Mini Review - (2022) Volume 14, Issue 5
Update is bariatric surgery contributing to a decreasing trend in COVID-19 infection and complication rate in obese patients?
Arbaab Khan* and
Tanvish Nitin Manwatkar
AIETI Medical School- David Tvildiani Medical University, Tbilisi 0159, Georgia, USA
*Correspondence:
Arbaab Khan, AIETI Medical School- David Tvildiani Medical University, Tbilisi 0159, Georgia,
USA,
Email:
Received: 25-Apr-2022, Manuscript No. ipaom-22-12728;
Editor assigned: 28-Apr-2022, Pre QC No. P-12728;
Reviewed: 17-May-2022, QC No. Q-12728;
Revised: 22-May-2022, Manuscript No. R-12728;
Published:
30-May-2022
Abstract
The objective of this study is to identify bariatric surgery as a treatment modality to reduce COVID-19 related morbidity, mortality and complication rate in the obese patients. This study involves the comparison of 2 researches in which COVID-19 affected patients were assessed for their severity of disease on the basis of their history of bariatric/ metabolic surgery (whether they had undergone bariatric surgery or not ) .The patients who had undergone bariatric procedure and their matched controls (both populations positive for COVID-19 infection) were compared to several variables like hospital admission , admission to ICU unit need for mechanical ventilation & dialysis during hospitalization ,other morbidities and also mortality .The comparison of results showed that patients who underwent bariatric surgery had a better prognosis and a better profile( in terms of morbidity and complication rate and severity) as compared to their matched controls indicating an indirect role of bariatric surgery in alleviating the morbidities related with COVID-19 in an obese patient.
Keywords
Bariatric; Surgery; COVID-19
Introduction
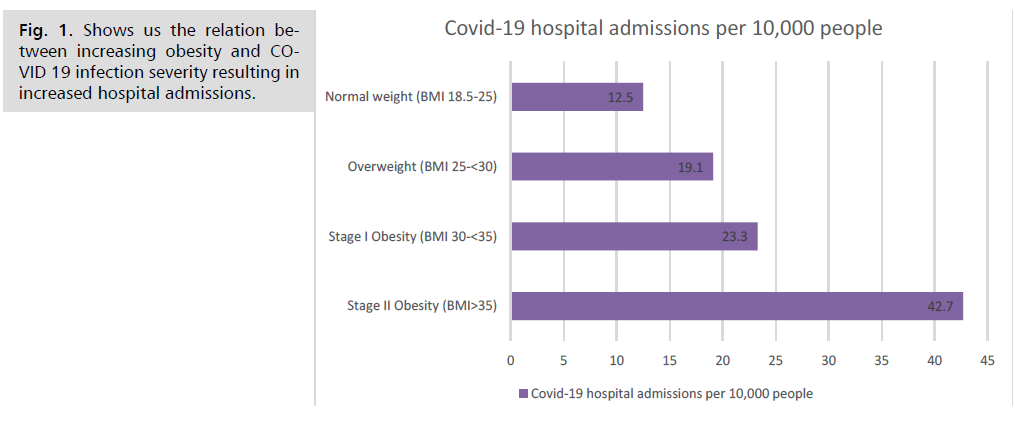
Antibiotics Bariatric surgery is a modality that aims at 2 kills with one bullet, it ends two of the world’s greatest pandemics, obesity and COVID-19 altogether.Obesity has co-morbidities like cardio-metabolic, pulmonary, and thromboembolic diseases; changes in the innate and adaptive immune response; coexistence of a pro-inflammatory state; restrictive changes to the mechanics of the lungs and chest wall; and limited response to mechanical ventilation, this can all lead to poor prognosis of COVID-19 in patients with obesityBariatric surgery offers substantial and sustained weight loss; improvement in obesity-associated pro- (Fig.1). inflammatory state, as well as improvement in cardio-metabolic risk factors, including diabetes and blood pressure control; improvement of cardiopulmonary and renal functions; decrease in risk of adverse cardiovascular events; and better survival in patients with severe obesity. Increased risk for obese patients is also supported by the fact that the coronavirus enters the body via ACE2 receptor (ACE2 is the receptor for SARS-CoV-2). This enzyme is present in cells along the lungs and fat tissue, which yields to the fact that patients with greater weight will have greater viral load. Also, obesity is associated with hyper-inflammation and shortness of breath, that makes it difficult to fight the viral infection. This is when bariatric surgery comes into help, after which fat tissue decreases over time in the body, leaving less amount of ACE2 receptors for COVID-19 to access. ACE2 receptors are also present in high amounts in the pericytes of the heart, and brain, thus contributing to the cardiac and CNS effects occurring with COVID-19 infection [1].
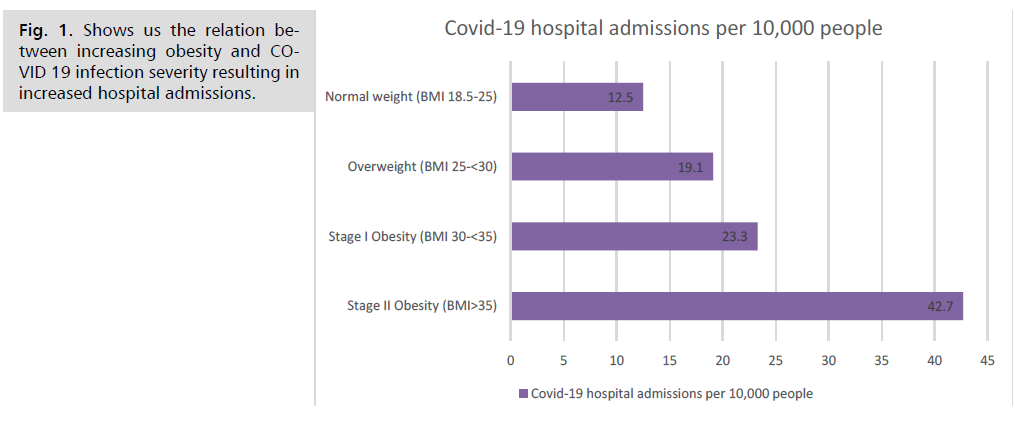
Fig 1: Shows us the relation between increasing obesity and COVID 19 infection severity resulting in increased hospital admissions.
The biology of obesity includes impaired immunity (fat cells infiltrate the organs where immune cells are produced and stored, like the spleen, bone marrow and thymus. Besides, function of T-cells is impaired in the obese state, which also affects production of “memory” T-cells affecting the ability to neutralize future attacks by the same virus.), chronic inflammation, and blood that’s prone to clot, all of which worsen COVID-19 .Another important thing to mention is that obesity leads to higher circulating leptin and lower circulating adiponectin (has anti-inflammatory effect) levels [2]. Adiponectin levels have been reported to be significantly lower in many of the COVID-19 “at risk” groups therefore bariatric surgery can be useful for indirectly increasing adiponectin which will produce anti-inflammatory effects preventing greater end organ damage.[3,4].
Objective
To identify bariatric surgery as a modality that reduces COVID-19 related morbidity, mortality and complication rate in the obese patients.
Methods
Study 1
4365 patients were studied in this research study, who were tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) between March 8, 2020 and July 22, 2020, in the Cleveland Clinic Health System. 33 patients were identified who had a prior history of bariatric surgery and these patients were matched on a ratio of 1:10 to nonsurgical patients on the basis of the Body Mass Indexed (BMI) 40.0 or above at the time of SARS-CoV-2 testing. The primary endpoint was the rate of hospital admission. The exploratory endpoints included admission to the Intensive Care Unit (ICU) need for mechanical ventilation and dialysis during hospitalization, and mortality [5].
Study 2
4,248,253 individuals were studied in a retrospective nationwide study with the ages of the patients between 15 to 75 years. The patients chosen in the study were obese and were diagnosed with COVID-19 . All obese inpatients, undergoing bariatric surgery or not, were recorded during the hospital stay with a mean observation time of 5.43 ± 2.93 years. This study involved the patients who had undergone bariatric surgery (n=389,671) (including adjustable gastric banding, sleeve gastrectomy, gastric bypass) versus who did not undergo bariatric surgery (n=3,858,582) and this variable was compared to different outcomes. The primary outcome was COVID-19 related death and the secondary outcome was the need for invasive mechanical ventilation [6].
Results
Study 1
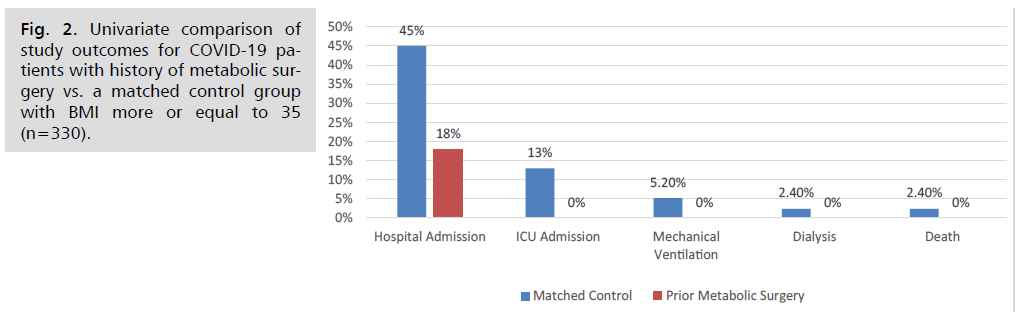
The average BMI of the surgical group was 49.1 before bariatric surgery and after the procedure it was found to be 37.2 at the time of SARS-CoV-2 testing (compared with the control group’s BMI of 46.7) (Tab 1). Comparison of several variables between bariatric and non-bariatric patients suffering from COVID-19 ) [5]. In the univariate analysis, 6 (18.2%) patients in the bariatric surgery group and 139 (42.1%) patients in the control group were admitted to the hospital. While none of 4 exploratory outcomes occurred in the bariatric surgery group 43 (13.0%) patients in the control group required ICU admission 22 (6.7%) required mechanical ventilation 5 (1.5%) required dialysis and 8 (2.4%) died (Fig 2). In the multivariate analysis, a prior history of bariatric surgery was associated with a lower hospital admission rate compared with control patients with obesity.
| Characteristics of bariatric surgery patients and matched control patients at the time of SARS-CoV-2 test |
| Baseline variables |
No. (%) of patients [Whole population n= 4365] |
| Bariatric surgery |
Matched control |
| (n=33) |
(n=330) |
| Gender |
| Female |
26 (78.8) |
239 (78.5) |
| Male |
7 (21.2) |
71 (21.5) |
| Age (years) |
46.1±12.7 |
49.8±14.3 |
| BMI (kg/m2) |
37.2±7.1 |
46.7±6.4 |
| Race |
| White |
16 (48.5) |
154 (46.7) |
| Black |
13 (39.4) |
159 (48.2) |
| Other |
4 (12.1) |
17 (5.2) |
| Ethnicity |
| Non-Hispanic |
32 (97.0) |
319 (96.7) |
| Hispanic |
1 (3.0) |
11 (3.3) |
| Smoking status |
| Current |
0 |
1 (0.3) |
| Former |
10 (30.3) |
100 (30.3) |
| Never |
21 (63.6) |
209 (63.6) |
| Unknown |
2 (6.1) |
20 (6.1) |
| Testing location |
|
|
| Ohio |
31 (93.9) |
310 (93.9) |
| Florida |
2 (6.1) |
20 (6.1) |
| Hypertension |
12 (36.0) |
205 (62.1) |
| Diabetes |
2 (6.1) |
113 (34.2) |
| Coronary artery disease |
4 (12.0) |
22 (6.7) |
| Heart failure |
2 (6.1) |
28 (8.5) |
| Asthma |
12 (36.4) |
114 (34.5) |
| COPD |
1 (3.0) |
10 (3.0) |
| Cancer |
1 (3.0) |
10 (3.0) |
| Steroid |
5 (15.0) |
56 (17.0) |
| Angiotensin converting enzyme inhibitor |
2 (6.1) |
52 (15.8) |
| Angiotensin receptor blocker |
4 (12.0) |
35 (10.6) |
Tab. 1. Comparison of several variables between bariatric and nonbariatric patients suffering from COVID-19.
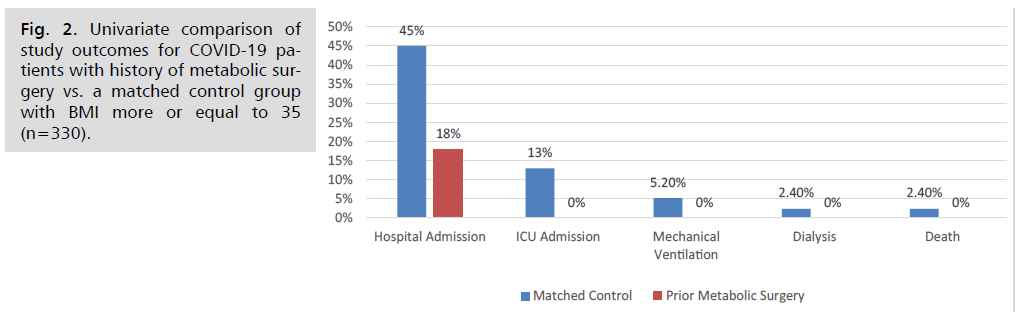
Fig 2: Univariate comparison of study outcomes for COVID-19 patients with history of metabolic surgery vs. a matched control group with BMI more or equal to 35 (n=330).
Study 2
Out of the 4,248,253 obese patients, 8286 (0.2%) obese individuals were admitted for COVID-19 infection between January 1st and May 15th 2020. 541 (0.14%) had a history of bariatric surgery and 7,745 (0.2%) did not. Invasive mechanical ventilation was necessary in 14.54% of patients and death occurred in 13.58% of cases. The need for an invasive mechanical ventilation and death occurred in 7% and 3.5% in the bariatric surgery group versus 15% and 14.2% in the non-bariatric surgery group, respectively. After a logistic regression, the risk of invasive mechanical ventilation significantly increased with age, being higher in the age class 61-75 male gender and hypertension whereas bariatric surgery showed an independent protective effect. Mortality was independently associated with increasing age, male gender, known history of heart failure, cancer, and diabetes, whereas BS was in favor with a protective effect.
Discussion
Beyond The association between obesity and COVID-19 can be assessed in various aspects. First obesity causes respiratory system dysfunctions like decreased chest wall elasticity (fat in the abdomen pushes up on the diaphragm, which presses on the lungs and restrict airflow) lung compliance, and expiratory reserve volume (this reduced lung volume causes collapse of airways in the lower lobes of the lungs, where more blood arrives for oxygenation than in the upper lobes) [7]. Second, obesity is associated with disorders such as type 2 diabetes mellitus, atherosclerosis, cardiovascular diseases, hypertension and cancer [8]. Which are also identified as risk factors for COVID-19.These comorbidities may exacerbate COVID-19 and increase the probability of hospitalization in the intensive care unit (ICU) and also increase mortality [9]. Third, it leads to hyper coagulopathy state and hyper inflammation, and it is well known that venous thromboembolism is a complication of severe COVID-19 infection as well, thus these 2 conditions when present together produce hypercoagulability and thromboembolism in a synergistic way. Inflammatory markers such as IL-6 and C-reactive protein are increased in obese patients [10,11]. These may become so severe that they can cause clots in vital organs and cytokine storm. In all these 3 conditions, the disease is severe and the risk of admission to the ICU and mortality is high. On the other hand, COVID-19 also has an impact on obesity as it increases social constraints and impedes mobility, which thus increases the weight and prevalence of obesity in society, and this gives way to a vicious cycle that is repeated all over again and again. Although there are ample advantages of bariatric surgery in the COVID-19 patient, there are certain limitations that are worthy of mention. Bariatric surgery, specifically bypass surgery, is likely to have an effect on the absorption of medications that are administered orally to COVID-19 patients. In case of hydroxychloroquine, a case report of three post-RYGB (Roux-en-Y procedure) patients with autoimmune disease was done (taking standard hydroxychloroquine doses), all three patients had sub therapeutic hydroxychloroquine blood levels and active disease; it was only after increasing their doses above the recommended 400 mg/day dosing that they were able to have therapeutic drug levels as well as better disease control. Thus hydroxychloroquine has inadequate absorption post-RYGB (and potentially other bariatric procedures), and COVID-19 bariatric patients may need higher doses of hydroxychloroquine than recommended [12]. For azithromycin a single-dose pharmacokinetic study involving 14 post-gastric bypass patients showed that bioavailability was reduced by 1/3rd in gastric bypass patients, when compared with matched controls [13]. Since maximal absorption of azithromycin occurs in proximal gut. During RYGB (Roux-en-Y procedure) the stomach is dissected, that leads to less acidic gastric pouch. Azithromycin with its basic nature (alkaline; pKa=8.5) and low water solubility, the dissolution of the large (500 mg) drug dose of azithromycin can be severely affected post-surgery thus affecting the absorption and bioavailability of azithromycin. In case of corticosteroids, the pharmacokinetics of dexamethasone and related steroids may be affected especially post-gastric bypass surgery. These drugs are mainly absorbed via the proximal gut which is hampered during the bariatric procedure. These are some of the limitations of the bariatric surgery procedure that need to be considered in a COVID-19 patient (Tab 2).
| Univariate analysis of preoperative risk factors distribution in Covid-19 obese patients in bariatric surgery and non-bariatric surgery cohorts [6] |
| Characteristic |
No. (%) of patients [Whole population n=8286] |
| Bariatric Surgery |
No Bariatric Surgery |
| (n=541) |
(n=7745) |
| Age in years, mean (SD) |
49.8 (12.0) |
59.8 (12.4) |
| 34-45 |
33 (6.1) |
218 (2.8) |
| 15-30 |
158 (29.2) |
899 (11.6) |
| 46-60 |
239 (44.2) |
2231 (28.8) |
| 60-75 |
111 (20.5) |
4397 (56.8) |
| Gender |
| Male |
127 (23.5) |
4169 (53.8) |
| Female |
414 (76.5) |
3576 (46.2) |
| COPD |
| Yes |
16 (3) |
567 (7.3) |
| No |
525 (97) |
7178 (92.7) |
| Cardiac failure |
| Yes |
18 (3.3) |
551 (7.1) |
| No |
523 (96.7) |
7194 (92.9) |
| Cancer |
| Yes |
11 (2) |
597 (7.7) |
| No |
530 (98) |
7148 (92.3) |
| Diabetes |
|
|
| Yes |
66 (12.2) |
2851 (36.8) |
| No |
475 (87.8) |
4894 (63.2) |
| Hypertension |
| Yes |
109 (20.2) |
3222 (41.6) |
| No |
432 (78.9) |
4523 (58.4) |
| Invasive mechanical ventilation |
| Yes |
|
|
| No |
38 (7) |
1158 (15) |
| |
503 (93) |
6587 (85) |
| Death |
| Yes |
19 (3.5) |
1098 (14.2) |
| No |
522 (96.5) |
6647 (85.8) |
Tab. 2. Univariate comparison of study outcomes for COVID-19 patients with history of metabolic surgery vs. a matched control group with BMI more or equal to 35. (n=330) [5].
Conclusion
In the studies that were discussed in this research paper .it made it clear that prior bariatric surgery patients were noted to have weight loss and improvement of metabolic abnormalities which led to lower rates of morbidity, mortality and hospital & ICU admission in patients with obesity that became infected with SARS-CoV-2 when compared to their matched controls. This helps us in understanding an indirect role of bariatric surgery in alleviating the morbidities related with COVID-19 in an obese patient. According to the American Society for Metabolic and Bariatric Surgery (ASMBS) the bariatric surgery is not an elective surgery and the lives of patients with obesity is in danger, and it should be acknowledged that a patient who undergoes bariatric surgery is much safer than the COVID-19 patients with obesity [14]. With limited research material available globally on the relation between bariatric surgery and COVID-19 there is much more research required in this field and more cues to be solved. Bariatric surgery can be a promising modality for reducing the severity of COVID-19 in obese patients with further advances in the near future.
Conflicts of Interest
All authors declare that they have no conflict of interest.
Data Availability
All data generated or analyzed during study are included in this review.
Funding
This study was not funded by any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
None.
REFERENCES
- He L, Mäe MA, Muhl L, et al. Pericyte-specific vascular expression of SARS-CoV-2 receptor ACE2–implications for microvascular inflammation and hypercoagulopathy in COVID-19. BioRxiv. 2020.
Google Scholar, Crossref, Indexed at
- Scherer PE. The many secret lives of adipocytes: implications for diabetes. Diabetologia. 2019; 62:223-232.
Google Scholar, Crossref, Indexed at
- Duncan BB, Schmidt MI, Pankow JS, et al. Adiponectin and the development of type 2 diabetes: The atherosclerosis risk in communities study. Diabetes. 2004;53:2473-2478.
Google Scholar, Crossref, Indexed at
- Abate N, Chandalia M, Snell PG, et al. Adipose tissue metabolites and insulin resistance in non diabetic Asian Indian men. J Clin Endocrinol Metab. 2004; 89:2750-2755.
Google Scholar, Crossref, Indexed at
- Association of prior metabolic and bariatric surgery with severity of Q18 coronavirus disease 2019 (COVID-19).
Google Scholar, Crossref, Indexed at
- Iannell A, Bouam S, Schneck AS, et al. Impact of previous history of bariatric surgery on outcome of covid 19: A nation-wide medico-administrative French study. Obes Surg. 2021;31:1455-1463.
Google Scholar, Crossref, Indexed at
- Uccelli M, Cesana GC, Ciccarese F, et al. COVID-19 and obesity: Postoperative risk in patients who have undergone bariatric surgery. Preliminary report from high volume center in Italy (Lombardy). Obes Surg. 2020;27:1-4.
Google Scholar, Crossref, Indexed at
- Blüher M. Obesity: Global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15:288-298.
Google Scholar, Crossref, Indexed at
- Banerjee M, Gupta S, Sharma P, et al. Obesity and COVID-19: A fatal alliance. Indian J Clin Biochem. 2020:1-8.
Google Scholar, Crossref, Indexed at
- Chiappetta S, Sharma AM, Bottino V, et al. COVID-19 and the role of chronic inflammation in patients with obesity. Int J Obes. 2020;44:1790-1792.
Google Scholar, Crossref, Indexed at
- Pasquarelli-do-Nascimento G, Braz-de-Melo HA, Faria SS, et al. Hypercoagulopathy and adipose tissue exacerbated inflammation may explain higher mortality in COVID-19 patients with obesity. Front Endocrinol (Lausanne). 2020;11:530.
Google Scholar, Crossref, Indexed at
- Thomas DE, Lyons JS ,Greene BS, et al. Low hydroxychloroquine blood levels in patients who have had gastric bypass surgery. Lupus Sci Med. 2019;6:e000335.
Google Scholar, Crossref, Indexed at
- Padwal R S, Ben-Eltriki M, Wang X, et al. Effect of gastric bypass surgery on azithromycin oral bioavailability. J Antimicrob Chemother. 2012;67:2203-2206.
Google Scholar, Crossref, Indexed at
- Beskow A, Duartez PM, Beheren E, et al. COVID-19 pandemic and bariatric surgery in Argentina. Res Square. 2020.
Google Scholar, Crossref, Indexed at