Key words
Hydrocephalus, ventriculoperotineal shunt, myelomeningocele repair.
Introduction
Neural tube defects (Neural dysraphism) are the most common congenital conditions affecting the nervous system, Myelomeningocele as one of neural tube defects is the most common congenital malformations that can result in severe lifelong disabilities, including paraplegia, hydrocephalus, Chiari II malformation (CM-II), incontinence, sexual dysfunction, skeletal deformations social and mental impairment [1, 2].
Myelomeningocele has been recognized since ancient times although written descriptions began not before the 17th century.
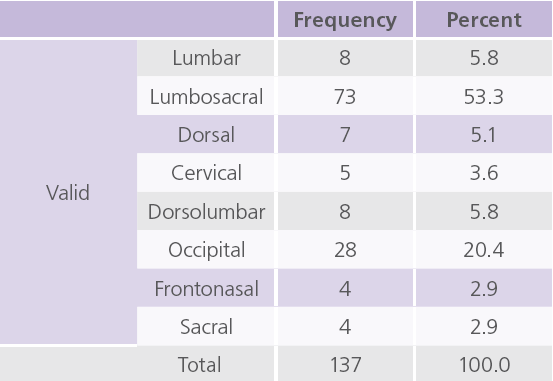
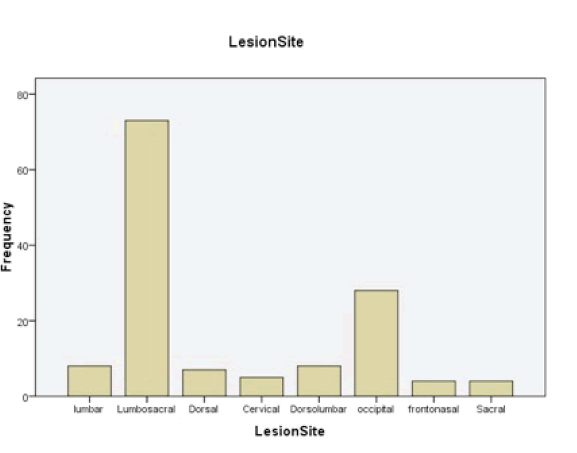
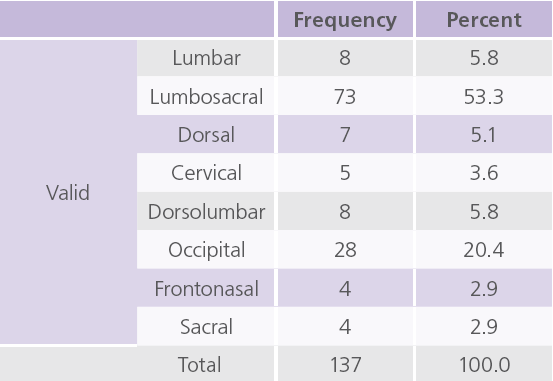
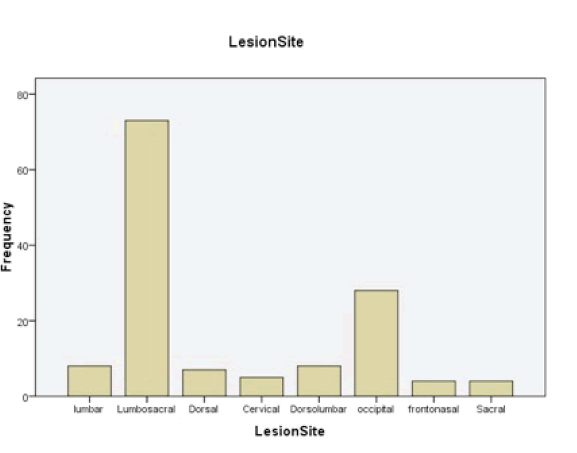
The usual site of the defect which is usually single is at the lumbosacral area but sometimes it is multiple and affects different sites like the dorsal or cervical spine. The same condition might affect the head and the brain (meningioencephalocele).
The extent of the problem
The incidence in the western community is low after controlling programs, in Africa the incidence is not known in most countries since the neurosurgical and pediatric surgery services are not well developed, but it is estimated to be high
The presentation of the condition in African children may be somewhat late, many factors contributed to this like lack of medical and surgical facilities, high expenses of such facilities, lack of awareness among population and professionals about the condition and its’ prognosis which is usually thought to be bad, and the presence of some traditional concepts about this condition.
The association of the condition with hydrocephalus worsen the situation and the prognosis in the affected individuals.
The establishment of programs to prevent and control this condition is necessary, such programs should recruit the efforts of both the professionals, the community and policy makers.
Myelomeningocele occurs in approximately 1 in 2900 live births in the United States. Fobe stated that myelomeningocele occurs in 0.4 for 1000 neonates and is associated with hydrocephalus in 85- 90% so the incidence is ranging between 1:2500 to 1: 3000 [3, 4].
Myelomeningocele is the most common type of spina bifida cystic. The late presentation and preoperative infection are associated with high mortality in those patients.
There is significant morbidity and mortality associating myelomeningocele specially within the first few decades of life [4]. The individuals affected with myelomeningocele are experiencing great difficulty in achieving normal milestones of development to adulthood life [5].
Neurological level in patients of myelomeningocele is the main factor that determined neurological abnormalities, major orthopedic deformities and ambulatory status [6].
Higher spinal cord lesion, hydrocephalus and complications due to its surgical management had a negative influence on physical, neurological and mental development of children born with myelomeningocele [7].
In African countries since there are no national efforts to prevent or compact this condition as the case in other regions of the world, the situation is worse.
In Saudia Arabia and in Cost Arica Latin American countries after folic acid flour fortification, there was an apparent decline in the incidence and the nature of NTDs in babies [8].
The recent trend in management of this condition is intrauterine surgical repair of the defects. In Africa there are no advanced antenatal care programs with early discovery or intrauterine surgical intervention for myelomeningiocele which can improve hydrocephalus and hindbrain herniation. Beside that the early repair can reduce the need for vetriculoperitoneal shunting, and may improve distal neurologic function in some patients.
Although myelomeningiocele is a complex condition, but most prevalent concomitant secondary conditions may be preventable through simple measures like support for skin, bladder care that can improve self-management and through health educational initiatives.
Large proportion of individuals with myelomeningocele had difficulties in participation and perceived low physical Health related quality of life HRQoL. Children with myelomeningocele had significantly reduced quality of life (QOL) compared to healthy individuals.
Many patients with myelomeningiocele reach adulthood and social continence; self-care may be expected in a large number of patients. Nevertheless, there are many associated neurological conditions that have to be faced.
Patients with a myelomeningocele born outside the hospital are prone to infectious complication. The most common cause of post-operative death was infection (65%).
Diagnostic tools
Ultrasound screening can identify most of central nervous system anomalies especially neural tube abnormalities [8].
Recently fetal MRI is an effective, noninvasive means of assessing fetal CNS anatomy.
Early diagnosis of hydrocephalus in children with myelomeningocele cannot reliably be made on physical examination alone and that other means mainly ultrasound and MRI of assessing ventricular size should be employed.
Postnatal MRI (of the defect, craniocervical junction and the brain) is considered very helpful in diagnosing the extent of the neurological involvement and putting the plan of the management.
Providing an advanced antenatal care programs with early discovery and sometimes intrauterine surgical intervention can improve hydrocephalus and hindbrain herniation, can reduce the need for vetriculoperitoneal shunting, and may improve distal neurologic function in some patients [4, 9].
Surgical repair
The management strategies ofmyelomeningocele (MMC) are early surgical treatment (Best with standard microneurosurgical techniques) to minimize the development of neurological defects. It is safe and effective to adopt surgery excision of the lesions with intradural exploration of the sac to release any potential adhesion bands.
Cerebral cortical malformations and hydrocephalus, in addition to the Chiari-II hindbrain malformation, are disorders caused by fetal CSF leakage. These malformations can be prevented with the technique of MMC closure [10, 11].
Primary management by endoscopic third ventriculostomy and choroid plexux cauterization ETV/CPC may avoids the increased danger of shunt dependence and infection for most infants with hydrocephalus associated with neural tube defects [12, 13].
The surgical treatment of hydrocephalus have to be done during the first month of life, care should be taken to avoid reoperations and infections that have unfavorable impact in the final outcome [3].
Since there is increased incidence of shunt complications many experts prefer to perform V-P shunt placement and myelomeningiocele repair in separate sessions while others suggest to do both in one session as they think that simultaneous insertion of shunt and correction of a myelomeningocele do not pose an additional risk to the patients health and do have some advantages, facilitating healing of the back without CSF leakage and protecting the brain from the effects of progressive ventricular dilatation. The insertion of a ventriculoperitoneal shunt, at the same session with the repair of the myelomeningocele, does not increase the risks of shunt infection or shunt malfunction.
Surgical repair of myelomeningocele may at times pose life-threatening complications mostly because of the associated anomalies like Chiari [14].
Some patients may show ascent of the cerebellar tonsils after postnatal myelomeningocele repair. Placement of a ventricloperitoneal shunt VP shunt may help to promote the ascent [15, 16].
Shunt complications remain an important cause of morbidity and mortality in myelomeningocele patients; particularly shunt infection [17].
Although Fetal surgery is nowadays adopted in many centers as alternative to post natal repair it might carry significant risks to the mother and fetus and these must be carefully considered prior to a final treatment decision [18].
Primary closure can be performed on clean, small defects with an intact sac. For defects larger than 25 cm(2) more soft tissue for well-vascularized coverage may be required [19].
The overall post-operative mortality was 8.3%, and in most of the cases ascribed to the Chiari malformation.
The situation in the Sudan
The national center of neurological sciences in Khartoum Sudan has great experience in managing this condition since the early seventies of the last century, it was and up to the recent days, the only center treating this condition in Sudan.
Material and methods
Retrospective review of cases which have been operated at the National Center for Neurological Sciences at Shaab hospital during the period from September 2010 to September 2012. The data obtained from a computerized data record system in the center and the patients clinically assessed by the author when they came for follow up in the refer clinic.
Results
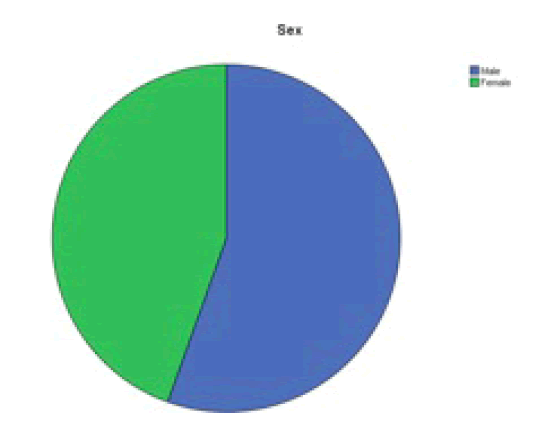
Sex distribution:
Male were 76 (55.5%).
Females were 61 patients (44.55%).
Level of the lesion
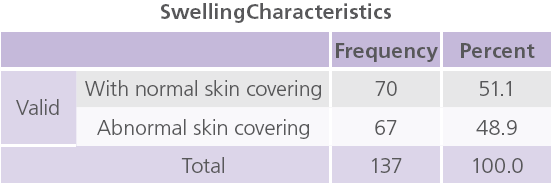
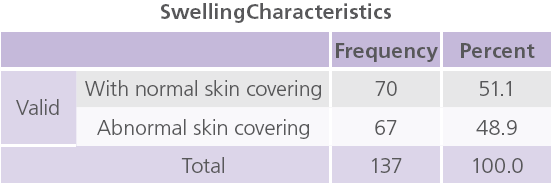
Skin over the lesion
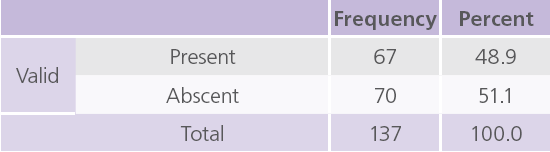
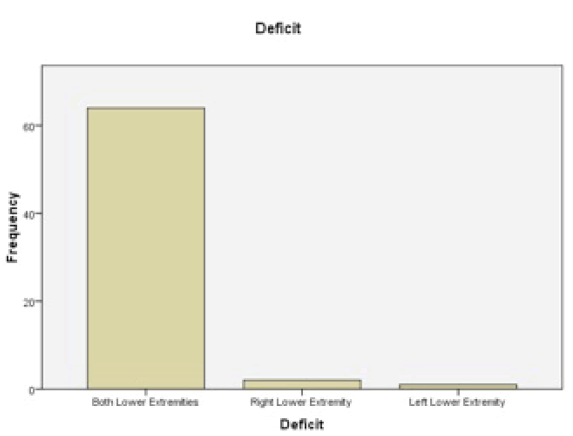
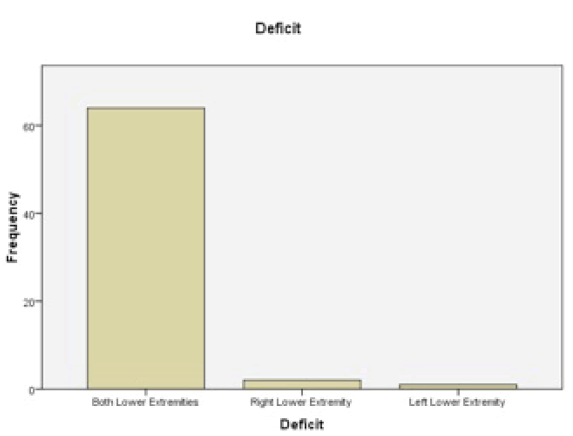
Neurological Deficit
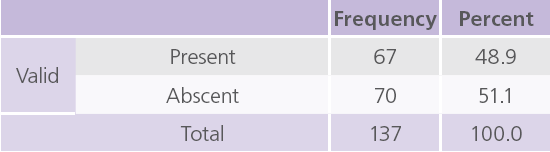
Lower Extremities Weakness
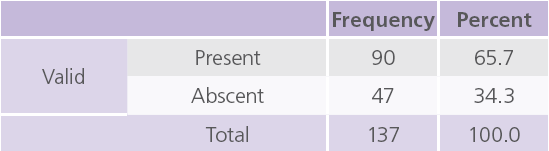
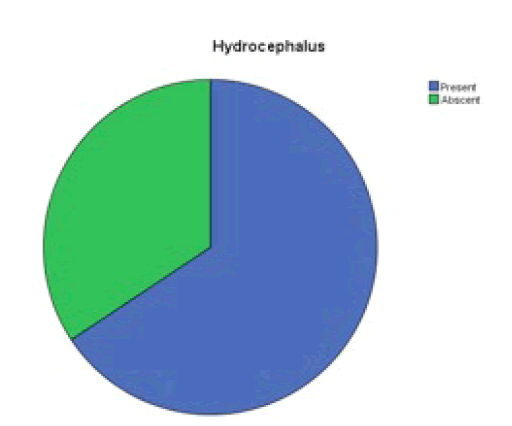
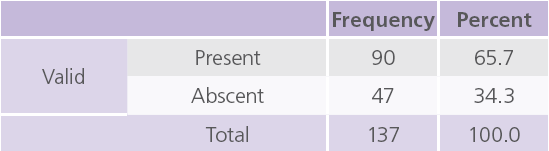
Hydrocephalus
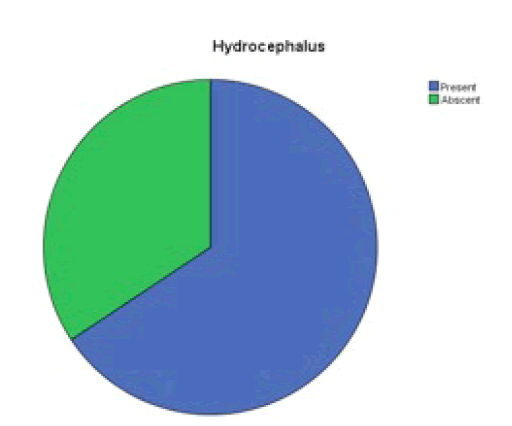
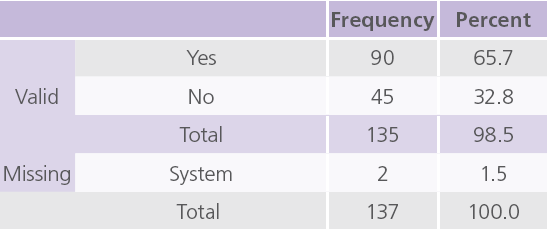
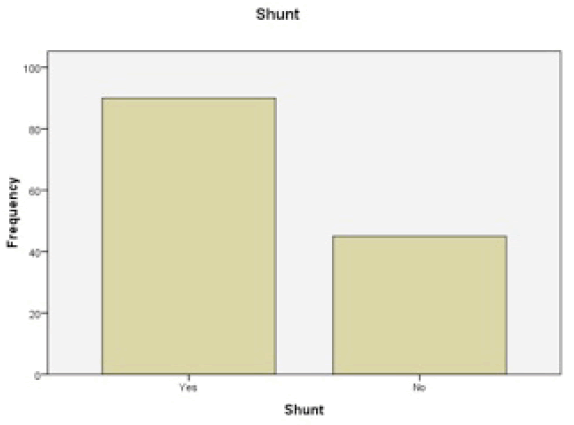
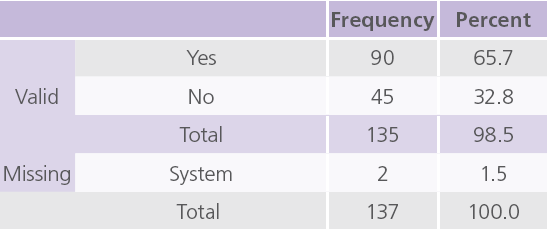
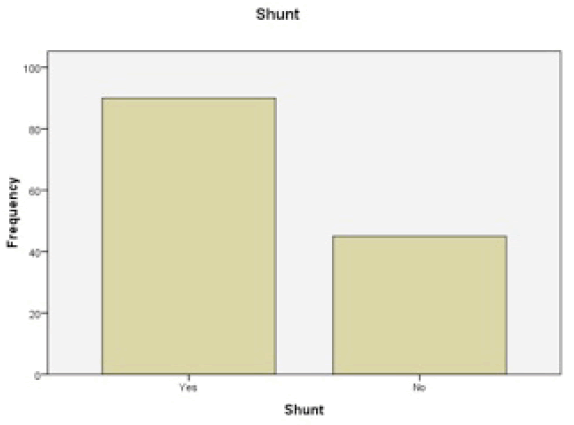
Ventriculoperitonial shunting
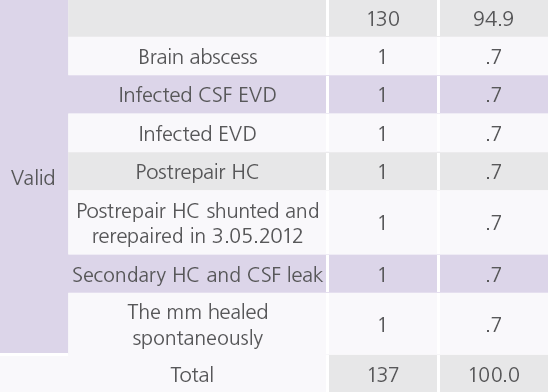
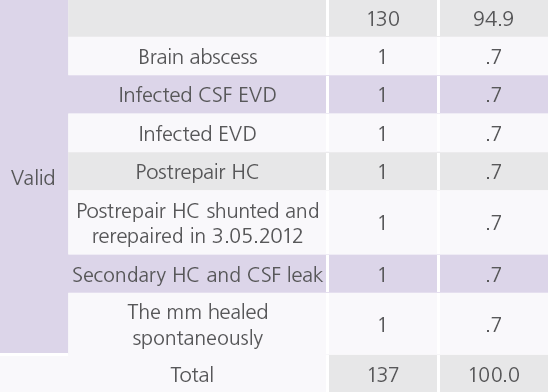
Complications
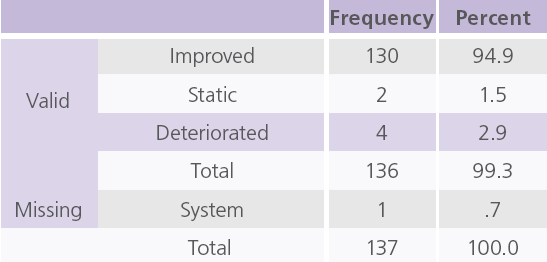
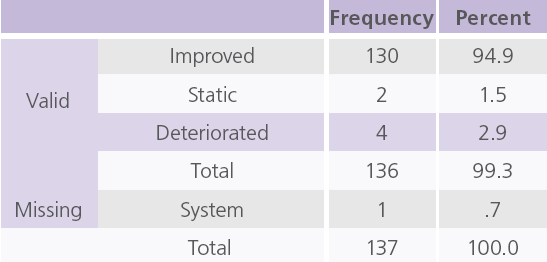
Final outcome
Conclusion
Spinal cord dysraphism is a serious neurological problems associated with aggressive morbidity and mortality.
Attention to this condition and establishment of preventive and early discovery and interventions programs is highly important.
Awareness of the community and medical professionals with impact of this problem with a sector of the community should be raised.
In our center the placement of ventriculoperitoneal shunt before surgical repair of the defect help to control the secondary effects on brain development and in achievement of solid sustainable repair free from tension and leaks of CSF a major cause of dehiscence of the repair The presence of cerebral spinal fluid shunting is a major contributor to increased survival of patients with MMC [20].
Tethered cord release can significantly improve symptoms in these patients and reduce the long term effect and complications of this condition [21]. The microsurgical procedures will help to prevent further neurological damage and deterioration during surgical intervention and may sometimes help to improve the neurological function.
Sometimes the presence of the defect might lessen the tension of hydrocephalus on the brain this might contribute to delayed presentation and in some cases surgical repair of the defect without previous shunting may lead to development of acute hydrocephalus.
In our center most of the patients tend to present early but late presentation is encountered from time to time.
The establishment of spina bifida association joining the families of the patients beside professionals and community workers as NGO and with its strong relations with local, regional and international corresponding bodies has helped in compacting the stigma of the condition and reducing the psychological and financial burden on the families of the patients .
The effort of Sudan government, the ministry of health and the national center of neurological sciences in providing the shunts and surgical treatment free of charge to all children below 5years of age helped in encouraging the families to bring their children early for the treatment.
1959
References
- Danzer, E., Adzick, NS. Fetal surgery for myelomeningocele: Patient selection, perioperative management and outcomes. Fetal Diagn. Ther. 2011; 30 (3): 163-73.
- Chan, WM., Dicianno, BE. Virtual socialization in adults with spina bifida. PM. R 2011; 3 (3): 25-219.
- Fobe, JL. et al. IQ in hydrocephalus and myelomeningocele. Implications of surgical treatment. Arq Neuropsiquiatr 1999; 57 (1): 44-50.
- Saadai, P., Farmer, DL. Fetal surgery for myelomeningocele. Clin. Perinatol. 2012; 39 (2): 88-279.
- Bellin, MH. et al. Interrelationships of sex, level of lesion, and transition outcomes among young adults with myelomeningocele. Dev. Med. Child Neurol. 2011; 53 (7): 647- 52.
- Iborra, J., Pages, E., Cuxart, A. Neurological abnormalities, major orthopaedic deformities and ambulation analysis in a myelomeningocele population in Catalonia (Spain). Spinal Cord. 1999; 37 (5): 351-57.
- Matuszczak, E., Lenkiewicz, T. Results of surgical treatment of myelomeningocele. Eur. J. Pediatr. Surg. 2006; 16 (5): 42-337.
- Aubry, MC., Aubry, JP., Dommergues, M. Sonographic prenatal diagnosis of central nervous system abnormalities. Childs Nerv. Syst. 2003; 19 (7-8): 391-402.
- Noetzel, MJ. Myelomeningocele: Current concepts of management. Clin. Perinatol. 1989; 16 (2): 311-29.
- Encinas, JL. et al. Maldevelopment of the cerebral cortex in the surgically induced model of myelomeningocele: Implications for fetal neurosurgery. J. Pediatr. Surg. 2011; 46 (4): 713-22.
- Tulipan, N., Hernanz-Schulman, M., Bruner, JP. Reduced hindbrain herniation after intrauterine myelomeningocele repair: A report of four cases. Pediatr. Neurosurg. 1998; 29 (5): 274-78.
- Warf, BC. Hydrocephalus associated with neural tube defects: Characteristics, management, and outcome in sub-Saharan Africa. Childs Nerv. Syst. 2011; 27 (10): 1589-94.
- Warf, BC., Campbell, JW. Combined endoscopic third ventriculostomy and choroid plexus cauterization as primary treatment of hydrocephalus for infants with myelomeningocele: Long-term results of a prospective intent-to-treat study in 115 East African infants. J. Neurosurg. Pediatr. 2008; 2 (5): 310-16.
- Singh, D. et al. Anesthetic concerns and perioperative complications in repair of myelomeningocele: A retrospective review of 135 cases. J. Neurosurg. Anesthesiol. 2010; 22 (1): 11- 15.
- Morota, N., Ihara, S. Postnatal ascent of the cerebellar tonsils in Chiari malformation Type II following surgical repair of myelomeningocele. J. Neurosurg. Pediatr. 2008; 2 (3): 188-93.
- Samuelsson, L. et al. MR imaging of syringohydromyelia and Chiari malformations in myelomeningocele patients with scoliosis. AJNR Am. J. Neuroradiol. 1987; 8 (3): 539-46.
- Tuli, S., Drake, J., Lamberti-Pasculli, M. Long-term outcome of hydrocephalus management in myelomeningoceles. Childs Nerv. Syst. 2003; 19 (5-6): 286-91.
- Gupta, N. et al. Open fetal surgery for myelomeningocele. J. Neurosurg. Pediatr. 2012; 9 (3): 265-73.
- Musluman, AM. et al. Clinical outcomes of myelomeningocele defect closure over 10 year. J. Clin. Neurosci. 2012; 19 (7): 984- 90.
- Davis, BE. et al. Long-term survival of individuals with myelomeningocele. Pediatr. Neurosurg. 2005; 41 (4): 186-91.
- Al-Holou, WN. et al. Secondary tethered cord syndrome in patients with myelomeningocele. J. Pediatr. Rehabil. Med. 2009; 2 (1): 29-36.