, and thus may lead to sustainable impacts upon health disparities, is widely accepted. Other factors influencing the adoption of new sustainable practices may include the age and education level of the community member. A community's most commonly used resource is typically trusted despite that it is not necessarily the most accurate source of information. Knowing that influence by community organizations plays a large role in helping communities adopt new practices is crucial. Methodology and practice where the community contributes to obtaining and disseminating information will likely influence the community motivation towards adopting technologies and interventions.
The American Recovery and Reinvestment Act of 2009 included $7.2 billion for the development and expansion of broadband infrastructure and services in communities across the country. Priority was given to development of low-income, underserved, or rural communities. These resources manifested into technologies theoretically suitable for improving digital access, patient-professional relationship, and awareness. Underserviced communities’ limited adoption of eHealth technology accounts for the present disparity they represent in obtaining access to preventative health measures. Yet health professionals treating these populations are infrequently acknowledged as contributors to health inequalities in rural communities.
Health professionals serving low-income and underserved individuals are at higher dispositions of only incorporating the minimum infrastructures necessary for managing electronic health records (EHR). Additionally, they are more likely to experience difficulties in adopting health IT than private physicians and hospitals that serve different populations (NORC, 2010). Various forms of EHR systems have demonstrated the ability to improve practice management systems and physician rapport through increasing efficiency and quality of patientphysician interactions. These systems incorporate diverse software in order to enhance productivity, recording, sharing, and collaborations between medical experts and health care organizations. They also incorporate a patient-centric dashboard, registries (vaccination tabs), and other patient alerts. Notable success in EHRs, such as Siemens Lifetime Clinical Record (LCR), in San Francisco’s Community Clinics Consortium has resulted in legal actions by the San Francisco Department of Public Health to obligate LCR implementation in all health care delivery systems.
Health care delivery through online resources has been efficient in implementing principles of IT acquisition and implementation in order to address health disparities. These principles alone are unlikely to resolve disparities between populations that do or do not experience regular access to online health resources and do or do not experience low mortality and morbidity rates [43]. Therefore, cumulative interventions targeting core issues including low income, health literacy, and self-efficacy are more suitable for gradually eliminating disparities. Zanaboni and Lettieri [44] recognized at risk populations are ill equipped to independently combat issues in the realm of eHealth due to overarching policies such as articulating fairness, rationality, and efficiency surrounding online health care delivery. Moreover these populations lack social bridges (i.e. broadband providers, software packages, investors, and energy resources) and tools necessary to establish network substructures [45]. These populations are also likely to lack expertise to maintain long-term management plans and IT personnel to optimize network usage.
Streamed healthcare inadvertently possesses social strains allowing it to develop as a tool for enhancing the awareness and health competency of higher income and educated populations [46,47]. Unfortunately, the opposite is true for marginalized communities. Underserved communities with high poverty and low literacy will began to experience 1) higher mortality from preventive complications and 2) greater disconnects with health professionals as eHealth resources become more integrated in medical practices. Without assistance these populations are likely to fall further behind as eHealth advances. Social assistance and strategies incorporating private and public infrastructures can curb health disparities by creating providing equitable health opportunities. Providing incentives to private entities that serve disadvantaged populations must include but is not limited to: subsidizing broadband serving vulnerable populations, stores offering affordable, healthy options, workplaces incorporating healthier management practices, and media articulating active patient roles in managing health [44,48,49].
eHealth focuses on providing creditable expert advice which has contributed to a social inequity beyond the scope of IT access [50]. The issue appears across socioeconomic populations and is due to an individual’s ability to articulate and comprehend, which takes place independently of a population’s access, suggesting that the dilemma hinges on more than just the digital divide. eHealth literacy is the “ability to seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem” [27]. Online health websites seeking to inform users on health complications may actually impose barriers to eHealth literacy. Websites are often developed outside the realm of targeted populations not being culturally sensitive to ease of navigation, content transparency, and preference to how communities process, understand, and apply information to their lives. Consistent overlooking of these facts might have unintentionally fostered a second divide based on eHealth literacy [51].
Access versus Meaning: The Yin and Yang of Dissemination and Discussion
The narrowing divide in eHealth technology across population groups, as a result of the declining divide in Internet access and computer ownership, warrants further exploration [52]. Streaming of high quality data is reaching more underserved geographic areas, with advances in online resources and reduced cost of broadband. However, increased access does not equate to improved interpretation and application of data. Belief systems, religious and cultural values, life experiences, and group identity act as powerful filters through which information is received. Matching the cultural characteristics of communities to public health interventions, that are designed to affect individuals within the group, may enhance receptivity to, acceptance of, and salience of health information and programs. Ten factors that affect meaning from data are the following:
Local commitment to health: Short-term impacts without local involvement ("buy in") are unlikely to change cultural norms or be sustained. Cultural norms often need an injection of resources to stimulate change. The North Karelia project (a long-term community-based project in Finland to decrease cardiovascular risk factors) was successful because leadership originated within the community and provided for long-term community involvement in goal setting and strategic planning. Within the context of community, the project also provided for small-scale initiatives with focused objectives, further contributing to its success [53].
Social Capital – building trust and the structural mechanisms that shape community norms:
Measuring and mapping existing social networks is a critical step in building the kinds of supportive and productive relationships encapsulated in the term ‘social capital’ [54]. Social networks are a necessary condition for social capital that forms a powerful pattern of connectivity as a tool for evidence-based policy and practice.
Sustainability: Interventions must parallel the resources available to sustain them [55]. Often the "gold standard" intervention that may result in the most impressive outcome is not sustainable over time or is too costly to implement beyond the pilot stage.
Target Populations: Decisions must be made as to whether an intervention is influencing the identified target group. Generally, those with the most limited resources for a healthy lifestyle are at the highest risk, requiring greater investment.
User Data: The Internet is all about people; however, ultimately humans know much more about friends and family than any computer ever could. Computers are quantitative, juxtaposing human interaction, which is qualitative. As such, computer programming is currently limited in that it is unable to sufficiently consider motivations, humanity, and situational contexts.
Curation: The importance of curation (collecting and sorting content) and hashtags as a means to aggregate content is becoming crucial to our economy, especially advertising. By aggregating users’ interest, parties are able to dissect what individuals really discuss on these sites. eHealth can therefore utilize this trend by using the data to enhance their user web publishing, and incorporating content that is relevant to users today. Rather than sifting through RSS readers, which collects news from various websites and provide news updates from a website in a simple form for your computer, Twitter feeds and news sites, curation provides information quickly in snapshots of viewer’s opinions and discussions. Curation is only going to explode in popularity as the public-seeks more efficient solutions.
Trusted sources: There is a great need for an established site, in good rapport, to rapidly test innovations in community health and in turn distribute the evidence, with hopes that successes can be replicated in multiple communities. In order to do so, policies would have to be shaped to provide individual ownership of personal data, while offering individuals and communities the ability to opt in to release their data to technology vendors and entrepreneurs.
Engagement/Conversation/attention span – what people want to know versus what others want them to know: Creating opportunities for community members to come together, deliberate, and take action collectively to address problems or issues that members themselves define as important, is critical so citizens themselves can decide what is appropriate and/ or needed. Therefore, meaningful use of the health domain by laypersons will require laypersons to become institutional in website conception and their view of credibility becomes more significant throughout development.
Economy: With an expected, but unprecedented, reduction in public sector spending, and a new culture of localism and co-production, community members will be expected to assume greater responsibility for what happens in their communities. It seems clear that neighborhood websites can play a role in fashioning these new relationships, providing transparent, informative spaces where issues are raised and, whenever possible, local solutions are found.
The dimensions of the network: Build community storage systems for multi-source integrated health data, including genomics, proteomics, sensors, lab data, pharmaceutical prescriptions, environmental data, social media data and non-obvious health data that will emerge as we learn to improve community health. Use regional partnerships between major clinical institutions, systems biology institutes and communities with consumers and patients learning to improve population and individual health.
A Model of Integration for community engagement
With the emergence of social media and networking applications, by far the most common web-based collaborative tools are wikis and blogs, which provide a content editing feature, with only a minimal technical background. The tools such as Facebook, Twitter, Drupal, and Joomla! can facilitate research efforts to build community relationships and to create a community dialogue. However, the community dialogue and research involvement are not usually happening in the same sphere. Thus, such potential provided by the informatics tools rarely, if ever, supports colearning, leveraging findings and knowledge for mutual benefit. One interesting direction in social network analysis is the development of algorithms that aim to predict which connections in a network would benefit both the individual nodes and the network as a whole.
Developing an informatics interface between community engagement, health education and health promotion in rural populations has not traditionally been included in the ten factors that affect meaning. Our approach tries to overcome this by providing a cyber-infrastructure also based upon the National Cancer Institute’s cancer Biomedical Informatics Grid (caBIG®) backbone, as it is implemented at the Winthrop P. Rockefeller Cancer Institute. Currently available semantic infrastructures, formal metadata and ontologies can converge to create a social semantic information source that merges content with meaning. Our approach and expected outcomes to this challenge include;
1) The SI approach, which is geared to disseminate information from research sphere to the communities and individual members in a context aware manner by which only semantically relevant information is shared.
2) To date, cohort trials addressing cancer issues in the Southern US are lacking. CI can lend to the building of prospective cohorts examining cancer survival for minorities in relation to genetic variation, socio-economic factors, and treatment patterns, taking into account the genetic admixture background of individuals.
3) The community members would seed and moderate discussions on individual and community health and well-being based on relatively accurate and reliable data.
4) Having the control of the data and who can access will improve the communities’ trust for the biomedical research, which will yield increase in participation.
Other outcomes include: making data available, providing sufficient descriptive information about the data, enforcing compliance to standard semantics and structure, and rendering the data in a usable format. For the research community, large databases afford an opportunity to study hypotheses that would otherwise be underpowered in smaller studies. For the community they can navigate through the data and ask questions of each other and their research collaborators. For example, developing a portal with community participation caused participants to feel a sense of ownership, and they were willing to invest their time to improve the portal [11]. It is also important to involve the community in determining what research questions will be addressed and allowing new questions to be developed as new experiences with an intervention accumulates [56]. In addition, allowing community members to develop research questions for their community could serve as new way of crowd sourcing scientific advancements. Thus, the size of the scientific and Arkansas communities affected by our approach is substantial and the impact on those communities could be equally large.
Accessible use of this data will define concepts for intervention and processes by helping to raise awareness of health risks and solutions, providing the motivation and skills needed to reduce these risks, helping find support from other people in similar situations, and affecting or reinforcing attitudes. Intermediate outcomes can lend to individual health choices or improved access to information and services. Eventually, these individual outcomes facilitate community outcomes, which in turn feeds back to affect individual outcomes. This feedback or dialogue between individual health and community health is perceived as a mechanism to foster log-term health sustainability for communities. Use of social networking tools that community members feel comfortable with increases the likelihood of success. Providing appropriate web-based tools for community members/groups to define and track their own health has the potential to lead to increased dissemination of health information and advocacy related to health disparities in the context of individual and community meaning. This approach will facilitate participation in clinical trials, research studies, and bio banking recruitment, because it integrates into the routine life of community members, has relevant content for local needs, is linked to government, schools, and social services.
Acknowledgement
This research was supported in part by a generous grant from the National Center for Advancing Translational Sciences, UL1TR000039, to TKE, UT, and WH. This research was also supported by the Arkansas Institutional Development Award (IDeA) Network of Biomedical Research Excellence (Arkansas INBRE) program funded by the NIGMS to BB.
9363
References
- Bryant K, Haynes T, Kim Yeary KH, Greer-Williams N, Hartwig M (2014) A rural African American faith community's solutions to depression disparities. Public health nursing 31:262-271.
- Hines R, Markossian T, Johnson A, Dong F, Bayakly R (2014) Geographic residency status and census tract socioeconomic status as determinants of colorectal cancer outcomes. Am J Public Health 104: e63-71.
- Griffith DM, Johnson J, Ellis KR, Schulz AJ (2010) Cultural context and a critical approach to eliminating health disparities. Ethn Dis 20: 71-76.
- Murimi MW, Harpel T (2010) Practicing preventive health: the underlying culture among low-income rural populations. J Rural Health 26: 273-282.
- Lu MC, Kotelchuck M, Hogan VK, Johnson K, Reyes C (2010) Innovative strategies to reduce disparities in the quality of prenatal care in underresourced settings. Med Care Res Rev 67: 198S-230S.
- Cook C (2011) Grassroots clinical research using crowdsourcing. J Man ManipTher 19: 125-126.
- Armstrong AW, Harskamp CT, Cheeney S, Wu J, Schupp CW (2012) Power of crowdsourcing: novel methods of data collection in psoriasis and psoriatic arthritis. J Am AcadDermatol 67: 1273-1281.
- McCoy AB, Wright A, Laxmisan A, Ottosen MJ, McCoy JA, et al. (2012) Development and evaluation of a crowdsourcing methodology for knowledge base construction: identifying relationships between clinical problems and medications. J Am Med Inform Assoc 19:713-718.
- Murphy SN, Weber G, Mendis M, Gainer V, Chueh HC, et al. (2010) Serving the enterprise and beyond with informatics for integrating biology and the bedside (i2b2). J Am Med Inform Assoc 17: 124-130.
- Goodall K, Ward P, Newman L (2010) Use of information and communication technology to provide health information: what do older migrants know, and what do they need to know? Qual Prim Care 18: 27-32.
- Cresci MK, Yarandi HN, Morrell RW (2010) The Digital Divide and urban older adults. Comput Inform Nurs 28: 88-94.
- Bowling A, Browne PD (1991) Social networks, health, and emotional well-being among the oldest old in London. J Gerontol 46: S20-32.
- Gibbons MC, Fleisher L, Slamon RE, Bass S, Kandadai V, et al. (2011) Exploring the potential of Web 2.0 to address health disparities. J Health Commun 16: 77-89.
- Harvey JB, Beich J, Alexander JA, Scanlon D (2012) Building the scaffold to improve health care quality in Western New York. Health Aff (Millwood) 31: 636-641.
- Fone DL, Dunstan F, White J, Kelly M, Farewell D, et al. (2013) Cohort profile: the Caerphilly health and social needs electronic cohort study (E-CATALyST). Int J Epidemiol 42: 1620-1628.
- Marriott LK, Nelson DA, Allen S, Calhoun K, Eldredge CE, et al. (2012) Using health information technology to engage communities in health, education, and research. SciTransl Med 4: 119mr1.
- Paton C, Hansen M, Fernandez-Luque L, Lau AY (2012) Self-Tracking, Social Media and Personal Health Records for Patient Empowered Self-Care. Contribution of the IMIA Social Media Working Group. Yearb Med Inform 7:16-24.
- Rigby M (2012) Personal Health, Person-centred Health and Personalised Medicine - Concepts, Consumers, Confusion and Challenges in the Informatics World. Yearb Med Inform 7:7-15.
- Lopez L, Grant RW (2012) Closing the gap: eliminating health care disparities among Latinos with diabetes using health information technology tools and patient navigators. J DiabetesSciTechnol 6:169-176.
- López L, Green AR, Tan-McGrory A, King R, Betancourt JR (2011) Bridging the digital divide in health care: the role of health information technology in addressing racial and ethnic disparities. JtComm J Qual Patient Saf 37: 437-445.
- Norman CD, Yip AL (2012) eHealth promotion and social innovation with youth: using social and visual media to engage diverse communities. Stud Health Technol Inform 172:54-70.
- Ishii K, Ogasahara M (2007) Links between real and virtual networks: a comparative study of online communities in Japan and Korea. CyberpsycholBehav 10: 252-257.
- Hennessey Lavery S, Smith ML, Esparza AA, Hrushow A, Moore M, etal. (2005) The community action model: a community-driven model designed to address disparities in health. Am J Public Health. 95:611-616.
- van Gemert-Pijnen JE, Wynchank S, Covvey HD, Ossebaard HC (2012) Improving the credibility of electronic health technologies. Bull World Health Organ 90: 323-323A.
- Norman CD, Skinner HA (2006) eHealth Literacy: Essential Skills for Consumer Health in a Networked World. J Med Internet Res 8: e9.
- Goodman J, Wennerstrom A, Springgate BF (2011) Participatory and social media to engage youth: from the Obama campaign to public health practice. Ethn Dis 21: S1-94-9.
- Williams K, Durrance JC (2008) Social Networks and Social Capital: Rethinking Theory in Community Informatics.
- Bennett GG, Glasgow RE (2009) The delivery of public health interventions via the Internet: actualizing their potential. Annu Rev Public Health 30: 273-292.
- Gold J, Pedrana AE, Stoove MA, Chang S, Howard S, et al. (2012) Developing health promotion interventions on social networking sites: recommendations from The FaceSpace Project. J Med Internet Res 14: e30.
- Connor M, Fletcher I, Salmon P (2009) The analysis of verbal interaction sequences in dyadic clinical communication: a review of methods. Patient EducCouns. 75: 169-177.
- Shuai X, Pepe A, Bollen J (2012) How the scientific community reacts to newly submitted preprints: article downloads, Twitter mentions, and citations. PLoS One 7: e47523.
- Cobb NK, Graham AL, Byron MJ, Niaura RS, Abrams DB; Workshop Participants (2011) Online social networks and smoking cessation: a scientific research agenda. J Med Internet Res 13: e119.
- Yip YL (2012) Unlocking the potential of electronic health records for translational research. Findings from the section on bioinformatics and translational informatics. Yearb Med Inform 7: 135-138.
- Glasgow RE, Klesges LM, Dzewaltowski DA, Estabrooks PA, Vogt TM (2006) Evaluating the impact of health promotion programs: using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Educ Res 21: 688-694.
- Masi CM, Suarez-Balcazar Y, Cassey MZ, Kinney L, Piotrowski ZH (2003) Internet access and empowerment: a community-based health initiative. J Gen Intern Med 18: 525-530.
- Boyd DM, Ellison NB (2007) Social network sites: Definition, history, and scholarship. Journal of Computer-Mediated Communication.14: 1.
- Andrews JO, Felton G, Wewers ME, Heath J (2004) Use of community health workers in research with ethnic minority women. J NursScholarsh 36: 358-365.
- Brownstein JN, Bone LR, Dennison CR, Hill MN, Kim MT, et al. (2005) Community health workers as interventionists in the prevention and control of heart disease and stroke. Am J Prev Med 29: 128-133.
- Krieger JW, Takaro TK, Song L, Weaver M (2005) The Seattle-King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health 95: 652-659.
- Lewin SA, Dick J, Pond P, Zwarenstein M, Aja G, et al. (2005) Lay health workers in primary and community health care. Cochrane Database SystRev : CD004015.
- Montague E, Perchonok J (2012) Health and wellness technology use by historically underserved health consumers: systematic review. J Med Internet Res 14: e78.
- Zanaboni P, Lettieri E (2011) Institutionalizing telemedicine applications: the challenge of legitimizing decision-making. J Med Internet Res 13: e72.
- Viswanath K, Kreuter MW (2007) Health disparities, communication inequalities, and eHealth. Am J Prev Med 32: S131-133.
- Cashen MS, Dykes P, Gerber B (2004) eHealth technology and Internet resources: barriers for vulnerable populations. J CardiovascNurs 19: 209-214.
- Wangberg SC, Andreassen HK, Prokosch HU, Santana SM, Sørensen T, et al. (2008) Relations between Internet use, socio-economic status (SES), social support and subjective health. Health PromotInt 23: 70-77.
- Garfield MJ, Watson RT (2003) Four case studies in state-supported telemedicine initiatives. Telemed J E Health 9: 197-205.
- Viswanath K (2011) Cyberinfrastructure: an extraordinary opportunity to bridge health and communication inequalities? Am J Prev Med 40: S245-248.
- Neter E, Brainin E (2012) eHealth literacy: extending the digital divide to the realm of health information. J Med Internet Res 14: e19.
- Atkinson NL, Saperstein SL, Desmond SM, Gold RS, Billing AS, et al. (2009) RuraleHealth nutrition education for limited-income families: an iterative and user-centered design approach. J Med Internet Res 11: e21.
- Lustria ML, Smith SA, Hinnant CC (2011) Exploring digital divides: an examination of eHealth technology use in health information seeking, communication and personal health information management in the USA. Health Informatics J 17: 224-243.
- McLaren L, Ghali LM, Lorenzetti D, Rock M (2007) Out of context? Translating evidence from the North Karelia project over place and time. Health Educ Res 22: 414-424.
- Hobbs G (2000) What is Social Capital? A brief literature overview. Economic and Social Reserach Foundation.
- Jha AK, Gurung D (2011) Reaching the unreached: a model for sustainable community development through information and communication technology. JNMA J Nepal Med Assoc 51: 213-214.
- Eysenbach G, Jadad AR (2001) Evidence-based patient choice and consumer health informatics in the Internet age. J Med Internet Res 3: E19.