Keywords
Awareness; General anesthesia; BIS; Monitoring
Introduction
It is necessary that the level of general anesthesia (GA) is suitable for the individual patient undergoing surgery. If anesthesia is deeper than required to keep a patient unconscious, it could tilt the risk of anesthesia-related morbidity, such as postoperative nausea, vomiting, and cognitive divergence. This can also extend recovery times and rise health care costs. If anesthesia is too light, the patient may not be totally unconscious and can lead to intraoperative awareness. Intra-operative awareness is a rather rare circumstance with an incidence of occurrence in approximately 1-2 patients per every 1,000. Lyons declared that, Awareness is known to trigger depression, anxiety and post-traumatic stress disorder (PTSD) [1].
Under GA, the patient is routinely monitored for signs of potential intra-operative awareness, including rapid heartbeat, high blood pressure, sweating, tear production, motion, grimaces and rapid breathing. In patients receiving inhaled GA, end-tidal volatile anesthetic concentration can be assessed to measure the profundity of anesthesia. However, clinical observation alone is not adequate for understanding the depth of anesthesia. Electroencephalography (EEG) has been developed to measure and interpret the electrical activity in the brain to provide a measure of consciousness. Most EEC units include a module that collects and analyzes raw data from sensors placed on the patient's forehead. The output is then displayed numerically on a monitor to be observed by the anesthesiologist to evaluate the deepness of unconsciousness. One of these EEG devices is the Bispectral Index (BIS) [2-4].
Aims of the study is to evaluate the clinical impact of BIS monitoring to reduce the incidence of awareness and its impact on hemodynamic parameters, drug consumption, the recovery time and the end-tidal concentration of volatile anesthetics in adult patients undergoing various types of surgery under general anesthesia.
Background
Awareness during anesthesia is a serious complication of potential long-term psychological consequences. Use of the Bispectral Index (BIS), can reduce the incidence of anesthesia awareness for the patient. Igor Kagan showed that awareness and memory of surgical events during anesthesia are side effects that can lead to mental disorders including PTSD. Awareness during anesthesia cannot always be completely prevented. A patient may be aware for a number of reasons, including: the level of anesthesia, the type of anesthesia, inadequate monitoring and anesthesiologist errors. However, there are measures taken to reduce the risk of awareness. BIS monitoring appears to be a promising tool in helping to reduce intra-operative awareness [5].
Bispectral Index (BIS) monitoring system allows the anesthetic professionals to access processed EEG information as a measure of the effect of certain anesthetics under the care of patients they select to monitor. BIS is a statistical indicator which involves a merger of the repetition sphere, time sphere and the high order of the spectral parameters. The BIS algorithm was attained by documenting EEC wave data from healthy patients undergoing evolution periods between unconsciousness and consciousness after administration of various impressive methods [6]. The BIS ratio is a sum between zero (absenteeism of brain reaction, EEG isoelectric), and one hundred (patient attentive). A preferred quota for the allotment of anesthesia should be from 40-60 [7].
It has become a well-known fact that patients who have experienced awareness are reluctant to talk about it if not directly asked. Interview methods for detecting experiences of awareness have been developed, first by Brice, et al. [8] and later modified by Liu, et al. [9]. The modified Brice interview has been widely adopted and is now used in most studies for detecting awareness.
The primary characteristics of awareness vary between published reports. In a study of 26 patients with intra-operative awareness, Moerman, et al. [10] found that the most common form of recall was hearing sounds, reported by 89% of the patients. Paralysis was the second most common feeling, recalled by 85% of the study population, while pain was reported by 39% of those included in the study. Cobcroft and Forsdick found pain to be the most common recollection reported by 39% of patients experiencing recall inter-operatively. Recollection of sounds was reported by 31% of this study population [11].
Ghoneim, et al. studied cases of awareness published between 1950 and 2005, and analyzed the risk factors and causes. Two hundred and seventy-one cases of awareness were expressed and these were compared with control patients from two large groups of surgical patients. The main element related to occurrence of awareness was light anesthesia. Aware patients were more prone than controls to be younger, female, and undergoing obstetrical or cardiac surgery. Thirty-eight percent of patients disclosed pain during the episode. Other accusations included hearing voices (66%), feel helpless or worried (34%), and the inability to move (34%). Delayed psychological disorders were recorded in 22% of patients [12].
Myles et al. conducted a study to assess if BIS-guided anesthesia diminished the incidence of awareness during surgery in adults. The method was a prospective, randomized, double-blind, multicenter study. Adult patients with a high risk of awareness were randomized to BIS-guided anesthesia or routine care. The patients were assessed by a blinded observer for awareness at 2-6 hours, 24-36 hours and 30 days after surgery. Anon-partisan committee blinded to group character reviewed the existence of awareness at each reporting phase. The primary endpoint was proved awareness under anesthesia at any time. The study included 2,463 eligible and consenting patients, 1,225 in the BIS group and 1,238 in the routine care group. There were two reports of awareness in the BIS-guided group and 11 reports in the routine care group (P=0.022). BIS-guided anesthesia diminished the risk of awareness by 82% (95% CI 17-98%). The authors concluded that BIS-controlled anesthesia diminishes the risk of occurrence of awareness in adult surgical patients receiving general anesthesia [13].
Objectives
(1) To evaluate if the introduction of BIS monitoring in clinical practice for the administration of anaesthesia reduces the risk of intra-operative awareness in surgical patients undergoing general anaesthesia. (2) To examine whether BIS monitoring reduces pharmaceutical expenditure, recovery time, and endtidal volatile anesthetic concentration in patients undergoing general anaesthesia. (3) To discover the possible risks of BIS monitoring in patients undergoing general anaesthesia.
Methodology
Study design
This study is a prospective, randomized, double-blind, controlled study. Patients were randomized to one of two groups: BISguided anesthesia and routine care. The patients were appraised by a blinded viewer for awareness at 24-36 hours. After surgery, a blinded separate panel unaware of group identity evaluated each awareness report.
The study population
The study groups subsisted of men (n=41) and women (n=18) older than 18 years, going through different types of electoral surgery under general anesthesia between September and December, 2015.
Sampling of the study
The study sample subsisted of 60 patients randomized to either: Group (1), n=30 patients who had BIS-monitored general anesthesia. Group (2) n=30 patients who had routine care under general anesthesia. Note, one patient withdrew from the study; thus, Group (2) is n=29 patients. Response rate was 98%.
Anesthesia protocol
Anesthesia system thoroughly checked (evaporator, infusion pumps, fresh gas flow and intravenous lines). This protocol has been regulated to decrease the insecurity of intra-operative awareness. Patients are pre-medicated with midazolam (2 mg) intravenously. Anesthetic induced with fentanyl® (2 mcg/kg), propofol® (2 mg/kg), and Norcuron® (rocuronium bromide) (1 mg/kg) was given to facilitate intubation derived by conservancy therapy with O2, N2O and sevoflurane® is administered. At the end of surgery, Atropine sulfate® (0.5 mg) is given prior to a Neostigmine Methylsulfate® injection to lessen the risk of bradycardia. Neostigmine Methylsulfate® (0.04 mg/kg) is administered for reversal of the effect of neuromuscular blocking agents (NMBA). ECG, heart rate, blood pressure, SpO2, endtidal sevoflurane concentration, BIS value, and clinical signs of inadequacy of deepness of anesthesia (movement, sweating, tearing, coughing, and jerking) are monitored and recorded. Bispectral index (BIS) commercialized by Covidien BIS loc 2 channels is linked via electrodes to the patient's forehead after preparation of the skin of the patient by cleaning the pad with the alcohol to provide good electrical contact and a signal is transcribe from the electro-encephalographic activity of the patient. BIS value ranges from 0-100. A BIS value of (0) indicates EEC silence, while close to (100) is the value of a fully awake adult. Values between 40 and 60 indicate an adequate level of anesthesia recommended by the manufacturer. BIS signal is near to 100 at the start of the operation when the patient is conscious and falls to about 50 after the induction stage when the patient loses consciousness.
The BIS monitor allows the anesthesiologist to detect excessively high or low hypnosis and consequently to adapt the titration of the anesthetic agents to avoid unsafe states. Changes in anesthetic delivery are led by the presence of clinical signs in relation to the BIS value. If the patient has hypertension or tachycardia and the BIS value is > 60, sevoflurane levels are increased. If BIS values are in the target range of 50-60, then fentanyl is administered. If the BIS value is <50, then sevoflurane is reduced and the patient is monitored for a lack of pain relief. In the control group, the anesthetist could change anesthesia management at his/her discretion, based on the patient's needs. BIS Monitoring starts before anesthesia induction and lasts throughout surgery. Monitoring is discontinued when patients are discharged from the operating room. An end-tidal agent monitor is used.
Primary outcome measure
Incidence of intra-operative awareness.
Secondary outcome measures
(1) Intra-operative inhalation anesthesia consumption (2) Intra-operative anesthetic medications consumption (3) Recovery outcomes (time to eye opening, time to first movement response, time to response to commands, time to phonation, and time to extubation) (4) Postoperative nausea and vomiting (PONV ) (5) Postoperative Pain (6) time until discharge from the PACU.
Questionnaire
Each study subject was interviewed at the 24-36 h by a blinded observer after surgery. Two independent endpoint adjudication committees were part of anesthesiologists and certified nurse anesthetics (CRNA), blinded to group identity, be assessed independently of each reporting awareness.
The questionnaire included demographic information including gender, age, BMI, smoking, previous surgery, previous medications, and chronic diseases. Interview questions for postoperative assessment of awareness were chosen from questionnaires in previous studies of awareness (Appendix 1) [14-16].
Validity of the interview tool
The validity of the interview tool was substantiated by a team of five arbitrators (two anesthetists, two anesthetic nurses and a statistician) after all members of the team collectively provided input on the questions.
Reliability of the interview tool
The reliability of the interview tool was proved outright by the reliability coefficient using the Chronbach Alpha Equation. The reliability was up to 70.0%.
Study instrument
Aldrete Score is a system for measuring recovery after anesthesia. The numerical range for the Aldrete scoring system is 0 to 10. Two points are possible in each of five categories: activity, breathing, consciousness, blood circulation and color, and pulse oximetry, according to calculation. The system determines a patient's candidacy to leave the post-anesthesia care unit. A patient must receive at least 9 of the 10 points on the Aldrete scoring system to be considered for discharge [17].
Variables of the study
Age, gender, smoking, ASA status, weight, height, BIS value, SBP, DBP, MAP, HR, and SPO2 were deliberated and registered before induction (control value), after intubation, after incision, and every 5 minutes during the operation until the extubation (when the operation is complete and the adhesive bandage is applied to the surgical site, it is time for extubation which is defined as the period from this moment until the endotracheal tube is extubated).Consumption of anesthetic agents, lacrimation, coughing, sweating, and movement were measured throughout the duration of anesthesia and surgery, and the time of discharge from the PACU was recorded.
Randomization and blindness
Following signing of consent, patients were randomized to receive BIS-guided anesthesia (BIS group) or routine anesthesia care (routine care group). All other settings peri-operative persisted constantly between the two groups. In the BIS group, the obligated anesthesiologist had continued access to BIS information. In the control group, the anesthetist could change anesthesia management at his/her discretion, based on the patient's needs. Postoperatively, the care provider and patient were blinded to the type of group the patient was assigned intraoperative. Random assignment to study groups was achieved through envelopes containing random numbers formerly arranged by a person who is not convoluted with any other component of the study.
Procedure
After acquiring endorsement from the Institutional Review Board (IRB) and the attainment of written informed consent from all patients, 60 patients with American Society of Anesthesiologists [ASA] physical status I-III, foreseen for various types of elective surgery under general anesthesia were enrolled in the study. After 3-5 minutes of preoxygenation in a 10-15° inclined position, anesthesia was administered at 2 μg/kg of fentayl, 2 mg/kg of propofol and 1 mg/kg of Norcuron to facilitate endotracheal intubation. Anesthesia was maintained by O2, N2O and Sevoflurane (1-1.5%). ECG, BP, HR, SpO2, and BIS were monitored regularly all through the surgical procedure. Endtidal seveflurane, N2O and CO2 concentration was measured under anesthesia. Patients received fentanyl (1 microgram/kg) intravenously if there were clinical signs suggestive of a lack of depth of anesthesia, including an increase of >20% of preanesthetic values in HR and MAP, tearing, coughing, sweating, and movement. All data were registered by a person, who was not knowledgeable of anesthesia management protocol and technique. BIS, HR and BP were measured and documented at designated points during anesthesia: before induction, 30 seconds after laryngoscopy and intubation, and every 5 minutes until extubation of the patient.
Sevoflurane and nitrous oxide were stopped upon the start and completion of skin closure, respectively. Reversal of muscle relaxation by (atropine and neostigmine) was administrated during skin closure. Patients were requested to open their eyes at one-minute intervals after extubation. The time period from the termination of the inhalational agents to eye opening was noted. All patients were interviewed 24-36 hours after surgery to determine awareness. The primary endpoint was the confirmation of awareness, as defined by the patient's memory of intraoperative events, determined by interview. Each member of the review committees reviewed the interview results, and the independent coded each report with "awareness" or "no awareness". Accepted awareness was defined as a unanimous coding of “awareness” or two committee members coding as “awareness”. The recovery time was measured from the completion of wound dressings and for most patients included eye opening and qualification for discharge.
Inclusion criteria for subjects in the study group
(1) 18 years of age and older (2) Males & females (3) Elective surgery of different types (4) General anesthesia.
Exclusion criteria for study group
(1) Use of beta-blockers: Patients on beta blockers that provide muscle relaxants during surgery, in that betablockers may mask fast heart rate, physical movements, or hemodynamic changes [18] (2) Patients with traumatic brain injury, memory impairment, psychosis, or known or suspected electroencephalograph abnormality (e.g., epilepsy, previous brain resection, or scarring). (3) Patients with a history of mental disease (4) Uncooperative patients (5) Patients with language barrier problems (6) Patients with a history of awareness (7) Patients with opium addiction (8) Patients with neuromuscular disorders.
Statistical analysis
The statistical analyses were performed by SPSS software 21. A statistical power analysis was performed to determine the size of study required to show that the BIS monitor reduces intra-operative awareness. We took 30 patients for each group. Statistical measures calculated were: frequencies and percentages, mean and standard deviation, Chronbach alpha coefficient, Mann-Whitney Test of differences in all quantitative variables under study due to the group type (Routine Care group and BIS group), Chi Square Test of association between each categorical variable under study and the group type (Routine Care group and BIS group).
Ethical consideration
The ethical principles followed are: respect, informed consent, charity, no harm done, truth and justice, and explanation of research protocols to the patient. The study follows the World Medical Association Declaration of Helsinki Ethical Principles for Medical Research on Humans [19]. Prior to the commencement of data collection, approval for this study was obtained from the An-Najah National University Institutional Review Board (IRB).
To mitigate bias and ensure the confidentiality of all study participants, identification numbers were assigned to each patient to avoid using any patient information that would identify the patient. No hazards to participation were identified for this study. The researchers conciliated with all patients undergoing surgery with general anaesthesia in the preoperative holding area on the day of the scheduled surgical procedure. The researchers elucidated the objectives of the study, the participant's role in the study, privacy concerns, and participation as voluntary. At that time, all patients who fit the criteria were requested to be engaged in the study.
Results
Data were collected from a total of 59 patients aged between 18 and 72 years and enrolled in the study, with 30 patients randomized to the routine control group (one patient dropped out by withdrawing his consent form) and 30 patients to the BIS group. 41 patients were male and 18 patients were female, and all underwent different types of surgery. Patients were randomized in two groups with the BIS group receiving titrated anesthetic to maintain BIS values between 40 and 60, while the conventional group received anesthetic without the use of BIS monitoring during operation. The majority of patients were ASA I-III status. 18 patients (64.3%) in the RC group and 18 (62.1%) in the BIS Group had previous surgery and 11 (37.9%) in the RC group and 10 (34.5%) in the BIS group have chronic diseases; 11 (37.9%) in the RC group and 15 (51.7%) were smokers (Table 1). Patient demographics and clinical characteristics of the two study groups are shown in Table 1. There were no significant differences between the two groups in all the general characteristics of patients.
| Variable |
Routine Care group
N=29 |
BIS group
N=30 |
P-value |
| Mean Age |
41.11±18.892 |
43.34±16.363 |
0.571 |
| Mean Weight |
77.17±17.994 |
75.79±14.369 |
0.889 |
| Mean Height |
170.25±7.347 |
169.97±8.695 |
0.955 |
| Patient Metabolic Index |
26.62±4.70 |
26.14±4.00 |
0.690 |
| Gender-male |
20(69%) |
21(70%) |
0.931 |
| Gender-female |
9(31%) |
9(30%) |
|
| Previous surgery-Yes |
18(64.3%) |
18(62.1%) |
0.862 |
| Previous surgery-No |
10(35.7%) |
11(37.9%) |
|
| Previous medication-Yes |
6(22.2%) |
5(17.2%) |
0.639 |
| Previous medication-No |
21(77.8%) |
24(82.8%) |
|
| Smoking-Yes |
11(37.9%) |
15(51.7%) |
0.291 |
| Smoking-No |
18(62.1%) |
14(48.3%) |
|
| Chronic diseases-Yes |
11(37.9%) |
10(34.5%) |
0.785 |
| Chronic diseases-No |
18(62.1%) |
19(65.5%) |
|
*Significant at 0.05 level. Data are Mean±SD with P-values derived from Mann-Whitney U test or Frequencies and Percentages (%) with P-values derived from Chi Square test.
Table 1: Comparison of demographic variables and clinical characteristics between study groups (Routine Care and BIS).
There is a statistically significant difference in the inspired concentration of the anesthetic between the two groups under study. For the RC group, the mean value was 0.0282% which was lower at 0.024% in the BIS group, P=0.043. The data also show a statistically significant difference in the mean dose of inhaled anesthetic agents between the two groups: for the RC group, the mean value was 0.029% and was 0.025%` for the BIS group, P=0.023. There is a statistically significant difference in the endtidal sevoflurane concentration: the mean value was 0.054 for RC group and 0.018 for the BIS group, P=0.004. There is a statistically significant difference in sevoflurane dosage between the two groups: for the RC group the mean value was 0.028 and it was 0.023 for the BIS group, P=0.023 (Table 2). This generally means that the consumption of inhaled anesthesia was significantly less in the BIS group compared to the RC group. These results confirm that using BIS monitoring reduces consumption of inhalational anesthesia.
| Induction Agent |
Routine Care group
N=29 |
BIS group
N=30 |
P-value |
| Propofol mg |
230±59.938 |
474.07±711.3 |
0.235 |
| Midazolam mg |
1.17±0.408 |
1.5±1 |
0.648 |
| Fentanyl (µg) |
77.76±40.523 |
115.56±94.18 |
0.035* |
| Inspired concentration of the Sevoflurane% |
0.028±0.007
(0.011-0.04) |
0.024±0.013
(0.0-0.07) |
0.043* |
| Mean dose of i.v. anesthetic agent (mg) |
221.07±56.197 |
260.67±243.678 |
0.936 |
| Mean dose of inhaled anesthetic agents |
0.029±0.008
(0.012-0.04) |
0.025±0.009
(0.01-0.035) |
0.023* |
| End-tidal sevoflurane concentration % |
0.054±0.166
(0.008-0.9) |
0.018±0.012
(0.006-0.06) |
0.004* |
*Significant at 0.05 level. Data are Mean ± SD with P-values derived from Mann-Whitney U test or Frequencies and Percentages (%) with P-values derived from Chi Square test.
Table 2: Comparison of induction agent levels between study groups (Routine Care and BIS).
There is a statistically significant difference in the fentanyl dosage between the two groups: for the BIS group, the mean value was 115.56, while it was 77.76 for the RC group, P=0.035 (Table 2). It is clear that patients in the RC group got significantly less amounts of fentanyl intra-operatively compared with the BIS group. There may have been insufficient doses.
There is a difference in the propofol dosage between the two groups: for the BIS group, the mean value was 474.07 ± 711.3 which was reduced to 230 ± 59.938 for the RC group, P=0.235 (Table 2). It is clear that patients in the RC group had a lower propofol dose than patients in the BIS group, but the difference was not significant.
There is statistically significant difference between the group type and intra-operative jerking with the percentage of intraoperative jerking reduced from f(%) 8(27.6%) in the RC group to 2(6.9%) in the BIS group, P=0.037 (Table 3). There are no statistically significant differences between the group types and intra-operative sweating, intra-operative lacrimation, pupillary dilatation, and intra-operative coughing (Table 3).
| Variable |
Categories |
Routine Care group
N=29 |
BIS group
N=30 |
P-value |
| Intra-operative Sweating |
No |
29(100%) |
26(96.3%) |
0.296 |
| |
Yes |
0(0%) |
1(3.7%) |
|
| |
Missing |
0 |
3 |
|
| Intra-operative lacrimation |
No |
24(85.7%) |
25(89.3%) |
0.686 |
| |
Yes |
4(14.3%) |
3(10.7%) |
|
| |
Missing |
1 |
2 |
|
| Pupillary Dilatation |
No |
27(96.4%) |
26(92.9%) |
0.553 |
| |
Yes |
1(3.6%) |
2(7.1%) |
|
| |
Missing |
1 |
2 |
|
| Intra-operative Coughing |
No |
28(96.6%) |
29(100%) |
0.313 |
| |
Yes |
1(3.4%) |
0(0%) |
|
| |
Missing |
0 |
1 |
|
| Intra-operative Jerking |
No |
21(72.4%) |
27(93.1%) |
0.037* |
| |
Yes |
8(27.6%) |
2(6.9%) |
|
| |
Missing |
0 |
1 |
|
*Significant at 0.05 level. Data are Frequencies and Percentages (%) with P-values derived from Chi Square test.
Table 3: Difference between intra-operative physiological variables between study groups (Routine Care and BIS).
Regarding anesthetic time, 76.6 ± 84.3 min was recorded in the RC group and 124.2 ± 124.4 min in BIS group; the difference was not significant (P=0.207).The surgical time was 73.8 ± 85.8 min in the RC group and 116.4 ± 106.2 min in the BIS group, and the difference was not significant (P=0.194).There is a statistically significant difference in time to phonation between the two study groups with the mean time to phonation of the RC group at 12.82 min and for the BIS group equal to 10.21 minutes, P=0.026 (Table 4). There are no statistically significant differences between the two study groups in any of the remaining time measures under study that are: time from cessation of inhalational agents to eye opening, time to response to commands, time to eye opening (either spontaneously or in response to command), time to first movement response, and time to extubation (Table 4).
| Variable |
Routine Care group
N=29
M(±SD) |
BIS group
N=30 |
P-value |
| Time of surgery(minutes) |
73.8±85.8 |
116.4±106.2 |
0.194 |
Length of Procedure (minutes)
Anesthesia time |
76.6±84.3 |
124.2±124.4 |
0.207 |
| Time from cessation of inhalational agents to eye opening (minutes) |
7.32±4.643 |
5.19±3.462 |
0.087 |
| Time to response to commands (minutes) |
10.03±5.335 |
8.11±4.516 |
0.205 |
| Time to eye opening (either spontaneously or in response to command) (minutes) |
10.81±5.955 |
8.24±4.833 |
0.086 |
| Time to first movement response (minutes) |
7.69±6.03 |
5.31±3.878 |
0.174 |
| Time to phonation (minutes) |
12.82±6.11 |
10.21±5.127 |
0.026* |
| Time to extubation (minutes) |
8.64±4.775 |
7.25±4.106 |
0.278 |
*Significant at 0.05 level. Data are Mean ±SD with P-values derived from Mann-Whitney U test.
Table 4: Differences in anesthesia management time variables between study groups (Routine Care and BIS).
There are statistically significant differences in perception of pain between study groups. 25% of patients in the RC group expressed mild levels of pain while 0% in the BIS group did. This happened because the BIS group had mild pain less than expected (count=0 and the expected count=3.4), while the RC group had mild pain more than expected (count=7 and the expected count=3.6). On the other hand, 7.1% of the RC group expressed moderate levels of pain, while 23.1% of the BIS group had moderate levels of pain. This happened because the BIS group had moderate pain more than expected (count=6 and expected count=3.9), while the RC group had moderate pain less than expected (count=2 and expected count=4.1), P=0.011 (Table 5).
| Variable |
Categories |
Routine Care group
N=29
F(%) |
BIS group
N=30
F(%) |
P-value |
| Nausea (yes/no) |
No nausea |
29(100%) |
26(100%) |
----- |
| Missing |
0 |
4 |
Pain
0(no pain)
1-3(Mild)
4-6(Moderate)
7-8(Severe)
9(Very Severe)
10(Worse Possible) |
No Pain |
19(67.9%) |
20(76.9%) |
0.011* |
| Mild |
7(25%) |
0(0%) |
| Moderate |
2(7.1%) |
6(23.1%) |
| Severe |
0(0%) |
0(0%) |
| Very Severe |
0(0%) |
0(0%) |
| Worse Possible |
0(0%) |
0(0%) |
| Missing |
1 |
4 |
*Significant at 0.05 level. Data are Frequencies and Percentages (%) with P-values derived from Chi Square test.
Table 5: Differences in nausea and pain between study groups (Routine Care group and BIS group).
There is a statistically significant difference in the time to discharge from the PACU between the two study groups: the mean time to discharge from the PACU was 12.38 minutes for the RC group and 9.23 minutes for the BIS group, P=0.007 (Table 6). It is evident that the patients in the BIS group were discharged from PACU earlier than patients in the RC group. There are no statistically significant differences in all other variables being studied, such as recovery time and Aldrete Score (Table 6).
| Variable |
Routine Care group
N=29
Mean ±S.D |
BIS group
N=30
Mean ±S.D |
P-value |
| Recovery time (minutes) |
11.64±5.09 |
9.95±4.261 |
0.210 |
Discharge Criteria Score
Aldrete Score |
9.72±0.75 |
9.7±1.67 |
0.185 |
| Time to Discharge from the PACU (minutes) |
12.38±4.989
(6-26) |
9.23±3.819
(4-20) |
0.007* |
*Significant at 0.05 level. Data are Mean±SD and (Minimum-Maximum) with P-values derived from Mann-Whitney U test.
Table 6: Differences in Recovery time, Discharge Criteria Score, Time to Discharge from the PACU between Study Groups (Routine Care group and BIS group).
There is a statistically significant difference between the two study groups in the pre operation respiratory rate (RR). The pre operation RR per min for the BIS group had a mean value of 15.13 ± 2.013 and for RC group 13.93 ± 2.071 min, P=0.033. Values of Pre-Operative RRs for both groups are within the normal range, so there is no clinical importance to this difference. There are no statistically significant differences between the two groups in the variables: SAT, CO2, HR, SBP, DBP, MAP Pre and Post operation (Table 7).
| Parameter |
Routine Care group
N=29
M ±SD |
BIS group
N=30
M ±SD |
P-value |
| Intra-operative SAT (SPO2)% |
98.52±1.01 |
98.7±1.35 |
0.249 |
| Intra-operative End-tidal CO2 (mm Hg) |
33.88±4.34 |
33.86±3.66 |
0.739 |
| Intra-operative HR (beat /min) |
78.77±12.37 |
77.25±13.27 |
0.544 |
| Intra-operative SBP (mmHg) |
112.64±19.13 |
116.91±21.82 |
0.458 |
| Intra-operative DBP (mmHg) |
69.9±16.15 |
70.2±13.39 |
0.779 |
| Intra-operative MAP (mmHg) |
83.38±14.79 |
84.87±14.86 |
0.514 |
| Pre Operation HR (beat/min) |
81.03±15.873 |
88.17±21.28 |
0.395 |
| Pre Operation Systolic Blood Pressure (mmHg) |
142.14±27.601 |
142.5±28.137 |
0.891 |
| Pre Operation Diastolic Blood Pressure(mmHg) |
87.28±20.32 |
86±16.233 |
0.976 |
| Pre Operation O2 SAT% |
98.48±2.011 |
99±1.857 |
0.330 |
| Pre Operation RR (breath/min) |
13.93±2.071 |
15.13±2.013 |
0.033* |
| Pre Operation TEMP(°C) |
36.643±0.2026 |
36.663±0.2883 |
0.514 |
| Post Operation HR (beat/min) |
78.58±17.948 |
89.67±26.192 |
0.155 |
| Post Operation Systolic Blood Pressure (mmHg) |
132.79±25.518 |
135.62±20.812 |
0.665 |
| Post Operation Diastolic Blood Pressure mmHg |
86.53±17.36 |
84.62±16.963 |
0.776 |
| Post Operation O2 SAT (%) |
99.05±1.682 |
99.19±1.078 |
0.755 |
| Post Operation RR (breath/min) |
14.68±1.916 |
15±1.581 |
0.525 |
| Post Operation TEMP (°C) |
36.195±1.2782 |
36.455±0.4522 |
0.221 |
*Significant at 0.05 level. Data are Mean ± SD with P-values derived from Mann-Whitney U test.
Table 7: Differences of anesthesia management parameters (SAT, CO2, HR, SBP, DBP, MAP and Pre and Post Operation Parameters) between study groups (Routine Care and BIS).
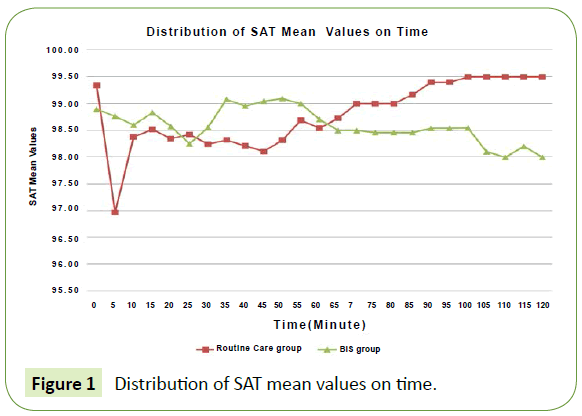
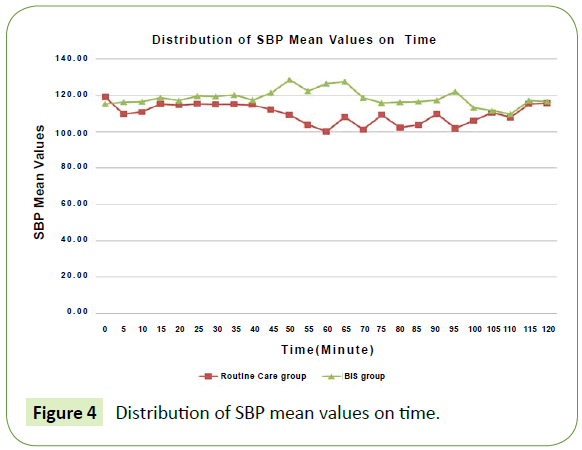
There are statistically significant differences between the BIS and Routine Care groups in SAT at the following time points during operations: 35 min. (Routine Care mean=98.32%, BIS mean=99.08%), 40 min. (Routine Care mean=98.21, BIS mean=98.96%), 45 min. (Routine Care mean=98.11, BIS mean=99.05%), 50 min. (Routine Care mean=98.32, BIS mean=99.10), but this data has no clinical relevance because all values are within the normal range. There are statistically significant differences between the two study groups in SBP during operation at the following time points: 50 min. (Routine Care mean=109 mmHg, BIS mean=128.45 mmHg), 55 min. (Routine Care mean=103.75 mmHg, BIS mean=122.25 mmHg), 60 min. (Routine Care mean=100.08 mmHg, BIS mean=126.29 mmHg), but, again, this result has no clinical relevance since all values are in the normal range for both groups (Table 8).
| Parameters at Specific Time Points-Minutes |
Routine Care group
N=29
M ±SD |
BIS group
N=30
M ±SD |
P-value |
| SAT_35 (%) |
98.32±1.145 |
99.08±1.1 |
0.014* |
SAT_40
% |
98.21±1.285 |
98.96±1.186 |
0.030* |
SAT_45
% |
98.11±1.823 |
99.05±1.046 |
0.046* |
SAT_50
% |
98.32±1.293 |
99.1±1.513 |
0.010* |
SBP_50
(mmHg) |
109±28.08 |
128.45±25.482 |
0.016* |
SBP_55
(mmHg) |
103.75±20.722 |
122.25±27.34 |
0.028* |
SBP_60
(mmHg) |
100.08±28.268 |
126.29±32.031 |
0.034* |
DBP_50
mmHg |
61.18±15.593 |
76±15.922 |
0.008* |
DBP_55
(mmHg) |
62.33±15.656 |
72.68±16.62 |
0.039* |
MAP_50
(mmHg) |
77.56±17.494 |
92.57±19.836 |
0.012* |
*Significant at 0.05 level. Data are Mean±SD with P-values derived from Mann-Whitney U test.
Table 8: Differences in anesthesia management parameters (SAT, CO2, HR, SBP, DBP and MAP) across time for routine care and BIS study groups.
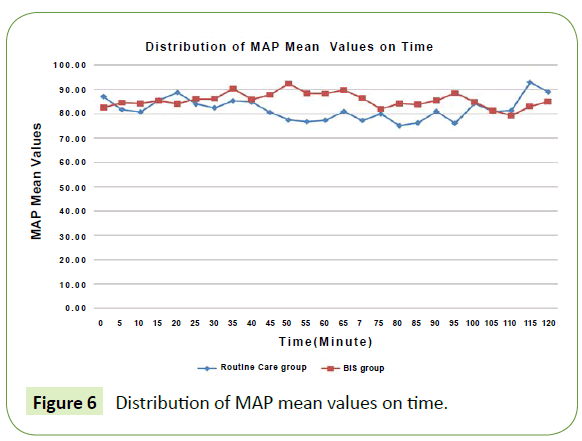
There are statistically significant differences between the two study groups (BIS and Routine Care) in DBP during operation at the following time points: 50 min. (Routine Care mean=61.18 mmHg, BIS mean=76), 55 min. (Routine Care mean=62.33 mmHg, BIS mean=72.68 mmHg). Again, this result has no clinical relevance since all values are in the normal range for both groups (Table 8).
There are statistically significant differences between the two study groups in MAP during operation at the 90 minute time point (Routine Care mean=77.56 mmHg, BIS mean=92.57 mmHg). Finally, there were no statistically significant differences between the two study groups for all other variables of blood pressure and time points, as we measured blood pressure every 5 minutes intra-operatively (Table 8).
Of the total 59 patients 29 patients were assigned to the routine control group and 30 patients to the BIS group. No case of awareness was reported in the BIS-guided group but 4 reports (13.8%) in the control group (P=0.035), BIS-guided anesthesia decreased awareness by 13.8% (95% CI (1.3%-26.4%) (Table 9). The most common forms of awareness was auditory perceptions, tactile perception and the sense of paralysis. Patients with awareness of the RC group, two patients undergoing cholecystectomy, one patient undergoing strabismus surgery and one patient undergoing Submucosal Resection of the nose (SMR).
| Variable/Category |
Group |
P-value |
Routine Care (n= 29 )
f(%) |
BIS (n= 30 )
f(%) |
| Incidence of Awareness |
No(n=55) |
25(86.2%) |
100( 96. 7%) |
0.0.035* |
| Yes(n=4) |
4(13.8%)* |
0(0%)* |
*Significant at 0.05 level. Data are Frequencies and Percentages (%) with P-values derived from Chi Square test.
Table 9: Association between awareness and study group (Routine Care and BIS).
Table 10 shows that there are no statistically significant association at the significance level α=0.05 between awareness measurement and gender, surgical time and age categories (all P-Values>0.05).
| Variable/Category |
Awareness |
P-value |
| No |
Yes |
| Gender |
Male(n=41) |
39(95.1%) |
2(4.9%) |
0.578 |
| Female(n=18) |
16(88.9%) |
2(11.1%) |
| Surgical Time |
0-30 minutes(n=10) |
10(100%) |
0(0%) |
0.675 |
| 31-60 minutes(n=23) |
20(87%) |
3(13%) |
| 61-90 minutes(n=10) |
10(100%) |
0(0%) |
| more than 90 minutes(n=16) |
15(93.8%) |
1(6.3%) |
| Age Categories |
less than 20(n=7) |
5(71.4%) |
2(28.6%) |
0.235 |
| 20-29(n=7) |
7(100%) |
0(0%) |
| 30-39(n=14) |
12(85.7%) |
2(14.3%) |
| 40-49(n=6) |
6(100%) |
0(0%) |
| 50-59(n=14) |
14(100%) |
0(0%) |
| 60-69(n=7) |
7(100%) |
0(0%) |
| 70 or more(n=2) |
2(100%) |
0(0%) |
Table 10: shows frequency, percentages and the P-values of the Chi Square test of association between awareness measurement and gender, surgical time and age categories.
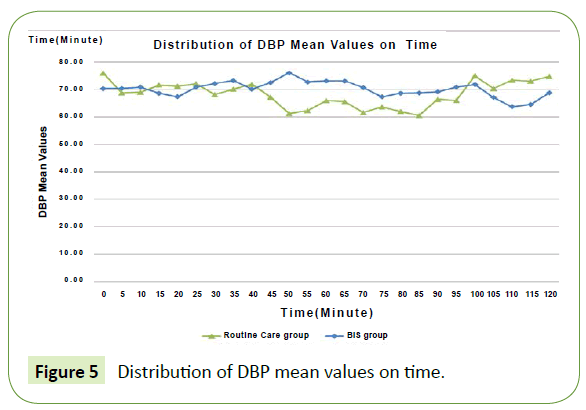
Figure 1 shows a rise in SAT levels for the RC group over the SAT levels for the BIS group after 60 minutes of operation duration. The differences were significant only at the minutes35, 40, 45, and 50 in favor of the BIS group. This result has no clinical relevance since all values are in the normal range for both groups.
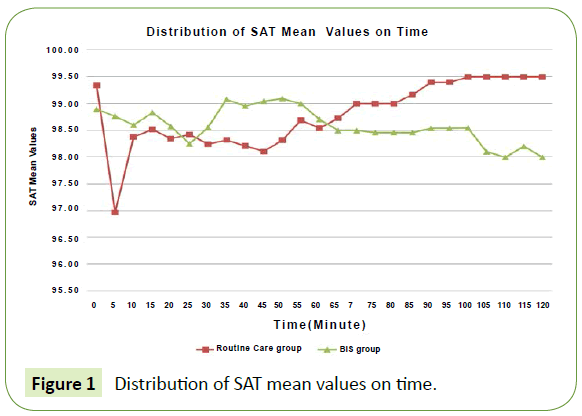
Figure 1: Distribution of SAT mean values on time.
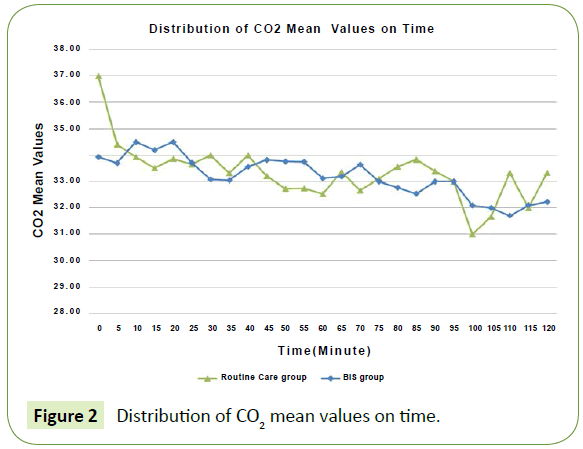
Figure 2 exhibits that end-tidal CO2 parameters do not differ between the two study groups over duration of operation. There were no significant differences between each two corresponding points.
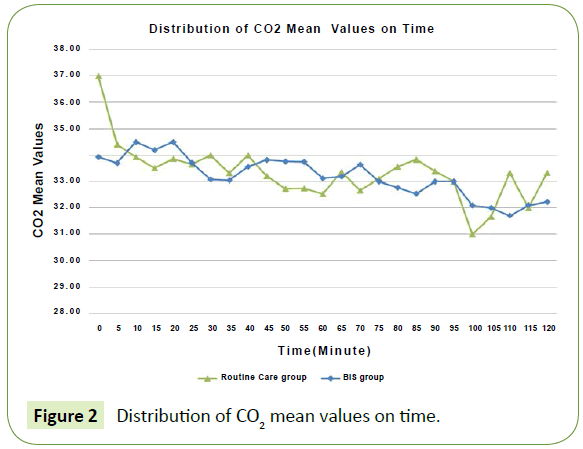
Figure 2: Distribution of CO2 Figure 2 mean values on time.
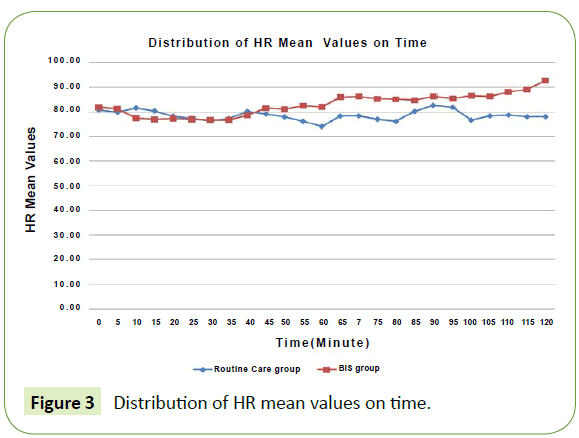
Figure 3 shows that HR levels do not differ between the study groups through the duration of the operation, except at the final time range (100 min. and afterward), but it is not significant. There were no significant differences between each two corresponding points.
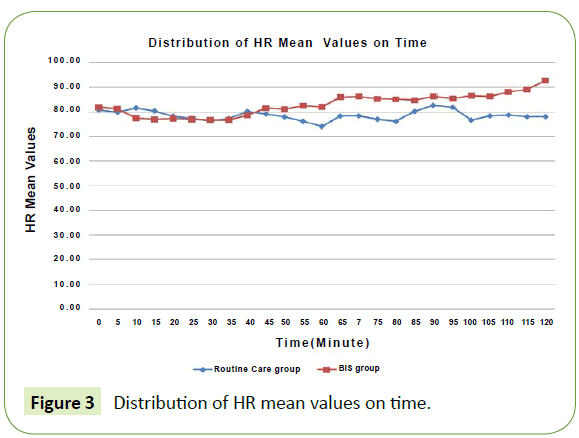
Figure 3: Distribution of HR mean values on time.
Figure 4 exhibits that the difference in SBP levels for the study groups does not differ through the duration of the operation. The differences were significant only at the minutes50, 55, and 60, P?0.05 in favor of the BIS group. This result has no clinical relevance since all values are in the normal range for both groups.
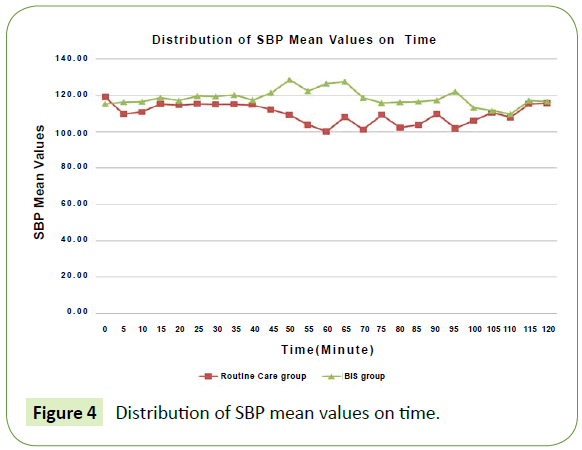
Figure 4: Distribution of SBP mean values on time.
Figure 5 exhibits differences in DBP levels for the study groups, with the DBP of the BIS group higher than for the RC group at the 50 and 55 minute time frames. The differences were significant only at the minutes 50 and 55, P?0.05 in favor of the BIS group. This result has no clinical relevance since all values are in the normal range for both groups.
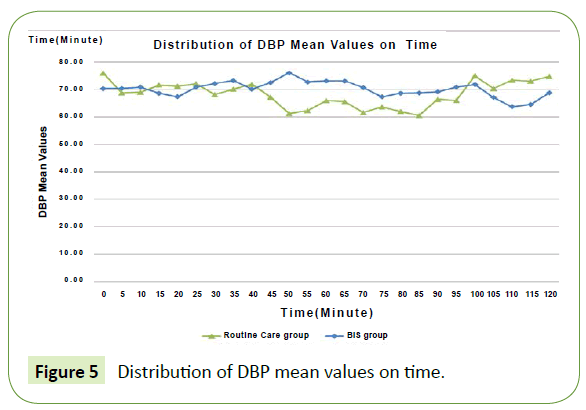
Figure 5: Distribution of DBP mean values on time.
Figure 6 shows differences in MAP for the study groups. The differences were significant only at the minute 50, P?0.05 in favor of the BIS group. This result has no clinical relevance since all values are in the normal range for both groups.
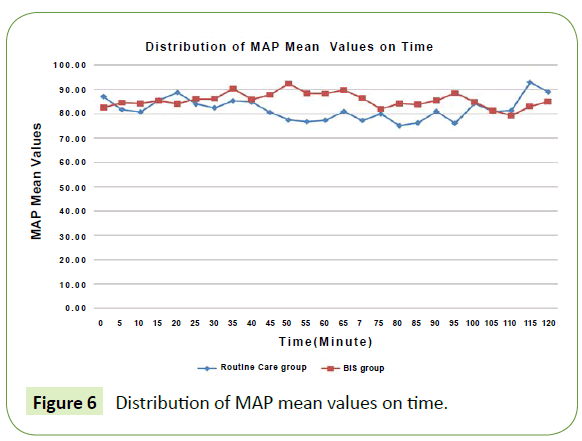
Figure 6: Distribution of MAP mean values on time.
Discussion
BIS monitoring has been introduced to the operating room to reduce the incidence of awareness, improve anesthesiologist ability to administer anesthetics and improve outcomes in early discharge from the recovery room. Of the total 59 patients 29 patients were assigned to the routine control group and 30 patients to the BIS group. No case of awareness was reported in the BIS-guided group but 4 reports (13.8%) in the control group (P=0.035), BIS-guided anesthesia decreased awareness by 13.8% (95% CI (1.3%-26.4%). The most common forms of awareness was auditory perceptions, tactile perception and the sense of paralysis.
BIS-guided Anesthesia can Reduce the Risk of Intra-operative Awareness
We have found that BIS-guided anesthesia can reduce the risk of intra-operative awareness in surgical patients. We observed a statistically significant difference in occurrence of awareness between patients undergoing routine care during surgery (4 out of 29, 13.8%) and patients monitored by a BIS device during surgery (0 out of 30, 0%) (P=0.035). BIS-guided anesthesia decreased awareness by 13.8% (95% CI (1.3%-26.4%). These results are in agreement with previous findings [13,20].
The results of the current study are consistent with the earlier findings of Chen et al. showed that the use of the BIS-guided anesthesia significantly reduced the incidence of awareness from 0.65% to 0.14% when compared with the control group [21].
The risk of intra-operative awareness varies from country to country, depending on the anesthetic methods. Our study is consistent with a study of Sebel, et al. from the US which showed that an incidence of intra-operative awareness of about 0.1% to 0.2% of patients undergoing general anesthesia [22]. Our study is also in line with a study from Europe that a large prospective study conducted by Samuelsson et al. who explored awareness of 11,785 patients undergoing general anesthesia. The incidence of intra-operative awareness with explicit recall was 0.1% without the use of neuromuscular blocking drugs. When they used neuromuscular blocking drugs, awareness was 0.18%) [23]. Our study also agrees with another European study by Liu et al. that reported incidence of recall of intra-operative events and dreams during non-obstetric operations, which was 0.2% and 0.9% respectively [9].
The results of the present study also agree with Ekman et al. who reported that fewer patients in the BIS-monitored group had significant explicit recall compared to a control group (0.04% compared with 0.18%, P<0.038). This represents a reduction in the incidence of intraoperative awareness in the BIS-monitored group by 77%. The author explained that it may be because the patients were kept in a deep anesthetic state, and anesthesiologists were told to avoid BIS values above 60 during induction and maintenance. The results showed that during the maintenance phase, the average BIS score was 38 (SD 8). According to BIS monitoring guidelines from the manufacturer, values below 40 indicate a deep hypnotic state, which is not recommended for surgical procedures [20].
Our results are also in line with a systematic review conducted by Punjasawadwong which provides sufficient evidence to support the use of BIS-monitoring to guide anesthesia administration and to prevent intra-operative awareness [24]. Also our results are confirmed by the findings of Sandin et al. who reported a reduced risk of awareness of 13% over a control group when BIS monitoring was used during general anesthesia [25]. The results of the current study are in accordance with the B-Aware trial conducted by Myles, et al., a multicenter, double-blind, randomized trial that evaluated the effectiveness of BIS monitoring in reducing awareness. Myles’ study reported an awareness risk reduction of 82% when BIS monitoring was used [13].
The results of the current study are also consistent with the study of Bergman et al., which showed that of 8,372 patients, reported incidents were 50 cases of definite awareness and 31 cases of a high probability awareness. Each group was further subdivided into incidents with no apparent cause of preventable awareness, incidents with a clearly documented cause of awareness and incidents caused by medication errors. There were 13 cases (16%) with no apparent cause. In 36 cases (44.5%), incidents were due to a low volatile inspired concentration or insufficient hypnosis, and in 32 cases (39.5%), the event was due to the drug's fault [26].
Results of the current study do not agree with the study of Mozafari et al., who showed no evidence that BIS monitoring reduced awareness in patients undergoing abdominal surgery under general anesthesia compared to patients monitored by routine anesthesia administration protocols [27]. Avidan et al. compared a BIS-based anesthesia administration protocol and a protocol based on measurement of end tidal anesthetic gas (ETA) and investigated reduction of anesthesia consciousness. They found that anesthesia consciousness was similar between both groups [28].
Respectively, our study does not agree with a study from Saudi Arabia carried out by Messahel and Al-Qahtani, which examined the incidence of intra-operative awareness of 4,368 patients who underwent surgery. In this study, all patients were given a premedication. This study reported no incidence of intraoperative awareness [29].
Authors of the current study suggest that examining the anesthetic technique is important to understand the cause of awareness during anesthesia. Patients in the routine care group were given a smaller amount of propofol that produces hypnosis, and a smaller amount of fentanyl to relieve pain and suppress motion than patients in the BIS group. This may be the cause of the patients in the routine care group having awareness but not in the BIS group in the current study. This suggests that the patient can be exposed to light anesthesia. When anesthesia is too light, it can lead to recall events or conversations that take place in the operating room. The cause is not clear. On the other hand, monitoring the depth of anesthesia using BIS should prevent intra-operative awareness and contribute to a precise dose of anesthetic.
Inhalational Anesthetic Agent Consumption
The depth of anesthesia is measured by clinical parameters during anesthesia (for example, blood pressure, heart rate, or drug concentrations). These parameters become unreliable for measuring depth of anesthesia over the term of titration of anesthetic agents [30]. Monitoring of inhalation anesthetic concentration by observing minimum alveolar concentration is part of routine anesthesia practice. It provides a method for monitoring the continuous brain concentration of volatile anesthetics. The BIS Index is a numerically treated, clinically validated EEG parameter that measures the effects of anesthesia and sedation on the brain [31]. According to the manufacturer of the BIS, this monitoring function provides a vital tool that allows clinicians to deliver anesthesia appropriate to a patient’s needs, and to assess and react appropriately to a patient's clinical condition during surgery. Over all, it can be helpful to maintain sufficient depth of anesthesia.
Our study showed a statistically significant reduction in the mean dose of inhaled anesthetics when using BIS monitoring as compared with routine care and anesthesia monitoring protocols. We also found a statistically significant reduction in end-tidal sevoflurane concentration when using BIS monitoring as compared with routine care and anesthesia monitoring protocols. Our results are in agreement with studies by Punjasawadwong, et al. who showed that BIS-guided anesthesia can significantly reduce anesthetic consumption [24] and with Croci et al. who showed that BIS monitoring in women undergoing general anesthesia for gynecological laparascopic surgery reduced desflurane consumption by 34.6% [32].Our study shows that the consumption of inhaled anesthesia was significantly less in the BIS group compared to the RC group. These results confirm that using BIS monitoring reduces consumption of inhalational anesthesia.
Anesthetic Drugs Consumption
Our results showed a significant increase in fentanyl dose in the BIS group as compared with the RC group and anesthesia monitoring protocols. Our results were not consistent with other studies [33-36].
Alkire, et al. showed that consumption of propofol during induction was significantly lower when using BIS monitoring as compared with routine care during general anesthesia. Our results are not consistent with this study [37]. Our data show that the consumption of propofol for induction does not differ significantly between BIS monitoring and routine care. However, we observed that patients in the BIS group consumed more propofol than patients in the routine care group (Table 2).
Driessen et al. studied the application of a balanced anesthesia (propofol, alfentanil, and N2O) under BIS monitoring and routine care and found that propofol consumption was lower in the BIS group compared to the routine group [38]. Yili-Hankala et al. compared propofol and sevoflurane under BIS and routine care protocols and found less consumption of both propofol and sevoflurane in the BIS monitored group. These studies show that BIS monitoring is helpful for lowering the consumption of propofol during anesthesia [39] which is not the case in our study. Friedberg et al. found that BIS index monitoring decreased propofol consumption by 20% as compared to routine care [40]. Our results show increased the consumption of propofol and fentanyl in the BIS group, which is not consistent with the study by Munoz Garcia et al., who mentions that BIS monitoring allows for reduced consumption of propofol, fentanyl and midazolam [41]. It is obvious that patients in the routine care group have been given a lesser amount of propofol and lesser amount of fentanyl than patients in the BIS Group. This has led to performing light anesthesia and this may be the cause of the patients in the routine care group having had more awareness than the BIS group in the current study.
Somatic Response and Clinical Signs of Awareness
Loss of somatic response due to painful stimuli is defined as no purposeful movement (twisting or jerking of the head, twitching or grimacing). In our study, we found no significant differences in somatic responses of sweating, tearing, pupil dilation and coughing between BIS-monitored and routine care patients. We did note a significant reduction in intra-operational jerking between the BIS-monitored and routine care patients. That BIS is highly useful to prevent painful stimuli and maintain complete loss of somatic response to a nociceptive stimulus.
Time to Extubation
Results of this study show no significant difference in time to extubation between the BIS-monitored and routine care groups. This observation is not consistent with previous studies that
showed that BIS monitoring is associated with reduced time to extubation. Alkire et al. showed that time to extubation was significantly shorter under BIS monitoring than under routine care [37]. Similar results were found by the following studies [35,39,42-44]. Our results are consistent with the study of Sadaqa et al. that showed no significant difference in time to extubation of BIS monitoring and routine care groups in a randomized control study using Bispectral index monitoring during cardiopulmonary bypass surgery [45].
The Recovery Time
In our study, we have been able to reduce time to eye opening but the difference was not significant except in relation to the time of phonation (Table 4). Therefore, the results of the current study are congruent with other studies which have shown that BIS monitoring had little effect on the time needed to recover from anesthesia, measured by eye opening [16,25]. Also, the results of the current study are consistent with those shown by Loveman et al. who studied controlled infusion of propofol and remifentanil under BIS monitoring in neurosurgery patients and found that the BIS monitoring did not impact recovery time [46].
In contrast, in a systematic review study of Punjasawadwong et al. showed that regardless of the anesthetic used, BISguided anesthesia reduced all components of early recovery times, which is the time to open eyes, in response to the voice command, extubation and orientation [24]. We do not also agree with the study conducted by Kruerer et al. who found that the time to open eyes, extubation and arrival to Post Anesthetic Care Unit (PACU) significantly reduced by using the BIS monitoring [33]. Additionally, our results are not consistent with those of Dagtekin et al. who reported that BIS monitoring facilitates stable hemodynamics and provides excellent recovery times for neuro-surgical patients under Total Intravenous Anesthesia (TIVA [47]. The authors propose a limitation of the current study is the total number of participants 59, and most studies of the BIS is performed with a larger number of participants. There may be a small sample size has affected the findings.
Time to Discharge from PACU and Postoperative Symptoms
We found a significant reduction in time to discharge from the PACU for BIS-monitored patients as compared to patients in the routine care group. This result is consistent with the study of Punjasawadwong et al. and Recart et al., which showed that BIS monitoring was associated with shortened duration in the PACU [44,48].
Gan et al. and Song et al. suggest that cerebral monitoring can be useful to improve the titration of the anesthetic, which, in turn, leads to a faster recovery from anesthesia [35,36]. In contrast, previously-mentioned studies by Drover et al. and Recart et al. did not find significant differences in length of stay in PACU or recovery time between BIS-monitored and routine care patients [44,49].
Pavlin showed no impact of BIS-guided anesthesia on time to home readiness after ambulatory surgery, despite a decline in PACU stay. They report that factors other than those related to anesthesia or surgery may have affected time of dismissal after ambulatory surgery. These included fatigue, nausea and vomiting, pain, and lack of immediate access to an escort [50].
Of note, in our study, the mild level of pain (25%) in the RC group as compared with 0% for the BIS group may be associated with the lower dose of fentanyl used for pain relief in the RC group as compared to the BIS Group.
The authors suggest that it is possible that pain was a risk factor that led to the patients in the RC group taking longer to be released from the PACU than those in the BIS group. To compare the results of this study with previous studies of nausea, in the current study, four patients in the BIS group complained of nausea after surgery and 0 patients complained of nausea in the RC group. This result is not consistent with results from Croci et al., which showed that the Bispectral Index-guided anesthesia can reduce postoperative nausea and vomiting [32]. Of note is that the nausea had no effect on the time of discharge of patients in the BIS group from the PACU.
Hemodynamic Parameters
This study showed significant differences in SBP, DBP and MAP at different points of operation between the BIS-monitored group and the routine care group (Table 7). Our results confirm the findings from Mozafari et al. who found that changes in hemodynamic parameters were not dependent on the type of monitoring technology during abdominal surgery [27]. Our results also agree with Payne et al. who reported that the hemodynamic responses during surgery do not decrease with BIS monitoring [51]. The authors suggest that significant differences in SBP, DBP and MAP at different points of operation between the BIS and routine care group were not clinically relevant.
Awareness and Gender, Surgical Time and Age
This study showed no statistically significant association between awareness measurement and gender, surgical time and age. These results are in line with Sebel et al. who showed that age and gender did not affect the incidence of awareness [52]. In the contrary, a study of Katoh et al. found that age strongly affected BIS points. At higher values of BIS, elderly subjects had higher probabilities of response compared to younger patients. Conversely, at lower values of BIS, elderly patients had a lower probability of response [53]. However, our findings are not consistent with those found by Ghoneim, et al. who reported that conscious patients were likely to be younger and women [12]. The authors proposed that, the limitation of the current study with a small sample size that contains different types of surgery that failed to detect the relationship between age, sex and time of surgery with awareness. Further research is needed with a larger sample size that includes the general population of surgical patients undergoing various types of surgery during general anesthesia.
Conclusion
BIS-guided anesthesia (BIS kept at 40-60) reduced the risk of awareness compared to routine care. The main reason for awareness of the RC group can considered a light general anesthetic. In addition, BIS monitoring reduces the usage of volatile anesthesia consumption and the time of discharge from the Post Anesthetic Care Unit.
Implications of BIS Monitoring for Anesthesia Nurses
Use of BIS monitoring is not very popular in a larger number of anesthesia departments (AD) in our country, even though the majority of anesthesiologists and anesthesia nurses working in AD are aware of the availability and function of BIS monitors. It is important that knowledge about improved anesthesia management be moved into the AD setting. BIS monitoring boosts the quality of patient care and should be an element of the standardized clinical practice in operating room settings.
18685
References
- Lyons R (1991) Macdonald.Awareness during caesarean section. Anaesthesia 46: 62-64.
- Todd M (1998) EEGs, EEG processing, and the bispectral index.Anesthesiology 89: 815-817.
- O'Connor MF, Daves SM, Tung A, Cook RI, Thisted R, et al. (2001) BIS monitoring to prevent awareness during general anesthesia. Anesthesiology 94: 520-522.
- Kalkman CJ, Drummond JC (2002)Monitors of depth of anesthesia, quo vadis? Anesthesiology 96: 784-787.
- Igor K (2008) Awareness Under General Anesthesia.Journal of Young Investigators100: 653-661.
- Sammartino M, Volpe B, Sbaraglia F (2010)Thebispectral index- role in pediatric sedation:abrief review. Int J Pediatr 82: 8347 .
- Struys MM1, Smet TD, Versichelen LF, Velde SVD, Broecke RV, et al. (2001) Comparison of closed-loop controlled administration of propofol using Bispectral Index as the controlled variable versus "standard practice" controlled administration. Anesthesiology 95: 6-17.
- Brice DD, Hetherington RR, Utting JE (1970) A simple study of awareness and dreaming during anaesthesia. Br J Anaesth 42: 535-541.
- Liu WH, Thorp TA, Graham SG, Aitkenhead AR (1991) Incidence of awareness with recall during general anaesthesia. Anaesthesia 46: 435-437.
- Moerman N, Bonke B, Oosting J (1993) Awareness and recall during general anesthesia. Facts and feelings. Anesthesiology 79: 454-464.
- Cobcroft M, Forsdick C (1993) Awareness under anaesthesia: the patients’ point of view. Anaesth Intensive Care 21: 837-843.
- Ghoneim MM, Block RI, Haffarnan M, Mathews MJ (2009) Awareness during anesthesia: risk factors, causes and sequelae: A Review of reported cases in the literature. AnesthAnalg 108: 527-535.
- Myles PS, Leslie K, McNeil J, Forbes A, Chan MT (2004) Bispectral index monitoring to prevent awareness during anaesthesia: The B-aware randomised controlled trial. Lancet 363: 1757-1763.
- Hadavi SMR, MDAllahyary E, Asadi S (2013) Evaluation of the Adequacy of General Anesthesiain Cesarean Section by Bispectral Index. IJMS 38: 244-247.
- Brice D, Hetherington R, Utting J (1970)A simple study of awareness and dreaming during anaesthesia. Br J Anaesth 42: 535-542.
- Eger EI II, Sonner JM (2005) How likely is awareness during anesthesia? AnesthAnalg100:1544.
- Aldrete JA (1995)The post anesthesia recovery score revisited [letter]. J ClinAnesth 7: 89-91
- JCAHO (2004) Joint Commission on Accreditation of Healthcare Organizations, Preventing and managing the impact of anesthesia awareness. JtCommPerspect24: 10-11.
- World Medical Association Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects (2013) JAMA 310.
- Ekman A, Lindholm ML, Lennmarken C, Sandin R (2004) Reduction in the incidence of awareness using BIS monitoring. ActaAnaesthesiologicaScandinavica 48: 20-26.
- Chen Z, Liang XU,Ya-qun MA (2011) Bispectral index monitoring prevent awareness during total intravenous anesthesia: a prospective, randomized, double-blinded, multi-center controlled trial. Chin Med J 124:3664-3669
- Sebel PS, Bowdle A, Ghoneim MM, Rampil IJ, Podilla RE (2004) The incidence of awareness during anesthesia: A multicentre U.S. study. AnesthAnalg 99: 833-839.
- Samuelsson P, Lennmarken C (2000) Awareness during anaesthesia: a prospective case study. Lancet 355:707-711.
- Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N (2007)Bispectral index for improving anaesthetic delivery and postoperative recovery (Review). Cochrane Database Syst Rev.
- Sandin RH, Enlund G, Sameuelsson P, Lennmarken C (2000) Awareness during anaesthesia: a prospective case study. Lancet 355: 707-711.
- Bergman IJ, Kluger MT, Short TG (2002) Awareness during general anaesthesia: a review of 81 cases from the Anaesthetic Incident Monitoring Study. Anaesthesia 57: 549-556.
- Mozafari H, Fakhr A, Salehi I, Moghimbigi A (2014). The Ability of Bispectral-Guided Management Compared to Routine Monitoring for Reflecting Awareness Rate in Patients Undergoing Abdominal Surgery. Iran Red Crescent Med J 16: 358-366.
- Avidan MS, Zhang L, Burnside BA, Finkel KJ, Searleman AC, et al. (2008) Anesthesia awareness and the bispectral index. N Engl J Med 1097-1108.
- Messahel FM, Al-Qahtani AS (2003) Awareness during surgery. Saudi Med J 24: 967970.
- Weber F, Seidl M, Bein T (2005) Impact of AEP – Monitor/2-derived composite auditory –evoked potential index on propofol consumption and emergence times during total intravenous anesthesia with propofol and remifentanil in children. ActaAnaesthesiolScand 49: 277-283.
- Bauer M, Wilhelm W, Kraemer T (2004) Impact of bispectral index monitoring on stress response and propofol consumption in patients undergoing coronary artery bypass surgery. Anesthesiology 101:1096-1104.
- Croci M, Panzeri MF, Lepera E, Greco S (2012)Bispectral index-guide anesthesia may reduce postoperative nausea and vomiting. Eur J Anaesthesiol 29:12.
- Kreuer S, Biedler A, Larsen R, Altmann S, Wilhelm W (2003) Narcotrend monitoring allows faster emergence and a reduction of drug consumption in propofol-remifentanil anesthesia. Anesthesiology 99: 34-41.
- LeslieK, Sessler DI, Schroeder M, Walters K (1995)Propofol blood concentration and the Bispectral Index predict suppression of learning during propofol/epidural anesthesia in volunteers. AnesthAnalg81: 1269-1274.
- Gan TJ, Glass PS, Windsor A, Payne F, Rosow C, et al. (1997)Bispectral index monitoring allows faster emergence and improved recovery from propofol, alfentanil, and nitrous oxide anesthesia. BIS Utility Study Group. Anesthesiology 87: 808-815.
- Song D, Joshi GP, White PF (1997) Titration of volatile anesthetics using bispectral index facilitates recovery after ambulatory anesthesia. Anesthesiology 87: 842-848.
- Alkire MT, Hudetz AG, Tononi G (2008) Consciousness and anesthesia. Science 322: 876-880.
- Driessen JJ, Harbers JIBM, Egmond JV, Booij LHDJ (1999) Evaluation of the electroencephalographic bispectral index (BIS) during fentanyl-midazolam anesthesia for cardiac surgery. Does it predict haemodynamic responses during endotracheal intubation and sternotomy? Eur J Anaesthesiol 16: 622-627.
- Yili-Hankala A, Vakkuri A, Annila P, Korttila K (1999)EEG bispectral index monitoring in sevoflurane or propofol anesthesia: analysis of direct costs and immediate recovery. ActaAnaesthesiolScand 43: 545-549.
- Friedberg BL, Sig lJC (1999) Bispectral (BIS) index monitoring decreases propofol usage in propofol-ketamine office based anesthesia. AnesthAnalg 88: S54.
- Garcia JM, Marcos AV, Lozano AR, Garcia CG (2012) Utility of bispectral index monitoring during intravenous sedation in the dental office. Int J Oral Maxillofac Implants 27: 375-382.
- Boztug N, Bigat Z, Akyuz M, Demir S, Ertok E (2006)Does using the bispectral index (BIS) during craniotomy affect the quality of recovery? J NeurosurgAnesthesiol 18:1-4.
- Burrow B, McKenzie B, Case C (2001) Do anaesthetized patients recover better after bispectral index monitoring.Anaesth Intensive Care 29: 239-245.
- Recart A, Gasanova I, White PF, Thomas T, Ogunnaike B, et al. (2003) The effect of cerebral monitoring on recovery after general anesthesia: a comparison of the auditory evoked potential and bispectral index devices with standard clinical practice. AnesthAnalg 97: 1667-1674.
- Sadaqa WA, Yahia SH, Othman W (2016) Intra-operative use of Bispectral Index Monitoring and Time to Extubation and Patients Length of Stay after Cardio Pulmonary Bypass Surgery, at An-Najah National University Hospital / Nablus / Palestine. A Randomized Control Study. J Biomedical Sci 5:3.
- Loveman E, Hooff JCV, Smith DC (2001)The auditory evoked response as an awareness monitor during anesthesia. Br J Anesth 86: 513-518.
- Dagtekin O, Berlet T, Delis A, Kampe S (2007)Manually controlled total intravenous anesthesia augmented by electrophysiologic monitoring for complex stereotactic neurosurgical procedures. J NeurosurgAnesthesiol 19: 45-48.
- Punjasawadwong Y, Boonjeungmonkol N, Phongchiewboon A (2007)Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev CD003843.
- Drover DR, Lemmens HJ, Pierce ET (2002) Patient state index: titration of delivery and recovery from propofol, alfentanil, and nitrous oxide anesthesia. Anesthesiology 97: 82-89.
- Pavlin DJ, Rapp SE, Polissar NL, Malmgren JA, Koerschgen M, et al. (1998) Factors affecting discharge time in adult outpatients. AnesthAnalg 87: 816-824.
- Payne S, Selb J, Boas DA(2009) Effects of autoregulation and co2 reactivity on cerebral oxygen transport. Ann Biomed Eng 37: 2288-2298.
- Sebel PS, Bowdle TA, Ghoneim MM, Rampil IJ, Padilla RE, et al. (2004)The incidence of awareness during anesthesia: a multicenter United States study. AnesthAnalg 99: 833-839.
- Katoh T, Bito H, Sato S (2000) Influence of age on hypnotic requirement, bispectral index, and 95% spectral edge frequency associated with sedation induced by sevoflurane. Anesthesiology 92: 55-61.