Key words
ESBL, AmpC β-lactamases, nosocomial, Eastern India.
Introduction
The production of a plethora of newer beta-lactamases like extended spectrum beta lactamases (ESBLs), Amp-C enzymes, and carbapenemases by gram negative bacteria is the major defense mechanism against the beta lactam antibiotics [1]. ESBLs, first reported in 1983 from Germany, are plasmid - mediated enzymes capable of hydrolyzing a wide variety of β-lactams, and having no detectable activity against cephamycins and imipenem, but are inhibited by ßlactamase- inhibitors such as clavulanate and tazobactam [2]. They have evolved from mutation in TEM, SHV, CTX-M and OXA enzymes, which are present mainly in Enterobacteriacae isolates (majority being Klebsiella pneumoniae, Klebsiella oxytoca and Escherichia coli) [3].
AmpC β-lactamases are cephalosporinases conferring resistance to cephalosporins in the oxyimino group, 7-α-methoxycephalosporins and poorly inhibited by clavulanic acid or β- lactamase Inhibitor / β-lactam combinations [4]. They have been reported in E.coli, Klebsiella pneumoniae, Salmonella spp, Citrobacter freundii, Enterobacter aerogenes and Proteus mirabilis [4].
Over the last few years, numerous outbreaks of infections with organisms producing ESBLs and AmpC β-lactamases have been reported with increasing trend from various parts of India and worldwide thereby increasing clinical concern. However, there is a paucity of such data from eastern India. The routine susceptibility tests performed by clinical laboratories fail to detect these strains, which may lead to inappropriate and unsuccessful therapy of the patient and unnecessary use of the drugs accelerating the ongoing problem.
The present study was designed in a tertiary care hospital of eastern India to generate data on the occurrence of ESBL and AmpC producing gram negative bacilli and analyse their antibiotic susceptibility pattern.
Material and Methods
Clinical isolates: A total of 180 consecutive, non-repetitive gram-negative clinical isolates over a period of four months (January to April, 2011) were obtained from clinical specimens of urine, wound, blood, tracheal aspirates, tracheostomy suction catheter, endotracheal tube, endotracheal aspirates, central venous catheter or sputum from the patients with suspected nosocomial infections. Isolation and identification of the causative bacteria were performed using standard methodology [5].
Antibiotic susceptibility testing [6]: The isolates were subjected to antimicrobial susceptibility testing using Kirby-Bauer disk diffusion method following CLSI guidelines, using commercially available 6mm discs (HIMEDIA,Mumbai,India) cefoxitin (30μg), cefotaxime (30μg), ceftriaxone (30μg), ceftazidine (30μg), cefipime (30μg),cefpodoxime (10μg), imipenem (10μg), aztreonam (30μg), amoxycillin/clavulinate (20/10μg), amikacin (30μg), pipercillin (100μg), ciproploxacin (5μg), gatifloxacin (5μg) and cotrimoxazole (1.25/23.75μg) on Mueller Hinton agar plate.
Screening for ESBLs and AmpC β-lactamases: According to CLSI guidelines (2007), those with a zone inhibition of ≤27mm with cefotaxime, ≤25mm with ceftriaxone, ≤22 mm with ceftazidime, ≤17mm with cefpodoxime or ≤27mm with aztreonam were considered potential ESBL producers and further proceeded for confirmation.
Isolates showing resistance or reduced sensitivity to cefoxitin, cefotaxime, ceftriaxone, ceftazidime, cefpodoxime or aztreonam and sensitive to cefepime were considered as a screen positive AmpC producer and subjected to AmpC disk test.
Detection of ESBLs and AmpC β-lactamases
1. Double disk synergy test [7]: A 0.5 McFarland of test isolate was swabbed on Mueller-Hinton agar plate and 30 μg antibiotic disks of ceftazidime or ceftriaxone or cefotaxime were placed on the plate, 20 mm (center to center) from the amoxicillin/clavulanate (20μg/10μg) disk and incubated at 35°C for 18-24 hours. A clear extension of the edge of ceftazidime or ceftriaxone or cefotaxime inhibition zone toward the disk containing clavulanate is interpreted as synergy, indicating the presence of an ESBL. (Figure 1)

Figure 1: Double disk synergy test [Amoxyclav(L) with ceftazidime(R)].
2. Combined disk test (Phenotypic confirmatory test) [6]: A disk of cefotaxime/ceftazidime (30μg) alone and a disk of ceftazidime + clavulanic acid (30μg/10μg)/ cefotaxime + clavulanic acid (30μg/10μg) were placed independently, 30mm apart, on a lawn culture of 0.5 Mc-Farland opacity of the test isolate on Mueller Hinton Agar (MHA) plate and incubated for 18-24 hours at 35°C. An increase of ≥5mm zone of inhibition diameter around the ceftazidime/ clavulanic acid and cephotaxime/clavulanic acid in comparison to ceftazidime and cefotaxime alone respectively confirmed ESBL production. (Figure 2)

Figure 2: Positive Combined disk test[Ceftazidime. (upper) & Ceftazidime /clavulanic acid (Lower)].
3. Minimal Inhibitory Concentration (MIC) Reduction test (Agar dilution method) [6]: MIC reduction test was done to all screening positive ESBL isolates. The ranges of concentration of antimicrobials tested were as follows: cefotaxime and ceftazidime: 1μg/ ml to 128μg/ml cephotaxime-clavulanic acid and ceftazidime- clavulanic acid: 0.25/4 μg/ml to 128/4μg/ml. A ≥ 3 twofold reduction in MIC of these strains when tested in combination of cefotaxime -clavulanic acid or ceftazidime-clavulanic acid as compared to MIC for cefotaxime or ceftazidime alone, confirmed that the strains were ESBL producer.
4. AmpC disk test [8]: Sterile disk (6 mm) moistened with sterile saline (20 μl) and inoculated with several colonies of test organism was placed beside a cefoxitin disk (almost touching) on the MHA plate lawned with a culture of E. coli ATCC 25922 and incubated overnight at 35°C. A positive test appeared as a flattening or indentation of the cefoxitin inhibition zone in the vicinity of the test disk [9]. A negative test had an undistorted zone. (Figure 3 & 4)
Figure 3: AmpC disk test showing indentation.
Figure 4: AmpC disk test showing flattening.
Quality control: Every batch of media prepared was checked for sterility for 24 hours. CLSI reference strains of ESBL positive K.pneumoniae ATCC 700603 and ESBL negative E.coli ATCC 25922 were included in the study.
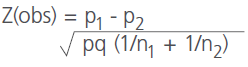
Statistical Analysis [10]: Significance between the resistance level of various drugs in ESBL and non-ESBL, AmpC and non-AmpC isolates was performed using the Proportion test( Z).
where p1 = Proportion of ESBL or AmpC isolates showing resistance to individual antimicrobial
p2 = Proportion of non-ESBL or non-AmpC isolates showing resistance to individual antimicrobial
n1= No. of ESBL or AmpC isolates
n2= No. of non-ESBL or non-AmpC isolates
p= n1p1 + n2p2 / n1 + n2
q= 1- p.
obs= observed value of Z.
At 5% level, tabulated or expected value of Z for both sided test is 1.96. So, if the observed value of Z is more than the tabulated value then it is said to be significant at 5% level and the P value is < 0.05.
Results
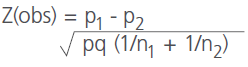
Of the 180 non-repetitive gram-negative isolates that were included in the study, the isolated gram-negative organisms were E.coli (n=69),Klebsiella spp.(n=65),P.aeruginosa (n=23), Proteus spp.(n=5),Citrobacter spp. (n=3), Enterobacter spp. (n=2) and Acinetobacter spp.(n=13). The number of potential ESBL and AmpC β-lactamase producers detected by the screening test were 80 and 59 respectively.
Detection of ESBLs
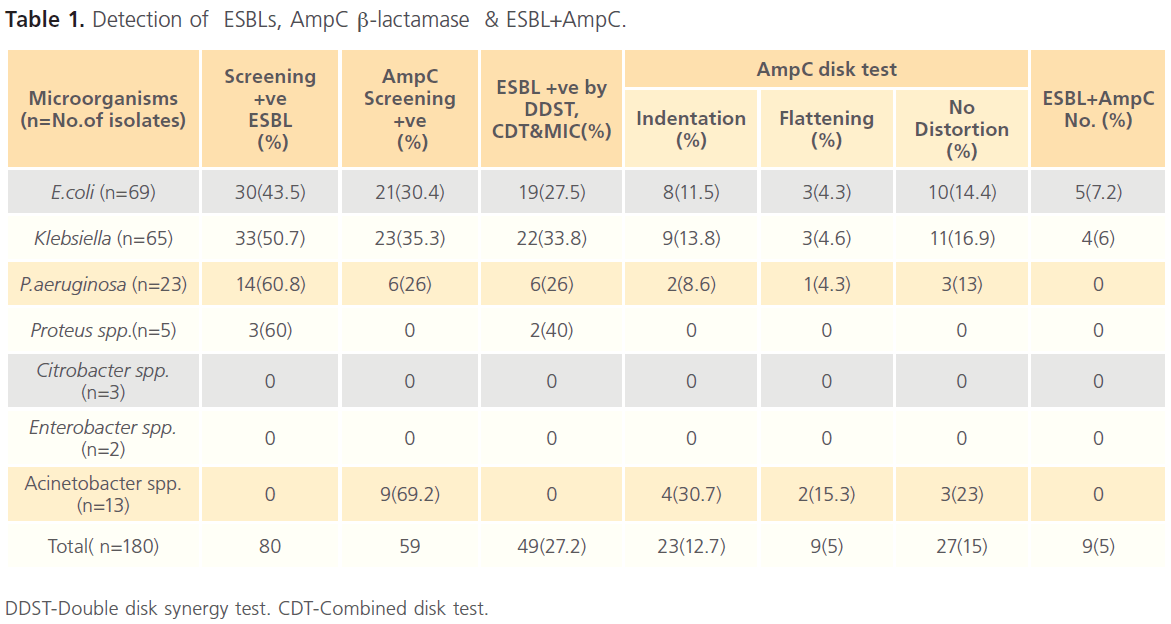
ESBL production was observed in 49(27.2%) isolates by double disk synergy , combined disk tests and MIC reduction test from 80 screening positive isolates, and amongst these 27.5%, 33.8%, 26% and 40% isolates were E.coli, Klebsiella spp., P.aeruginosa and Proteus spp respectively.(Table 1)
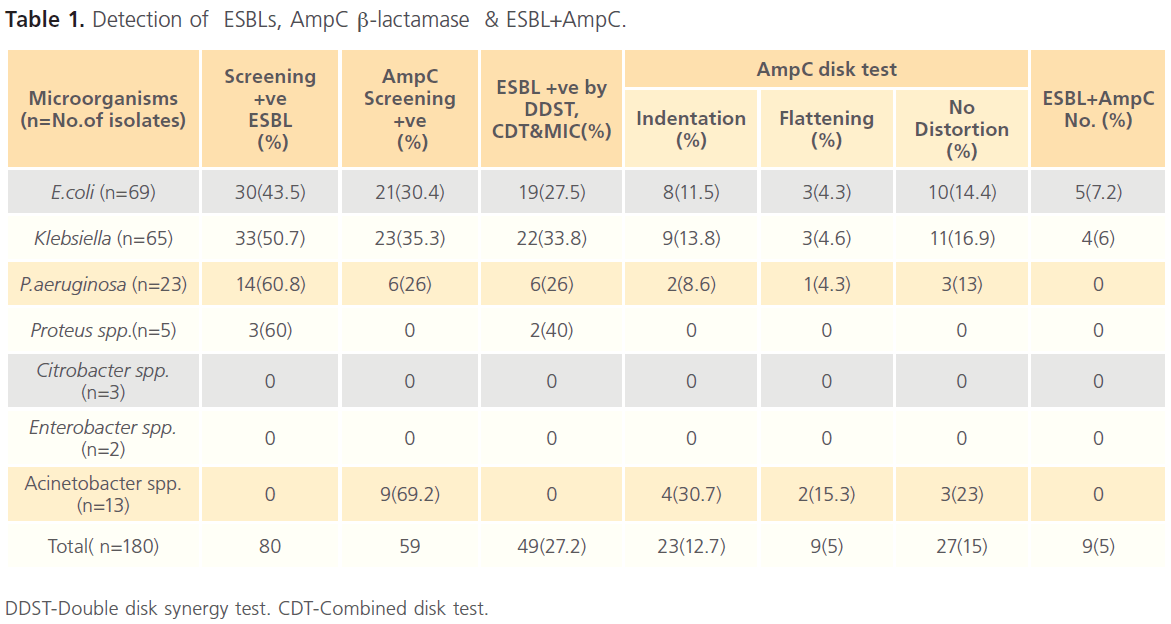
Table 1: Detection of ESBLs, AmpC β-lactamase & ESBL+AmpC.
Detection of AmpC β-lactamases
AmpC disk test detected AmpC enzymes in 32(17.7%) isolates with the highest incidence in Acinetobacter spp (46.1% ) followed by Klebsiella spp (18.4%), E.coli (15.9%) and P.aeruginosa (13%). Indentation indicating strong AmpC producer was observed in 23 isolates whereas flattening (weak AmpC) in 9 isolates [9]. (Table 1).
Detection of ESBLs in presence of AmpC β-lactamases
This study demonstrated the co-existence phenotype of both ESBLs and AmpC in 9(5%) isolates of which 5(7.2%) and 4(6%) isolates were E.coli and Klebsiella spp respectively. (Table 1)
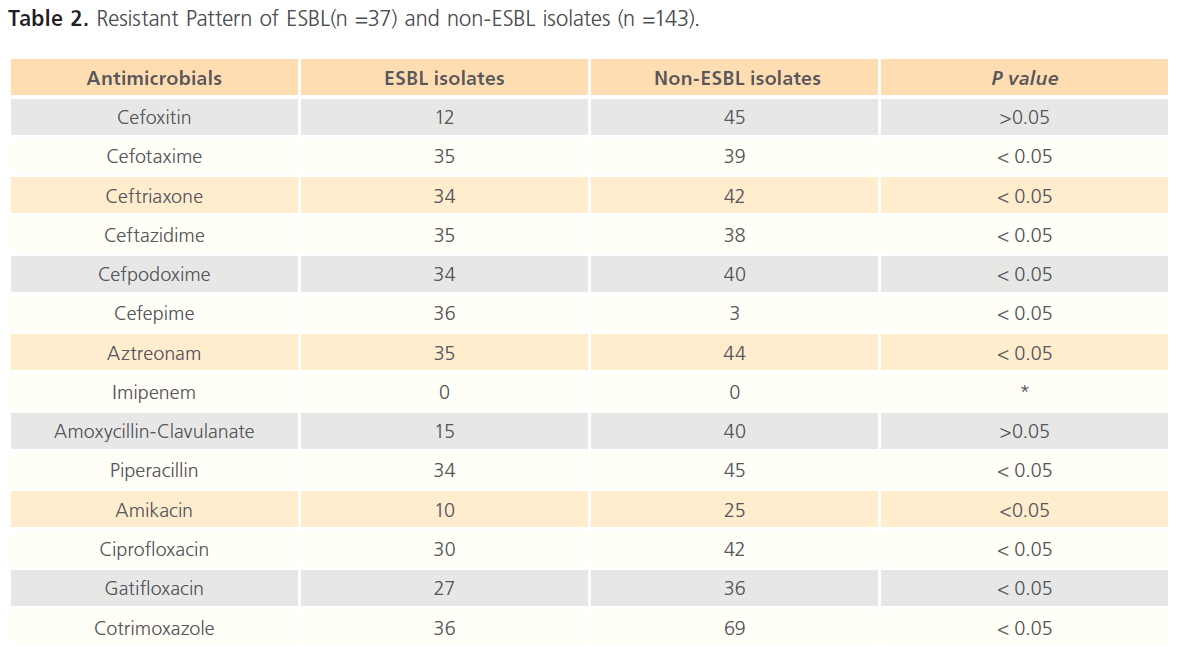
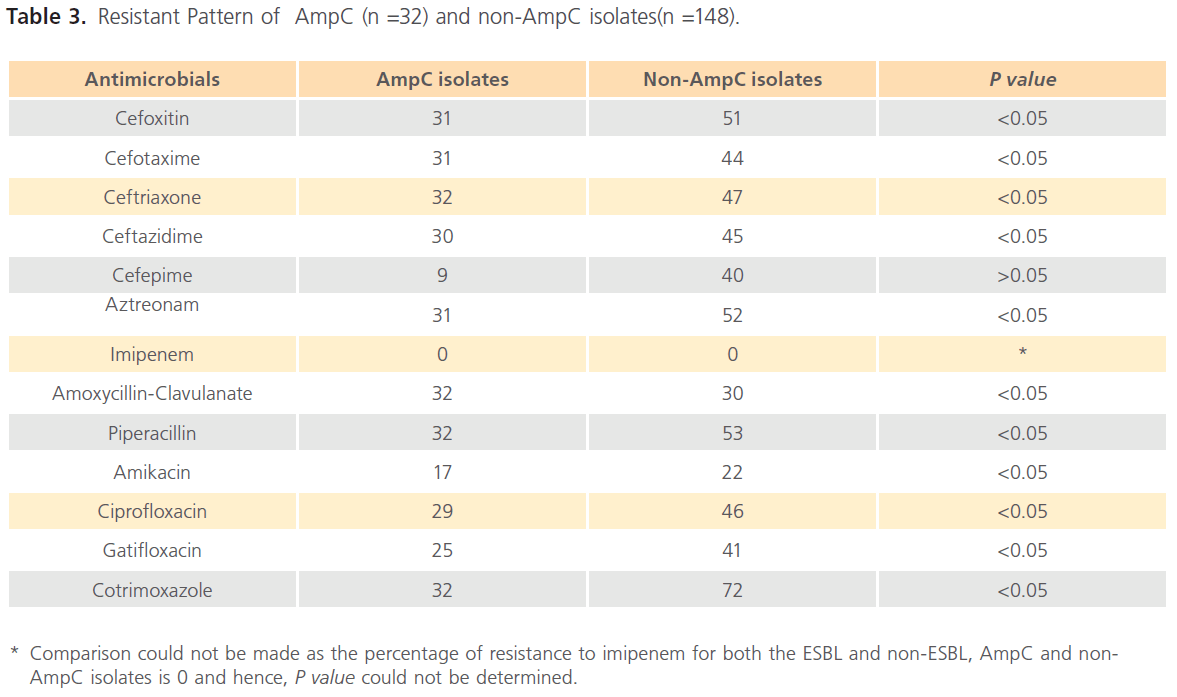
The comparison of anti-microbials resistance for ESBL and non-ESBL, AmpC and non-AmpC isolates producing strains is shown in (Table 2 & 3).
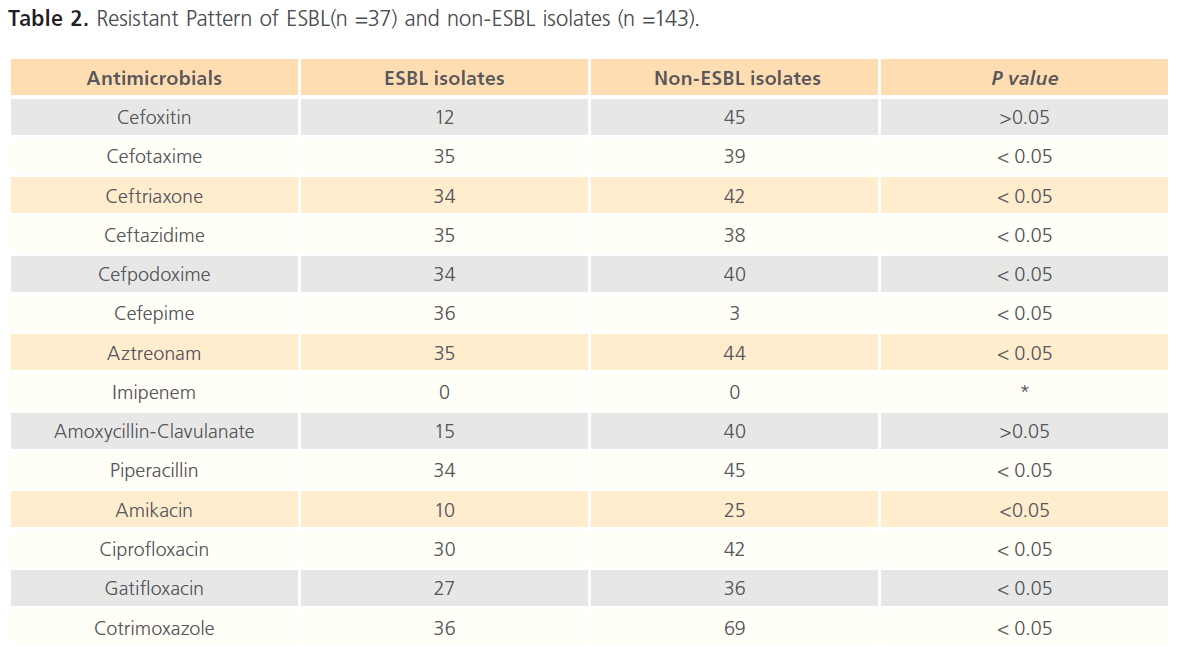
Table 2: Resistant Pattern of ESBL(n =37) and non-ESBL isolates (n =143).
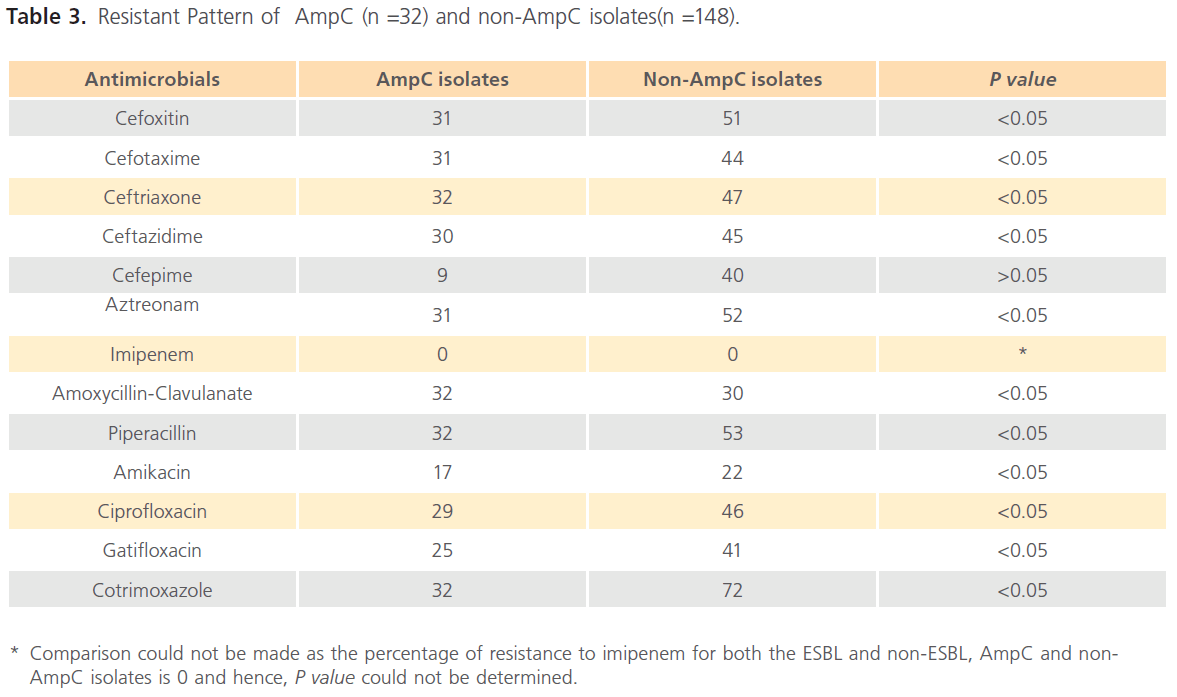
Table 3: Resistant Pattern of AmpC (n =32) and non-AmpC isolates(n =148).
Discussion
The incidence of ESBLs (27.2%) in the present was lower in comparison to reports from different parts of the country (28% to 84%) [11-13]. This might be due to judicious usage of extended spectrum cephalosporins and adopting appropriate infection-control measures in our hospital.
The occurence of AmpC β-lactamases (17.7%) in this study was higher than that of Singhal S et al (8%) and Hemalatha V et al (9.2%) but was lower than the various documented figures in India [9,14-17].
The co-existence of ESBL and AmpC found in 7.2% E.coli and 6.1% of Klebsiella spp. could be due to dissemination of plasmid encoding both AmpC and ESBL enzymes among Enterobacteriaceae and thus might give false negative tests for the detection of ESBLs. In such situations, it is desirable to develop an ESBL detection test that includes a substrate displaying a higher degree of resistance to AmpC enzymes like cefepime. Singhal S et al observed the co-existence phenomenon in two (1%) isolates (one each of Klebsiella spp. and E. coli) and Sinha P et al in 8% of the isolates [9,16].
We observed that the MIC of cephotaxime and ceftazidime against the ESBL producers ranged between 32 and ≥128μg/ ml and in presence of beta lactam inhibitors (clavulanic acid), the MIC of most ESBL isolates ranged between 2 and 32μg/ ml showing ≥3 twofold reduction.
Among the third generation cephalosporins, resistance to ceftazidime and cefotaxime by the ESBL producers was 94.59%, and hence Ceftazidime and cefotaxime were equally effective in detecting ESBL producers. Cormican MG et al showed maximum ESBL detection by ceftazidime [18]. Other workers have reported maximum ESBL detection by ceftriaxone followed by cefotaxime and ceftazidime [19].
Double disk synergy test (DDST) showed 100% concordance with combined disk test for ESBL detection. Tsering DC et al revealed similar report [20]. Datta P et al , Thomson et al and Vercauteren E et al found 96% ,79% and 93% sensitivity rate for the DDST respectively [21-23].
This study reflected that multidrug resistance was significantly (P < 0.05) higher in ESBL and AmpC β-lactamase producers than non-ESBL and non- AmpC producers. Resistance to cefoxitin(32.4%),3rd( 93.24%) and 4th(97.29 %) generation cephalosporins, and aztreonam (94.59 %) were observed in most of the ESBL producers, whereas resistance to cefoxitin(96.87%) ,3rd(97.65%) and 4th (28.12 %) generation cephalosporins, and aztreonam(96.87%) were shown by AmpC isolates. Interestingly, ESBL and AmpC producers also showed concurrent resistant to amikacin (27.02%and 53.12%), ciprofloxacin (81.08% and 90.62%), gatifloxacin (72.97% and 78.12%) and cotrimoxazole (97.29% and100 %) respectively. Similar finding was reported by Manchanda V et al , Datta P et al and Jain A et al [15,21,24]. However, all the ESBL and AmpC producing isolates were sensitive to Imipenem, thereby reiterating the continued efficacy of carbapenems as the first line agents for treatment of nosocomial infections caused by Enterobacteriaceae producing ESBL and AmpC beta lactamases. Similar data has been published in the MYSTIC Program in Europe and the US (1997-2004) and other studies which claim that worldwide 99.9% of ESBL and AmpC β-lactamases producing Enterobacteriaceae remain susceptible to carbapenems [25].
To conclude, 27.2% and 17.7% of ESBL and AmpC producers were detected respectively in our hospital. Double disk synergy and combined disk tests were equally effective for ESBL detection. AmpC disk test is simple, easy to perform and interpret requiring less expertise for the rapid detection of AmpC isolates. Adoption of this test would make it possible to learn more about the clinical implications of AmpC ß-lactamases and to contain the spread of organisms possessing this resistance mechanism. The limitation of this study was that advance molecular methods could not be accessed due to lack of infrastructure.
Acknowledgment
Authors acknowledge the Department of Statistics, All India Institute of Health and Hygiene, Kolkata and Shri M Jaydeba Singh for statistical analysis.
150
References
- Medeiros AA (1997) Evolution and dissemination of β-lactamases accelerated by generations of β-lactam antibiotics. Clin Infect Dis 24:19–45.
- Bradford PA (2001) Extended spectrum beta-lactamases in the 21st century: characterization, epidemiology and the detection of this important resistance threat.ClinMicrobiol Rev 14:933-951.
- Livermore DM (1995) β-lactamases in laboratory and clinical resistance. ClinMicrobiol Rev 8:557–584.
- Philippon A, Arlet G, Jacoby GA (2002) Plasmid-determined AmpC-type β-lactamases Antimicrob Agents Chemother 46 (1): 1–11.
- Winn WC , Allen SD, Janda WM, Koneman EW, Procop GW (2006) Introduction to microbiology part II: Guidelines for the Collection, Transport, Processing, Analysis and Reporting of Cultures from Specific Specimen Sources. In Koneman’s Color Atlas and Textbook of Diagnostic Microbiology, 6th ed.Philadelpjia: Lippincott William & Wilkins. 67-105p.
- Wayne PA (2010) Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Twentieth Informational Supplement M100-S20.
- Jarlier V, Nicolas MH, Fournier G, Philippon A (1988) Extended spectrum beta-lactamases conferring transferable resistance to newer beta-lactam agents in Enterobacteriaceae: hospital prevalence and susceptibility patterns. Rev Infect Dis 10:867-878.
- Black JA, Moland ES, Thomson KS (2005) AmpC disk test for detection of plasmid-mediated AmpC β-lactamases in Enterobacteriaceae lacking chromosomal AmpC β-lactamases. J ClinMicrobiol 43:3110– 3113.
- Singhal S, Mathur T, Khan S, Upadhyay DJ, Chugh S et al (2005) Evaluation of methods for AmpC β lactamase in gram negative clinical isolates from tertiary care hospitals. Ind J Med Microbiol 23:120-124.
- Mahajan BK (1999) Sampling variability and significance. In: Methods in Biostatistics. New Delhi: Jaypee Brothers. 115-129p.
- MetriBasavaraj C, Jyothi P, PeerapurBasavaraj V (2011) The Prevalence of ESBL among Enterobacteriaceae in a Tertiary Care Hospital of North Karnataka, India. J ClinDiagn Res 5(3):470-475.
- ChaudhuriBN,Rodrigues C, Balaji V, Iyer R, Sekar U et al (2011) Incidence of ESBL Producers amongst Gram-negative bacilli Isolated from intra-abdominal Infections across India (Based on SMART Study, 2007 Data). J Assoc Physicians Ind 59:287-292.
- Das A, Ray P,Garg R, Kaur B (2001) Extended spectrum beta lactamase production in gram-negative isolates from cases of septicaemia. In:Proceedings of Silver Jubilee Conference. New Delhi: All India Institutes Of Medical Sciences. 21-25p.
- Hemalatha V, Padma M, Sekar U, Vinodh TM, Arunkumar AS (2007) Detection of Amp C beta lactamases production in Escherichia coli &Klebsiella by an inhibitor based method. Indian J Med Res 126: 220- 223.
- Manchanda V, Singh NP (2003) Occurrence and detection of AmpC β lactamases among gram negative clinical isolates using a modified three dimensional test at Guru TeghBahadur Hospital, Delhi, India. J AntimicrobChemother 51: 415-8.
- Sinha P, Sharma R, Rishi S, Sharma R, Sood S et al (2008) Prevalence of extended spectrum beta lactamase and AmpC beta lactamase producers among Escherichia coli isolates in a tertiary care hospital in Jaipur .Indian J Path Microbiol 51: 367-9
- Patel MH,Trivedi GR, Patel SM, Vegad MM (2010) Antibiotic susceptibility pattern in urinary isolates of gram negative bacilli with special reference to AmpC β-lactamase in a tertiary care hospital. Urology Annals 2(1):7-11.
- Cormican MG, Marshall SA, Jones RN (1996) Detection of extended spectrum beta-lactamase (ESBL)-producing strains by the Etest ESBL screen. J ClinMicrobiol 34:1880-9.
- Coudron PE, Moland ES, Sanders CC (1997) Occurrence and detection of ESBL in members of the family Enterobacteriacieae at a Veterans Medical Center . J ClinMicrobiol 35: 2593-7.
- Tsering DC, Das S,Adhiakari L, Pal R, Singh TSK (2009) Extended spectrum beta-lactamase detection in gram-negative bacilli of nosocomial origin. J Glob Inf Dis 1:87-92.
- Datta P, Thakur A, Mishra B, Gupta V (2004) Prevalence of clinical strains resistant to various β-lactamases in a tertiary care hospital in India. Jpn J Infect Dis 5: 146-9.
- Thomson KS, Sanders CC. 1992. Detection of extended–spectrum beta-lactamases in members of the family Enterobacteriaceae: comparison of the double-disk and three-dimensional tests. Antimicrob Agents Chemother. 36:1877-1882.
- Vercauteren E, Leven M, Gossens H (1997) Comparison of screening mrthods for the detection of ESBLs and their prevalence amongst blood isolates of E.coli and Klebsiella spp. in a Belgian Hospital. J ClinMicrobiol 35:2191-7.
- Jain A ,Mondal R (2007) Prevalence & antimicrobial resistance pattern of extended spectrum beta-lactamase producing Klebsiellaspp isolated from cases of neonatal septicaemia. Indian J Med Res 125:89- 94
- Goossens H, Grabein B (2005) Prevalence and antimicrobial susceptibility data for. Extended spectrum beta lactamase and AmpC producing Enterobacteriaceae from the MYSTIC program in Europe and the US (1997-2004).DiagnMicrobiol Infect Dis 53:257-264