Keywords
Recurrent stroke; Hemorrhagic stroke; Intracerebral hemorrhage
Introduction
South Korea has changed drastically over a period of two decades, and the first change is the incredible growth of the economy; the gross domestic product per capita in 2014 was 24,565 USD, and it increased by 80% between 1997 and 2014. The second change is that South Korea has become an aging society over the past 20 years, and it is widely accepted that the country will become a hyperaging society. Recent changes in lifestyle in both developed and developing countries have altered the average ages of stroke patients, and the increase in socioeconomic expense. The South Korean government has put significant efforts and money into prevent strokes.
Cheonan city, where our hospital is situated at the center of Chungnam (Chungchungnam-do state), is one of the major cities in Korea along with the capital Seoul. As a transportations hub, it has become rapidly industrialized in the past two decades, and it is also one of the few cities in the country in recent years whose population is growing.
The goal of this study was to analyze the age trends for firstever or recurrent stroke onset in the city that has been rapidly growing for the past 19 years and to find the influencing factors of the age trend of stroke.
Methods
We assessed the age trends in stroke incidence from 1997 to 2015 using a total of 12,370 patients, enrolled retrospectively, who had suffered a first-ever or recurrent stroke during the 19 years of the study period. First-ever stroke was defined as the first occurrence (no history of stroke in prior medical records) of rapidly developing signs of focal neurological disturbance of presumed vascular pathogenesis lasting >24 hours [1]. Hemorrhagic stroke (HS) was defined as intracerebral hemorrhage (ICH) and subarachnoid hemorrhage (SAH); ischemic stroke (IS) was defined as thrombotic brain infarction, cardioembolic stroke, and lacunar infarct. To evaluate the differences of proportion of stroke patients and population by age, age were divided into three groups; young age was < 45, middle age was 45-64, and old age was >64.
All patients were diagnosed as having fully clinical strokes, with significant clinical symptoms and signs, and we excluded undetermined and silent strokes (diagnosed by imaging only). The risk factor survey was conducted in the same patients in both 1997 and 2015, and the risk factors assessed were hypertension, diabetes mellitus, previous stroke history, congestive heart failure, atrial fibrillation, chronic obstructive pulmonary diseases, chronic kidney diseases, obesity, current smoking status, and alcohol consumption. Hypertension was defined as systolic blood pressure ≥140 mm Hg and diastolic blood pressure ≥90 mm Hg or use of antihypertension medication. Diabetes mellitus was defined as self-reported previous diabetes mellitus history or use of antidiabetic medications. Body mass index (BMI) was calculated as weight (kg) divided by height (in m) squared, and obesity was defined as above 30 kg/m2. We calculated the trends in mean age of stroke from the annual changes by sex and stroke subtype (ICH and IS) using a regression model: log(rt)=a+bt, where log denotes the natural logarithm and t is the year. The trend b was estimated from the ordinary regression, where a represents the constant and b represents the estimated annual change in age. In addition, to find other factors that affected the stroke age trends, we investigated the national health policy in Chungnam. We defined statistical significance as P< 0.05 and used SPSS version 18.0 for Windows (SPSS Inc, Chicago, IL, USA) for the analyses.
Results
Our hospital data
Table 1 shows the demographic characteristics of the patients from 1996 to 2015; we included a total of 12,370 patients (36% in HS, 64% in IS) with a first-ever or recurrent stroke. The mean age of overall stroke was 63.9 ± 13 years (men: 61.6 ± 13.4, women: 66.3 ± 12.7), and the mean ages of IS and HS were 65.9 ± 12 and 60.2 ± 13 years, respectively. There were no significant changes in the proportions of risk factors over the 19 years.
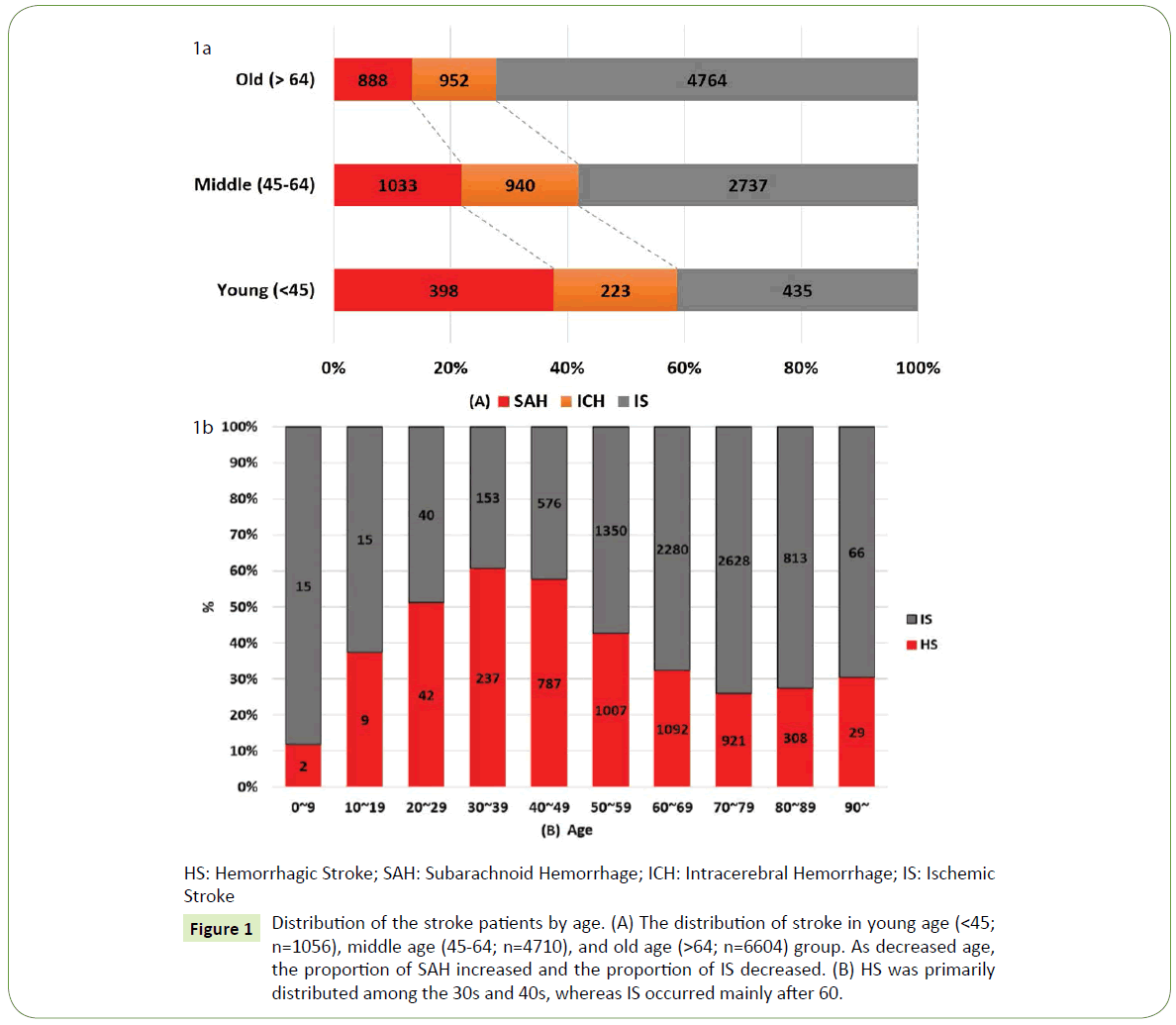
Figure 1 shows the distribution of the stroke patients who had suffered the first-ever or recurrent stroke according to age group. There were 1056 stroke patients in young age (< 45) group, 4710 patients in middle age (45~64), and 6604 patients in old age (>64) group. The ratio of SAH in young age, middle age, and old age group were 38%, 22%, and 13%, respectively. The ratio of IS in young age, middle age, and old age group were 41%, 58%, and 72%, respectively. As decreased age, the proportion of SAH increased. As increased age, the proportion of IS increased (Figure 1A). 61% were HS in 30s patients and 74% were IS in 70s patients. HS has the main distribution in 30s and 40s and IS has the main distribution after 60s (Figure 1B). In the HS with young age, 61.5% were men and 64.1% were SAH.
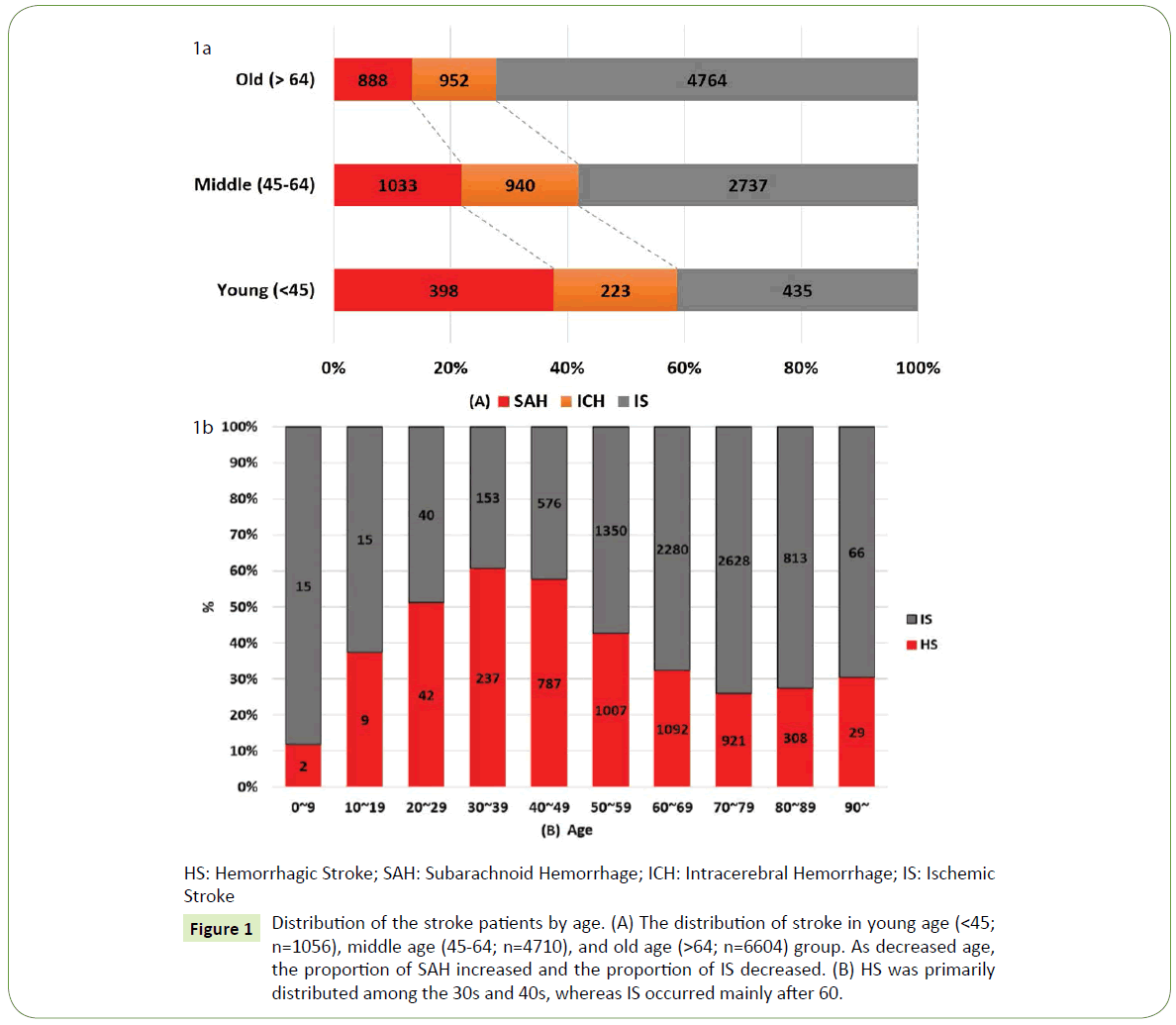
Figure 1: Distribution of the stroke patients by age. (A) The distribution of stroke in young age (< 45; n=1056), middle age (45-64; n=4710), and old age (>64; n=6604) group. As decreased age, the proportion of SAH increased and the proportion of IS decreased. (B) HS was primarily distributed among the 30s and 40s, whereas IS occurred mainly after 60.
Table 2 shows the mean onset ages of and trends in first-ever or recurrent stroke in our hospital between 1996 and 2015. By sex, the mean age of HS onset in men decreased significantly (P< 0.05), by 0.23 year annually, and that of IS increased significantly (P< 0.05), by 0.23 year annually; meanwhile, the mean age of HS onset in women decreased by 0.11 year annually, and that of IS onset increased significantly, by 0.36 year annually. However, the mean age of HS onset showed different trends before and after 2010; the mean age of HS onset before 2010 decreased significantly, by 0.25 year annually and after 2010, increased significantly, by 0.72 year annually (P< 0.05). The mean age of IS onset before 2010 increased significantly by 0.32 year annually and after 2010 increased steadily, by 0.03 year annually.
| YEAR |
Overall |
Hemorrhagic stroke |
Ischemic stroke |
| Onset Age in urban |
Onset Age |
Onset Age |
| Men |
Women |
Total |
Men |
Women |
Total |
Men |
Women |
Total |
| 1997 |
61.07 |
65.04 |
63.12 |
60.43 |
64.98 |
62.79 |
61.43 |
65.07 |
63.30 |
| 1998 |
60.31 |
65.04 |
62.64 |
56.64 |
63.41 |
60.11 |
62.23 |
66.01 |
64.05 |
| 1999 |
61.66 |
65.98 |
63.76 |
59.03 |
66.58 |
63.25 |
62.64 |
65.63 |
63.99 |
| 2000 |
60.96 |
64.94 |
62.92 |
57.45 |
63.81 |
60.92 |
62.29 |
65.53 |
63.80 |
| 2001 |
61.23 |
66.13 |
63.54 |
57.12 |
60.92 |
59.43 |
62.05 |
68.21 |
64.72 |
| 2002 |
61.30 |
65.92 |
63.83 |
59.25 |
63.51 |
61.80 |
62.13 |
67.22 |
64.80 |
| 2003 |
62.44 |
66.02 |
64.22 |
60.04 |
64.17 |
62.38 |
63.44 |
67.23 |
65.18 |
| 2004 |
61.20 |
66.71 |
63.97 |
56.18 |
67.38 |
61.93 |
63.21 |
66.42 |
64.81 |
| 2005 |
61.93 |
66.91 |
64.09 |
57.23 |
63.09 |
60.11 |
63.46 |
68.60 |
65.58 |
| 2006 |
62.96 |
68.89 |
65.82 |
57.93 |
66.16 |
61.91 |
64.37 |
69.65 |
66.92 |
| 2007 |
60.70 |
65.89 |
63.23 |
54.00 |
61.75 |
58.29 |
64.41 |
69.44 |
66.64 |
| 2008 |
62.98 |
65.93 |
64.29 |
58.88 |
60.79 |
59.92 |
64.54 |
69.44 |
66.48 |
| 2009 |
61.62 |
64.83 |
63.32 |
55.77 |
59.43 |
57.99 |
64.90 |
70.04 |
67.32 |
| 2010 |
61.05 |
67.07 |
63.76 |
53.24 |
63.36 |
58.77 |
65.03 |
70.74 |
67.23 |
| 2011 |
62.25 |
64.74 |
63.42 |
53.93 |
59.99 |
57.53 |
66.70 |
71.01 |
68.30 |
| 2012 |
60.29 |
66.87 |
63.37 |
54.31 |
63.28 |
58.92 |
64.31 |
70.19 |
66.86 |
| 2013 |
61.17 |
66.48 |
63.82 |
54.30 |
62.24 |
59.12 |
64.63 |
71.03 |
67.32 |
| 2014 |
62.01 |
68.82 |
65.44 |
56.73 |
65.54 |
61.80 |
65.62 |
72.68 |
68.72 |
| 2015 |
63.05 |
66.78 |
64.88 |
57.47 |
63.41 |
61.22 |
65.12 |
69.88 |
67.07 |
| Trends |
0.05 |
0.09 |
0.07 |
-0.23 |
-0.11 |
-0.14 |
0.23 |
0.36 |
0.27 |
| 97-09 |
0.11 |
0.09 |
0.10 |
-0.21 |
-0.28 |
-0.25 |
0.27 |
0.41 |
0.32 |
| 10-15 |
0.29 |
0.29 |
0.34 |
0.84 |
0.45 |
0.72 |
-0.07 |
0.05 |
0.03 |
for trends <0.05 by a regression model
Table 2: The trends in mean age of first-ever or recurrent stroke onset from 1996 to 2015 by sex.
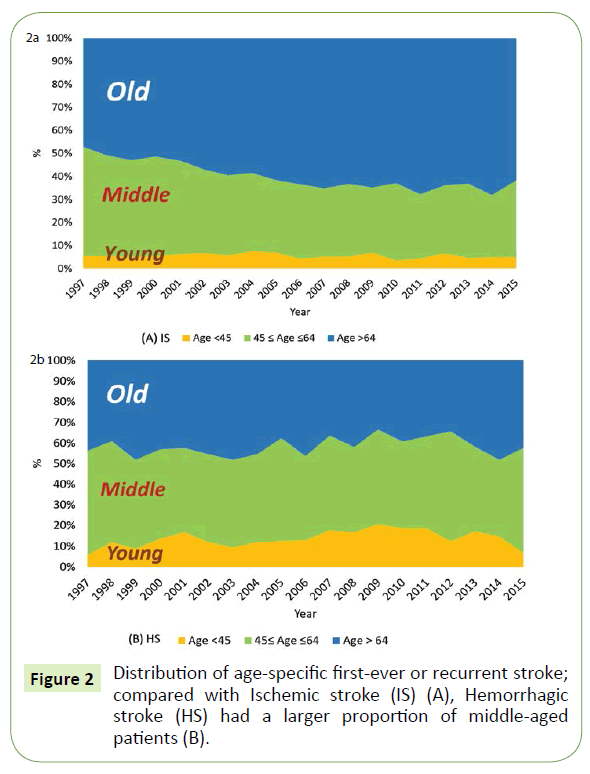
Figure 2 shows the age-specific distributions of first-ever or recurrent strokes over the past 19 years. For IS, the proportion of old age group steadily increased (47% in 1997 to 62% in 2015) and that of middle age decreased (47% in 1997 to 33% in 2015). However, for HS, the proportion of middle age group was steadily constant (51% in 1997 to 51% in 2015). Compared with IS, the young and middle age in HS has the large proportion (59% in HS; 39% in IS)
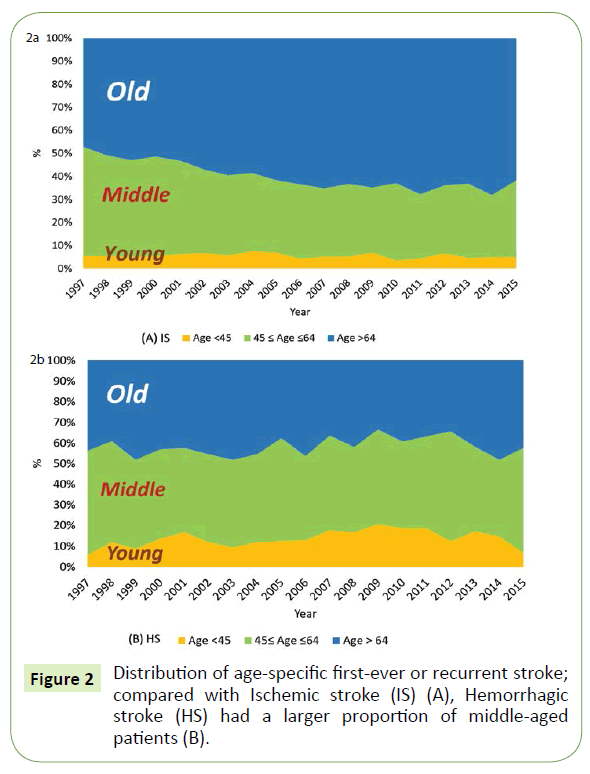
Figure 2: Distribution of age-specific first-ever or recurrent stroke; compared with Ischemic stroke (IS) (A), Hemorrhagic stroke (HS) had a larger proportion of middle-aged patients (B).
The changes in population distribution in Chungnam
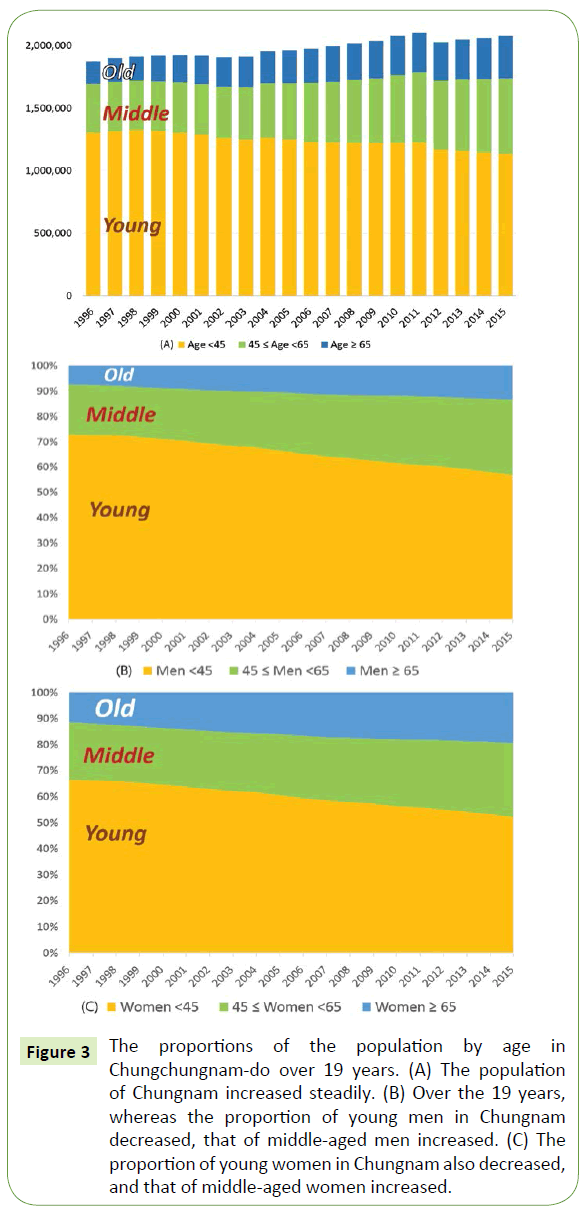
Figure 3 shows the demographic changes in age groups in Chungnam, where our hospital is located, from 1996 to 2015. During the 19 years of the study period, the population increased from 1,873,499 to 2,077,649 (11% growth); the proportion of young age people decreased, but that of the middle age people increased. For the same period, the populations of men and women in the area also grew, from 940,771 to 1,054,439 (12% growth) and from 932,728 to 1,023,210 (9.7% growth), respectively. Whereas the proportions of the young age people in Chungnam steadily decreased among both men and women (men; 73% in 1996 to 57% in 2015, women; 66% in 1996 to 52% in 2015). The proportions of the middle age people increased steadily among both sexes (men; 20% in 1996 to 30% in 2015, women; 22% in 1996 to 28% in 2015). The proportions of the old age people increased steadily among both sexes (men; 7% in 1996 to 13% in 2015, women; 12% in 1996 to 19% in 2015). Although the proportion of young age people decreased, middle and old age people increased in Chungnam. This changing trend in the population distribution in Chungnam is reflected in the decreasing mean ages of HS onset (mean age of HS; 63 in 1997, 59 in 2010).
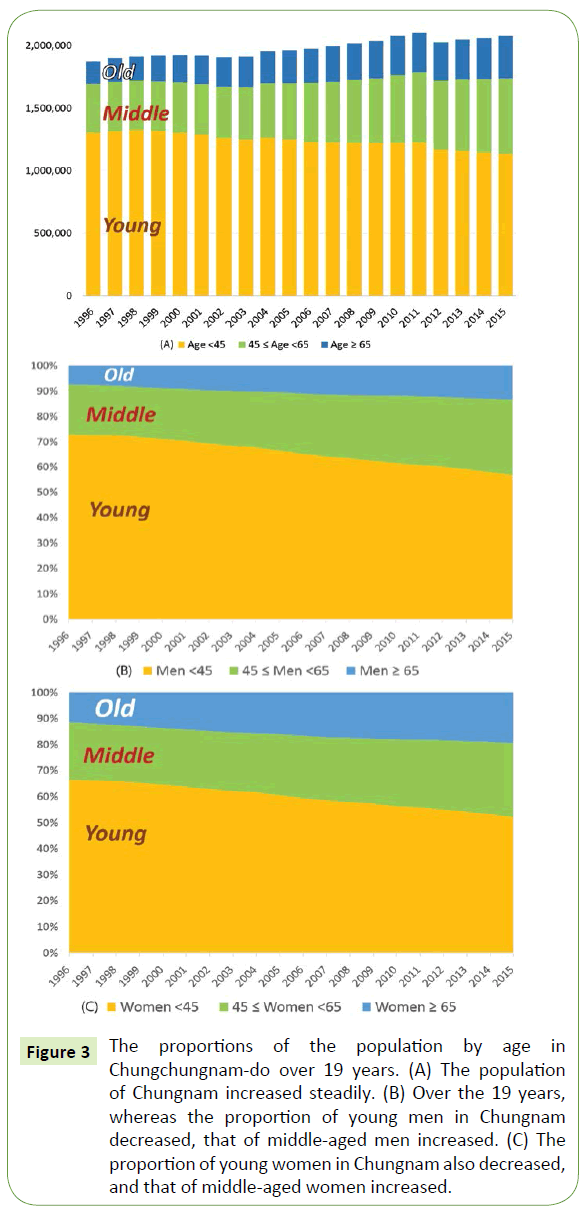
Figure 3: The proportions of the population by age in Chungchungnam-do over 19 years. (A) The population of Chungnam increased steadily. (B) Over the 19 years, whereas the proportion of young men in Chungnam decreased, that of middle-aged men increased. (C) The proportion of young women in Chungnam also decreased, and that of middle-aged women increased.
National health policy over the past two decades
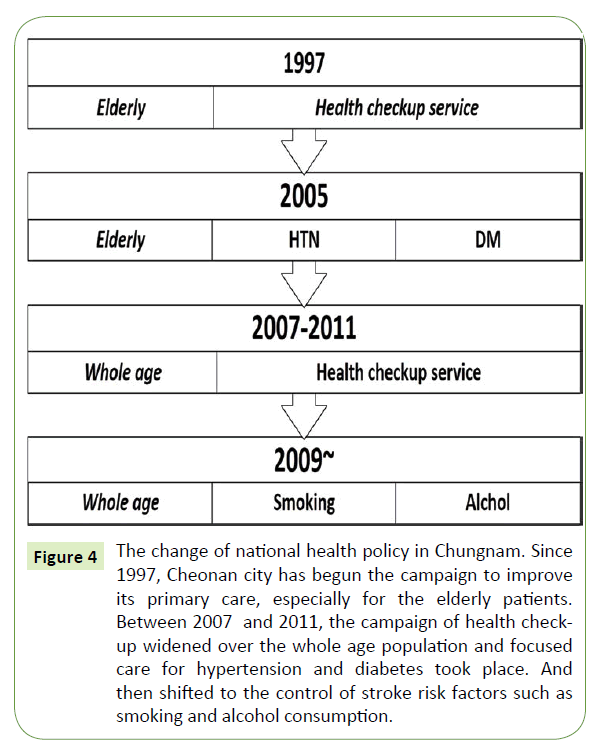
In 1997, Cheonan city (in the Chungnam) began a campaign to increase usage of the health check-up service at the public health center and to improve primary care, especially for elderly patients, in an effort to better prevent first strokes. Based on 2005, nationwide research data on public health and diet, the public health center announced that the prevalence of hypertension among over-30-year-olds was 27.9%. The center set the goal of maintaining 27.9% prevalence over the coming four years, and the suggested strategies for achieving the goal were the early diagnosis of hypertension and diabetes, special care for newly diagnosed patients, and a focus on the groups with high risk factors. Between 2007 and 2011, the health checkup campaign widened to the whole population and focused on care for hypertension and diabetes, and in 2009, the focus shifted to controlling stroke risk factors such as smoking and alcohol consumption. As our research shows, the mean age of HS onset began to suddenly increase after 2010 (mean age of HS; 59 in 2010 to 61 in 2015), when the city's health campaign had widened its focus from the elderly to the general population; this policy appears to have prevented strokes in the young and middle aged (Figure 4).
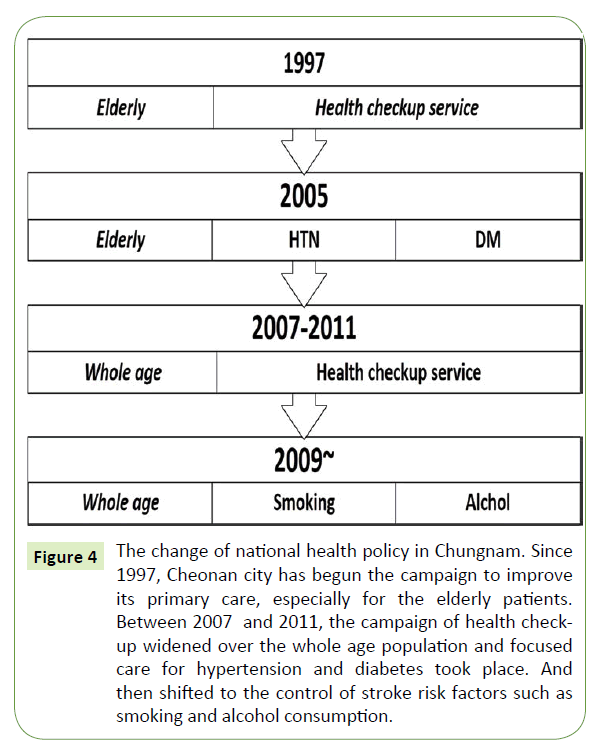
Figure 4: The change of national health policy in Chungnam. Since 1997, Cheonan city has begun the campaign to improve its primary care, especially for the elderly patients. Between 2007 and 2011, the campaign of health checkup widened over the whole age population and focused care for hypertension and diabetes took place. And then shifted to the control of stroke risk factors such as smoking and alcohol consumption.
Discussion
Our study showed that while the mean age of IS onset in rapidly developing urban area in South Korea increased over the past 19 years (from 1997 to 2015), that of HS showed a decreasing tendency. However, since the city's health campaign had widened to young and middle age population in 2010, the mean age of HS began reversing to older age. The young and middle age in HS has the large proportion compared with IS, and the proportion of SAH increased in young age patients, especially in men. And there are more male smokers in South Korea. HS and IS have many differences on aspects of epidemiology and risk factors. Some studies reported that an inverse relationship with rupture occurring more in young age (< 40) patients and in SAH patients younger than 40 years, males were predominate [2-4]. HS patients generally have more poor prognosis and higher mortality within the first 3 months after stroke onset, compared with IS [5]. And the relative role of risk factors is different between HS and IS [6]. While IS related with aging processing atherosclerosis, SAH seems to be more related with genetic and cigarette smoking in patients-related factor [7]. Although our study could not evaluate the correlation with other symptoms and signs such as hypertension, diabetes during 19 years, the proportion of risk factors (hypertension, diabetes, and BMI etc.) were similar between 1996~2005 and 2006 ~2015 (Table 1).
| Category, n (%) |
Hemorrhagic stroke |
Ischemic stroke |
Total |
| Number, n (%) |
4434 (36) |
7936 (64) |
12370 (100) |
| Men, n (%) |
1952 (44) |
4382 (55) |
6334 (51) |
| Mean age (years) ±SD |
60.2 ± 13 |
65.9 ±12 |
63.9 ±13 |
| Variables |
1996-2005 |
2006-2015 |
1996-2005 |
2006-2015 |
Total |
| Number, n (%) |
1716 (49) |
2718 (51) |
3830 (48) |
4106 (52) |
12370 (100) |
| Hypertension, n (%) |
868 (50.6) |
1418 (52.2) |
1991 (51) |
2011 (49) |
6288 (51) |
| Diabetes, n (%) |
360 (21) |
516 (19) |
842 (22) |
833 (20) |
2823 (23) |
| Obesity (BMI > 30kg/m2) , n (%) |
635 (37) |
951 (35) |
1072 (28) |
985 (24) |
3643 (29) |
| Current smoker, n (%) |
806 (47) |
1196 (45) |
1876 (49) |
1847 (45) |
5725 (46) |
| Previous stroke, n (%) |
257 (15) |
489 (18) |
842 (22) |
1026 (25) |
2614 (21) |
| Congestive heart failure |
145 (9) |
152 (6) |
498 (13) |
451 (11) |
1246 (10) |
| Atrial fibrillation |
170 (10) |
218 (8) |
764 (20) |
1010 (24) |
2162 (18) |
| COPD |
102 (6) |
163 (6) |
306 (8) |
410 (10) |
981 (8) |
| Chronic kidney disease |
85 (5) |
147 (5.4) |
268 (7) |
328 (8) |
828 (7) |
COPD: Chronic Obstructive Pulmonary Disease; BMI: Body Mass Index
Table 1: The demographic characteristics of patients with first-ever or recurrent stroke in patients who admitted on our hospital from 1996 to 2015.
Stroke has many variable patterns based on age, nation, risk factors, economic status, and residence in rural versus urban areas [8-10]. In South Korea, the stroke incidence was 216 per 100,000 person-years, and this incidence increased steeply with age; patients of old age comprised the main proportion of strokes. Meanwhile, the relative proportion of HS decreased steadily from 2000 to 2009 (35.3% to 23.9%) [11].
Considering Korea's rapid progress toward becoming an aging society and the pathogenesis of stroke, Chungnam is not an exception to the national trend. The number of young people age under 45 decreased over the past 19 years by approximately 10%, especially among the male population. Cheonan city, an important transportation hub in the country, transformed itself from an agricultural to an industrial town over the past two decades, and its population is steadily growing, unlike in most comparable cities. In the midst of these industrial and demographic changes, the changes in stroke onset age differed between IS and HS. In our city, the mean age of HS onset decreased over the 19 years, whereas that of IS increased steadily. In more detail, the mean age of HS onset decreased until 2010 and then increased suddenly after that; this sudden change in the trend for HS is especially notable. IS onset age showed a continuous increase, but the rate slowed after 2010. The changes in the population distribution and the national health policy influenced our HS age trends by modulation of risk factors of stroke for young and middle age population. According to national health policy of South Korea, health check-up service of Chungnam was widen from old age to young and middle age population in 2007 and Service to improve lifestyle through risk assessment and reinforce of post management was started to prevent the cardiovascular diseases since 2009. This policy could prevent the stroke of young age. Not only this health policy but also the increasing proportion of middle age population in Chungnam influenced the age trend of HS onset.
Given that the mean age of HS was lower than that of IS, the HS age trend could have been more influenced by the change in the proportion of middle-aged residents.
There are few cities like Cheonan city, whose population is aging but at the same time increasing as the process of industrialization is ongoing; most major cities whose industrialization took place in the mid- to late 1990s have been losing population. In continuously developing cities such as Cheonan city, it is notable that the mean age of HS onset decreased at the same time that its population of under-45s decreased as well. The health of the productive age group is a pillar of a society's economy, especially in the rapidly aging country that South Korea has become. It is clear that strokes in the young are a huge socioeconomic loss [12]. We think that this trend could appear in other developing countries and cities. In particular, it is necessary to investigate the mean age trends of first-ever or recurrent stroke in rapidly developing but aging urban areas for stroke prevention; our study suggests that the focus should be on HS among the young. A positive perspective is that the trends show that the prevention campaign that actively includes the middle aged appears to be improving the situation.
There are a number of limitations to this study. First, we investigated the stroke age trends between our hospital. So there are some differences in the incidence of HS in our hospital compared with the reports using the national wide data’s [11]. Recent reports of national wide data’s showed that the mean age of stroke onset has been increased. But the purpose of our study is that the change of age trend of stroke onset in rapidly developing urban area, so that it was meaningful as specific data. In particular, considering the status of our hospital as the centrally located major university hospital that would absorb most stroke patients in the city, I believe that our data are statistically significant, especially in 19 year worth of accumulation. Second, although the risk factors from our hospital’s data had no significant change on proportion between 1996-2005 and 2006-1015. We thought that other risk factors such age use of antiplatelet or anticoagulant and family history etc. should be more investigated.
Conclusion
Whereas the age of first-ever or recurrent stroke in a rapidly developing urban area in South Korea increased overall over the past 19 years, that of hemorrhagic stroke showed a decreasing tendency. However, in 2010, the mean age of HS began reversing to older age. From this trend, we conclude that stroke age trends can be affected by many factors such as the population distribution and the health care system.
Funding
This research was supported by the Soon Chunhyang University Research Fund.
Conflict of Interest
None.
19922
References
- Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, et al. (1980)Cerebrovasculardisease in the community: Results of a WHO collaborative study. Bull World Health Organ58:113-130.
- Juvela S, Poussa K, Lehto H, Porras M (2013) Natural history of unruptured intracranial aneurysms: A long-term follow-up study. Stroke44:2414-2421.
- Sonobe M, Yamazaki T, Yonekura M, Kikuchi H (2010) Small unruptured intracranial aneurysm verification study: SUAVe study, Japan. Stroke41:1969-1977.
- Locksley HB (1966) Natural history of subarachnoid hemorrhage, intracranial aneurysms and arteriovenous malformations. Based on 6368 cases in the cooperative study. J Neurosurg25:219-239.
- Andersen KK, Olsen TS,Dehlendorff C, Kammersgaard LP (2009) Hemorrhagic and ischemic strokes compared: stroke severity, mortality, and risk factors. Stroke40:2068-2072.
- Jamrozik K, Broadhurst RJ, Anderson CS, Stewart-Wynne EG (1994) The role of lifestyle factors in the etiology of stroke. A population-based case-control study in Perth, Western Australia. Stroke25:51-59.
- Lee S, Kim IK, Ahn JS, Woo DC, Kim ST, et al. (2015) Deficiency of endothelium-specific transcription factor Sox17 induces intracranial aneurysm. Circulation131:995-1005.
- Wang J, Bai L, Shi M, Yang L, An Z, et al. (2016) Trends in Age of First-Ever Stroke Following Increased Incidence and Life Expectancy in a Low-Income Chinese Population. Stroke47:929-935.
- Kissela BM, Khoury JC, Alwell K, Moomaw CJ, Woo D, et al. (2012) Age at stroke: Temporal trends in stroke incidence in a large, biracial population. Neurology79:1781-1787.
- Feigin VL, Krishnamurthi RV, Barker-Collo S, McPherson KM, Barber PA, et al. (2015) 30-year trends in stroke rates and outcome in Auckland, New Zealand (1981-2012): A multi-ethnic population-based series of studies. PLoS One10:e0134609.
- Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, et al. (2013) Stroke statistics in Korea: part I. Epidemiology and risk factors: A report from the korean stroke society and clinical research center for stroke. J Stroke15:2-20.