Jamry Andrzej1*, Gzik Marek2, Jałyński Marek3, Wolanski Wojciech2 and Brocki Marian4
1II Surgical Department District Hospital Starachowice, Poland
2Department of Biomechatronics, Biomedical Engineering Faculty, Silesian University of Technology, Zabrze, Poland
3Chair of Surgery and X-ray Diagnostics, University of Warmia and Mazury, Olsztyn, Poland
4Department of Chest and General Surgery, Medical University of Lodz, Poland
Corresponding Author:
Jamry Andrzej
Langiewicza 30, 27-200 Starachowice, Poland
Tel: +48 602 795 259
Fax: +48412739135
Received date: April 01, 2016; Accepted date: May 16, 2016; Published date: May 23, 2016
Citation: Andrzej J, Marek G, Marek J, et al. Slow-absorbing Sutures for Mesh Fixation in Laparoscopic Ventral Hernia Repair. Arch Med. 2016, 8:3.
Keywords
Laparoscopic surgery; Ventral hernia; Postoperative pain; Suture techniques; Surgical meshes
Introduction
Despite the tension-free nature of laparoscopic ventral hernia repair (LVHR), it is one of the few laparoscopic procedures with a pain level comparable to that of open ventral hernia repair [1-3]. Chronic pain after this type of operation is observed in 1 to 27% of patients. Potential source of it can by the formation of tension between gradually shrinking mesh and non-absorbable points of its attachment [1,4-7]. Additionally this condition may lead to cutting the fascia at the suture anchoring sites, with a risk of secondary granulomas, hematomas and infections. Therefore, the use of slow-absorbing fixation devices, which degrade simultaneously with the process of shrinkage the mesh, can perhaps reduce chronic postoperative pain with preserved proper fixation. The use of sutures in comparison with other devices provides more durable fixing and allows to avoid tension in the attachment points immediately after surgery (if the sutures are tied after desuflation of the peritoneal cavity). Therefore, we decide to analyze usefulness of slow - absorbable sutures for LVHR. In the available literature, we did not find any biomechanics research about the utility of slow-absorbing sutures for DynaMesh laparoscopic Intraperitoneal onlay Mesh (IPOM) stabilization. Slowly degradable sutures are suitable for classic abdominal cavity closure [8-10]. However, after mesh implantation in LVHR, the biomechanical environment is different; thus, the results from other procedures cannot be easily extrapolated to LVHR [11,12]. Consequently, we decided to evaluate this problem for two kind of slow-absorbable sutures (Maxon and PDS II) which differing slightly in speed of degradation depending on the environment [8,13].
Materials and Methods
The study was conducted in an animal model using 12 Polish Large White breed pigs (PLW) aged 12 weeks (weigh 30 to 40 kg). The examination was performed in the Veterinary Surgery Ward of the University of Warmia and Mazury (Approval No. 02/2009; Ethical Committee of the University of Warmia and Mazury). A two-layer DynaMesh IPOM mesh was used: the parietal wall is made of polypropylene, and visceral wall is made of polyvinylidene fluoride (PVDF) (DynaMesh IPOM FEG Textiltechnik mbH, Aachen, Germany). Two types of slow-absorbing 1-0 sutures, PDS II (Ethicon Endo-Surgery, Cincinnati, Ohio, USA) and Maxon (Covidien, Dublin, Ireland), were used to fix the meshes.
Operative technique
Two surgeons performed all the procedures. The animals were subject to general anesthesia, and a pneumoperitoneum was generated with a Veress needle (pressure of 12 mmHg). Optical (11 mm) and working (5 mm) trocars were introduced in the midline. Through the 11 mm port, mesh fragments with attached sutures were introduced into the peritoneal cavity. Each animal was implanted with two mesh fragments (6.0 cm × 6 cm) that were fixed with four PDS II or Maxon stiches spaced up to 4 cm apart. Then, sutures were passed through the abdominal wall and tied after desufflation. Thirty minutes before the procedure, a preventative dose of penicillin procaine (1.2 million units; penicillin procaine L TZF, Polfa Trachomin, Poland) was administered intramuscularly, and two additional doses were administered at 8-hour intervals. A painkiller (metamizolum natricum, Pyralgin Polpharma SA, Warsaw, Poland) was administered at 8-hour intervals over the following three days. The animals were then offered water ad libitum. The animals were also provided light and scheduled feedings.
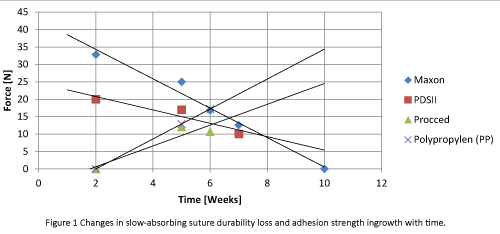
Time of strength testing
To determine whether slow-absorbing sutures are suitable for the stabilization of mesh, we used available data to determine the time after implantation at which mesh stability provided by the sutures and mesh adhesions was the smallest. If meshstabilizing forces are sufficient during this period, it will suggest that slow-absorbing sutures are suitable for the IPOM technique. The available database does not contain detailed information about DynaMesh IPOM. However, data regarding the increased time with adhesion forces for tree other meshes (Proceed, PP, Parietex) and the decreasing tensile strength of two (Maxon, PDS II) slow-absorbing stitches were identified (Figure 1) [4,5,7,14-19]. These results led to the conclusion that the period between 4 and 6 weeks after implantation is crucial (area where the trend line is crossed). Based on these data, a strength test was performed 6 weeks post operation. The strength of the adhesion between the mesh and the abdominal wall was examined using a System MTS insight 10 kN static strength-testing machine (MTS Systems, Créteil, France). The adhesion resistance was analyzed by measuring the maximum force required to detach the mesh from the abdominal wall and was expressed as N. Next, the average force and mean detachment force per cm of mesh width and per sq.cm of mesh-abdominal wall as well as the adhesion were calculated. This type of calculation was performed for all pieces of mesh combined and separately fixed with Maxon and PDS II sutures.
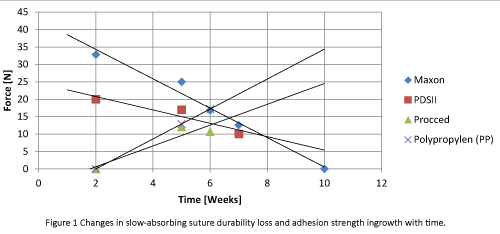
Figure 1: Changes in slow-absorbing suture durability loss and adhesion strength ingrowth with time.
Calculation of total mesh stabilization force at the sixth postoperative week
The abdominal wall defects that could be repaired with the LVHR technique had a diameter between 2.5 and 10 cm, and the mesh overlap should have a width similar to the diameter of the gap. Based on this principle and on the basis of the obtained results, we calculated the total stabilization force (surface of overlap (sq. cm) × [detachment force N/sq.cm]) and compared this value with the maximal push force generated through intraabdominal pressure=defect surface (sq.cm) × [maximal push force (2.0) N/sq.cm] (mathematical model developed in other studies) [15,16,18-20]. The differences between these two values allowed us to estimate whether the DynaMesh IPOM had proper stability 6 weeks post implantation. This analysis was performed for all mesh fragments and separately performed for those affixed with Maxon and PDS II sutures.
Statistical analysis
Statistical analyses were performed using the Grubbs and Tukey tests for excluding deviated data, the Shapiro-Wilk (0.05) and Levine (0.05) tests for evaluating normal data distribution, and Student’s t test (0.05) for comparing detachment forces between meshes fixed with Maxon and PDS II stitches.
Results
Distribution of force required to detach the mesh fragments
When analyzing the force required to detach the mesh fixed with slow-absorbing sutures, we observed two peaks at the beginning and end of the examination that corresponded to the suture anchoring sites (4 cm distance). A relatively flat lower value that corresponded to the strength of the adhesion formed between the mesh and the peritoneum was also noted. This finding suggests that the sutures' supportive capabilities were preserved 6 weeks after surgery, and the force required to break the sutures was much higher than the force required to break the adhesion between the mesh and the abdominal wall in the remaining part of the implant.
Maximum detachment forces
In two cases (PDS-1 and Maxon-6), the force exceeded 50 N due to fistulas along the suture canal that led to extensive scarring and subsequent strong adhesion. These two data points were excluded from statistical analysis based on the Grubbs and Tukey tests. The mean maximum detachment force for all the DynaMesh IPOM mesh fragments was 21.97 N (range (6.58-41.66) and standard deviation (sd2) 8.489).
Average forces
The average force necessary to detach all fragments of the DynaMesh IPOM mesh was calculated. The mean averaged detachment force for all the mesh fragments was 10.68 N (range, 3.47-18.84); sd2, 3.544). The mean average force for mesh implants fixed with Maxon sutures was 10.20 N (range, 3.47-14.98; sd2, 3.436). The mean average detachment force for mesh implants fixed with PDS II sutures was 11.16 N (range, 7.17-18.84; sd2, 3.75). Based on these data, the mean force required to detach the mesh per cm of the width was calculated and reported as N/cm. For implants fixed with Maxon sutures, the value of this parameter was 3.93 N/cm. For implants fixed with PDS II sutures, the value was 5.4 N/cm.
Force necessary to detach 1 sq.cm of the mesh
The mean value of the forces necessary to detach 1 sq.cm of the mesh surface stabilized with both types of sutures (at 4-cm intervals) was calculated. The mean force per surface unit (F mean/S) for all mesh fragments was 0.68 N/sq.cm (range, 0.21- 1.18; sd2, 0.243). The mean force per surface unit (F mean/S) for meshes fixed with Maxon sutures was 0.62 N/sq.cm (range, 0.21- 1.04; sd2, 0.2368). The mean force per surface unit (F mean/S) for meshes fixed with PDS II sutures was 0.73 N/sq.cm (range, 0.42-1.18; sd2, 0.247).
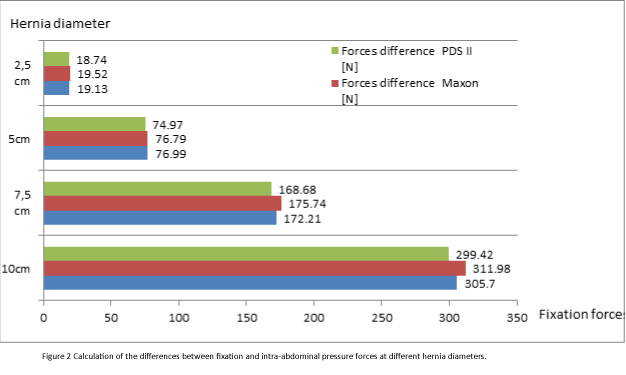
Differences between total fixation and push force
Based on current knowledge, LVHR should be indicated for hernias with a defect diameter between 2.5 and 10 cm. According to this date, we calculated differences between the total fixation force and the force generated through the maximal intraabdominal pressure. The obtained results for the extreme size of the hernia (2.5 and 10 cm) and overlap width suitable for the defect diameter were 157 and 251.2 N, respectively. This value exhibited an increased anchoring force in relation to the maximal forces generated through the intraabdominal pressure. A similar calculation was performed for meshes fixed with PDS II and Maxon sutures, and a similar conclusion was obtained (Figure 2). The above calculations suggest that slow-absorbing sutures (Maxon and PDS II) may be used satisfactorily in LVHR for fixing DynaMesh IPOM. The results of this experimental study suggest that research on the use of slow-absorbing stitches to fix the mesh in the LVHR technique in humans is justified.
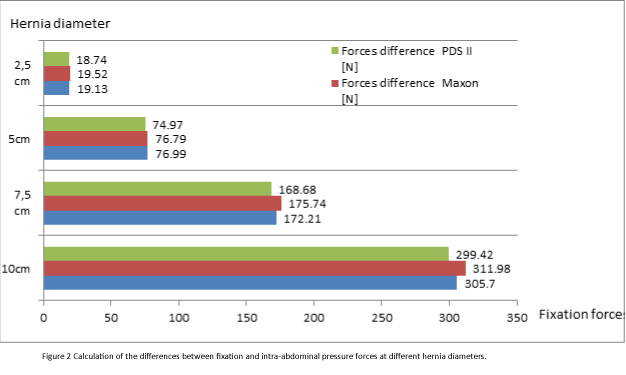
Figure 2: Calculation of the differences between fixation and intra-abdominal pressure forces at different hernia diameters.
Comparison of the detachment forces between meshes fixed with Maxon and PDS II stitches
The mean maximum detachment force for mesh implants affixed with Maxon sutures was 19.84 N (range, 6.58- 32.83; sd2, 7.862), and the mean maximum detachment force for mesh implants affixed with PDS II sutures was 24.09 N (range, 12.25-41.66; sd2, 8.919). The mean average force for mesh implants fixed with Maxon sutures was 10.20 N (range, 3.47-14.98; sd2, 3.436). The mean average detachment force for mesh implants fixed with PDS II sutures was 11.16 N (range, 7.17-18.84; sd2, 3.75). Based on these data, the mean force required to detach the mesh per cm of the width was calculated [N/cm]. For implants fixed with Maxon sutures, the value of this parameter was 3.93 N/cm. For implants fixed with PDS II sutures, the value was 5.4 N/cm. The mean force per surface unit (F mean/S) for meshes fixed with Maxon sutures was 0.62 N/sq.cm (range, 0.21-1.04; sd2, 0.2368). The mean force per surface unit (F mean/S) for meshes fixed with PDS II sutures was 0.73 N/sq.cm (range, 0.42 -1.18; sd2, 0.247).
The statistical analysis (Student’s t test) indicated that the differences were not statistically significant (Table 1). The results suggest that the differences are not statistically significant. However, the test power analysis indicated that the small number of cases are underpowered and require further study.
| |
Mean force-Maxon |
Mean force-PDS |
T |
Df |
P |
| Maximum force [N] |
19.84 |
24.09 |
-1.19 |
20 |
0.249 |
| Average force [N] |
10.20 |
11.16 |
-0.63 |
20 |
0.537 |
| Average force [N/sq.cm] |
0.62 |
0.73 |
-1.13 |
20 |
0.273 |
Table 1: Statistical analysis (Student’s t test) comparing detachment forces for meshes fixed with Maxon and PDS II sutures.
Discussion
One of potential sources of the pain in the late postoperative period post LVHR can by the formation of tension between gradually shrinking mesh and non-absorbable points of its attachment. Therefore use slow-absorbing sutures, which degrade simultaneously with the process of shrinkage the mesh can perhaps reduce chronic postoperative pain with preserved proper fixation. According to the data from available publications, the critical period for mesh stabilization with slow- absorbable sutures appears between 4 and 6 weeks after surgery [6,7,12]. Consequently, in the present study, we assessed fixing forces of the mesh 6 weeks after implantation [18-21]. When we attempted to compare obtained results with other studies, we must first state that we were unable to find any biomechanical analyses of DynaMesh IPOM fixed with PDSII and Maxon stiches in the literature. The results of studies using other meshes and fixation methods differ in the following aspects: time after implantation, separate analysis of the tensile strength of the sutures (in vitro or in vivo) or the detached forced generated through adhesions (after removal of the attachments devices), and meshes fixed together with sutures and protack devices. The method of the presentation of the results also differs (the maximum value of the detachment force or the detachment force per unit width of the mesh). Thus, a simple comparison of the obtained results with other studies is difficult or even impossible. Based on the obtained results, it is clear that slow-absorbing sutures played important roles in mesh stabilization after 6 weeks. At this time, the implant stabilization corresponds to the sum of the forces generated by the sutures and mesh adhesions to the parietal peritoneum. However data regarding adhesion formation obtained by Majercik indicated that as early as 2 weeks after implantation and fixation of the mesh fragments (2 × 7 cm) with protack, the adhesion strength achieves 73.6% (3.56 N) of the level that is achieved after 12 weeks (5.02 N) [7]. Papers addressing the adhesion strength at 4 weeks indicate that the strength required to detach a mesh fragments (10 × 15 cm) fixed with transparietal sutures and protacks was 5.9 N for Parietex, 12.1 N for Proceed and 12.9 N for the polypropylene mesh [12]. These data are similar to our results (10.68 N for all mesh fragments, 10.20 N for implants fixed with Maxon sutures, and 11.16 N for mesh implants fixed with PDS II). In a pig experimental model, Gonzales demonstrated that the fixation strength for mesh fragments (10 × 10 cm) fixed with non-absorbable sutures past 12 weeks is 194 ± 37 N for polyester (PE) meshes and 159 ± 43 N for polypropylene meshes (PP) [5]. Mc Ginty demonstrated that the mesh peel strengths from the abdominal wall after 4 weeks were 1.3 N/cm of mesh width for ePTFE, 2.8 N/cm for PCO and 2.1 N/cm for PPM.22 These data can be compared with our results, which were higher, as mentioned above. For meshes fixed with Maxon sutures, the value was 3.93 N/cm. For meshes fixed with PDS II, the value was 5.4 N/cm. The explanation for this difference may be the fact that in our study overgrowth the mesh lasted of two weeks longer [4,6,12,17,22].
According to accessible data, Maxon and PDS II sutures may degrade at different rates depending on their environment. After 3 weeks in the blood environment, the force required to break the Maxon sutures was 28 N and 18 N for PDS II sutures. In a pH 7 solution, these values were reduced (25 N and 17 N, respectively). In the other fluids, the endurance of PDS II sutures after 5 weeks was 10 N. After 4 weeks, the value for Maxon sutures is 16.4 N [13]. However; Metz observed that despite the increased baseline endurance of Maxon sutures, these sutures lose their supportive capability more rapidly in vivo than PDS II sutures [13,18,23,24].
In the present study the maximal fixing forces are greater 19,85 [N] (Maxon) and 24,09 [N] (PDS II). However, it should be clarified that the measurement technique made it impossible the separation of the restraining forces arising from the existing mesh adhesions to the abdominal wall on the strength of sutures.
The obtained results suggest that slow-absorbing sutures adequately maintained mesh stability at 6 weeks post implantation in an experimental model. However, it should be noted that an experimental study in pigs couldn’t be simply extrapolated to humans. The most important factors influencing the results include the different rates of degradation for slow-absorbing sutures and mesh overgrowth. Therefore, the conclusions drawn from the present study justify the decision to use these stitches during LVHR for further studies in humans. Additionally, we compared fixation forces between Maxon and PDS II [13,23,24]. These results indicate that both materials (Maxon and PDS II) are equally useful for mesh fixation in LVHR because the differences were statistically insignificant (Table 1). However, due to the small sample size in the analyzed groups, the proposal requires confirmation in a larger number of cases.
Conclusions
1. Six weeks after the surgery, stabilization forces generated by slow-absorbing sutures (introduced at 4-cm distances) and adhesions between DynaMesh IPOM and the abdominal wall provide adequate mesh fixation in an experimental model.
2. Both types of analyzed stitches (Maxon and PDS II) appear to exhibit similar properties in LVHR. However, further studies using a larger number of cases are necessary before conclusions are drawn.
9583
References
- Nienhuijs SW, Boelens OB, Strobbe LJ (2005) Pain after anterior mesh hernia repair. J Am Coll Surg 200: 885-889.
- Rakic S, Wassenaar EB, Raymakers JTFJ (2006) Chronic pain after laparoscopic repair of ventral and incisional hernia. 10th World Congress of Endoscopic Surgery, 14th International Congress of the European Association for Endoscopic Surgery (E.A.E.S.), Berlin, Germany.
- Eriksen JR, Poornoroozy P, Jorgensen LN, Jacobsen B, Friis-Andersen HU et al. (2009) Pain, quality of life and recovery after laparoscopic ventral hernia repair. Hernia 13: 13-21.
- LeBlanc K (2001) Laparoscopic treatment of ventral hernia. Surg Endosc 15: 1242.
- Gonzalez R, Fugate K, McClusky D 3rd, Ritter EM, Lederman A, et al. (2005) Relationship between tissue ingrowth and mesh contraction. World J Surg 29: 1038-1043.
- van't Riet M, de Vos van Steenwijk PJ, Kleinrensink GJ, Steyerberg EW, Bonjer HJ (2002) Tensile strength of mesh fixation methods in laparoscopic incisional hernia repair. Surg Endosc 16: 1713-1716.
- Majercik S, Tsikitis V, Iannitti DA (2006) Strength of tissue attachment to mesh after ventral hernia repair with synthetic composite mesh in a porcine model. Surg Endosc 20: 1671-1674.
- Hodgson NC, Malthaner RA, Ostbye T (2000) The search for an ideal method of abdominal fascial closure: a meta-analysis. Ann Surg 231: 436-442.
- Meijer EJ, Timmermans L, Jeekel J, Lange JF, Muysoms FE (2013) The principles of abdominal wound closure. Acta Chir Belg 113: 239-244.
- Krukowski ZH, Cusick EL, Engeset J, Matheson NA (1987) Polydioxanone or polypropylene for closure of midline abdominal incisions: a prospective comparative clinical trial. Br J Surg 74: 828-830.
- Reynvoet E, Berrevoet F, De Somer F, Vercauteren G, Vanoverbeke I, et al. (2012) Tensile strength testing for resorbable mesh fixation systems in laparoscopic ventral hernia repair. Surg Endosc 26: 2513-2520.
- Jacob BP, Hogle NJ, Durak E, Kim T, Fowler DL (2007) Tissue ingrowth and bowel adhesion formation in an animal comparative study: polypropylene versus proceed versus Parietex composite. Surg. Endosc. 21: 629-33.
- Freudenberg S, Rewerk S, Kaess M, Weiss C, Dorn-Beinecke A, et al. (2004) Biodegradation of absorbable sutures in body fluids and pH buffers. Eur Surg Res 36: 376-385.
- Hollinsky C, Göbl S (1999) Bursting strength evaluation after different types of mesh fixation in laparoscopic herniorrhaphy. Surg Endosc 13: 958-961.
- Hollinsky C, Hollinsky KH (1999) Static calculations for mesh fixation by intraabdominal pressure in laparoscopic extraperitoneal herniorrhaphy. Surg. Laparosc. Endosc. Percutan. Tech. 9: 106-109.
- Inaki N, Waseda M, Schurr MO, Braun M, Buess GF (2007) Experimental results of mesh fixation by a manual manipulator in a laparoscopic inguinal hernia repair model. Surg Endosc 21: 197-201.
- Sadava EE, Krpata DM, Gao Y, Schomisch S, Rosen MJ, et al. (2013) Laparoscopic mechanical fixation devices: does firing angle matter? Surg. Endosc. 27: 2076-2081.
- SmietaA, Ski M, Bigda J, Iwan K, Ko A‚ Odziejczyk M, Krajewski J, et al. (2007) Assessment of usefulness exhibited by different tacks in laparoscopic ventral hernia repair. Surg Endosc 21: 925-928.
- Hernández-Gascón B, Mena A, Peña E, Pascual G, Bellón JM, et al. (2013) Understanding the passive mechanical behavior of the human abdominal wall. Ann Biomed Eng 41: 433-444.
- Cobb WS, Burns JM, Kercher KW, Matthews BD, James Norton H, et al. (2005) Normal intraabdominal pressure in healthy adults. J Surg Res 129: 231-235.
- Schwab R, Schumacher O, Junge K, Binnebosel M, Klinge U, et al. (2008) Biomechanical analyses of mesh fixation in TAPP and TEP hernia repair. Surg Endosc 22: 731-738.
- McGinty JJ, Hogle NJ, McCarthy H, Fowler DL (2005) A comparative study of adhesion formation and abdominal wall ingrowth after laparoscopic ventral hernia repair in a porcine model using multiple types of mesh.Surg. Endosc. 19: 786-790.
- Sanz LE, Patterson JA, Kamath R, Willett G, Ahmed SW, et al. (1988) Comparison of Maxon suture with Vicryl, chromic catgut, and PDS sutures in fascial closure in rats. Obstet Gynecol 71: 418-422.
- Metz SA, Chegini N, Masterson BJ (1990) In vivo and in vitro degradation of monofilament absorbable sutures, PDS and Maxon. Biomaterials 11: 41-45.