Franca Bilora1*, Lucia Sarolo1, Fabio Pomerri2 and Paolo Prandoni1
1Department of Cardiovascular Sciences, University of Padua, Italy
2Institute of Radiology, University of Padua, Italy
Corresponding Author:
Franca Bilora i, Vascular Medicine Unite
University of Padua, Via Giustiniani 2, 35128 Padova , Italy
Tel: +39 049 8212650
Fax: +39 049 8213108
E-mail: franca.bilora@sanita.padova.it
Syncope is a common cause of hospitalization, and its frequency increases with age. Its prognosis is largely unpredictable, pending the origin of the sudden loss of consciousness. We report a case of an old woman affected by severe chronic heart failure, who died soon after the development of an episode of syncope, which was eventually attributed to pulmonary embolism. Anticoagulant therapy, promptly instituted, was ineffective. In the differential diagnoses of syncope, pulmonary embolism should always be considered, especially in old patients with risk factors for venous thromboembolism such as a severe heart failure. In patients with high risk of death according to the widely adopted risk stratifications score, aggressive therapy may be considered also in elderly people to prevent unfavourable outcomes.
Keywords
Syncope, Sudden death, Pulmonary embolism
Introduction
Syncope is defined as a transient loss of consciousness that has a rapid onset, short duration and spontaneous recovery, and is supposedly due to temporary cerebral hypoperfusion. According to recent classifications, syncope can be neurally-mediated, due to orthostatic hypotension or of cardiovascular origin (i.e., arrhythmias, structural cardiovascular diseases or pulmonary embolism [PE]) [1,2]. It is a common case of hospitalization in the Unites States. According to the results of a recent observational cross-sectional study, the hospital mortality rate for syncope is low (0.28%) [3].The likelihood of death was found to increase with age, becoming more prominent after the age of 40, and was found to be associated with the severity of the comorbidity index, the odds ratio (OR) of death being 1.39 (95% CI, 1.20-1.62) in patients with moderate index, and 4.14 (95% CI, 3.05-5.61) in those with severe one [3]. We report a case of an 87 years woman with chronic heart failure, who developed an orthostatic syncope caused by pulmonary embolism. Soon after recovery from the episode of consciousness, she was found to be hemodynamically stable. In spite of prompt diagnosis, she died few hours after the institution of full-dose anticoagulation.
Case Report
An 87 years old woman presented to the Emergency Department of the University Hospital of Padua after experiencing an orthostatic episode of syncope associated with vomit. She had had a similar episode one month earlier, which had remained unexplained. No fever, cough, dyspnoea, chest pain, palpitations or fainting prior to the event.
The patients had a history of remote colon cancer, acute myocardial infarction and symptomatic bradycardia requiring the positioning of an indwelling pace maker. Recently, she had suffered from recurrent episodes of heart failure requiring hospital admission and diuretic treatment. She had an impaired cognitive state and a mild renal insufficiency. The patient’s supine blood pressure was 200/95 mmHg, heart rate 100 arrhythmic. She presented pulmonary crackles, moderate mitralic systolic murmur and bilateral leg edema. Blood tests showed a mild renal and liver insufficiency, normal troponin I level and remarkably elevated values of pro-BNP and D-dimer value. Overall, she was regarded as hemodynamically stable. However, the simplified PESI score (n=5) placed patients at a substantial risk for unfavorable adverse events, had a PE been detected [4].
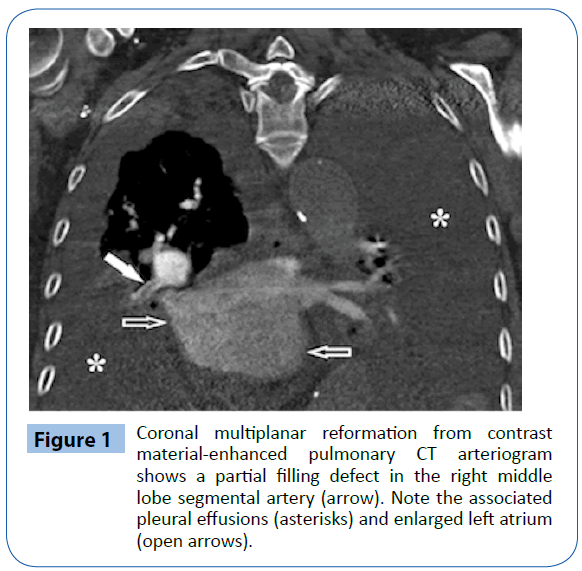
The electrocardiography revealed a (previously unknown) atrial fibrillation and a well working pace maker. The leg veins ultrasonography excluded deep vein thrombosis, the chest X-ray evidenced bilateral pleural effusion and an enlarged heart. A CT pulmonary angiography, promptly performed, showed a thrombotic defect in the right middle lobe segmental artery (Figure 1).
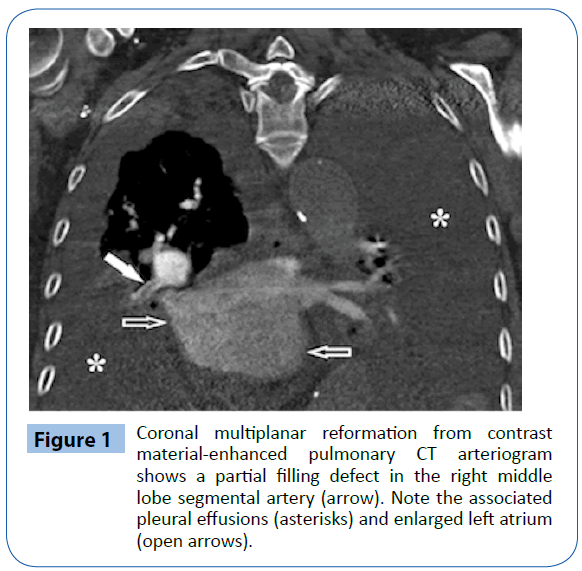
Figure 1: Coronal multiplanar reformation from contrast material-enhanced pulmonary CT arteriogram shows a partial filling defect in the right middle lobe segmental artery (arrow). Note the associated pleural effusions (asterisks) and enlarged left atrium (open arrows).
Soon after diagnosis, she was given therapeutic doses of lowmolecular- weight heparin. While on treatment, she had a cardiac arrest few hours later. The cardiopulmonary resuscitation was ineffective, and she died.
Discussion
Syncope is a well known and quite common manifestation of PE, and its prognosis is largely dependent on the timeliness of diagnosis and treatment [1,2]. In our patients, the loss of consciousness that prompted hospital admission had been preceded by a similar episode one month earlier, which had unfortunately remained without explanations.
When the patient was admitted to our department we promptly suspected PE because of the presence of a number of well known risk factors for venous thromboembolism (including old age, chronic heart failure and poor mobilization) and the remarkable high values of pro-BNP and D-dimer. Our suspicion was confirmed by a CT pulmonary angiography, so that we started treatment with full dose low-molecular weight heparin. In spite of this, after few hours she underwent a fatal cardiac arrest. Are there lessons to be learned from this case?
Syncope is a serious manifestation of PE. Firstly, it places patients at risk of death because of the unpredictable consequences of the loss of consciousness. Secondly, it generally represents the manifestation of either anatomical or clinically severe PE. Indeed, the simplified PESI score (n=5) qualified our patient as being at a substantial risk for unfavorable outcome, although the blood pressure was high [4]. Whether implementing or not aggressive (i.e., thrombolytic) therapy in patients with PE and high risk of adverse events in spite of stable clinical condition is a matter of debate, as a recent major randomized clinical trial showed that the benefit/risk of such strategy may not be favorable, especially in patients older than 75 [5]. However, physicians should be alerted and consider this option whenever there are not contraindications other than elderly age to thrombolysis. Patients may be offered adjusted-dose intravenous unfractionated heparin instead of low-molecular-weight heparin in order to achieve a rapid anticoagulation, and should be carefully monitored, so that the decision whether continuing anticoagulation alone or associate it with a course of a thrombolytic therapy is timely taken.
7722
References
- Task Force for the Diagnosis and Management of Syncope; European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA); Heart Failure Association (HFA); Heart Rhythm Society (HRS), Moya A, Sutton R, Ammirati F, Blanc JJ, et al. (2009) Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J 30: 2631-2671.
- Strickberger SA, Benson DW, Biaggioni I, Callans DJ, Cohen MI, Ellenbogen KA et al. (2006) AHA/ACCF Scientific Statement on the evaluation of syncope. Circulation 113: 316-328.
- Alshekhlee A, ShenWK, Mackall J, ChelimskyTC (2009) Incidence and mortality rates of syncope in the United States. Am J Med 122: 181-188.
- Jiménez D, Aujesky D, Moores L, Gómez V, Lobo JL, et al. (2010) Simplification of the pulmonary embolism severity index for prognostication in patients with acute symptomatic pulmonary embolism. Arch Intern Med 170: 1383-1389.
- Solbiati M, Casazza G, Dipaola F, Rusconi AM, Cernuschi G, et al. (2015) Syncope recurrence and mortality: a systematic review. Europace 17: 300-308.