The test of six minutes is the most common test for evaluating the capacity of exercise tolerance in patients with pulmonary hypertension (PAH). It has the advantage to be a simple exercise to perform, without the need for sophisticated equipment and the lack of invasiveness, and can be repeated to monitor the clinical evolution. It also allows an assessment of the response to the different treatments.
Serves as predictive for the survival of these patients. Existing direct correlation with the cardiovascular functional status and inverse correlation with the pulmonary resistance, but not with mean pulmonary arterial pressure. Also correlates positively with the peak of maximum O2 consumption (VO2 max) during exercise [1]. Also, the decrease in arterial O2 saturation of more than 10% during the six minutes of the test involves an increased risk of mortality of 2.9 (2-4). It has been shown that distances of less than 325 meters (m) (5), TA systolic <120mmHg during the test (6), VO2 <10.4 ml / kg / min or NYHA functional class III and IV in the initial assessment of the PHA, imply data of bad prognosis (2), although most of these studies are performed in patients with PAH of idiopathic etiology, familiar or associated with connective tissue diseases.
Therefore, we propose to undertake a study to assess the functional status of patients with PAH from any source, using the six-minute walk test, as well as the variation of the same and the influence of possible treatments after a period of 4-6 months.
Material and Methods
This is a prospective longitudinal descriptive study. The start of the follow-up period begins from June 1, 2006, when it began to conduct clinical surveys for patients who accepted telephonically the inclusion in the study. Previously these patients were diagnosed of severe PHA according to the existing guidelines nowadays [2,7,8].
In these interviews, up to date clinical data was collected from the patient, the current treatment and a six-minute walk test was performed for an initial functional assessment.
After a period of not less than 4 months (except death or abandonment of the study), there was a new interview, in which it was re-assess the same parameters, new test of 6 minutes was performed, and it was accounted incomes and changes of treatment if there had been.
The follow-up ended when the patient completed the study, died, or when he refused to continue either by telephone or because of absence.
The walking test was made in a corridor of 76 m in length with subdivisions every 6 m, and all of them made by the same investigator.
For its implementation ATS recommendations were followed [9]. Prior to the start of the test there were 10 minutes of rest, in which the heart rate (HR), blood pressure (BP) and arterial oxygen saturation were measured. Later, they started walking up to the maximum of possibilities for 6 minutes monitoring heart rate and oxygen saturation and at the end of the test, after one minute of recovery, the same data were measured. In addition to that, it was picked up if the patient finished or not the test and the reason, and it was calculated the maximum O2 consumption (VO2 max):
0.1 ml / kg / min x distance (m) / +3.5 ml / kg / min Time (min).
The data were analyzed using the statistical program SPSS 11.5. Initially it was performed a descriptive statistics of the data, obtaining the following parameters for each variable: measures of central tendency (arithmetic mean), measures of dispersion (standard deviation, range and variance), minimum and maximum values.
All values of p are bilateral, and the statistical significance used was p <0.05.
Categorical data was analyzed using the chi-square test or Fisher’s exact test, as it was more appropriate.
If the variables satisfy the conditions of normality (Kolmogorov-Smirnov test and Shapiro-Wilks test) and homocedasticity (equal variances using Levene test), it was used the t-student test for the comparison of means, and if this was not the case, the Mann-Whitney U was used.
In the case of determinations of the same quantitative variables at two different times, it was used the Wilcoxon test for related data, or t-student for paired data, according to whether they meet or not conditions of normality and homocedasticity.
Among the quantitative variables it was used the Pearson correlation analysis when the data followed a normal distribution and Spearman when they were not.
Results
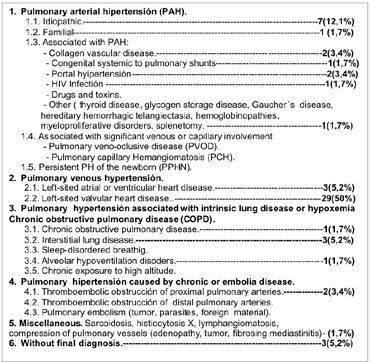
Data were collected from 58 patients, 32 females and 26 males, mean age 63.88 + 11.88 years. Of them, 75.9% of patients had more than 60 years. The etiology of PAH is shown in Table 1.
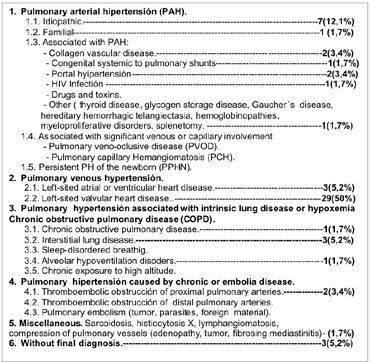
Table 1:
The average time elapsed between the first and second visit was 5.1 + 4.4 months (range from 1 month to 21 months). The end of follow-up occurred in 71.4% (n = 40) for completion of the study with the second interview, 19.6% (n = 11) because of patient refusal to continue and 10.3% ( n = 6) because of death. Of these, 50% (n = 3) died of respiratory failure, 16.6% (n = 1) for heart failure and 33.3% (n = 2) for other reasons: massive bleeding and liver failure.
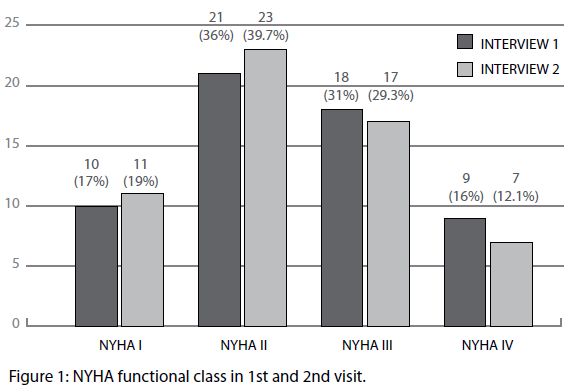
Functional class for dyspnea in both interviews, expressed according to the New York Heart Association (NYHA) is shown in Figure 1. On the second visit, in case of death of the patient, was taken as the functional class the one they had in the days before it. Also in cases of abandonment of the study by the patient, it was taken that functional class present at the time.
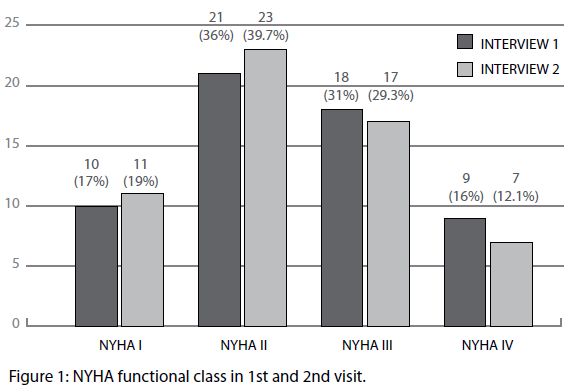
Figure 1: NYHA functional class in 1st and 2nd visit.
The 24.1% of patients (n = 14) improved the functional class from the first to the second visit, being lower the number of patients in NYHA functional class III or IV at the second visit (p=0.003). The presence of functional class III or IV was not significantly associated with a higher frequency of death in the first or second visit (p=0.087 and p=0.072 respectively).
Most patients in our series had a prior entry related to pulmonary hypertension (dyspnea, chest pain of no coronary characteristics ...) with a median of 3.3 + 3.9 entries per patient. Also during the relatively short follow-up between the first visit and the end of the study, 45 entries in 58 patients occurred (0.7 + 0.8 revenue per patient).
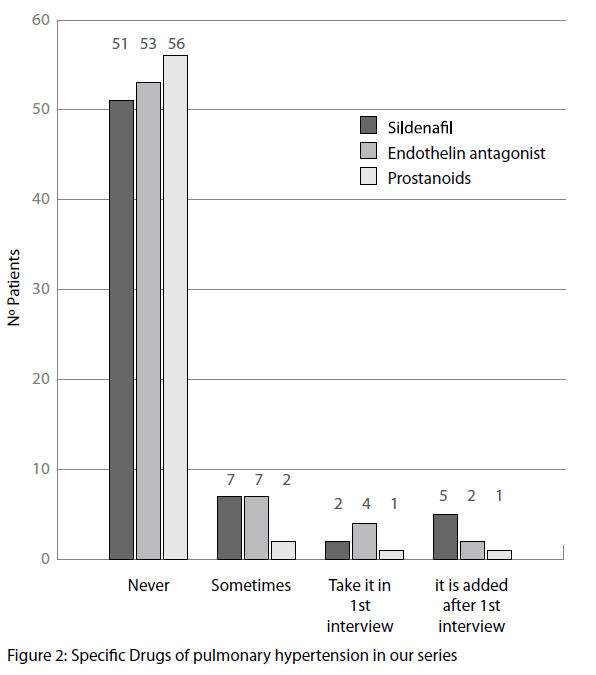
Only 12.06% (n = 7 patients) of the study population had one of the specific treatment of PAH in the first visit. Of which, antagonists of endothelin receptors 6.9% (4), were the most frequent, followed by sildenafil 3.4% (2) and prostacyclins 1.7% (1). Only 1 patient carried a combination of treatments (1.7%) with sildenafil and prostacyclins. During the study, 8 specific PAH treatments were added (5 sildenafil, 2 antagonists of receptors of endothelin and 1 prostacyclin).
At the end of the study at the second visit, 13.8% (n = 8 patients) had a specific treatment of PAH. Of these 7 patients (12.1%) with sildenafil, 3 patients (5.2%) with antagonists of receptors of endothelin (in 3 other occasions this treatment was removed, on two occasions they had it in the first visit and it is modified and on another occasion was removed because of intolerance by the patient) and 2 patients with prostacyclins (3.4%). 4 patients took combined treatment (6.9%), 2 took sildenafil and antagonist of the receptors of endothelin, and 2 prostacyclin and sildenafil) Figure 2.
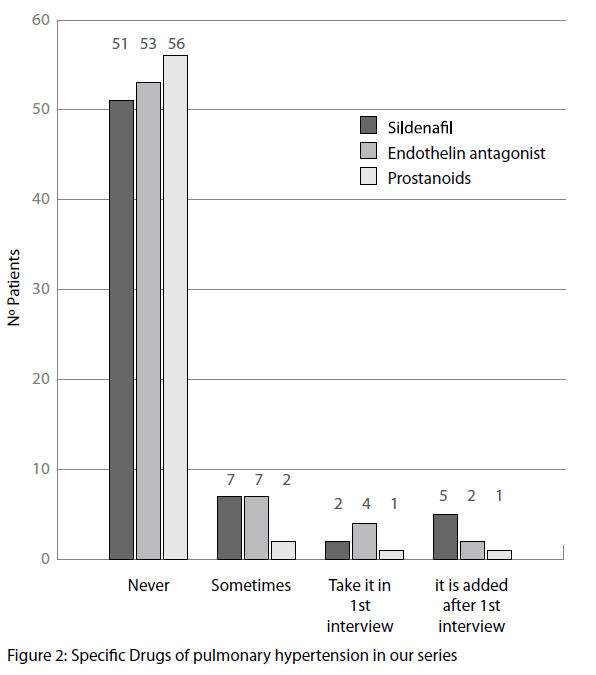
Figure 2: Specific Drugs of pulmonary hypertension in our series
Regarding the need for oxygen treatment, 24.1% (14) had taken it in some occasion, 10.3% (6) had it in the first interview and in 3 cases (5.2%) the treatment was added during the study. The 6 minutes tests were carried out without this contribution.
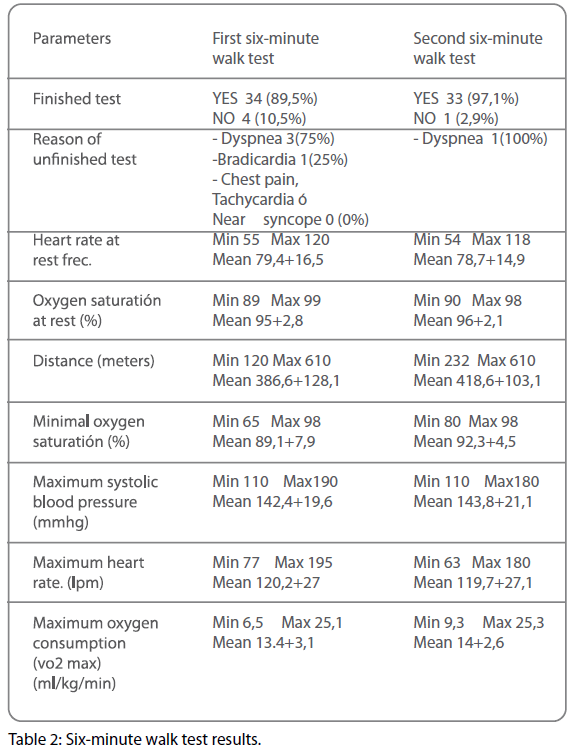
The first walking test could be made in 65.5% of patients (n = 38), whereas it was not possible in 34.5% (n = 20), because of poor NYHA functional class in 55% (11) and because of denying access to its implementation in 45% (9).
The second test was carried out on 58.6% of patients (n = 34), and it was not possible in 41.4% (n = 24), because of poor NYHA functional class in 33.3% (8), because of denying access to its implementation in 45.83% (11) and because of death in 20.8% (5). The results obtained in both tests are shown in Table 2.
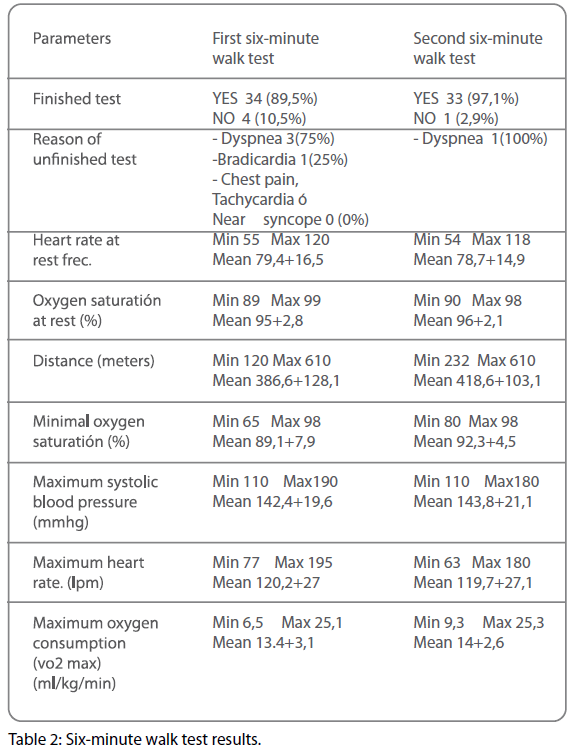
Table 2: Six-minute walk test results.
Both six-minute walk test were done by a total of 29 patients (50%) of which 14 patients increased the meters walked from the first to the second (48.2%) 2 did the same meters (3.4% ) and 13 decreased the distance (22.4%).
There were 8 patients (13.8%) who did the first test and not the second (4 for poor functional class, and 2 because they refused to do so, the 2 remaining died).
In 3 cases (5.2%), the second test was performed without being able to do the first, being the three times for poor functional class that improved from the first to second visit.
The distance walked was greater in men in both the first and the second test (p=0.049 and p=0.006).
It was observed statistically significant correlation between the meters walked and the height 0.351 (p=0.031) but not with age or body mass index.
No etiology was found that walked less than 325 meters with more frequence than the rest.
We compared the measurements of the parameters in the first and second test founding that the minimal saturation O2 was higher in the second test of 6 minutes in a meaningful way with respect to the first (p=0.021).
Taking into account the parameters of the six-minute walk test, as is described in the literature, are associated with poor prognosis (decrease of O2 saturation in more than 10% during the test; distance walked less than 325 m; Consumption O2 <10.4 ml / kg / min and TA systolic <120 mmHg during the test) we analyzed by Chi-square test or Fisher’s exact test depending on the data. Among the deceased patients it was observed a higher frequency of desaturations > 10% in the first test of 6 minutes (p=0.032) but not in the second walking test (p=1).
Regarding the relationship of the NYHA functional class with the parameters measured in the walking test, we find that the improvement of functional class from first to second visit was significantly associated with a greater distance walked in the second test (p=0.002). Also, patients in advanced functional class (III or IV) walked a distance significantly smaller in both the first and the second walking test (p=0.006 and p=0.028). The saturation of the minimum O2 was significantly lower in patients with NYHA III or IV in the first test (p=0.001).
With regard to treatments in relation to the distance walked in the sixminute walk test, we observed that patients treated with O2 at home in some occasion, walk more often distances of less than 325M in the first test (p=0.014). This data was not significant in the second test because of the 5 patients who walked <325 m in 2nd walking test had only taken O2 some time (p=0.228).
Also in patients who were treated with sildenafil after the first visit it was observed an improvement in meters walked from the first to the second walking test (p=0.023). Was not significant the start of other treatments.
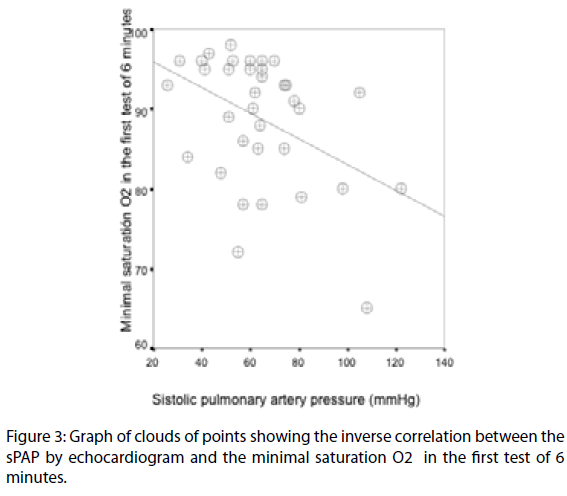
Correlation study was performed between the systolic pressure of pulmonary artery (PASP) measured by echocardiogram and hemodynamic study (Table 3) and data obtained in tests of 6 minutes (Total meters traveled, maximum heart rate, minimal saturation O2 and maximum O2 consumption). There was a negative correlation between the systolic pressure of pulmonary artery (PASP) measured by echocardiogram and minimal saturation O2 during the first test of 6 minutes (-0.368 (p=0.029) (Figure 3).

Table 3: Clinical and Hemodynamic data at clinical trials of Pulmonary Hipertensions.
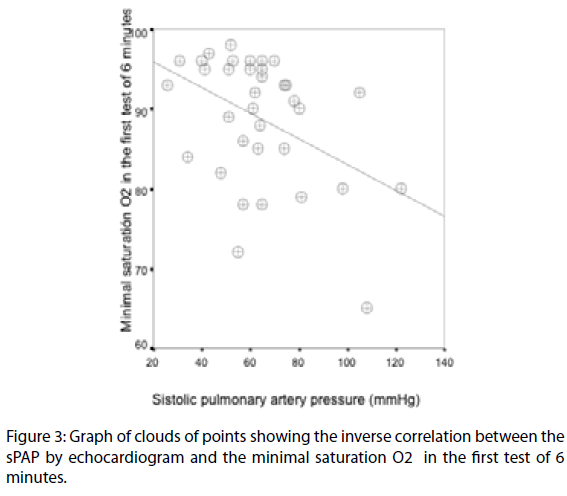
Figure 3: Graph of clouds of points showing the inverse correlation between the sPAP by echocardiogram and the minimal saturation O2 in the first test of 6 minutes.
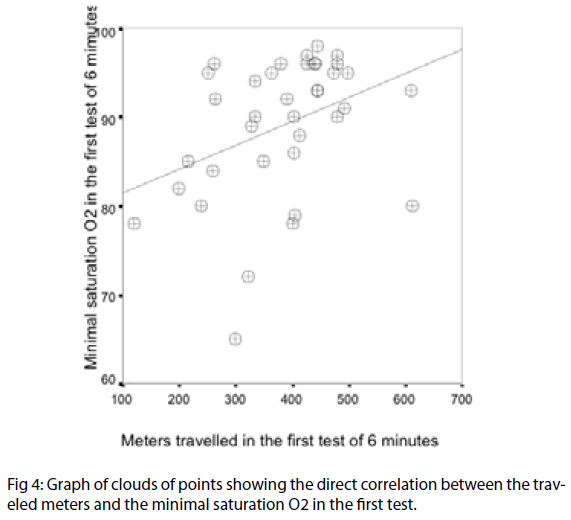
It was also found a positive correlation between total meters walked in the first test of 6 minutes and minimal saturation O2 obtained during this test: 0.439 (p=0.006) (Figure 4).
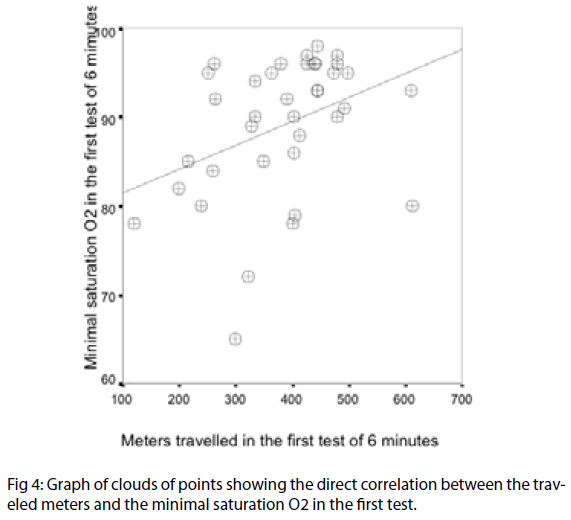
Figure 4: Graph of clouds of points showing the direct correlation between the traveled meters and the minimal saturation O2 in the first test.
Discussion
A review of the literature shows that the normal walking speed is 83 m / min [10]. It has also been proposed regression equations to predict the six meters walked in healthy adults [11].
According to this study in 173 healthy men and 117 women between 40 and 80 years of age, the average distance traveled was 576m for men and 494m for women, with a variance of 42% and 38% in the 6 minutes test respectively.
It should be considered factors that generate variability of the test: 1) reduce the distance traveled: Old age, female sex, obesity, low height, lung disease, cardiovascular and musculoskeletal, cognitive impairment, short hallway. 2) Increase the distance traveled: being tall, male sex, high motivation, prior experience in the test, long corridor and supplementation of oxygen in patients with exercise-induced hypoxemia [11].
In our study, the average distance walked was 386.6 + 128.1 in the first test and 418.6 + 103.1 in the second test of walking. Both values below those considered normal, but higher than that expressed in other studies [12-14] Table 3. This may be due to the higher percentage of patients in advanced functional class (III and IV) within those studies, as these classes demonstrate a significantly lower number of meters traveled than with functional classes I and II in our study as in others as the French registry [12].
Although two large prospective series have confirmed the importance of the NYHA functional class as a prognostic variable [15,16], most of the published studies refer to it at the time of diagnosis of PAH, being often patients with idiopathic etiology or familiar and less frequent in other causes. The percentages of advanced functional class are high in those patients who have not yet begun treatment [12,13] (75% in class III or IV at diagnosis in the French Registry or 72.4% in an American series).
In our series all etiologies of PAH are collected and in some cases patients had already been treated for his illness, which modifies the average age and functional class.
Even so, the percentage of patients in advanced functional class III or IV on the first visit is high (47%). This may be related in part to the high number of patients with advanced valvular heart diseases joined to patients newly diagnosed untreated. Besides the high percentage, some patients had been admitted to periods close to the first visit and it is a voluntary testing which could explain in a way that 34.5% of patients did not conduct the first six-minute walk test.
The fact that a 24.1% improved in functional class from first to second visit may be due to initiation of specific treatments for PAH in some patients, or the solution or improvement of the cause of PAH, such as the valve replacement, which was performed 5 times during our follow-up or treatment of hyperthyroidism.
A study that describes that oxygen supplementation during exercise in patients with COPD or interstitial disease, increase a mean of 83 m (36%) on the distance walked in the 6 minutes test [17]. Also other international study conducted in COPD patients, says that taking the inhaler with corticoids prior to the walking test increases a mean of 33m (8%) that distance [18].
Our patients did the test without the addition of O2, or immediately after taking the inhaler, so we do not know if it had been able to influence the distance traveled. There was a statistically significant direct correlation between distance walked and the minimum oxygen saturation obtained during the test 0.439 (p=0.006), what confirms that with better oxygenation a longer distance is walked (Figure 4).
Several authors have demonstrated the high prognostic value of test of 6 minutes in the PAH, although different distances are proposed as a marker of poor prognosis. In one of the first controlled studies of PAH a distance <150 m was associated with very poor prognosis [19]. Miyamoto et al showed that patients who walked <332 m had a lower survival rate than those who walked greater distances [20]. Another study found a 18% reduction in risk of death for each 50 m walked in patients with idiopathic PAH [4] and Sitbon et al reported that patients in functional class III or IV NYHA walking <250 m before the start of treatment with epoprostenol or <380 m after 3 months treatment with epoprostenol have a worse prognosis than those who walk greater distances [21]. The fact of choosing 325 m as cutoff point for our study may be equally valid, as it is presented in the recent literature on patterns of activity in this disease [5] we decided to use it in our series.
Although some series show different distances according to the etiology of PAH [12,13], we do not have a large number of cases so as to assess this, and we did not find any etiology that was significantly associated with a traveled distance less than 325 m.
The studies that have evaluated the usefulness of the test of 6 minutes have shown varying results [22-26]. Although this test is easy to implement, most patients apparently do work less (sub-maximal effort) compared to cycle-ergometer.
In patients with COPD, some studies have found no significant differences in maximum minute ventilation and VO2 between effort tests in cycle-ergometer and walking 12 min [23]. Similar findings have also been described in patients with severe heart failure [24-26]. Based on these results some authors suggest that at least in patients with advanced cardiopulmonary, distance traveled during the walking test (usually seen as a capacity index of sub-maximal effort), probably reflects the capacity of maximum effort.
Regarding other parameters of poor prognosis, although there were no significant findings with respect to O2 consumption and blood pressure among the deceased patients in the study, it was observed a higher frequency of desaturations > 10% in the first 6 minutes test (p=0.032). Not the same thing happened in the second walking test (p=1) (probably because only 1 of the patients who died during the study did the second test).
In our series, higher levels of sPAP measured by echocardiogram correlates with lower results of minimal saturation O2. This is logical since the exchange of O2 is worse with higher PAP, from there the predictive value of the 6 minutes test. The failure to not find statistical significance with the sPAP measured by hemodynamic study may be due to fewer measurements made by this method.
Although in our study it was done 2 times the test of 6 minutes, this did not help at times to assess the response to specific treatments for PAH, because there was not a prior test to initiation of the treatment and patients already were taking medication in our first visit. Hence we could only assess the cases in which treatment was initiated after the first visit or when a 6 minutes test was done before the start of the new treatment.
Thus, it has been objectified in our sample that patients who began treatment with sildenafil improved the distance traveled after the first visit from the first to the second test of 6 minutes (p=0.023). Of the 5 treatments started 4 of them increased the number of meters traveled in an average of 131 m (minimum 35 m, maximum 280 m) and remaining patient died before being able to conduct the second test. This is consistent with studies supporting the use of sildenafil [27,28]. Distances described in these studies vary from 47 m to 154 m according to different etiologies, ages and doses employed. This is why the comparison is difficult, since in our case the etiology of our patients were varied (two idiopathic, one familiar, one associated with pulmonary fibrosis, and other associated to collagen diseases).
Different studies have shown improvement in the functional class after initiation of treatment [27-30]. We have not found that the initiation of any specific treatment of PAH was significantly associated with improvement of functional class. However there is a trend to improvement in the initiation of treatment with sildenafil (p=0.085). Perhaps these data are influenced by the low number of registered specific treatments, and studies and monitoring are necessary to show that broader trend.
394
References
- Lopez J, Montes de Oca M, Ortega Balza M, Lezama J. “Enfermedad pulmonar obstructiva crónica. Evaluación de la tolerancia al ejercicio utilizando tres tipos diferentes de pruebas de esfuerzo”. Arch Bronconeumol 2001; 37:69-74.
- Galiè N, Torbicki A, Barst R et al. Guías de Práctica Clínica sobre el diagnóstico y tratamiento de la hipertensión arterial pulmonar. Rev Esp Cardiol. 2005; 58:523-66.
- Guyatt GH, Sullivan MJ, Thompson PJ. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J 1985; 132: 919-23.
- Paciocco G, Martinez F, Bossone E, Pielsticker E, Gillespie B, Rubenfire M. Oxigen desaturation on the six-minute walk test and mortality in untreated primary pulmonary hypertension. Eur Respir J 2001; 17: 647-52.
- Escribano P, Gómez MA, Jiménez C y Ruiz MJ. Evidencia científica en Hipertensión pulmonar. Manual de actuación. ISBN: 84-689-6176-0. Dep. Legal: M-4460-2006.
- Wensel R, Opitz CF, Ander SD, Winkler J, Hoffken G, Kleber FX, Sharma R, Hummel M, Hetzer R, Ewert R. Assessment of survival in patients with primary pulmonary hipertensión: importance of cardiopulmonary exercise testing. Circulation. 2002; 106: 319-324.
- Galiè N, Torbicki A, Barst R et al. Guidelines on dignosis and treatment of pulmonary arterial hypertension. The Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology.Eur Heart J 2004;25:2243-78.
- McGoon M, Gutterman D, Steen V, Barst R, McCrory DC, Fortin TA, Loyd JE. Screening, Early Detection, and Diagnosis of Pulmonary Arterial Hypertension: ACCP Evidence-Based Clinical Practice Guidelines Chest, Jul 2004; 126: 14S - 34S.
- ATS Statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166: 111-117.
- Lerner-Frankiel MB, Vargas S, Brown MB et al. Functional community ambulation: what are your criteria?. Clin Manag Phys Ther 1986;6: 12-15.
- Enright P, Sherrill D. “ Reference equations for the six-minute walk in healthy adults”. Am J Respir Crit Care Med 1998;58: 1384-1387.
- Humbert M, Sitbon O, Chaocuat A et al. Pulmonary Arterial Hypertension in France. Results from a National Registry. Am J Respir Crit Care Med 2006; 173: 1023-1030.
- Zagolin B, Mónica, Wainstein G, Eduardo, Uriarte G De C, Polentzi et al. Caracterización clínica, funcional y hemodinámica de la población con hipertensión pulmonar arterial evaluada en el Instituto Nacional del Tórax. Rev. méd. Chile, mayo 2006, vol.134, no.5, p.589-595. ISSN 0034-9887.
- Thenappan T, Shah S J, Rich S and Gomberg-Maitland M. A USAbased registry for pulmonary arterial hypertension: 1982-2006. Eur Respir J 2007; 30:1103-1110.
- McLaughlin VV, Shillington A, Rich S. Survival in primary pulmonary hypertension: the impact of epoprostenol therapy. Circulation. 2002;106:1477-82.
- McLaughlin VV, Presberg KW, Doyle RL, et al. Prognosis of Pulmonary Arterial Hypertension: ACCP Evidence-Based Clinical Practice Guidelines. Chest, Jul 2004; 126: 78S - 92S.
- Leach RM, Davidson AC, Chinn S, Twort CHC, Cameron IR, Batemen NT. Portable liquid oxygen and exercise ability in severe respiratory disability. Thorax 1992; 47: 781-789.
- Paggiaro PL, Dhale R, Bakran I, Frith L, Hollingwoth K, Efthimiou J. Multicentre randomised placebo-controlled trial of inhaled fluticasone in patients with COPD. Lancet 1998; 351: 773-780.
- Barst RJ, Rubin LJ, Long WA, McGoon MD, Rich S, Badesch DB. A comparison of continuous epoprostenol (prostacyclin) with conventional therapy for pulmonary hypertension. The Primary Pulmonary Hypertension Study Group. N Engl J Med 1996;334: 296-302.
- Miyamoto S, Nagaya N, Satoh T, et al. Clinical correlates and pronostic significance of six-minute walk test in patiens with primary pulmonary hypertension. Comparision with cardiopulmonary exercise testing. Am J Respir Crit Care Med 2000; 161:487-92.
- Sitbon O, Humbert M, Nunes H, et al. Long-term intravenous epoprostenol infusion in primary pulmonary hypertension: prognostic factors and survival. J Am Coll Cardiol. 2002; 40: 780-8.
- Montemayor T, Ortega F, Sanchez H. Valoración de la capacidad de esfuerzo en la EPOC. Revisión crítica de las pruebas de marcha. Arch Bronconeumol 1999;35:34-39.
- Baarends EM, Schols AM, Mosert R, Janssen PP, Wouters EF. Analysis of themetabolic and ventilatory response to self-paced 12 minute treadmill walking in patients with severe chronic obstructive pulmonary disease. J Cardiopulm Rehabil 1998; 18:23-31.
- Cahalin LP, Mathier MA, Semigran MJ, Dec W, DiSalvo TG. The sixminute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest 1996; 110:325-332.
- Faggiano P. Assessment of oxygen uptake during the six minute walk test in patients with Herat faliure. Chest 1997;111:1146.
- Cahalin LP. Assessment of oxygen uptake during the six minute walk test. Chest 1997; 111:1465-1466.
- Galie N, Ghofrani HA, Torbicki A, et al. Sildenafil Use in Pulmonary Arterial Hypertension (SUPER) Study Group: sildenafil citrate therapy for pulmonary arterial hypertension. N Engl J Med 2005;353(20):2148-57.
- Michelakis ED, Tymchak W, Noga M, et al.. Long-term treatment with oral sildenafil is safe and improves functional capacity and hemodynamics in patients with pulmonary arterial hypertension. Circulation. 2003;108: 2066-9.
- Rubin LJ, Badesch DB, Barst RJ, Galie N, Black C, Keogh A, et al. For the Bosentan Randomized Trial of Endothelin Antagonist Therapy Study Group. Bosentan therapy for pulmonary arterial hypertension. N Engl J Med. 2002;346:896-903.
- Galie N, Beghetti M, Gatzolius M, et al. BREATHE-5: Bosentan improves hemodynamics and exercise capacity in the first randomized placebo-controlled trial in eisemenger phsiology. Chest 2005; 129: 496S.