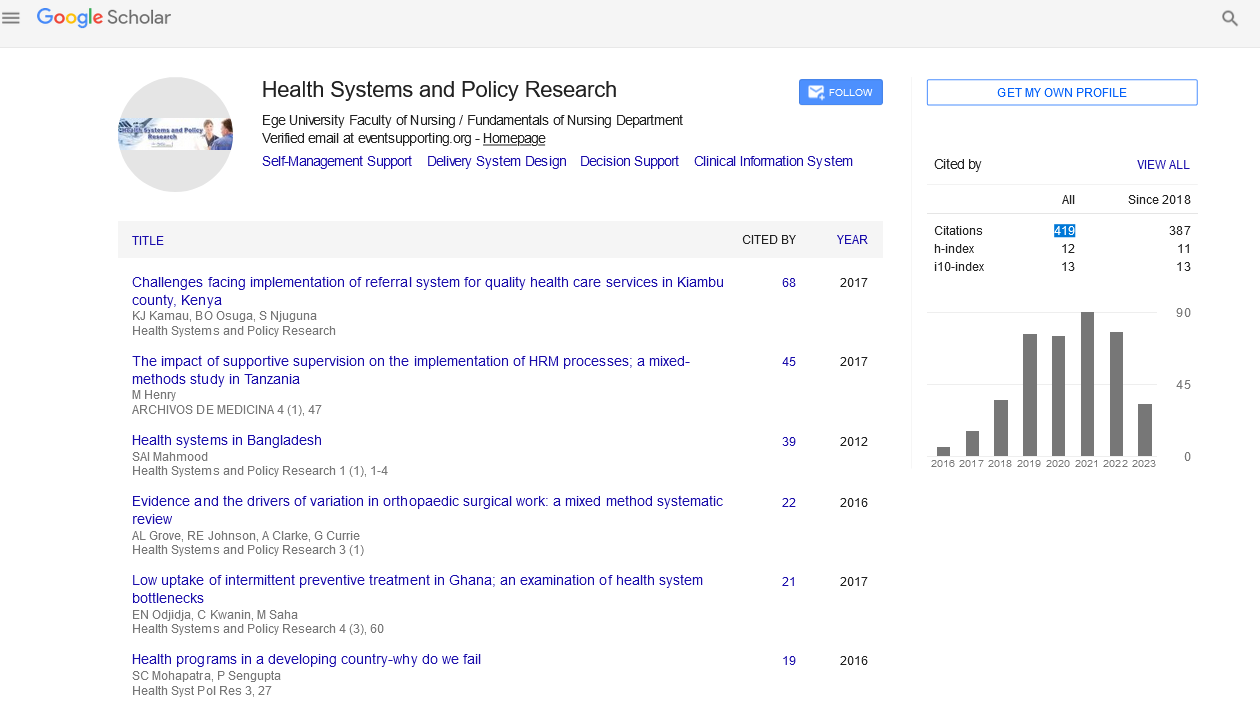
Perspective - (2022) Volume 9, Issue 12
Social determinants of health two different disparities in disease of covid 19 in both colours of Americans
Sarha Ali*
Department of health care, University of Health care, United States
*Correspondence:
Sarha Ali, Department of health care, University of Health care,
United States,
Email:
Received: 01-Dec-2022, Manuscript No. Iphspr- 22-13342;
Editor assigned: 09-Dec-2022, Pre QC No. Iphspr-22-13342;
Reviewed: 19-Dec-2022, QC No. Iphspr-22-13342;
Revised: 26-Dec-2022, Manuscript No. Iphspr- 22-13342 (R);
Published:
30-Dec-2022, DOI: 10.36648/2254- 9137.22.9.164
Abstract
The increased prevalence of Coronavirus Disease among racial and ethnic minority communities in the United States has exacerbated racial and ethnic health inequalities. Non-Hispanic Black and Hispanic/Latinx people with COVID-19 are more likely to require hospitalisation, admission to an intensive care unit, and pass away than non-Hispanic White people. In these minority communities, there may be discrepancies in COVID-19-related severity and outcomes, which may be attributed to a number of variables, including the higher prevalence of cardiovascular and metabolic illnesses, which is covered in our companion review article. When compared to non-Hispanic White people, social determinants of health have a significant but frequently underappreciated role in explaining racial and ethnic-related health inequalities in non-Hispanic Black and Hispanic/Latinx people.
Keywords
Covid-19; Infection Risk; Social Determinants; Structural Racism; Health Disparities; Hispanic Americans
INTRODUCTION
Consequently, the goal of this study is to concentrate on the
crucial health disparities in chronic illnesses and COVID-19
results in minority communities are influenced by socioeconomic
variables [1]. Here, we start by concentrating on structural racism
as a social determinant of health at the society level that fuels
subsequent social level and individual level health behaviours
that result in health inequalities. Last but not least, we wrap
up with a discussion of useful applications and suggestions for
future research and public health initiatives that aim to lessen
health inequalities and the total burden of disease [2]. More than
280 million individuals will have tested positive for Coronavirus
disease by the end of December 2021, including over 50 million
Americans [3]. Coronavirus disease is an ailment brought on by
severe acute respiratory syndrome coronavirus-2.1 [4]. Racial and
ethnic minorities in the US bear a disproportionate amount of the
COVID-19 burden. Non-Hispanic Black and Hispanic/Latinx people
with COVID-19 have higher chances of hospitalisation, intensive
care unit admission, and mortality than non-Hispanic White
people [5]. 2-4 Additionally, during the COVID-19 pandemic, the
US saw the biggest reported absolute rise in excess mortality,
which is defined as the increase in death from all causes relative
to predicted mortality [6].
Discussion
The age-standardized excess death rates in the US are significantly
higher for non-Hispanic Black and Hispanic/Latinx people than
for non-Hispanic White people, despite the fact that testing
capacity and reporting policy can have a significant impact on
the reported numbers of cases and deaths [7]. The processes
driving differences in COVID-19 severity and outcomes associated
to race and ethnicity are intricate. However, it is evident that a
larger occurrence of as reported in our companion review article
Cardiometabolic illness and its accompanying pathophysiological
symptoms, which are more common in non-Hispanic Black and
Hispanic Latinx people, significantly raise the risk of COVID-19
infection and mortality from severe cases [8]. This review's main
goal is to explain how socioeconomic determinants of health
affect racial and ethnic disparities in Cardiometabolic illness and
poorer health outcomes associated to COVID-19 [9]. We also draw
attention to how the racial and ethnic gap in social determinants of health has been widened by the COVID-19 epidemic. Finally,
we offer suggestions for public health policies based on research
that aim to address the socioeconomic determinants that cause
these health inequalities [10]. Here, we will examine the social
determinants of health that have an impact on both individual
and society health habits, including diet and physical activity. At
the social level, racism, economics, and public policy all have an
impact on health. Racism is a social construct that establishes,
upholds, and justifies unequal access to opportunities and
resources in society based on factors like race, nationality,
ethnicity, and other indicators of social rank. 8 Socioeconomic
imbalances are supported by the US's history of racial terrorism,
chattel slavery, and Jim Crow period regulations.
Conclusion
In recent years, systemic racism has had a much worse impact on
health and the persistence of health inequalities than overt acts
of racism on an individual level. Structural Racism includes laws,
regulations, and practises, institutions that control the economy,
as well as cultural and social structures within a society that
benefit racial and ethnic groups perceived as superior or having
greater status overall. 9 Structural racism works to disadvantage
other groups by giving benefits to some groups. Neighborhood
settings, for instance, are influenced by institutional and systemic
racism in the US. Racial residential segregation was implemented
by federal, state, and municipal laws and supported by real estate
practises like redlining and racist violence during the majority of
the 20th century in the US. 12 The geographical distribution of
a neighbourhood’s economic, educational, and environmental
attributes was established through intentional racial residential
segregation to benefit White residents.
Acknowledgement
None
Conflict of Interest
None
References
- Gold JAW, Rossen LM, Ahmad FB, Sutton P, Li Z, et al. (2020) Race, ethnicity, and age trends in persons who died from COVID‐19—United States, May‐August 2020. MMWR Morb Mortal Wkly Rep 69: 1517-1521.
Indexed at, Crossref, Google Scholar
- Hatef E, Chang HY, Kitchen C, Weiner JP, Kharrazi H, et al. (2020) Assessing the impact of neighborhood socioeconomic characteristics on COVID‐19 prevalence across seven states in the United States. Front Public Health 22: 571808.
Indexed at, Crossref, Google Scholar
- Wadhera RK, Wadhera P, Gaba P, Figueroa JF, Joynt Maddox KE, et al. (2020) Variation in COVID‐19 hospitalizations and death across New York city boroughs. JAMA 323: 2192‐2195.
Indexed at, Crossref, Google Scholar
- DiMaggio C, Klein M, Berry C, Frangos S (2020) Black/African American communities are at highest risk of COVID‐19: spatial modeling of New York City ZIP code‐level testing results. Ann Epidemiol 51: 7‐13.
Indexed at, Crossref, Google Scholar
- Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, et al. (2018) The state of US health, 1990‐2016: burden of diseases, injuries, and risk factors among US states. JAMA 319: 1444‐1472.
Indexed at, Crossref, Google Scholar
- Iavarone M, Ambrosio R, Soria A, Triolo M, Pugliese N, et al. (2020) High rates of 30‐day mortality in patients with cirrhosis and COVID‐19. J Hepatol 73: 1063-1071.
Indexed at, Crossref, Google Scholar
- Moon AM, Webb GJ, Aloman C, Armstrong MJ, Cargill T, et al. (2020) High mortality rates for SARS‐CoV‐2 infection in patients with pre‐existing chronic liver disease and cirrhosis: preliminary results from an international registry. J Hepatol 73: 705‐708.
Indexed at, Crossref, Google Scholar
- Loupy A, Aubert O, Reese PP, Bastien O, Bayer F, et al. (2020) Organ procurement and transplantation during the COVID‐19 pandemic. Lancet 395: e95‐e96.
Indexed at, Crossref, Google Scholar
- Mannucci E, Nreu B, Monami M (2020) Factors associated with increased all‐cause mortality during the COVID‐19 pandemic in Italy. Int J Infect Dis 98: 121‐124.
Indexed at, Crossref, Google Scholar
- Blach S, Kondili LA, Aghemo A, Cai Z, Dugan E, et al. (2021) Impact of COVID‐19 on global HCV elimination efforts. J Hepatol 74: 31‐36.
Indexed at, Crossref, Google Scholar
References
- Gold JAW, Rossen LM, Ahmad FB, Sutton P, Li Z, et al. (2020) Race, ethnicity, and age trends in persons who died from COVID‐19—United States, May‐August 2020. MMWR Morb Mortal Wkly Rep 69: 1517-1521.
Indexed at, Crossref, Google Scholar
- Hatef E, Chang HY, Kitchen C, Weiner JP, Kharrazi H, et al. (2020) Assessing the impact of neighborhood socioeconomic characteristics on COVID‐19 prevalence across seven states in the United States. Front Public Health 22: 571808.
Indexed at, Crossref, Google Scholar
- Wadhera RK, Wadhera P, Gaba P, Figueroa JF, Joynt Maddox KE, et al. (2020) Variation in COVID‐19 hospitalizations and death across New York city boroughs. JAMA 323: 2192‐2195.
Indexed at, Crossref, Google Scholar
- DiMaggio C, Klein M, Berry C, Frangos S (2020) Black/African American communities are at highest risk of COVID‐19: spatial modeling of New York City ZIP code‐level testing results. Ann Epidemiol 51: 7‐13.
Indexed at, Crossref, Google Scholar
- Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, et al. (2018) The state of US health, 1990‐2016: burden of diseases, injuries, and risk factors among US states. JAMA 319: 1444‐1472.
Indexed at, Crossref, Google Scholar
- Iavarone M, Ambrosio R, Soria A, Triolo M, Pugliese N, et al. (2020) High rates of 30‐day mortality in patients with cirrhosis and COVID‐19. J Hepatol 73: 1063-1071.
Indexed at, Crossref, Google Scholar
- Moon AM, Webb GJ, Aloman C, Armstrong MJ, Cargill T, et al. (2020) High mortality rates for SARS‐CoV‐2 infection in patients with pre‐existing chronic liver disease and cirrhosis: preliminary results from an international registry. J Hepatol 73: 705‐708.
Indexed at, Crossref, Google Scholar
- Loupy A, Aubert O, Reese PP, Bastien O, Bayer F, et al. (2020) Organ procurement and transplantation during the COVID‐19 pandemic. Lancet 395: e95‐e96.
Indexed at, Crossref, Google Scholar
- Mannucci E, Nreu B, Monami M (2020) Factors associated with increased all‐cause mortality during the COVID‐19 pandemic in Italy. Int J Infect Dis 98: 121‐124.
Indexed at, Crossref, Google Scholar
- Blach S, Kondili LA, Aghemo A, Cai Z, Dugan E, et al. (2021) Impact of COVID‐19 on global HCV elimination efforts. J Hepatol 74: 31‐36.
Indexed at, Crossref, Google Scholar
Citation: Ali S (2021) Social Determinants of
Health Two Different Disparities in Disease
of Covid 19 in Both Colours of Americans.
Health Sys Policy Res, Vol.9 No. 12: 164.