Sukanya Sudhaharan1, Padmasri Chavali 1, Sandhya Devi Karanam1, Liza Rajsekhar2, Srujana Arekal2 and Lakshmi Vemu1*
1Departments of Microbiology, Nizam’s Institute of Medical Sciences, Panjagutta, Hyderabad, India.
2Department of Rheumatology, Nizam’s Institute of Medical Sciences, Panjagutta, Hyderabad, India
*Corresponding Author:
Dr.V.Lakshmi Professor and Head
Department of Microbiology
Nizam’s Institute of Medical Sciences
Panjagutta, Hyderabad
Tel: +009104023489141
E-mail: lakshmi57vemu@gmail.com
Received date: October 28, 2015; Accepted date: November 30, 2015; Published date: December 07, 2015
Keywords
Cutaneous melioidosis; SLE; Abscess; Immunocompromised; Melioidosis; Cutaneous
Introduction
Melioidosis caused by the Gram negative bacillus, Burkholderia pseudomallei, is an infectious disease of public health importance. It is usually associated with various immunocompromised states [1,2]. However it is rarely seen in patients with Systemic Lupus Erythematosus (SLE) [3]. Cutaneous melioidosis is rare and is usually under-diagnosed due to lack of awareness and diagnostic facilities [4]. We report a case of thigh abscess due to B. pseudomallei in a SLE patient on immunosuppressive therapy.
Case History
A 27-year-old female on immunosuppressive therapy, consisting of Wysolone (prednisolone) and Mycofenolate Mofetil (MMF) for SLE for the past 7 years, was admitted under the rheumatology services of our hospital with complaints of low backache and knee joint pain of one month duration. She had history of vomiting and loose stools for the past 25 days. She did not provide a history of any febrile illness.
On clinical examination, the patient was afebrile with normal vitals. There were no signs of sepsis. She was found to have bilateral lower limb flaccid paralysis, urinary retention and sacral sensory loss. The neurologist opined as cauda equina syndrome or myelitis. The rest of the systemic examination was insignificant.
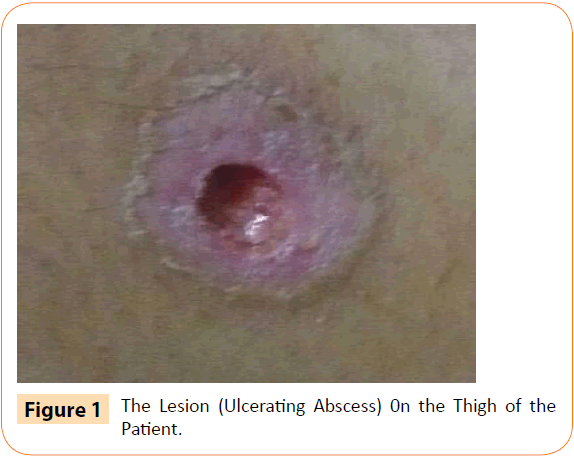
An erythematous ulcer with undermining edges with purulent discharge over the right thigh was detected incidentally (Figure 1). The patient, however, was neither troubled nor complained about the ulcer. On further questioning, the patient informed that the lesion was present since the past one week. She also had similar lesions on the upper limbs that had healed without any specific treatment.
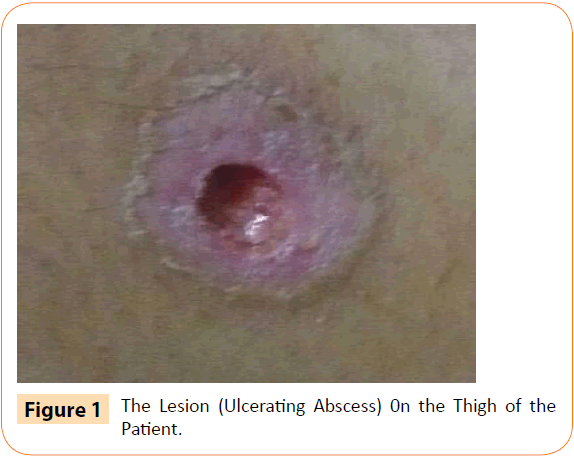
Figure 1: The Lesion (Ulcerating Abscess) 0n the Thigh of the Patient.
The clinical impression at this stage was SLE with cauda equina syndrome or myelitis and lupus enteritis. Empiric therapy with I/V meropenem 1 g 8th hourly and I/V ceftriaxone 1 g 12th hourly were administered along with the immunosuppressant therapy that she was receiving.
Laboratory investigations
Clinical chemistries and complete blood count were all within normal limits except for a raised Erythrocyte Sedimentation Rate of 50 mm / hour. A swab from the purulent ulcer on the thigh was submitted for microbiological analysis for any infectious pathology. However, no histology was done for the lesion.
Microbiology
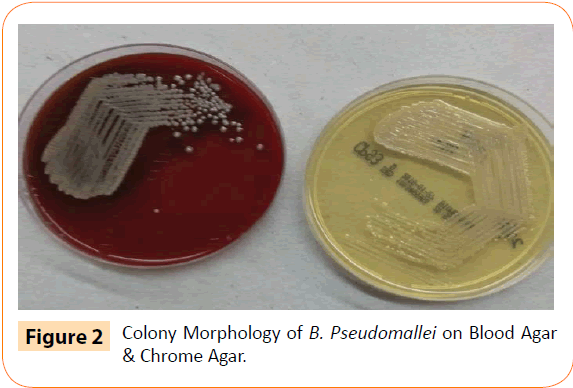
The swab specimen was processed for bacterial pathogens on 5% sheep blood agar (COS) (bioMérieux) and Chromogenic agar (CPS ID) (bioMérieux), incubated aerobically at 37°C for 48 hours. Gram stain of the specimen showed scanty neutrophils with no organisms. After 48 hours, the culture plates showed growth of non-hemolytic and non-pigmented pale flat colonies (Figure 2). They were identified as Gram negative bacilli on Gram’s stain. The isolate was processed on Vitek 2(bioMérieux, Marcy l’Etoile, France) for identification (ID GN panel) and Antimicrobial Susceptibility (AST N 281). The isolate was identified as B. pseudomallei. However, the AST was inconsistent on Vitek 2 and was repeated on API (bioMerieux) using the ATB PSE 5 panel. The isolate was susceptible to ceftazidime, imipenem, meropenem and cotrimoxazole.
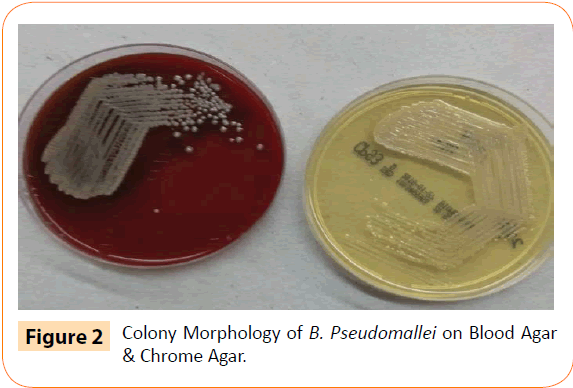
Figure 2: Colony Morphology of B. Pseudomallei on Blood Agar & Chrome Agar.
Based on the culture and the AST reports, oral cotrimoxazole double strength (160 mg/ 800 mg) 12th hourly, along with I/V meropenem 1 g 8th hourly were initiated as a specific therapy for B. pseudomallei.
A repeat culture from the ulcer, after two days, again showed growth of B. pseudomallei. Two sets of blood cultures (Standard and FA+ bottles, bioMerieux) were sterile after 5 days. The antibiotic treatment was continued for the next 14 days. The ulcer began to heal by the third day and was healed completely at the time of discharge. The patient was discharged after 14 days of initiation of treatment. The general condition of the patient, at the time of discharge was stable with no further complaints. She was advised physiotherapy for her paralysis and asked to continue oral Co-trimoxazole for 3 months. She is under regular follow up and doing well.
Discussion
It is usually a fatal systemic infection caused by the intracellular Gram negative bacteria B. pseudomallei. It occurs in people who are in contact with contaminated soil or water. Melioidosis is regarded as endemic to Northern Australia and South East Asia, including India [5,6].
The clinical manifestations of melioidosis are protean and primary infection and suppurative complications may involve virtually every organ. On one end of the spectrum, acute Pneumonia and bacteremia are the most common manifestations associated with high mortality. Other presentations include genitourinary infection, suppurative parotitis, various forms of central nervous system infection, osteomyelitis and septic arthritis, intraabdominal abscess (mainly involving the spleen, liver or adrenals), nectrotizing skin infection, mycotic aneurysms or pericarditis and corneal abscesses. Almost all patients have diabetes mellitus as an associated comorbidity [7,8].
At the other end of the spectrum are asymptomatic infections and localized skin ulcers or abscesses without systemic illness, as seen in our patient. In a small proportion of these people the infection can re-activate from a latent form many years later [9].
The skin lesions in this patient were an incidental finding, as she was neither troubled nor complained about the ulcers, until she was questioned. The localized ulcer with healed skin lesions, elsewhere on the body, could be due to a Primary cutaneous melioidosis, which is often localized and less severe than secondary cutaneous melioidosis [6]. However, in South East Asia the infection has been reported to be associated with necrotizing fasciitis, sepsis, and internal organ abscesses [9]. Serious infection is a common problem in immunosuppressed patients with Systemic Lupus Erythematosus (SLE) [3]. Though there are a few case reports of melioidosis in SLE patients [3,6,10-13] however, cutaneous lesions of melioidosis in SLE patients has not been reported as of date, to the best of our knowledge. Hence this case is being reported. The route of infection in the present case was not known. The patient is a student of biotechnology and had neither history of contact with contaminated water or soil nor any history of travel. The only associated and known risk factor in the patient was immunosuppressive therapy.
Appropriate treatment should be given to avoid relapse of meliodosis, as the organism can remain latent in the body for a long period of time [5]. The specific antimicrobial treatment for melioidosis includes I/V ceftazidime or meropenem or imipenem with or without cotrimoxazole as initial therapy for 10-14 days and cotrimoxazole with or without doxycycline as eradication therapy for 3 months [14]. As per a recently conducted multicenter double blinded randomized controlled trial, cotrimoxazole alone is not inferior to cotrimoxazole plus doxycycline for eradication therapy [15]. In a large cohort of 58 patients with primary skin melioidosis, reported from Australia, the patients had fewer underlying medical conditions, and had better outcomes than did those with other forms of melioidosis [9]. There may be a role for exclusive oral antibiotic therapy for some cases of primary skin melioidosis. Our patient is being continued on the maintenance therapy without any recurrence of fresh cutaneous lesions as on date.
Conclusion
As infections are a common feature in SLE on immunosuppressive drugs, a high degree of suspicion of rare infections such as melioidosis for an early diagnosis and appropriate antimicrobial therapy is called for.
Funding
This report received no speci?c grant from any funding agency in the public, commercial, or not for-pro?t sectors
Conflict of interest
The authors have no con?icts of interest to declare.
7772
References
- John TJ (2002) Melioidosis, the mimicker of maladies. Indian J Med Res 119:6-8.
- Pandey V, Rao SP, Rao S, Acharya KK, Chhabra SS (2010) Burkholderiapseudomallei musculoskeletal infections (melioidosis) in India. Indian J Orthop44: 216-20.
- Badsha H, Edwards CJ, Chng HH (2001)Melioidosis in systemic lupus erythematosus: the importance of early diagnosis and treatment in patients from endemic areas. Lupus 10: 821-823.
- Parry CM, Wutheikanum V, Hao NT, Diep TS, Thao LT, et al. (1999) Melioidosis in southern Vietnam: clinical surveillance and environmental sampling. Clin Infect Dis 29:1323-1326.
- Cheng AC, Currie BJ (2005)Melioidosis: epidemiology, pathophysiology, and management. ClinMicrobiol Rev 18:383-416.
- Rao PS, Dhawan R, Shivananda PG (2002) Burkholderiapseudomallei infections: case reports of five cases. Tropical Doctor 32:174-175.
- Gilad J, Schwartz D, Amsalem Y (2007) Clinical features and laboratory diagnosis of infection with the potential bioterrorism agents Burkholderia mallei and Burkholderiapseudomallei. Int J Biomed Sci 3: 144-152.
- Mustafa M, Balingi J, Menon J, Robinson F, Rahman MS (2015) Clinical manifestations, diagnosis, and treatment of Melioidosis. IOSR Journal of Pharmacy 5:13-19.
- GibneyKB, Cheng AC, Currie BJ (2008) Cutaneous Melioidosis in the Tropical Top End of Australia: A Prospective Study and Review of the Literature. Clin Infect Dis 47: 603-609.
- Christenson-Bravo B, Rodríguez JE, Vázquez G, Ramírez Ronda CH (1986) Pseudomonas pseudomallei (melioidosis): acute septicemia and meningitis in patient with systemic lupus erythematosus. BolAsoc Med P R78: 347-349.
- Samad I, Wang MC, Chong VH (2014) Intracerebralcoinfection with Burkholderiapseudomallei and Cryptococcus neoformans in a patient with systemic lupus erythematosus. Southeast Asian J Trop Med Public Health45:352-356.
- Vachvanichsanong P, Dissaneewate P, Prukprasert P,Wongchanchailert M, Thongmak S, et al. (2002)Melioidosis and brain abscess in a girl with systemic lupus erythematosus. Infect Dis ClinPrac 11: 211-213.
- Issack MI, Bundhun CD, Gokhool H (2005)Melioidosis in Mauritius. Emerg Infect Dis 11:139-140.
- Mandell GL, Bennett JE, Dolin RD (2010)Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases. 7th ed, Philadelphia (PA): Elsevier Churchill Livingstone2869-2877.
- Chetchotisakd P, Chierakul W, Chaowagul W, Anunnatsiri S, Phimda K,et al.(2014) Trimethoprim-sulfamethoxazole versus trimethoprim-sulfamethoxazole plus doxycycline as oral eradicative treatment for melioidosis (MERTH): a multicentre, double-blind, non-inferiority, randomised controlled trial.Lancet383:807-814.