Leonard G Trujillo*
Department of Occupational Therapy, East Carolina University, USA
*Corresponding Author:
Leonard G. Trujillo
Professor, Chair, Department of Occupational Therapy
East Carolina University, 600 Moye Blvd, HSB
3305, MS 668 Greenville, NC 27858, USA
Tel: 01-252-744-6195, 01-252-26-58-0363
Fax: 01-252-744-6198
E-mail: trujillol@ecu.edu; donleonardo@aspenslope.com
Received date: March 31, 2017; Accepted date: April 17, 2017; Published date: April 20, 2017
Citation: Trujillo LG. The Effectiveness of Interactive Metronome® as a Restorative Modality to Improve Cognition and Motor Performance in Healthy Older Adults in Eastern North Carolina. J Neurol Neurosci 8:2. doi:10.21767/2171-6625.1000186
Keywords
Occupational therapy; Interactive metronome; Cognitive rehabilitation
Introduction
The rate of growth for adults over the age of 65 is irrefutable. The population for adults aged 65 and over has increased from 35.9 million in 2003 to 44.7 million in 2013; it is projected to more than double to 98 million in 2060 [1]. As the population grows, the need for research on healthy aging adults living in their community becomes greater. Research should address how to improve functioning of adults with impairments, but it should also focus on prevention of functional decline due to aging.
The Occupational Therapy Practice Framework (OTPF): Domain and Process 3rd Edition (OTPF) highlights the need for, “preservation of occupational identity for those who are at risk for developing an illness, injury, disease, disorder, condition, impairment, disability, activity limitation or participation restriction” (American Occupational Therapy Association [AOTA]) [2]. Additionally, the International Classification of Functioning, Health and Disability (ICF) offers a model for describing functioning and disability; two of the major components addressed in the model are activities and participation. Activities and participation are described in terms of the amount of participation and the restrictions of the individual based on functioning as per the World Health Organization (WHO) [3]. Similarly to the Occupational Therapy Practice Framework (OTPF), the ICF outlines the importance of viewing an individual’s participation as a primary determinant of health, and highlights the need for prevention to be a component of intervention as per WHO, in 2002. In order to successfully address the needs of healthy aging adults, it is important to support participation in activities that promote well-being and enhance self-efficacy so they may live longer within their communities. Occupational therapists can bolster the health of populations in need through utilizing preventative methods, rather than focusing primarily on rehabilitative methods [4,5].
Problem
There is a growing initiative to support older adults aging in the community. Due to the high rate of growth among this population, more research needs to examine interventions that support healthy aging in the community [6,7]. Cognitive decline is a typical occurrence in the aging adult, and these cognitive changes can impact Healthy Older Adult’s (HOA) ability to problem-solve and process information efficiently, potentially impacting Activities of Daily Living (ADL) and Independent Activities of daily Living (IADL) participation [8]. Participation in occupations such as ADLs and IADLs is associated with independence [9], and in order to perform ADLs and IADLs, individuals must employ the use of executive functions, attention, memory, fine and gross motor skills [10-12]. Mild cognitive impairments may disrupt many of these everyday tasks making it challenging for older adults to live independently [10,13]. Research is lacking in the area of intervention methods which can be utilized by therapists to support HOAs, prevent cognitive decline, and maintain functional performance in ADLs and IADLs [14,15].
Purpose
The purpose of this study was to examine the relationship between healthy older adults’ participation in a restorative modality, Interactive Metronome® (IM) and participant scores on tests of cognition and motor abilities. Healthy normal aging adults were choses as this age group has been identified as seeking to make use and be as healthy as possible in their golden years of retirement. As the population grows, the need for research on healthy aging adults living in their community becomes greater. Research should address how to improve functioning of adults with impairments, but it should also focus on prevention of functional decline due to aging [1,16]. The IM was chosen as the training tool because it provides a standardized measurement that will be compared to the assessments included in the study. Fifteen healthy older adults completed 18 sessions of IM protocol and researchers gathered data from IM assessments, d2 Test of Attention, and Nine Hole Peg Test across four points of measure; a total of 30 participants completed 12 intervention sessions and 3 points of evaluation Schaffer et al. [17] explains IM is an evidencebased tool that improves timing, rhythm and synchronization in the brain which can support motor planning and sequencing. Koomar et al. [18] states because of the potential impact on synchronization, IM may be a beneficial tool to combine with other interventions to support skills such as motor planning and sequencing in various diagnoses. The IM was selected as a research tool for this study because research indicates a positive relationship between IM participation and scores on tests of motor abilities, attention, and other cognitive functions in various populations including attention deficit hyperactivity disorder, cerebral vascular accident, traumatic brain injury, and coordination disorders [17-21]. The IM is a brain-based assessment and treatment tool that focuses on improving motor planning and sequencing through the use of rhythm, timing, and synchronization of motor movements [22]. A typical IM session involves the client standing or sitting with headphones on, and a trigger attached to the hand glove. The individual be looking at a computer screen which provides visual feedback during the exercise [23]. Attention is identified as being one of the most basic functions of the human brain and some theories suggest it is the basis for many other cognitive functions [24], and motor abilities enable adults to maintain independence as they age [11]. Therefore, researchers hope to examine the use of IM in the HOA population to support prevention of cognitive and motor decline.
Methodology
A review of quasi experimental designs was undertaken and subsequently a repeated-treatment design was developed and employed for this study. Specifically the study introduces a treatment period, removes the treatment for a set period of time and reintroduces the treatment over time. Thus a 01 × 02 × 03 × 04 nomenclature is used. William Shadish et al. [25] makes references to the use of this design in discusses the design’s positive removal of threats to validity of outcomes. There was no control group; each participant established a baseline for their individual performance [26]. The IM served as an intervention tool and assessment tool. In addition to the Long Form Assessment (LFA); other assessments included in were measures of cognitive skills and fine and gross motor abilities. The d2 Test of Attention (d2) addressed the cognitive components; the Nine Hole Peg Test (NHPT) assessed fine motor changes.
Prior to data collection, IRB approval was granted. The PI recruited participants living in a local continual care retirement community in eastern, NC. Interested individuals were screened to determine if they met the inclusion and exclusion criteria. All selected participants received and signed the informed consent form.
IM developers and researchers suggested that in order for the treatment to be effective, the participant should receive treatment three times per week for a minimum of thirty minutes per session. However, researchers were interested in assessing if performance changes could occur with less duration and frequency so treatment sessions were modified from a previous research project to fit the needs of the healthy older adult population and included 9 tasks. These Tasks were submitted as part of the protocols reviewed in the IRB approval process. They involved Upper Body Movement patterns where they were hitting a trigger in conjunction with the IM as an example two handed clapping motion with a trigger switch in their dominant hand; single handed right/life clapping on the side of the body; alternating hands crossing one’s midline in a diagonal movement with touch switches on each side, etc. In the current study participants completed only two sessions per week and the shortest session was 15 minutes; progressing to 35 minutes in length. Changes were made based on the individual’s ability to respond and sense of endurance for the day.
Analysis and Results
In addition to the Paired t-test analysis that was run, which had indicated a clear significance in change both in cognitive changes for attention and attention to detail as well as improved fine motor skills, a repeated measures analysis was run. This was possible due to the four different measurements acquired during the 3 Phases of the study. As anticipated from the results of the t-tests run the repeated measures analysis provided significance at the p=0.001 level at each of the outcomes measurement level with each of the 3 different measurements. The NHPT was lower in its output change, but as one was familiar with the raw measurements of performance on the NHPT it was typically less than 3 seconds of change that made a normative change for evaluation purposes.
A final comparison was run between the group that completed just the first session of training to the group that completed both the Phase I and Phase III treatment interventions. In the analysis, there was a much smaller indication in significance in change between final outcomes indicating that clients did make minor improvements p= 0.049 as compared to the p=0.001 value change from Pre-test A => B or A = > D. The change from B = >D was much less substantial.
Discussion
It is important to recall that the participants of this study self-identified themselves as living healthy normal status within their aging process. A number had pre-morbid conditions that they were living with, as part of their normal life style. Yet, we see notable, significant change on both the IM Long Form Assessment and the standardized evaluation tools used in this study.
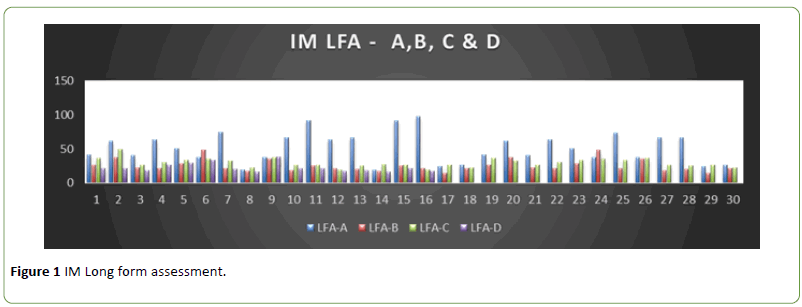
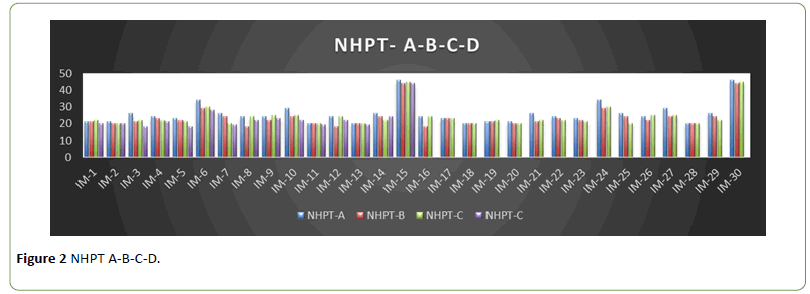
In Figure 1 IM Long Form Assessment, one can see the progress of change in a downward movement on each client. These downward scores are positive improvements indicating improved skill levels. These are the raw scores obtained by the participants. The first 15 completed the all 3 Phases of the Study and the last 15 completed the initial intervention and post-test 6-8 weeks out from the treatment interventions. One can easily see the positive outcomes on the assessment scores. The same graphic view can be seen with the raw scores obtained on the Nine Hole Peg Test as illustrated in Figure 2 NHPT A-B-C-D, where A-B-C-D represent the assessments taken.
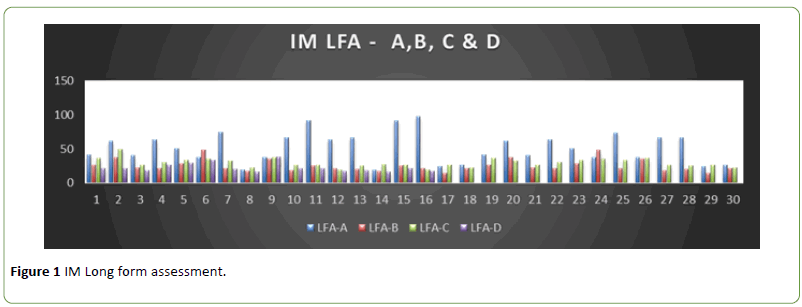
Figure 1: IM Long form assessment.
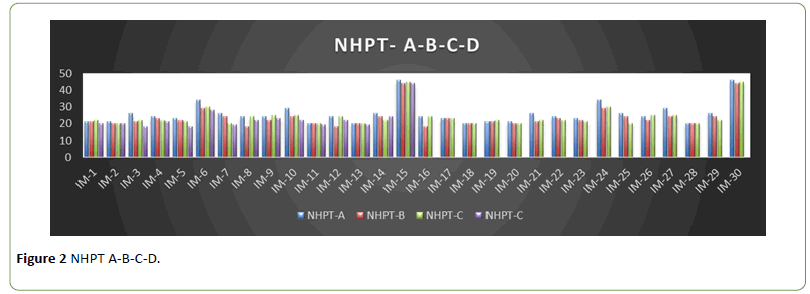
Figure 2: NHPT A-B-C-D.
The participants related anecdotally that the changes they experienced were subtle changes in their daily lives. Such things as “feeling more organized”; balancing their check book seemed easier; signing their name more legibly; enjoyed the water aerobics classes with more confidence. Indications are that participants reached a positive change in status and were able to maintain that level with little statistical change of a 6-8 weeks break, regained their original improves and made a measureable change in their new level of performance, though not substantial in comparison.
Conclusion
The use of the Interactive Metronome as an effective modality in maintaining, enhancing and improving basic daily life tasks appears to be plausible. While the study has a small population and there was no control group, the outcomes measured over time appear to be more than just improvements based on learning curves or by chance [25]. The type of improvements noted in the participant’s daily activities come as gradual changes that are incorporated into their level of ability and performance, sometimes without notice [27]. This is much the same way we fail to see our decline in performance as we age and find that looking over one’s shoulder as you pull out of the driveway is more difficult than it used to be. This study leads us to believe it would be important to do a larger study with varying locations and include more functional evaluations that are related to an individual’s ability to perform and their satisfaction of performance particularly in regard to their ADLs and IADLs. The IM may be incorporated into therapy for healthy older adults as a preventative and restorative modality, with healthy older adults showing signs of cognitive decline in order to gain more insight into the impact of IM on improving cognition, and functional performance.
Acknowledgements
The author would like to acknowledge Rebekah Reilly MS, OTR and Lauren Christy OTR for their support in the partial data collection of this study.
18926
References
- Department of Health and Human Resources Administration on Aging (2014) Aging statistics.
- American Occupational Therapy Association (2014) Occupational therapy practice framework domain and process (3rd edn). American Journal of Occupational Therapy 68: S1-S48.
- World Health Organization (2007) International classification of functioning, disability and health. Geneva: World Health Organization.
- Metz WC, Lamb AJ (2013) Occupational therapy in prevention and wellness: Retaining relevance in a new health care world. Am J OccupTher 67: 266-271.
- Metz A, Robnett R (2011) Engaging in mentally challenging occupations promotes cognitive health throughout life. Gerontology Special Interest Section Quarterly 34: 1-4.
- Bacsu J, Jeffery B, Novik N, Abonyi S, Oosman S, et al. (2014) Policy, community and kin: Interventions that support rural healthy agingactivities. Adaptation and Aging 38: 138-155.
- Orellano E, Colon WI, Arbesman M (2012) Effect of occupation- and activity-based interventions on instrumental activities of daily living performance among community-dwelling older adults: A systematic review. Am J OccupTher 66: 292300.
- Glover JS, Wright J (2013) Special needs of the older adult. In H. M. Pendleton and W. Schultz-Krohn (Eds.), Pedrettis occupational therapy practice skills for physical dysfunction. St. Louis, MS: Mosby Elsevier, NY. 7: 1228-1245.
- Hertzog C, Kramer F, Wilson R, LindenbergerP(2009) Enrichment effects on adult cognitive development: Can the functional capacity of older adults be preserved and enhanced? PsycholSci Public Interest 9: 1-65.
- Burton CL, Strauss E, Hultsch DF, Hunter MA (2006) Cognitive functioning and everyday problem solving in older adults. ClinNeuropsychol 20: 432-452.
- Dayanidhi S, Valero-Cuevas FJ (2014) Dexterous manipulation is poorer at older ages and is dissociated from decline of hand strength. J Gerontol A BiolSci Med Sci 69: 1139-1145.
- Incel N, Sezgin M, As I, Cimen O, Sahin G (2009) The geriatric hand: Correlation of hand-muscle function and activity restriction in elderly. Int J Rehabil Res 32: 213-218.
- Felix HC, Adams B, Cornell CE, Fausett JK, Krukowski RA, et al. (2014) Barriers and facilitators to senior centers participating in translational research. Res Aging 36: 22-39.
- Fratiglioni L, Paillard-Borg S, Winblad B (2004) An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol 3: 343-353.
- Green CS, Bavelier D (2008) Exercising your brain: A review of human brain plasticity and training-induced learning. Psychology and aging 23: 692.
- US Department of Health and Human Services (2014) Administration for community living and Administration on aging: A profile of older Americans.
- Shaffer RJ, Jacokes LE, Cassily JF, Greenspan SI, Tuchman RF, et al. (2001) Effect of Interactive Metronome training on children with ADHD. Am J OccupTher 55: 155-162.
- Koomar J, Burpee JD, DeJean V, Frick S, Kawar MJ, et al. (2001) Theoretical and clinical perspectives on the interactive metronome: A view from occupational therapy practice. Am J OccupTher 55: 163-166.
- Cosper S, Lee G, Peters S, Bishop E (2009) Interactive Metronome training in children with attention deficit and developmental coordination disorders. Int J Rehabil Res 32: 331-336.
- Nelson LA, Macdonald M, Stall C, Pazdan R (2013) Effects of interactive metronome therapy on cognitive functioning after blast-related brain injury: A randomized controlled pilot trial. Neuropsychology 27: 666-679.
- Shank TM, Harron W (2015) A retrospective outcomes study examining the effect of interactive metronome on hand function. J Hand Ther 28: 396-402.
- Interactive Metronome (2007) IM certification provider training manual. Interactive Metronome. Inc.
- Interactive Metronome (2015) Certification: Interactive metronome for pediatrics and adults. IM Certification Course; Raleigh, NC.
- Gillen G (2013) Evaluation and treatment of limited occupational performance secondary to cognitive dysfunction. In H. M. Pendleton and W. Schultz-Krohn (Eds.), Pedrettis occupational therapy practice skills for physical dysfunction. St. Louis, MS: Mosby Elsevier, NY.7: 648-677.
- Shadish WR, Cook TD, Cambell DT (2002) Experimental and quasi-experimental designs for generalized causal inference.Boston: Houghton Mifflin. pp: 113-114.
- Cook TD, Campbell DT (1979) Quasi-experimentation: Design and analysis for field settings. Rand McNally, Chicago, Illinois.
- Bontje P, Kinbanian A, Josephsson S, Tamura Y (2004) Occupational adaptation: The experiences of older persons with physical disabilities. Am J OccupTher 58: 140-149.