Sanou M1, Ky/Ba A2, Tamini/Toguyeni L2, Ouedraogo A-S3, Konkobo A4, Bakiono F12, Compaore T R4,9, Nagalo B M4,8*, Bissye C10, Yokoda R8, Borad M J8, Sanou I6, Sangare L7, Ouedraogo/Traore R1, Simporé J11
1Pediatric University Hospital Charles De Gaule, Ouagadougou, Burkina Faso, West Africa
2National Public Health Laboratory, Ouagadougou, Burkina Faso, West Africa
3University Hospital Souro-Sanou, Bobo-Dioulasso, Burkina Faso, West Africa
4University Ouagadougou, Burkina Faso, West Africa
5National Office of Public Health, Ouagadougou, Burkina Faso, West Africa
6University Hospital Blaise Compaoré, Ouagadougou, Burkina Faso, West Africa
7UniversityHospitalYalgado Ouedraogo, Ouagadougou Burkina Faso, West Africa
8Department of Hematology/Oncology, Mayo Clinic Scottsdale, AZ, USA
9Muraz Research Center, Bobo-Dioulasso, Burkina Faso, West Africa
10Laboratory of Cellular and Molecular Biology, University of Franceville, BP 943, Franceville, Gabon
11Pietro Annigoni Biomolecular Research Center (CERBA), Department of Biochemistry-Microbiology, University of Ouagadougou, West Africa
12Armed Forces Health Service, Ouagadougou, Burkina Faso, West Africa
Corresponding Author:
Pr Jacques Simporé
Pietro Annigoni Biomolecular Research Center (CERBA)
Department of Biochemistry-Microbiology
University of Ouaga I Prof Joseph Ki Zerbo
Tel: +22670230792
E-mail: jacques.simpore@yahoo.fr
Received Date: February 08, 2018; Accepted Date: February 12, 2018; Published Date: February 16, 2018
Citation: Sanou M, Ky/Ba A, Tamini/Toguyeni L, Ouedraogo A-S, Konkobo A, et al. (2018) Treatment and Management of Bacterial Purulent Acute Otitis at the Bogodogo District Community Hospital, Burkina Faso, West Africa. Arch Clin Microbiol. Vol.9 No.1:75 doi:10.4172/1989-8436.100075
Copyright: © 2018 Sanou M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
PAOM; Bacteria; Antibiotics sensitivity; Resistance; Burkina Faso
Introduction
Purulent acute otitis media (PAOM) refers to a group of inflammatory disease of the middle ear caused by either bacterial or viral infection, often characterized by a purulent or mucopurulent effusion in the tympanic body [1-3]. Along with nasopharyngitis, PAOM is one of the leading causes of antibiotic prescriptions in children [3-5]. In Burkina Faso, ear infections are among the top 10 reasons for consultation in medical centers [6]. In 2012, the otorhinolaryngology unit (ORL) of the Bogodogo district community hospital reported 542 cases of PAOM with 41.1% (223) of patients aged 14 years and older [7]. Infection of the middle ear can in chronic and complicated forms affect some of the organs near the mastoid cavities including the facial nerve or the inner ear but also extend to the skull and cause neurological disorders [8].
Unfortunately, the increasing number of PAOM cases is correlated with the increase of antibiotic-resistant bacterial strains due in large part to extensive unnecessary prescriptions [9]. Indeed, in the 1950s, the supposedly bacterial origin of PAOM led to the systematic prescription of available antibiotics, which caused the emergence of antibiotic-resistant germs and therapeutic failures [10]. This situation has led to a complete reformulation of the treatment regimens, including the choice of molecules to be prescribed in developed countries such as France. As a direct consequence, the French agency for health products Security (AFSSAPS) has developed a guideline of recommendations to standardize the management of acute otitis media to further reduce the rate of bacterial resistance [10]. According to the agency, the main causative organisms are Streptococcus pneumoniae, Haemophilus influenzae, Moraxella (Branhamella) catarrhalis, while studies in sub-Saharan African countries, particularly in Burkina Faso, have found that the main germs observed were enterobacteria, staphylococci and Pseudomonas [1]. In Sub-Saharan Africa, the odds that patients would be prescribed the wrong antibiotic are higher than anywhere else due to the lack of national regulations that direct physicians, variations in bacterial epidemiology and strains [11]. Therefore underlying the need of constantly update healthcare workers in current bacterial species that are treatment resistant. This study aimed to provide relevant clinical data on antibiotic-resistant germs for the treatment of PAOM with the goal of improving patient outcomes in Burkina Faso.
Materials and Methods
Patients’ recruitment
This was a cross-sectional descriptive study that focused on the ear pus collections of patients consulted in the ORL of the Bogodogo district community hospital from June 2014 to January 2015. These samples were analyzed at the National Laboratory of Public Health. Patient’s informed consents were obtained in a written form from adults or guardians. Sampling was non-probabilistic, patients were systematically recruited when the diagnosis of PAOM was made and there was no ongoing antibiotic therapy. A sample of pus was collected using two sterile cotton swabs. One was used to make smears for fresh microscopic examination and Gram staining and the other for bacterial culture.
Bacteria isolation and identification
The bacteriological examination consisted of making cytobacteriological analysis of the ear pus samples. These analyze included macroscopic and microscopic examination.
Contamination-free bacteria growth media was used to isolate colonies. Samples were seeded on a brain heart infusion broth and incubated at 37°C for 24 hours. Suspected germs were reseeded on a specific agar. Chocolate Agar with IsoVitalex was used for Hæmophilus influenzae, Moraxella catarrhalis and Staphylococcus. Eosin Methylene Blue (EMB) for Gram-negative Enterobacteriaceae and Gram-negative Bacilli. Other media such as Cysteine Lactose Deficient in Electrolytes (CLED), DNase, Müller Hinton (MH), Sabouraud, and Chapman were used depending on the Gram results and the results of the primary culture. Experiments were carried out following the European Society of Clinical Microbiology and Infectious Diseases guidelines. Bacterial isolation and identification were performed based on morphological, cultural, biochemical and antigenic features.
In the presence of Gram-positive cocci, catalase status detected (with hydrogen peroxide) to differentiate between streptococci and staphylococci (staphylococci are catalase producers). Thus negative catalase indicates the presence of Streptococci and positive catalase will most likely indicate the presence of staphylococci. To further confirm the presence of Staphylococci, a Chapman medium was used along with DNase test. S. aureus is Chapman, Mannitol and DNase positive. Chapman contains mannitol, 7.5% NaCl and phenol red as a pH indicator. It is red in color but can turn yellow when mannitol is fermented by S. aureus. S. saprophyticus is Chapman and Mannitol positive finally S. epidermidis is Chapman positive. For Gram-negative bacilli: an oxidase test was performed to distinguish between Enterobacteria on the one hand, and Pseudomonas and Haemophilus on the other hand.
When the oxidase is positive, a re-isolation is done on the CLED agar (Cystine-Lactose-Electrolyte-Deficient Agar) for the research of Pseudomonas aeruginosa (makes it possible to better visualize the appearance of a green coloring: pyoverdine). The identification is confirmed by the determination of the biochemical characteristics using the API 20 E gallery (Bio- Mérieux). The growth factors X and V were used when the presence of Haemophilus was suspected (coco bacilli or Gramnegative polymorphic bacilli).
The antibiotic sensitivity screening used the KIRBY-Bauer method using diffusion on agar medium, according to guidelines (2013) of the French Society of Microbiology Antibiogram Committee (CA-SFM).
Statistical analysis
The data was recorded with Microsoft office Excel 2017 and analyzed with the CSpro version 5.0.
Ethical considerations
This study was approved by the National Public Health Laboratory of Burkina Faso Ethics Committee. Informed consent was obtained from adults and parents or guardians of individuals under 18 years old.
Results
For eight months, 64 cases of acute purulent otitis media were collected at the ORL department of the Bogodogo district hospital. Patients were aged from 1 month to 70 years with an average age of 22 years and a sex ratio of 1.32. The majority Patients were over 15 years of age (53.4%), followed by children under the age of 04 who accounted for almost a quarter of the sample (25.9%). Of the 64 samples from PAOM 62 had a positive culture with 96.9% of positivity rate. A total of 62 bacteria (13 bacterial species) and six (06) yeasts were identified.
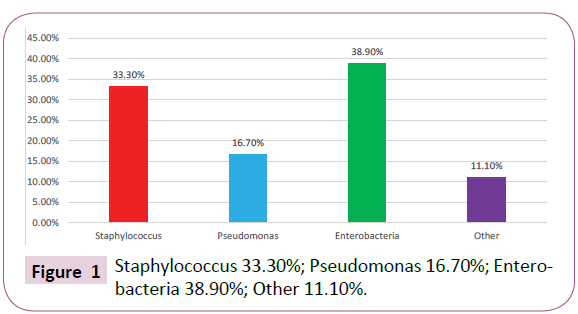
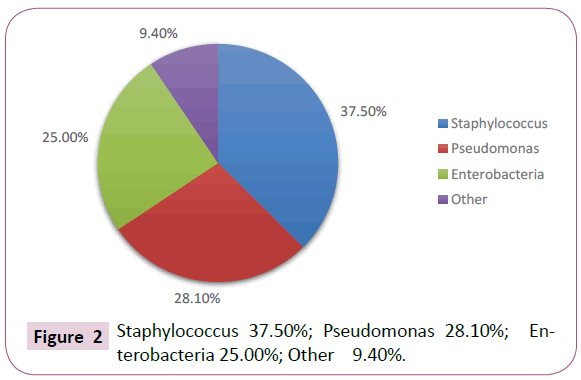
Most of the bacteria observed were Staphylococci (37.1%), followed by Enterobacteriaceae (32.2%) and Pseudomonas (22.6%) Table 1. When considering age, Enterobacteriaceae were predominant in patients younger than 4 years Figure 1 and Staphylococci were predominant in patients over the age of 15 Figure 2. Among the bacterial species, whatever the age, Staphylococcus aureus (35.5%) was the predominant species, followed by Pseudomonas aeruginosa (16.1%) and Escherichia coli (11.3%).
| |
0-3 years |
4-6 years |
7-14 years |
≥15 years |
Total |
| Staphylococcus |
6 |
5 |
0 |
12 |
23 |
| Pseudomonas |
3 |
1 |
1 |
9 |
14 |
| Enterobacteries |
7 |
5 |
0 |
8 |
20 |
| Other |
2 |
0 |
0 |
3 |
5 |
| Total |
18 |
11 |
1 |
32 |
62 |
Table 1: Bacterial repartition by age.
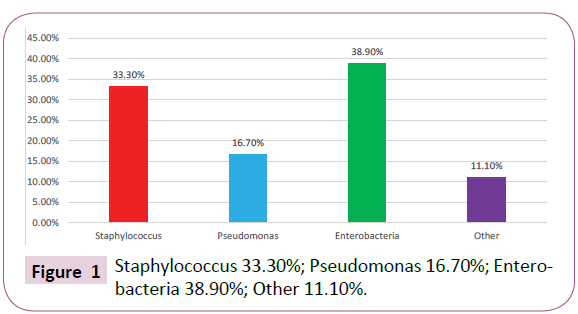
Figure 1: Staphylococcus 33.30%; Pseudomonas 16.70%; Enterobacteria 38.90%; Other 11.10%.
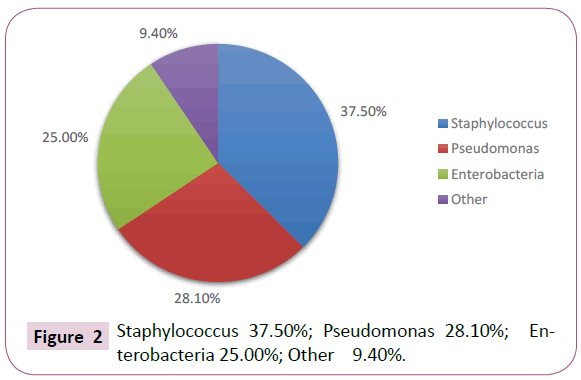
Figure 2: Staphylococcus 37.50%; Pseudomonas 28.10%; Enterobacteria 25.00%; Other 9.40%.
In general, isolated bacteria had good sensitivities for four (4) antibiotics, namely Ciprofloxacin (97%), Gentamicin (98%), Imipenem (82%) and Ceftriaxone (76%). The sensitivity to other antibiotics was 47% for Cotrimoxazol, 3% for Ampicillin and 18% for Amoxicillin + clavulanic acid. In spite of the latter, there was a strong resistance noted with the use of Ampicillin (94%), Erythromycin (77%) and Amoxicillin + Clavulanic acid (74%). Depending on the organisms, susceptibility to antibiotics varied from one bacterium to another. Staphylococci were sensitive to Ciprofloxacin (100%), Gentamicin (100%) and Ceftriaxone (96%). However, their sensitivity was low with the antibiotics commonly used in particular with Ampicillin (00%), Amoxicillin plus (+) clavulanic acid (17%) and 57% with Cotrimoxazol. Enterobacteriaceae showed 100% sensitivity to Gentamicin, 95% to Ciprofloxacin, 85% to Imipenem, 60% to Cotrimoxazol, 10% to Ampicillin, and 35% to Amoxicillin + clavulanic acid. If all Pseudomonas were sensitive to Ciprofloxacin, none was affected by Ampicillin and Amoxicillin + clavulanic acid. However, we obtained a sensitivity of 64% to Ceftriaxone, 42% to Imipenem, 93% to Gentamicin and 7% to Cotrimoxazol.
For the other bacteria, no sensitivity was noted with Ampicillin and Amoxicillin + clavulanic acid. Also, their sensitivity were 100% to Gentamicin, 80% to Ciprofloxacin and Imipenem, 60% to Cotrimoxazol and 20% to Ceftriaxone.
In our sample, bacterial associations were observed. Those associations involved Staphylococcus aureus with four bacteria and one yeast Table 2.
| Associations |
Number |
| Staphylococcus aureus + Candida Sp |
3 |
| Staphylococcus aureus + Escherichia coli |
2 |
| Staphylococcus aureus+ Acinetobactersp. |
1 |
| Staphylococcus aureus + Klebsiellapneumoniae |
1 |
| Staphylococcus aureus + Enterobacter sp. |
1 |
Table 2: Observed bacterial associations.
Discussion
In the present study, male patients were the most represented, with 56.9% of cases, and a sex ratio of 1.32. According to database of Burkina Faso Ministry of Health, the same observation was done with a higher sex ratio (1.8) [6]. Of the 64 cultures performed, the positivity rate was 96.9%. This high rate is partly related to the conditions of inclusion in our study which only took into account patients without antibiotic therapy. This strong crop positivity has also been observed in other studies with the same positivity rate [2].
Generally speaking, the most common germs were Gramnegative bacilli, about 63%. This predominance is due to the fact that they constitute a great variety of bacteria and are the most encountered in human pathologies.
The present study found that Micrococaceae were the most bacteria represented (37.7%), followed by Enterobacteriaceae (29.5%), and Pseudomonaceae (23.0%). It is the same as that reported in Senegal by Cisse et al. who found a predominance of Micrococaceae (37%), followed by Enterobacteria (26%), and Pseudomonaceae (25%) [3]. However, Ghanpur et al. revealed predominance of Pseudomonas aeruginosa (33%), Methicillin Resistant Staphylococcus aureus (MRSA) (18%) [12]. In another study in Chile, Streptococcus pneumoniae and Haemophilus influenzae were predominant [13].
Concerning the bacterial species involved in this infection recall that according to the AFSSAPS, S. pneumoniae (25 to 40%), H. influenzae (30 to 40%) and M. catarrhalis. S. pyogenes (group A streptococcus) are the main bacteria involved in purulent AMO of children over 3 months of age and S. aureus played a minor role (<5%) [10]. However, Staphylococcus aureus was the most commonly encountered bacterial species in our series (35.5%), followed by Pseudomonas aeruginosa (16.1%) and Escherichia coli (11.3%). In addition, no cases of pneumococcus, Haemophilus or Moraxella were isolated. This is in line with other work carried out in Africa, notably in Senegal [3]. This difference would be associated, on the one hand, with the bacterial ecosystem varying from one continent to another, sampling and manipulation techniques given the fragility of these germs and, on the other hand, the role of vaccination in reducing of the circulation of these two germs in Burkina Faso. As part of the Expanded Program routine on Immunization (EPI) in Burkina Faso, children have been receiving free vaccination against Haemophilus influenzae B and against Streptococcus pneumoniae, since 2013.
In comparison with the susceptibility of the organisms to the antibiotics tested, the study showed low sensitivities of staphylococci, enterobacteria and Pseudomonas with respect to ampicillin and Amoxicillin plus clavulanic acid. This strong resistance of these germs to the molecules has been observed in the country and which could be associated with a production by these β-lactamase bacteria [6]. Ciprofloxacin, Gentamicin and Imipenem were very active on Staphylococcus aureus, Escherichia coli and Pseudomonas aeruginosa. Cissé et al. also showed a high sensitivity of Pseudomonas aeruginosa to Ciprofloxacin and to Gentamicin [3]. In general, four antibiotics showed good activity on the 62 isolated bacteria: Ciprofloxacin (97%), Gentamicin (98%), Imipenem (82%) and Ceftriaxone (76%). Low sensitivities were observed with Ampicillin (3%), Erythromycin (21%) and amoxicillin plus clavulanic acid (18%) and Cotrimoxazole (47%). This lower sensitivity of bacteria to cotrimoxazole could occur its frequent use in the management of opportunistic infections with the advent of HIV. These low sensitivities could be due to selection pressure and β-lactamase production. In fact, β-lactams, in particular amoxicillin and the amoxicillin/ clavulanic acid combination, are commonly used antibiotics because of their greater accessibility (cost and availability) and are also well known to prescribers. This would encourage consumption and possible self-medication.
Conclusion
This study allowed us to determine the main bacteria responsible for acute purulent otitis media at the Bogodogo district hospital and their susceptibility profile to antibiotics most commonly used in our context.
These infectious agents, because of the frequent and probabilistic prescription of antibiotics in infections of the ORL sphere, are subjected to a strong selection pressure. Monitoring the evolution of resistance ensures the success of a probabilistic treatment especially in Burkina Faso where the bacteriological examination is not systematically asked in the presence of a bacterial infection. Knowledge and updating of data on bacterial epidemiology and antibiotic susceptibility profiles of the most isolated bacteria are essential.
Acknowledgements
We are grateful to all the participants of this study. We would like to thank the staff of the National Public Health Laboratory of Burkina Faso and the partnering University Hospitals for their intellectual and technical support and help.
Conflict of Interest Statement
The authors declare no conflict of interest.
21964
References
- Ovnat TS, Shemesh S, Oron Y, Marom T (2017) Acute otitis media guidelines in selected developed and developing countries: uniformity and diversity. Arch Dis Child 2017 102: 450-457.
- Sako A [Suppurative otitis media, bacteriologic study and therapeutic management] (1995) VestnOtorinolaringol 15: 12-14.
- Cisse MF, Sow AI, Adjovi DR, Samb A (1995) Bacteriological study of purulent otitis media in children in CHU in the tropical zone. Arch Pediatr 2: 29-33.
- Takata GS, Chan LS, Shekelle P, Morton SC, Mason W, et al. (2001) Evidence assessment of management of acute otitis media: I. The role of antibiotics in treatment of uncomplicated acute otitis media. Pediatrics 108: 239-247.
- Ministère de la Santé Burkina Faso (2013) AnnuaireStatistique. Ouagadougou: Ministère de la Santé 20: 214.
- Ministère de la Santé Burkina Faso (2012) AnnuaireStatistique. Ouagadougou: Ministère de la Santé 13: 121.
- Hoberman A, Paradise JL, Rockette HE, Shaikh N, Wald ER, et al. (2011) Treatment of acute otitis media in children under 2 years of age. N Engl J Med 364: 105-115.
- Vergison A, Dagan R, Arguedas A, Bonhoeffer J, Cohen R, et al. (2010) Otitis media and its consequences: beyond the earache. Lancet Infect Dis 2010 10: 195-203.
- AgenceFrançaise de Sécurité Sanitaire des Produits de Santé (2011) Good practice recommendations. General antibiotic therapy in routine practice in upper respiratory infections in adults and children. Otitis Middle acute 144.
- Biagio L, Swanepoel DW, Laurent C, Lundberg T (2014) Paediatric otitis media at a primary healthcare clinic in South Africa. S Afr Med J 104: 431-435.
- Ghanpur AD, Nayak DR, Chawla K, Shashidhar V, Singh R (2017) Comparison of Microbiological Flora in the External Auditory Canal of Normal Ear and an Ear with Acute Otitis Externa. J ClinDiagn Res 11: MC01-MC04.
- Rosenblut A, Napolitano C, Pereira A, Moreno C, Kolhe D, et al. (2017) Etiology of acute otitis media and serotype distribution of Streptococcus pneumoniae and Haemophilusinfluenzae in Chilean children <5 years of age. Medicine (Baltimore)96: e5974.