Porta-Etessam J*, Muñiz S, Cuadrado ML, González-García N, Orviz A, Abarrategui B, Fernández-Matarrubia M
Headache Unit. Neurology Department. Hospital Universitario Clínico San Carlos. Madrid. Spain
*Corresponding Author:
Jesús Porta-Etessam
C/ Andrés Torrejón, 15, 7º 28014 Madrid
Telephone: +0034667062490
E-mail: jporta@yahoo.com
Key words
Hypnic headache, flunarizine, caffeine, indomethacin
Introduction
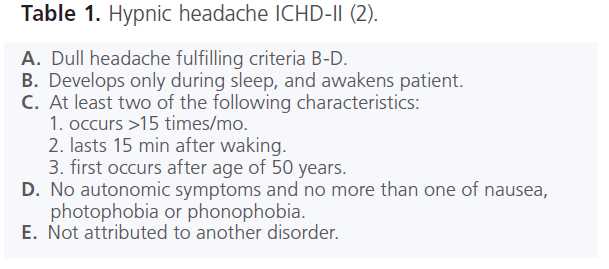
Hypnic headache (HH) is primary headache described by Raskin in 1988 and characterized by recurrent nocturnal episodes of headache that periodically wake the sleeping patient (1). In the second edition of International Headache Society classification, this syndrome was included in section 4.5, in the group of “Other primary headaches” (2) (table 1). The pathophysiology of HH is still unknown. It has been postulated that HH is a spectrum disorder overlapping with other primary headaches. For other authors could be a particular subtype of cluster headache (3). There have been reported symptomatic cases due to a pontine reticular formation ischemic stroke and posterior fossa meningioma (4-5).
We describe six patients with hypnic headache according to the HIS-II classification and initially treated with flunarizine. Structural lesion has been rule out performing brain MRI in all cases.
Patients and methods
We select six patients (3 females and 3 males) that had been diagnosed of hypnic headache in our clinic fulfilled the HIS-II criteria for hypnic headache and other possible causes for their headaches were excluded. All patients have been initially treated with flunarizine.
Case reports
Case 1
51 years old man, a 1-year history of headache every night, at variable hours, the headache was very severe and throbbing in character. The headache appears only during sleep, and awaked patient. No autonomic symptoms such as lacrimation, ptosis, rhinorrhoea, photophobia, or phonophobia were noted. The physical and neurological examinations were normal. Brain MRI was normal. Flunarizine 2,5 mg was then administered once daily at bedtime, and the headaches almost completely disappeared.
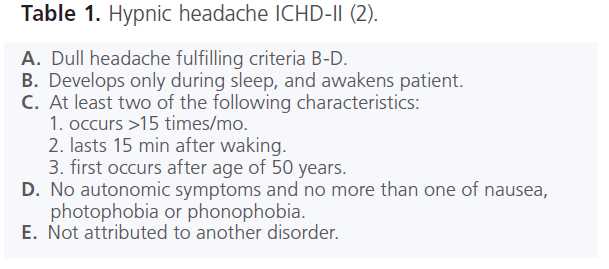
Table 1: Hypnic headache ICHD-II (2).
Case 2
A 57-year-old male with a history of hypertension treated by enalapril complained of recurrent headache attacks that woke twice a week. The pain was dull frontotemporal, bilateral, of mild intensity, and occurred reliably about 4 o’clock. During the headaches there were no autonomic or focal neurologic signs. He had no symptoms during the day. The examination and a brain MRI were absolutely normal. Flunarizine was started and was effective in relieving headache.
Case 3
A 67-year-old woman was evaluated because dull headache attacks for 6 month occurring nearly every night and starting about 60 min after sleep onset. The pain was holocranial and intense. No autonomic symptoms were reported. Neurological, physical examination and MRI were absolutely normal. The duration of headache was 15-30 min. Following flunarizine 2,5 mg previous sleep time, the symptomathology completely released.
Case 4
A 63-year-old woman was admitted to our outpatient clinic. She complained of severe nightly non-pulsating headache holocranial attacks without any autonomic symptoms or nausea or vomiting. The attacks were 4-6 per month for 11 month at the time of evaluation. The neurological examination and MRI scan of the brain were normal. She became asymptomatic with flunarizine 5 mg per night.
Case 5
Male, 52 years old, with 2 years of throbbing headache that invariably occurred at 3 a.m. and lasted for 30 min. The pain was referred to be bitemporal regions, and was of moderate intensity. All studies including brain MRI and analyses were normal. Flunarizine 2,5 mg/day caused a improvement in the frequency of headache, and no other medication has brought any benefit.
Case 6
Female, 74 years old with 1 year history of dull right unilateral headache that waked the patient every night, about 1 hour after sleep onset. There were not any autonomic symptoms. Brain MRI and physical and neurological evaluation were absolutely normal. Flunarizine 2,5 mg per night initially reduce the frequency, but required flunarizine 10 mg without improve, then she was treated with indomethacin becoming asymptomatic.
Discussion
HH is a rare recurrent headache that occurs strictly during sleep, and is usually a late onset headache. Although frequency of headache, location and quality of pain are variable among the patients, is always similar in each patient. It is mandatory to exclude secondary causes in HH patients because of wake pattern headache. Some authors have shown that the onset of HH attacks is associated with REM sleep in almost all patients (3, 7, 8).
We report six patients fulfilling the diagnostic criteria HISII for HH treated with flunarizine. In the literature different drugs have been used in HH treatment, lithium is the most frequently used and also showed the best average efficacy (3). However, flunarizine, caffeine and indomethacin could obtain similar ratios, and they have a better adverse effect profile (3, 6-10). In our opinion flunarizine is a very good alternative in the prophylactic treatment of HH. The efficacy of flunarizine was moderate only in one of our patients. According to our patients evolution we think that flunarizine is a good therapeutic option for HH, and the low doses (2,5 mg night) could be enough.
2104
References
- Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders, 2nd edn. Cephalalgia 2004; 24 Suppl. 1: –-160.
- Evers, S., Goadsby, PJ. Hypnic headache: Clinical features, pathophysiology, and treatment. Neurology 2003; 60: 90–-909.
- Peatfield, RC., Mendoza, ND. Posterior fossa meningioma presenting as hynic headache. Headache 2003; 43: 1007-1008.
- Moon, H-S., Chung, C-S., Kim, H-Y., Kim, D-H. Hypnic headache syndrome: report of a symptomatic case. Cephalalgia 2003; 23: 67–- 674.
- Perez-Martinez, DA., Berbel-Garcia, A., Puente-Munoz, AI., Saiz- Diaz, RA., de Toledo-Heras, M., Porta-Etessam, J., Martinez-Salio, A. Cefalea hípnica: un nuevo caso. Rev Neurol. 1999; 28: 883-884.
- Pinto, CAR., Fragoso, YD., Souza Carvalho, D., Gabbai, AA. Hypnic headache syndrome: clinical aspects of eight patients in Brazil. Cephalalgia 200 ; 2;: 82–-827.
- Evers, S., Rahmann, A., Schwaag, S., Lüdemann, P., Husstedt, I-W. Hypnic headache – the first German cases including polysomnography. Cephalalgia 2003; 23: 2–-23.
- Morales-Asin, F., Mauri, JA., Iñiguez, C., Espada, F., Mostacero, E. The hypnic headache syndrome: report of three new cases. Cephalalgia 1998; 18: 15–-158.
- Ivañez, V., Soler, R., Barreiro, P. Hypnic headache syndrome: a case with good response to indomethacin. Cephalalgia 1998; 18: 22–-226.