Keywords
Midwives; Rural health facilities; Maternal health
List of Abbreviations
CCT: Conditional Cash Transfer; CHEWs: Community Health Extension Workers; MNCH: Maternal, Neonatal & Child Health; MSS: Midwives Service Scheme; PHC: Primary Health Care; SBA: Skilled Birth Attendant; SURE P MCH: Subsidy Reinvestment & Empowerment Programme on Maternal & Child Health
Introduction
Nigeria, with over 170 million people has made tremendous efforts to meet the Millennium Development Goals (MDGs) relating to improving health outcomes for approximately 39 million women of child bearing age [1,2]. An estimated 40,000 maternal deaths occur yearly in Nigeria, comprising 14% of the global burden of maternal mortality [3]. Maternal mortality is a major public health challenge in Nigeria at the present ratio of 576 per 100,000 live births, 39% of women receiving no antenatal care and only 38.1% of mothers giving birth with a skilled birth attendant [1]. Despite the benefits and effectiveness of postnatal care (PNC), the 2013 National Demographic Health Survey (NDHS) reported that 58% of women received no PNC [1]. These averages disguise wide variations across the country with skilled birth attendant varying from 12.3% in the North-West geopolitical zone to 82.5% in the South-West zone. Overall, 22.7% of women in rural areas deliver with a skilled birth attendant as against 67.0% in urban areas. One in five births, particularly in Northern Nigeria takes place at home with no one present [4]. These patterns are replicated in other reproductive health key indices [1].
The health care worker (HCW) to population density in Nigeria (20 doctors, nurses and midwives per 10,000 population) is a little below the WHO recommendations of 23 per 10,000 [5]. However, the health workers in Nigeria are poorly distributed in favor of urban areas, southern zones, secondary and tertiary health care facilities. This inequitable distribution of skilled birth attendants is very apparent in the northern parts of the country and primary health care facilities in rural areas [1].
The shortage of skilled birth attendants such as midwives and doctors in rural Nigeria affects the utilization of services by women in these areas [5]. Since 2009, strategies towards improving these indices by the Government have focused on programmes that strengthen the health system by improving access to healthcare and health outcomes [6]. This led to the introduction of a high profile umbrella approach of the Saving One Million Lives (SOML) programme. This ensured the integration of existing primary health care activities such as the Midwives Service Scheme (MSS) introduced in 2009 and the Subsidy Reinvestment and Empowerment Programme on Maternal and Child Health (SURE-P MCH) introduced in 2012 [7]. The gap in utilization of primary health care services for skilled births alongside other poor maternal and child health indices led to the conception of the MSS and SURE-P MCH by the Nigerian Government.
The MSS aimed to address the inequitable coverage of maternal, neonatal and child health services (MNCH) and distribution of midwives. This was done by engaging and deploying newly graduated, unemployed and retired but still able midwives to work in selected primary health care (PHC) facilities in rural communities [7,8]. However the deployment of skilled birth attendants under the MSS did not improve the demand and uptake of maternal health services at the PHCs [8]. The Government of Nigeria inspired by the success and lessons learnt from the MSS and also committed to improving the health care system, established a maternal and child health (MCH) component of the Subsidy Reinvestment and Empowerment Programme (SURE-P). The SURE P MCH had two main components: the supply and demand side activities. The supply side components encompassed deployment of human resources for health, supplies of medical tools, equipment, drugs and other commodities, capacity building and infrastructure development whilst the demand side initiatives supported uptake of services by using cash based and other incentive schemes and outreach services.
This new programme supported an additional 1000 primary health care (PHC) facilities in rural communities across Nigeria and also implemented strategies to mitigate some of the challenges encountered in implementing the MSS [9].
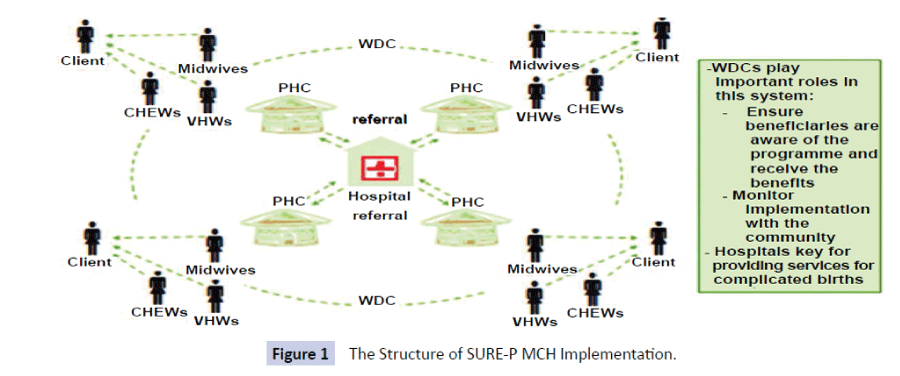
This paper presents a study of the implementation of the provision of maternal health services by midwives in the 1000 PHC facilities supported by the SURE-P MCH initiative. These facilities are located in all the 36 States plus the Federal Capital Territory under the 6 geopolitical zones of Nigeria. The facilities were structured as a hub and spoke model, with 4 PHC facilities and a referral General hospital in a Local Government area. These facilities were designated to provide free maternal, newborn and child health services at all times. The supply components comprised of 4 midwives, 2 community health workers and 6 village health workers deployed to each PHC (Figure 1). The purpose was to ensure the provision of 24 hour service and availability of skilled birth attendant at all times. In addition, these facilities were renovated and provided a source of water supply, drugs, commodities and medical equipment.
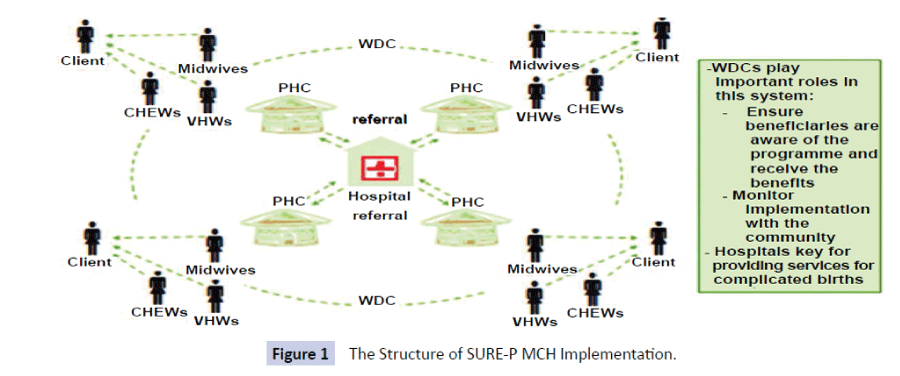
Figure 1: The Structure of SURE-P MCH Implementation.
Midwifery is a key element of sexual, reproductive, maternal and newborn health care. It is defined as the health services and workforce needed to support and care for women and newborns, including sexual and reproductive health and especially pregnancy, labour and postnatal care [10].
The midwives had three core responsibilities; Clinical services - provision of antenatal care, delivery of babies, referral of complicated cases and postnatal care, Education of pregnant women - health education through health promotion talks on breast feeding, nutrition at the clinics and provision of information leaflets and Administrative services-team meetings, recording of activities and supervisory functions. The midwives and other health care workers received refresher training at appropriate levels on Life Saving Skills and Care of the Newborn. The midwives also provided mentoring support to the community health extension workers and village health workers.
The challenge of low uptake of maternal services at the PHCs were partly addressed by the introduction of a conditional cash transfer (CCT) scheme for mothers accessing MNCH services at these facilities. The CCT programme provided financial incentives to enrolled women for attending key health services. The goal was to promote retention throughout the continuum of care [11]. A pregnant woman receives 5000 naira (approximately $30 USD) which is pro-rated according to the responsibilities she completes. The value was based on average cost of out of pocket expenses throughout the period of pregnancy.
The outcomes of the CCT initiative which is the main demand component of this programme has been published elsewhere [12]. In summary the CCT intervention was associated with significant increase in number of women attending four or more ANC visits and those receiving two or more doses of tetanus toxoid during pregnancy [12].
The objective of this study was to assess the potential of using midwives as skilled birth attendants in providing access to maternal health services in rural Nigeria using the SURE P MCH programme. It is envisaged that this will eventually contribute towards building the health care system. The results from the SURE-P MCH programme is presented in this paper. This focused on access to antenatal care and skilled birth attendant indicators. It also discusses the challenges encountered in implementing such a programme.
Subjects and Methods
The implementation of the SURE P MCH programme was preceded by establishing core baseline maternal health indicators (Table 1) in the 1000 Primary Health Care (PHCs) facilities which are the subject of this study. The rationale for the baseline survey was to provide a clear framework for future monitoring and evaluation. The selection criteria for the facilities included remote and rural location, covering a population of between 10,000 to 30,000 people and providing maternal and child health services. The study area covered an estimated 25 million population. The numbers of primary health care (PHCs) facilities selected in each rural location was dependent on the maternal mortality and health burden (Table 2).
| PHCs with 24 hours maternal health services |
| Number of Midwives (Skilled Birth Attendants present) |
| Total Antenatal Care (ANC) Visits |
| New ANC visits |
| Pregnant women with 4 or more ANC visits |
| Deliveries by skilled birth attendants |
| Post natal check visits |
| Use of contraceptive methods |
Table 1: Core indicators.
| Geopolitical Zone |
States |
Number of Primary Health Care facilities |
| North Central Zone |
7 States |
24 facilities per state=168 |
| North East Zone |
6 States |
32 facilities per state=192 |
| North West Zone |
7 States |
32 facilities per state=224 |
| South East Zone |
5 States |
24 facilities × 4 states=96 plus 32 facilities in one state=128 |
| South South Zone |
6 States |
24 facilities per state=144 |
| South West Zone |
6 States |
24 facilities per state=144 |
| Total |
37 |
1000 |
Table 2: Distribution of Primary Health Care Facilities under the Programme.
A nationwide survey was conducted in November 2012 using trained field workers to collect information on the core indicators at baseline (Table 1) for a period of six months before programme commencement. The same survey was repeated in August 2014 to collect the follow-up data for a period of six months. The data collected focused on the indicators outlined in (Table 1).
The SURE P MCH monitoring and evaluation data collection tool adapted from the National Health Management Information System tools and other MNCH survey tools previously used in Nigeria was used for the survey [13]. The tool was adapted by working in partnership with monitoring and evaluation officers from the 36 States and Federal Capital Territory (FCT).
Field officers were engaged and trained on the use of the survey tool to collect information from the primary health care facility based registers such as the ANC, labour and delivery and immunization registers. They were also trained on the use of the guidelines produced for the field implementation. The field officers were fluent in reading and writing both English and a local language. The survey was carried out in all 1000 SURE-P MCH supported primary health care facilities across the 6 zones and 36 States and the FCT. Two field workers were assigned to collect data from three or four clusters with 4 PHCs making up a cluster, for a 3 day period. Each of the six geographical zones had one supervisor. Completed survey tools were returned to the SURE-P MCH Project Implementation Unit by the supervisors, for data validation, processing and analysis.
Data analysis
Data was collected using appropriate tools and after thorough data cleaning, was entered into an excel based pre-analytic template. Data summary was done electronically in the excel program with collation starting from the lowest point (facility) up to the national level. A summary of proportions was done of the indicators of interest. From the data collected on the core indicators aforementioned, four line elements (1) Pregnant women with 4 or more ANC visits (2) Births by Skilled Birth Attendance (3) Postnatal check visits 2 days after delivery, and (4) Contraceptive use (any method), were compared to the baseline information derived from the 2013 NDHS report. Rural percentages from the NDHS Report 2013 were used as SURE-P MCH interventions were focused on rural facilities. The percentage change in terms of numeric size of the follow-up data relative to the baseline data collected before the programme started were also measured. The percentage proportional difference between specific line indicator at baseline and follow-up were tested statistically using the chi-square test of proportions and Wilcoxon signed test (nonparametric version). Also the levels of statistical significance were determined for each of the four core-indicator domain. The level of significance for the test statistics was set at p <0.05.
The choice of test statistics was based on the satisfaction that the sample met the critical requirement for the chi-square test of proportions and Wilcoxon signed tests. Epi Info software (version 7) was used for the analysis.
Ethical approval for the collection of data from the PHC facilities was not required by the as the data is already in the public domain and does not identify individual patients. However, we sought permission and obtained approval from the State Ministry of Health and the Local Governments responsible for the PHC facilities.
Results
A total of 1000 primary health care facilities across the six geopolitical zones were supported by the SURE P MCH programme and provided 24 hour services which did not obtain before the programme commenced. A total of 3158 midwives were recruited and deployed between October 2012 when the programme started and 2014. There were no midwives in all facilities before October 2012. The newly engaged midwives were distributed across the 1000 facilities according to the structure (See figure 1) where possible. A total of 597 midwives were deployed to the North-Central zone, 389 to North-East zone, 586 to North-West zone, 509 to South-East zone, 571 in South-West zone and 506 in South-South zone.
(Table 3) compares the baseline national percentages from the National Demographic Health Survey (NDHS) report of 2013 and the follow-up data from SURE-P MCH initiative. The difference in the number of births by the skilled birth attendants (the midwives deployed to the facilities supported by SURE P MCH) and the number of women now using a contraceptive method in the areas where these facilities are located were significant.
| Maternal Health Indicator |
Baseline-National Percentages (NDHS 2013)* Rural Areas |
Follow-up National Percentages(SURE-P MCH) |
P-values (Chi-Square) |
| Pregnant women with 4 or more ANC visits |
38.2% |
30.0% |
0.296 |
| Deliveries by skilled birth attendance |
22.7% |
56.0% |
0.0001* |
| Post natal check visits after 2 days |
29.0% |
33.0% |
0.647 |
| Usage of contraceptive method (any method) |
9.0% |
66.0% |
0.0001* |
*P value <0.0001
Table 3: Maternal Health Indicators: Baseline National Percentages Compared to Follow Up National Data from SURE P MCH Programme.
The analysis of data collected before the programme started and follow-up for the core indicators are highlighted in (Table 4). The total numbers of antenatal care (ANC) visits were up by 42%, new ANC visits by 39% and four or more ANC visits increased by 30% after the follow-up survey. Births by skilled birth attendants were up by 56%, postnatal visits by women were also up by 33% and women using contraceptive methods increased by 66%.
| SURE P MCH Core Indicators |
SURE P MCH Baseline (April to September 2012) |
SURE P MCH Follow Up March to August 2014 |
Percentage (%)increase from Baseline |
| PHCs with 24 hours Maternal health Services |
0 |
1000 |
100 |
| Number of midwives present in the facilities |
0 |
3158 |
100 |
| Total ANC Visits |
316,784 |
545,160 |
42 |
| New ANC Visits |
126,068 |
207,361 |
39 |
| Pregnant women with 4 or more ANC visits |
98,863 |
141,937 |
30 |
| Deliveries by Skilled Birth Attendants |
35,898 |
81,830 |
56 |
| Post natal Check Visits after 2 days |
84,217 |
125,944 |
33 |
| Use of any Contraceptive methods |
29,893 |
88,422 |
66 |
Table 4: Baseline Data Compared to Follow up Data under the SURE P MCH Programme.
Disaggregated data analysis for the same number of facilities supported by the SURE-P MCH programme in each State in the North-East and North-West zones showed increases from the baseline for all core indicators (Table 5). The skilled delivery at birth and use of contraceptive methods showed only marginal increase at follow-up for both zones.
| |
Total ANC |
4+ANC Visits |
Skilled Birth Delivery |
Post-natal Check Visits |
Use of Contraceptive Methods |
Use of Contraceptive Methods |
| Zone |
Baseline |
Follow-up |
Baseline |
Follow-up |
Baseline |
Follow-up |
Baseline |
Follow-up |
Baseline |
Follow-up |
Baseline |
Follow-up |
| North East |
95,906 |
132,355 |
46,173 |
62,171 |
15,777 |
31,430 |
9,332 |
16,778 |
40,282 |
50,578 |
5,814 |
7,899 |
| North West |
98,819 |
199,417 |
42,960 |
79,294 |
32,298 |
44,938 |
9,280 |
23,962 |
9,491 |
22,329 |
9,546 |
16,207 |
| North Central |
29,064 |
56,742 |
10,937 |
56,742 |
11,596 |
13,809 |
4,603 |
11,135 |
4,468 |
7,011 |
3,977 |
7,006 |
| South-South |
22,478 |
39,378 |
7,473 |
9,573 |
10,189 |
14,607 |
7,942 |
5,813 |
12,815 |
13,155 |
2,426 |
5,573 |
| South East |
13,932 |
36,651 |
5,230 |
12,471 |
3,520 |
8,664 |
3,728 |
5,970 |
3,904 |
5,092 |
1,518 |
2,519 |
| South West |
55,585 |
80,617 |
13,295 |
21,298 |
25,483 |
28,489 |
8,040 |
18,172 |
9,432 |
27,779 |
6,612 |
10,180 |
| Median |
42,325 |
68,680 |
12,116 |
39,020 |
13,687 |
21,548 |
7,991 |
13,957 |
9,462 |
17,742 |
4,896 |
7,453 |
| P-value* |
0.028 |
0.028 |
0.028 |
0.028 |
0.046 |
0.028 |
Related-samples Wilcoxon Signed Rank Test*
Table 5: Baseline Data Compared to Follow Up Data in Facilities in the Six Geo-Political Zones.
Similar patterns were observed in the North-Central zone and South- South zone. Although the number of births by skilled birth attendants fell slightly at follow up, there was still a slight increase in the number of postnatal visits in the South-South zone (Table 5).
Similar patterns were also recorded in the South-East and South-West zones. Although the South-West zone showed more remarkable increases in total and new ANC visits, births by skilled birth attendants, postnatal visits and number of women using contraceptive methods (Table 5).
In summary, p-value for all core indicators were statistically significant, with a range of 0.48 – 0.46 (p<0.05). Thus showing the intervention had a positive impact on maternal health care improvement.
Discussion
The routine monitoring information of core indicators identified at the beginning of the Subsidy Reinvestment and Empowerment programme on maternal and child health (SURE-P MCH) demonstrated overall improvements in access to maternal health services at follow up. These improvements in care observed after deploying midwives to rural areas is a timely and an important issue which can influence policy decisions in many rural areas. The midwives who are the skilled birth attendants were supported by the community health extension workers (CHEWs) and the Village Health workers (Figure 1) who provided outreach services and therefore augmented the demand side of the programme. The Conditional Cash Transfer (CCT) initiative under the programme piloted in a subset of 78 facilities in 18 states also contributed to increase in uptake of services [12]. As part of strengthening the health system, the midwives were also supported with refresher courses, supply of drugs and consumables, medical equipment and other relevant tools for provision of quality services. Midwives, when educated and regulated to international standards, have competences to deliver 87% of services needed by pregnant women [10].
Timely and appropriate ANC visits can reduce maternal morbidity and mortality [14]. When women avail themselves of ANC services, pregnancy associated complications that may affect pregnancy adversely are identified early [15,16]. The World Health Organisation [17] recommends focused antenatal care which encourages early booking. However despite the advantages of early booking, late booking or non-attendance at ANC is common in Nigeria [18,19].
(Table 5) shows the changes over time by comparing the follow-up data in 2014 to the baseline data in 2012 (pre-implementation) on the core indicators by geopolitical zones. The improvements were almost even across all zones except for the facilities in South-South zone which did not show any improvements in skilled births and postnatal visits at the facilities. The North- East zone also showed minor improvements in new acceptors of contraceptive methods. The lack of improvements in these indicators in the South-South zone could be due to frequent health care worker strikes in the zone and the tendency of the facilities requiring women to pay for services which are meant to be provided for free at all SURE-P MCH supported facilities. The very low increase in use of modern contraceptive methods in the North-East may be due to cultural and religious views on family planning services and a significant percentage (60%) of women still give birth to their babies at home [4] in the Northern zones. The analysis of the findings by zones is helpful for programme implementers to identify areas that require more support to enhance improvements. Although the p value for all the core indicators for all zones was significant, these improvements cannot only be attributed to the midwives.
However, the findings here are in keeping with the evidence that midwives as skilled birth attendants can make a difference to maternal morbidity and mortality and are crucial to improving access to maternal health services at primary health care facilities and more especially in rural areas [19,20]. Furthermore the combination of supply and demand elements in this programme enhanced the outcome achievements outlined in this paper.
Accelerated and equitable expansion in access and utilization of these evidence based interventions will be vital to meeting the new Sustainable Development Goals [21] in Nigeria and other countries. Rapid expansion of this initiative can be achieved through effective recruitment and deployment of appropriately skilled and motivated health care staff with the support of the demand side initiatives.
Despite these improvements, the programme continues to face a number of challenges such as non-availability of midwives to be deployed to the primary health care facilities in the North- East and North-West zones where the need is greatest. This is shown by the difference between the actual number of midwives recruited and deployed and the numbers required according to the programme structure. For example facilities in the North-East zone required 768 midwives but only 389 were available for recruitment and deployment. The experience gathered in implementing the Midwives Service Scheme (MSS) helped identify the need to modify the National policy to allow Community Health Extension Workers provide more services such as contraceptive injectable to women and also review some tasks to compliment the role of midwives particularly where they are not available [11].
In most cases, when available midwives are deployed, retaining them becomes a challenge because of the insecurity issues such as the Boko Haram insurgency in the North-East region of the country. Retention of midwives in the rural communities where these facilities are located is also a challenge due to inadequate basic amenities such as good schools, language issues and housing accommodation. To mitigate some of these challenges the programme embarked on constructing a two bedroom house for each cluster of four primary health care facilities in a Local Government Area. The Ward Development Committees, a group of the community’s local leaders, were also used to support the midwives by providing them with extra accommodation and security. The programme also explored incentive schemes to support the retention of health care staff in the field. These challenges are being explored in further details in another study.
Limitations
Although all the 1000 facilities supported by the programme were located in the rural area according to the criteria for selection, some potentially confounding factors may include the differences in the characteristics of the facilities and the communities such as level of education, cultural and religious beliefs which may influence behaviour towards accessing the services. The data used for the analysis in this programme was collected from maternal and child health registers at the primary health care facilities which are sometimes poorly recorded and incomplete. However adequate training was given to the field officers and standardized tools were used for the validation of the data collected by their supervisors. The follow-up analysis presented only shows change over time which cannot be definitely attributed to the midwives alone until an impact evaluation is carried out. However to share the potentials of the programme and the experiences from our assessments, the follow-up survey results were also triangulated by comparing them to the same indicators from rural areas in the National Demographic Health Survey of 2013. The programme covered all the 36 States and the Federal Capital Territory within the six geopolitical zones in the country and 393 out of 774 Local Government Areas. The results from the programme are therefore representative of different areas of the country and will add to the efforts of strengthening health systems and reducing maternal morbidity and mortality in the country.
Despite the limitations discussed above the information provided by this study of the Subsidy Reinvestment and Empowerment programme on Maternal and Child Health has demonstrated the potential to improve access to maternal health services in the rural communities. The midwives and other categories of health care workers were not present in these facilities before October 2012 when the programme commenced. This programme builds on the lessons learnt from the Midwives Services Scheme established by the Government in 2009 by implementing a demand (initiatives to increase uptake of services) and supply side (initiatives such as deployment of human resources for health, drugs and commodities etc.) component of the programme.
Conclusion
The information presented in this paper suggests that women are more likely to have more supervised births and use more contraceptives in rural facilities when midwifery services are present particularly in rural communities. This will invariably contribute to strengthening the primary health care system. The outcomes of this programme should encourage the 36 States and the Federal Capital Territory using the platform of the recent National Health Act [22] to scale up this programme to other facilities in their state not covered by the programme whilst taking on board the challenges outlined. The achievements of this programme if replicated in every ward in Nigeria and other countries with similar maternal health burden will enable the acceleration towards achieving the new United Nations Sustainable Development Goals [21].
Acknowledgements
The authors are grateful to all the members of the Subsidy Reinvestment and Empowerment programme on maternal and child health, the health care workers and all stakeholders at the Federal, State and Community level that supported the implementation of a successful programme.
Conflict of Interest
The authors have no conflict of interest.
Authors Contributions
UO and CE wrote the first draft. All authors (UO, CE, MSA, TO, AO and WE) contributed to the reviews and redrafting and final approval of the manuscript.
9734
References
- (2013) National Population Commission (Nigeria), ICF International (2014): Nigeria Demographic and Health Survey 2013. Abuja, Nigeria and Rockville, Maryland, USA: NPC and ICF International.
- World Bank (2014) World Development Indicators. Washington, DC: World Bank.
- World Health Organization (2014) Trends in Maternal Mortality: 1990 to 2013 – WHO, UNICEF, UNFPA and World Bank Estimates. Geneva.
- Fapohunda BM, Orobaton NG (2013) When women deliver with no one present in Nigeria: Who, What, Where and so what? PLoS One 8.
- World Health Organization (2010) Atlas of Healthcare Workforce Report. Geneva.
- Koblinsky M, Mathew Z, Husssein J, Mavalankar D, Mridha MK, et al. (2006) Going to scale with professional skilled care. Lancet 368: 13377-1386.
- Williams A (2014) The Evolution of Programs Designed to Increase Utilization of Skilled Birth Attendance in Nigeria. In Science of Delivery Case Study.
- Okeke E, Glick P, Abubakar Isa S (2015) The Better Obstetrics in Rural Nigeria (BORN) Study, An Impact Evaluation of the Nigerian Midwives Service Scheme. RAND Corporation.
- Abimbola S, Okoli U, Olubajo O, Abdullahi MJ, Pate MA, (2012) The Midwives Service Scheme in Nigeria. PLoS Med 9:e1001211.
- UNFPA, ICM, WHO, (2014) The State of the World’s Midwifery Report: A Universal Pathway. A Woman’s Right to Health, United Nations Population Fund.
- Abimbola S, Ihebuzor N, Okoli U (2015) Five ways an innovative program increased facility birth in Nigeria, MHTF-PLoS open –access collections – Translating Research into Practice Series.
- Ugo O, Morris L, Oshin A, Pate MA, Aigbe C, et al. (2014) Conditional cash transfer schemes in Nigeria: potential gains for maternal and child health service uptake in a national pilot programme. BMC Pregnancy and Child Birth 14: 408.
- (2012) The Subsidy Reinvestment & Empowerment Programme: Monitoring and Evaluation Routine Data Collection Tool.
- Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, et al. (2008) What works? Interventions for maternal and child under nutrition and survival. Lancet 371:417-440.
- Aluko JO, Oluwatosin A, (2008) Pattern and outcome of antenatal care among women attending a catholic mission hospital in Ibadan, Nigeria. African Journal of Medical Sciences 37: 231-238.
- Raj P (2005) Pregnancy Complications among married women in Uttar Pradesh and health seeking behaviour of these women. Research and Practice in Social Science 1: 48-63.
- World Health Organization (2011) WHO Statement on antenatal care. Geneva.
- Adekanle DA, Isawumi AI (2008) Late antenatal care booking and its predictors among pregnant women in South Western Nigeria. Online Journal of Health Allied Sciences 7:4.
- Osunbor KM, Fatusi AO, Chiwuzie JC (2006) Maternal health seeking behaviour and associated factors in rural Nigeria community. Maternal Child Health J 36: 159-169.
- Federal Ministry of Health (2011) Saving New born Lives in Nigeria: New born Health in the Context of the Integrated Maternal, New born and Child Health Strategy.
- United Nations (2015) Sustainable Development Goals, The Road to Dignity, UN Secretary General’s Office.