Ahmed M Moeen* and Diaa A Hameed
Oncological Urology Unit, Urology and Nephrology Hospital, Assiut, Egypt
*Corresponding Author:
Ahmed M. Moeen
Oncological Urology Unit, Urology and Nephrology Hospital, Assiut, Egypt
Tel: 00201003960931
Email: moeen3@yahoo.com
Received date: March 20, 2017; Accepted date: March 29, 2017; Published date: March 31, 2017
Citation: Moeen AM, Hameed DA. The Orthotopic Neobladder: Does the Length of the Isoperistaltic Limb Matter?. Arch Can Res. 2017, 5:1. doi:10.21767/2254-6081.1000137
Introduction
Radical cystectomy and urinary diversion is the standard treatment for muscle invasive bladder cancer and some cases of T1G3 who failed intravesical therapy. The orthotopic neobladder is the summit of all urinary diversions as it is physiologically close to the normal bladder and provides a superior quality of life compared to other types of diversion [1].
Several techniques for neobladder reconstruction were described. The uretero-enteric anastomosis is a very critical step, if improperly done it puts the upper urinary tract at risk. The application of anti-reflux technique is debated [2]. The use of an isoperistaltic limb (chimney) for uretero-enteric anastomosis is a well-known technique to overcome reflux and other difficulties as short ureters, short intestinal mesentery and short urethral stump [3]. However, the length of the isoperistaltic limb is a matter of controversy.
Originally, Studer et al. stated that a 20 cm isoperistaltic ileal segment can prevent reflux by transmission of the intraabdominal pressure on this afferent segment during voiding using Valsalva maneuver [4]. However, during his first 20 years of experience, he minimized this length to 14 cm to 16 cm [5]. Moreover, Hautmann modified his original technique and performed the anastomosis of the ureters to a short isoperistaltic limbs about 3 cm to 5 cm in a freely refluxing end to end manner instead of Le Duc anti-reflux procedure. This decreased the incidence of stenosis from 9.5% to only 1% [6].
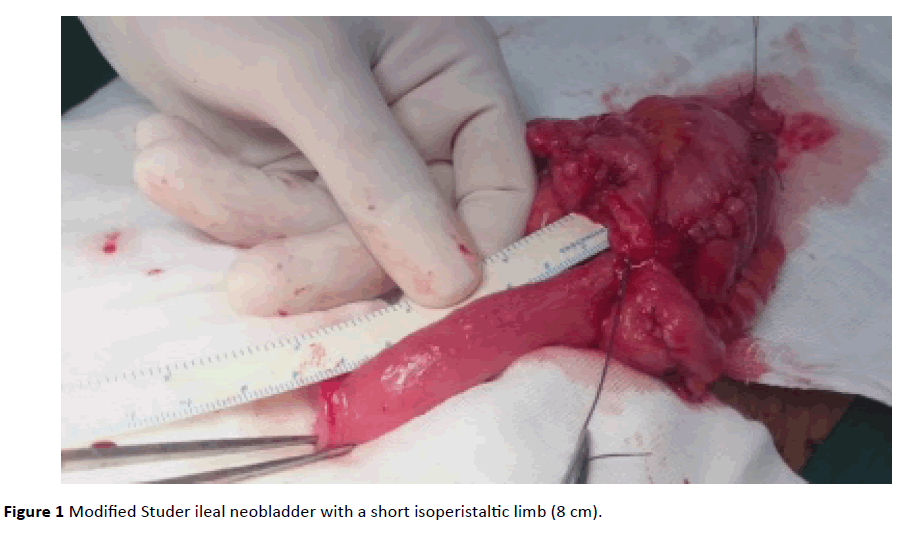
In 2016, we published our report about the functional evaluation of a modified Studer ileal neobladder (Moeen’s modification) using only 40 cm of ileum, 32 cm for the reservoir and 8 cm as a short isoperistaltic limb for direct ureteral re-implantation (Figure 1). In this study, we tested the notion that a short chimney will not increase the incidence of reflux [7].
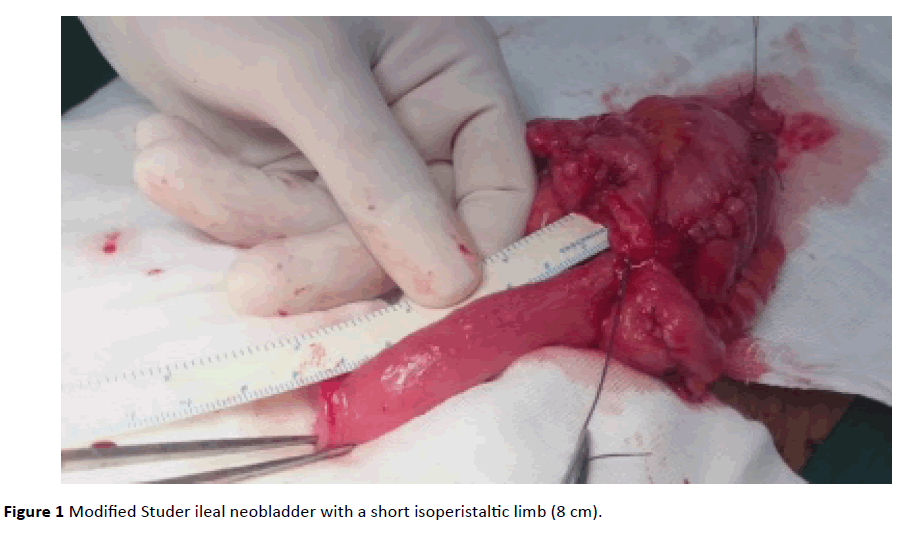
Figure 1 Modified Studer ileal neobladder with a short isoperistaltic limb (8 cm).
Discussion
Our rational in using a shorter chimney is that reflux prevention – which necessity is controversial – does not depend solely on the length of chimney. Hence, a shorter one will allow more preservation of the intestine and preservation of the lower segment of the ureters which participate in reflux prevention [5,6]. It was shown that the pressure in the lower segment of the ureters is about 20 cm to 30 cm H2O which is enough to compate the bladder end filling pressure at a capacity of 450 ml which is 20 cm H2O [8].
In addition, reflux did not occur in many direct anastomoses and if occurred it does not significantly alter the renal function [9]. Also, as the functional capacity of the reservoir increases over time, the probability of reflux decreases. Moreover, voiding after neobladder reconstruction occurs by Valsalva creating a higher intra-abdominal pressure that is evenly transmitted on the reservoir, chimney, ureters and renal pelves decreasing the incidence of reflux [10].
Despite the short length of the isoperistaltic limb we used, six patients only (10.3%) had reflux (3 unilateral and 3 bilateral, all of them had normal renal function) and 1 patient developed uretero-intestinal anastomotic stricture.
Conclusion
In conclusion, there are multiple factors affecting the occurrence of reflux. We believe that a freely refluxing ureteral anastomosis to this short isoperistaltic limb is feasible, safe and with no harmful effect on the renal function.
18818
References
- Gakis G, Stenzl A (2010) Ileal neobladder and its variants. European Urology Supplements 9: 745-753.
- Hautmann RE, Abol-Enein H, Hafez K, Haro I, Mansson W, et al. (2007) World Health Organization (WHO) Consensus Conference on Bladder cancer and Urinary diversion. Urology 69: 17–49.
- Pantuck AJ, Han KR, Perrotti M, Weiss RE, Cummings KB (2000) Uretero-enteric anastomosis in continent urinary diversion: long term results and complications of direct versus non-refluxing techniques. J Urol 163: 450 –455.
- Studer UE, Spiegel T, Casanova GA, Springer J, Gerber E, et al. (1991) Ileal bladder substitute: Anti-reflux nipple or afferent tubular segment? Eur Urol 20: 315–326.
- Studer UE, Burkhard FC, Schumacher M (2006) Twenty years’ experience with an ileal orthotopic low pressure bladder substitute, lessons to be learned. J Urol 176: 161–166.
- Hautmann RE (2010) Surgery Illustrated – Surgical Atlas. Ileal Neobladder. BJU International 105: 1024–1035.
- Moeen AM, Hameed DA, Gadelkareem RA, Abdelsalam YM, Abdel-Hafez SES, et al. (2016) Functional evaluation of a modified Studer ileal neobladder. AFJU 22: 153–161.
- Buzelin JM (1993) Physiologie et explorations fonctionnelles de la voie excretrice urinaire. Rapport au 87e`me Congre`s Francais d’Urologie, Paris, France.
- Helal M, Pow-Sang J, Sanford E (1993) Direct (non-tunneled) uretero-colonic re-implantation in association with continent reservoirs. J Urol 150: 835.
- Hautmann RE, Volkmer BG, Schumacher MC, Gschwend JE, Studer UE (2006) Long-term results of standard procedures in urology: The ileal neobladder. World J Urol 24: 305–314.