Keywords
Cervical cancers; Screening; Female health workers; Utilization
Introduction
Cervical cancer is a type of cancer that can be preventable and treatable through early screening [1], it is also a public health problem in the world including developing countries [2]. Cervical cancer is the 2nd most commonly diagnose and leading causes of death among child bearing women in the world and more than 85% of cases and deaths are found in less developed countries [3].
Globally, cervical cancer is a responsible to kill 275,000 women every year; It is also the second largest cancer case and death in low and middle-income countries; Project estimate that half a million women will die of cervical cancer by 2030 [4].
Around 60,098 African women are diagnosed with cervical cancer annually and most of them (47%) are found in east Africa. According to ICO HPV information Centre, cervical cancer is the 2nd most prevalent next to breast cancer in Ethiopia and also every year 7095 new cases and 4732 deaths occurred among reproductive women and the average crude incidence rate is 16.3 per 100000 women and large proportion of women were diagnosed in advance stage of cervical cancer.
The current estimate indicate that Ethiopia has 29.43 million female populations greater than 15 years who are at risk for developing cervical cancer [5]. Women who started their sexual life before the age of 16 are a high risk than 20 years old because of an increase exposure to Human Papilloma Virus. In most countries, including Ethiopia data showed that the incidence of cervical cancer begins to rise in age of 20 to 29 years and peak at 40 and 50 years [1,3,6].
The main causative agent for the development of cervical cancer is Human Papilloma Virus (HPV) and it account 70% responsible in the world plus 97% in Ethiopia. The Potential risk factors for the persistent of HPV and the development of cervical cancer are multiple sexual partners, sexually transmitted disease, longterm use of hormonal contraceptives, multiparty, age of first sexual intercourse, early age at first birth, smoking and immune suppression.
Cervical cancer screening has a benefit to reduce the incidence, the progression of advanced stage of cancer as well as its mortality. Screening reveals abnormal change of cervical cells and this change is detectable 5-20 years prior to cervical cancer. The methods which used for screening are Pap smear, VIA, VILI and HPV test; but VIA followed by treatment is an effective method, relatively simple procedure and feasible in resource limited [7,8].
Screening of cervical pre-cancer and cancer should be done in women who have started sexual activity or as soon as the woman has tested positive for HIV regardless of age. Screening even once in a lifetime will be beneficial to avoid advanced cancer but the intervals may vary [9,10]. According to the WHO, United States Preventive Services Task Force and the American Cancer Society women should start cervical cancer screening at the age of 21 at least once every three-five year interval. Ethiopia also adopted the “see and treat” strategy using Visual Inspection with Acetic acid (VIA) and cryotherapy for women age thirty and above unless HIV positive [11-13].
Even though cervical cancer can be fully treated through screening; the trend of new cases is being increasing year to year and the service is hardly utilized.
In developed countries, the achievement of screening coverage was more than 80%. However, many developing countries did not get such success. In Ethiopia the coverage of screening is 0.8% at national level and 0.4% in the rural area of women age of 25-64 years.
This low cervical screening coverage is a big problem to prevent and control of cervical cancer in the developing countries and the reasons for not utilizing a cervical screening were found to be fear of procedure, fear of negative outcome, low awareness of services, embarrassment, privacy issues, societal stigma, cost and health service systems: Accessibility, time and health provider attitude towards the utilization.
The prevention efforts in the world have focused on screening of women at risk of disease and scholars suggested that the current screening status at this level did not bring significant changes on the incidence and mortality of cervical cancer unless involving the female health workers and also recommended to consider the health workers for the successful program of cervical cancer screening.
Ethiopia currently launched a strategy of national cancer control program for the next 5 years pertaining to National health sector transformation plan /HSTP/ 2015/16-2019/20 to reduce cancer burden through primary prevention, life style change, screening and early diagnose in order to reach 80% of screening coverage through conducting community awareness on the availability, importance of screening and treatment.
Identifying the associated factors of utilization of cervical cancer screening in female health worker is important to increase overall screening rates. A study suggested focusing on public health practitioners has a potential to improve the uptake of cervical cancer screening in the community [2]. Hence, this study aims to get a better understanding on utilization and associated factors on female health workers in Arba Minch town and Zuria-woreda public health institutions, Southern Ethiopia, from getting cervical cancer screening. The finding will also assist policy makers and managers to design program that helps as an input for evidence based decision making.
Materials and Methods
Institution Based cross-sectional study was employed from March 15 to May 15, 2017 among 364 female health workers who works in public health institutes in Arba Minch town and Zuria woreda.
The source and study population of the study was all female health workers working in Arba Minch town and Zuria-woreda public health institutions. Female health workers who are working in Arba Minch town and Zuria-woreda public health institute and whose age is 21 and above were included in the study and female health workers who are severely ill and unable to respond during data collection time were excluded.
First, a list of all health workers was obtained from respective health offices and female health workers had been registered with number and a sample frame was also constructed for all 364 female health workers working in public health facility in the Arba Minch town and Zuria-woreda then with computer generated technique, the sample were selected for the study participants.
Utilization of cervical cancer screening is the dependent variable of the study and the independent variables include; sociodemography variables, knowledge of female health worker about cervical cancer screening, perception of susceptibility about cervical cancer and screening, perception of severity about cervical cancer and screening, perception of Benefits about cervical cancer and screening, perception of barriers about cervical cancer and screening, available and Acceptable Health service delivery.
Data quality management
Training was given for data collectors and supervisor; and Pretest was conducted on 5% of the sample. Based on the pre-test, modification was made on the questionnaire. Data compilation system and data completeness were checked and strictly controlled by principal investigator and supervisors. Data were entered using EPI info version 7.2.0.1 and exported to SPSS version 20 software packages. Double data entering, and random checking was done to ensure the validity of the study. The issue of confidentiality and privacy would be given more emphasis during the training session and data collection time.
Data processing and analysis
Data analysis was carried out using SPSS version 20. Frequency distribution, percentages, graphs and proportion was computed. A binary logistic regression was used to determine the relationship between the outcome and each independent variable and those variables having P value of <0.25 in binary logistic regression analysis were candidates for multivariable logistic regression analysis and inferences were made with 95% of confident interval and significant of p-value less than 0.05.
Ethical consideration
This study was approved by Institutional Review Board of Arba Minch University School of medicine and public health. An official letter of co-operation was written to concerned body, from Arba Minch University public health department. A Letter from the Research Ethics Committee has been submitted to the town and Zuria health office to get permission for conducting the study in health facility. Respondents were informed about the objective and purpose of the study and verbal consent was obtained from each respondent before administering the and also confidentiality had been maintained throughout the study.
Results
Socio-demographic characteristics of the respondents
Out of the total respondents, 281 were responded to the questionnaire, making the response rate of 95.6%. The age of participant’s ranges from 23 to 58 years with mean of 30.37 and standard deviation of ±5.96. Majority 131 (46.6%) of the respondents were in the age group of 28-30 years. The work experiences of the respondents range from 1 to 37 years with mean of 7.44 and standard deviation of ±5.72. 164 (58.4%) of the study participants were orthodox followers, followed by protestants 114 (40.6%). Majority 183 (65.4%) of the respondents were Gamo, and 77 (24.4%) were Amhara (Table 1).
| Variable |
Category |
Frequency |
Percentage (%) |
| Age group |
21-29 |
166 |
59.07 |
| 30-39 |
93 |
33.09 |
| 40-49 |
13 |
4.62 |
| 50+ |
9 |
3.2 |
| Religion |
Orthodox |
164 |
58.36 |
| Protestant |
114 |
40.57 |
| Others* |
3 |
1.07 |
| Ethnicity |
Gamo |
183 |
65.1 |
| Amhara |
77 |
24.4 |
| Others* |
21 |
7.5 |
| Marital status |
Single |
75 |
26.9 |
| Married |
206 |
73.3 |
| Number of birth/parity |
Nulli para |
90 |
32 |
| 1-2 child |
152 |
54.1 |
| >3child |
39 |
13 |
| Type of profession |
Nurse |
204 |
72.6 |
| Health officer |
77 |
27.4 |
| service year |
<7 year |
145 |
51.4 |
| >7 year |
136 |
48.4 |
| Educational status |
Diploma |
211 |
75 |
| Degree |
70 |
25 |
| *Others religion: Muslim and Adventist; *Others ethnicity:Burji, Derashe, Gofa Gurage, Oromo, Wolayta |
Table 1: Socio-demographic characteristics of Percentage distribution of the female health workers in Arba Minch town and zuria woreda, Arba Minch, Ethiopia, April 2017 (n=281).
Knowledge of female health workers on cervical cancer screening
About 248 respondents had known the availability of cervical cancer screening service in their health facility or around their residents. The main sources of information were mass media (36.3%) followed by training (25.6%) and doctors (23.5%). Among respondents 20.6% had mentioned HPV and multiplesexual intercourse was the risks factors respectively. Around half of respondents cited that both women in the reproductive age groups and age above 50 years were vulnerable to cervical cancer. About 72.4% of the respondents had stated one or two symptoms of cervical cancer (vaginal bleeding and foul vaginal discharge), and 25.3% had cited three and above symptoms (vaginal bleeding, foul smelling of vaginal discharge, contact bleeding and post-menopausal bleeding). From all respondents the most mentioned symptom was Vaginal bleeding 108 (38.4%). Around 35.6% of respondents did not know the way of any kind of screening, however, 24.5% had known at least three screening types (Pap smear, Visual inspection with acetic acid (VIA) and Lugol’s solution (VILI). About 66% of the respondents mentioned that one of a prevention method was avoiding multiple- sexual intercourse. Regarding cervical screening, 51.2% of respondents had cited that women whose age is 30 and above were the target groups and 35.6% respondents had quoted women whose age is 21 and above were the target groups (Table 2).
| Variable |
Responses |
Frequency |
Percent |
| Risk of cervical cancer |
Multiple sexual intercourse, early sex, HPV, smoking |
34 |
12.1 |
| Multiple sexual intercourse, early sex, HPV |
42 |
14.9 |
| Multiple sexual intercourse and early sex |
83 |
29.5 |
| HPV |
48 |
20 |
| Multiple sex |
48 |
20 |
| Don’t know |
26 |
9.2 |
| Symptoms of cervical caner |
Vaginal bleeding, foul smelling of vaginal discharge, contact bleeding and post-menopausal bleeding |
41 |
15.6 |
| Vaginal bleeding and discharge |
83 |
29.5 |
| Vaginal bleeding |
46 |
44.8 |
| Vaginal discharge |
41 |
14.6 |
| Contact bleeding |
34 |
12.1 |
| Don’t know |
36 |
12.8 |
| Prevention method |
Avoid multiple sex, avoid early sex, HPV vaccine, quit smoking |
48 |
17 |
| Avoid multiple sex, HPV vaccine |
119 |
42.3 |
| Avoid multiple sex |
65 |
50.5 |
| HPV vaccine |
37 |
13.2 |
| Don’t know |
32 |
11.3 |
| Method of screening |
PAP, VIA, VIL, HPV DNA |
64 |
22.7 |
| Pap and VIA |
39 |
13.8 |
| PAP smear |
57 |
20.2 |
| VIA |
21 |
7.4 |
| Don’t know |
100 |
35.6 |
Table 2: Assessment of knowledge on the risk, symptoms, prevention of cervical cancer and method of cervical cancer screening among female health workers in Arba Minch town and Zuria woreda, 2017.
Perception of study participants towards cervical cancer screening
Perception of study participant was computed from the total mean of the perception. Respondents who have a mean score of 4.07 and above were considered as having positive perception, while those having perception score less than 4.07 are considered as having negative perception. In this study, around 50.2% of respondents had a positive perception and 49.8% had negative perception towards the cervical cancer screening. Among those screened female health workers, 70.4% believed that they were susceptible to cervical cancer, 77.8% perceived that screening could help to show the pre-cancerous stage earlier and also 77.8% had perceived to consult doctors without scared.
Perceived susceptibility
The total respondents, 147 (52.3%) had strongly agreed that all reproductive age group women can acquired cervical cancer.
Perceived seriousness
About 58.5% of female health workers had strongly agreed as cervical cancer is one of the most prevalent cancer in Ethiopia.
Perceived benefits
Around 60% of the respondents had strongly perceived that screening can prevent from getting cervical cancer and detect pre-cancerous changes earlier and 52.3% of the respondents perceived that screening has no harm to the clients.
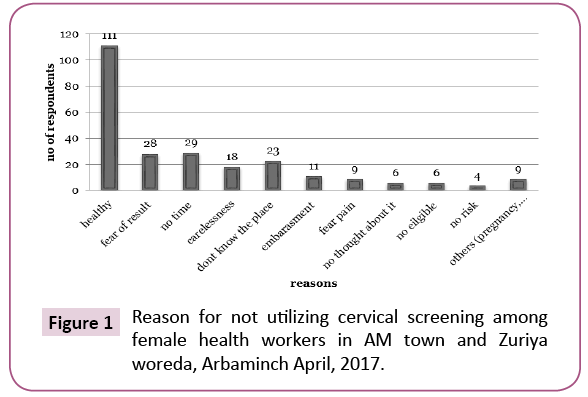
Perceived barriers
The main reason of not being screened were; considering themselves as a healthy (39.5%), lack of time (10.3%) and fear of result (10.0%) respectively (Figure 1).
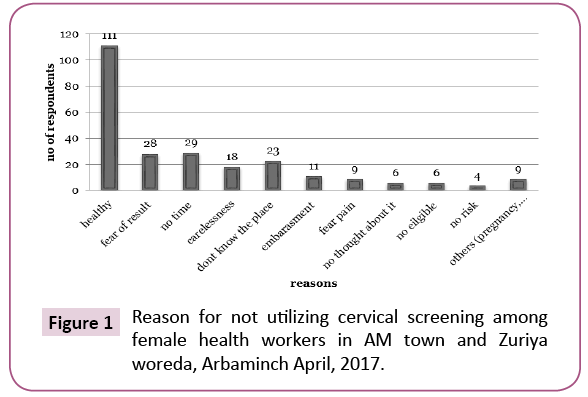
Figure 1: Reason for not utilizing cervical screening among female health workers in AM town and Zuriya woreda, Arbaminch April, 2017.
Perceived self-efficacy
One hundred twenty (42.7%) of the respondents were strongly agreed with screening, even though the service is expensive and 47.3% didn’t agree since they believed that the screening service is embarrassed. Among those screened 93.6% recommend to others.
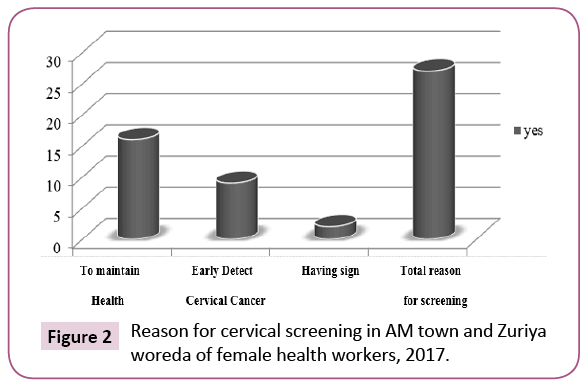
Utilization of cervical cancer screening
Out of the total respondents, 9.6% of them utilized cervical cancer screening service and their main reason for utilization of the service was to maintain healthy (59.8%) and to detect early cervical cancer change (33.3%) (Figure 2).
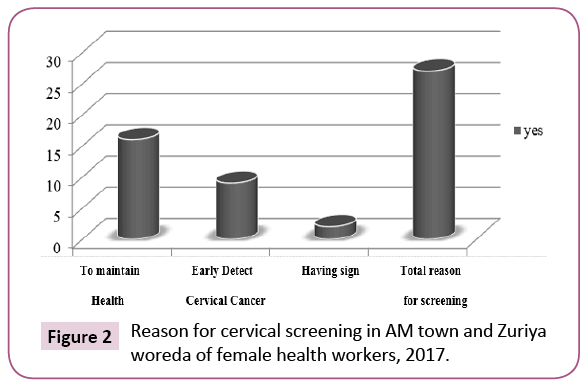
Figure 2: Reason for cervical screening in AM town and Zuriya woreda of female health workers, 2017.
Factors associated with utilization of cervical cancer screening
Service year of the respondents and knowledge were independently associated with ever screening for cervical cancer. The odds of ever screening for cervical cancer is 5 times higher for those who served more than or equal to 7 years than those who served less than seven years (AOR [95% CI]=4.99 [1.36- 18.10]). Knowledge about cervical cancer is also associated with utilization of cervical cancer. Those respondents who have good knowledge about cervical cancer were 1.78 times more likely to utilize cervical cancer screening compared to those who have poor knowledge about cervical cancer (AOR [95% CI] = 1.78[1.05- 3.02]) (Table 3).
| Variable |
Ever screened
YesNo |
COR [95 % CI] |
AOR[95 % CI] |
P value |
| Age |
| <30 year |
3 |
45 |
1 .00 |
1 |
|
| >30year |
16 |
51 |
3.90 (1.64-9.27) |
1.64 (0.588-4.60) |
0.341 |
| Educational status |
| Diploma |
16 |
195 |
1 |
1 |
|
| degree |
11 |
59 |
1.80(0.73-4.36) |
1.32(0.49-3.54) |
0.574 |
| Marital status |
| Single |
5 |
70 |
1 |
1 |
|
| Married |
22 |
184 |
1.64(0.61-4.51) |
1.47(0.45-4.78) |
0.769 |
| Source of information |
| Media |
8 |
67 |
0.37(0.50-4.59) |
- |
- |
| Training |
9 |
57 |
0.13(0.69-5.97) |
0.72(0.48-1.07) |
0.108 |
| doctors |
10 |
130 |
1 |
1 |
- |
| service year |
| <7 years |
6 |
176 |
1 |
1 |
- |
| >7 years |
21 |
78 |
5.49(1.38-21.13) |
4.99(1.36-18.10) |
0.013* |
| Knowledge |
| Good |
13 |
65 |
3.00(1.08-8.31) |
1.78(1.05-3.02) |
0.033* |
| Moderate |
8 |
99 |
2.47(0.97-6.30) |
- |
| Poor |
6 |
90 |
1 |
1 |
- |
| Allow male providerto be screened |
| Agreed |
23 |
214 |
1.85(0.69-4.91) |
1.43(0.39-5.22) |
0.583 |
| Disagreed |
4 |
40 |
1 |
1 |
- |
Table 3: Analysis of factors for utilization of cervical cancer screening among the female health workers in Arba Minch town and zuria woreda, Arba Minch Ethiopia, April 2017 (n=281).
Discussion
In this study, the level of utilization of cervical cancer screening is 9.6%, which is almost similar to studies conducted in Niger (9%), Nigeria (10%) and Mekele (10.7%). The possible reason for this low level is mainly resulted from the insufficiency of knowledge about cervical cancer screening. However, the result of this study is quite lower as compared to studies from Qatar (42.2%), Bagdad (18.8%), Turkey (54.2%), Uganda (19%), Tanzania (15.4%) and Addis Ababa (17%). This difference may be due to the difference in strategies to make conducive situation and comprehensive screening of cervical cancer [14-25].
This study revealed that, service year (AOR [95% CI]=4.99 [1.36- 18.10]) and knowledge of cervical cancer (AOR [95% CI]=1.78 [1.05 - 3.02]) were found to be significantly associated factors for cervical cancer screening. However, service year of the respondents were not being significantly associated with the uptake of cervical screening in Mekele [18], India and Nigeria [26- 29]. This might be due to the fact that female health workers who have higher work experience may have repeated information and exposure with patients that help themselves to be screened.
Regarding to knowledge, knowing about cervical cancer and screening had a significant relation with ever screened in this study which is almost similar with other studies which was done in Nigeria, Bagdad, India and Addis Ababa [17-27]; this might be due to the fact that health workers translated their knowledge to practice. However, knowledge of cervical cancer screening was not associated with the utilization of cervical screening in studies conducted in India and Nigeria. This may be due to less awareness creation about the service in the later studies and also most health workers did not interpret their knowledge to the utilization of the screening services [29].
Strength and limitation of the study
Strength
By ensuring privacy during the completion of the questionnaire and using the self-administered, an attempt was made to minimize social desirable bias.
Limitation
The findings in this study were more descriptive. Whereas further research is needed to explore deeply with qualitative approach to dig a hidden part that why not screened for cervical cancer.
Conclusion
This study showed that, utilization of cervical cancer screening is very low (9.6%). Knowledge of cervical cancer screening and service year were factors significantly associated with the outcome variable.
Based on the findings the study the following recommendations are forwarded.
1. More should be done on awareness creation and sensitization of health workers on cervical cancer screening and sustaining national screening programs widely.
2. Health workers need to be marked at first since they have crucial role in any potential screening activities in order to achieve screening coverage in the community.
3. Even though, knowledge is necessary it is usually insufficient to change individual behavior. So that motivation and sensitization needed for health workers about cervical cancer and the importance of screening to raise the uptake of screening besides to this, strategies should be designed for cervical cancer test to avoid barriers through advocacy.
Authors’ Contribution
TS wrote the proposal, participated in data collection, analyzed the data and drafted the paper. AY, GK and FG approved the proposal with great revisions and revised subsequent drafts of the paper. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest that competes with any of the contents of the manuscript.
21517
References
- Abate SM (2015) Trend of cervical cancer in Ethiopia. Cervical Cancer 1: 103.
- Ali F, Kuelker R, Wassie B (2012) Understanding cervical cancer in the context of developing countries. Ann Trop Med Public Health5: 3-15.
- Bruni L, Barrionuevo-Rosas L, Albero G, Aldea M, Serrano B, et al. (2016) ICO information centre on HPV and cancer (HPV Information Centre). Human papilloma virus and relateddiseases in world. Summary Report. October 7, 2016. [dataaccessed]
- Popat K, McQueen K, Feeley TW (2013) The global burden of cancer. Best PractRes Clin Anaesthesiol27:399-408.
- Bosch FX, Manos MM, Munoz N, Sherman M, Jansen AM, et al. (1995) Prevalence of human papillomavirus in cervical cancer :Aworldwide perspective. JNCI 87: 796-802.
- Smith JS, Lindsay L, Hoots B, Keys J, Franceschi S, et al. (2007) Human papillomavirus type distribution in invasive cervical cancer and high ÃÂgrade cervical lesions: A meta ÃÂanalysis update Int.J Cancer 121: 621-632.
- Chidyaonga-Maseko F, Chirwa ML, Muula AS (2015) Underutilization of cervical cancer prevention services in low and middle incomecountries: A review of contributingfactors. Pan Afr Med J 21:231.
- Giakdon E, Nordhagen S, Obermeyer Z (2008) Coverage of cervical cancer screening in 57 countries Low averagelevel and large in equality.PLOSMed5:e132.
- Broutet N (2014) Comprehensive cervical cancer control, a guide to essential practice.(2ndedn). World HealthOrganization,Geneva,Switzerland.
- Aldrich T, Becker D, Garcia SG, Lara D (2005) Mexicanphysiciansknowledge and attitudes about the human papillomavirus and cervical cancer: A national survey. SexTransm Infect 81:135-141.
- Virginia AM (2012) Screening for cervical cancer: U.S. preventive services task force recommendationstatement. Ann Intern Med156: 880-891.
- Co C (2002) Cancer prevention and earlydetectionfacts and figures 2008. American Cancer Society, Atlanta, Georgia, USA.
- Greenwald P, Cullen JW (1984) The scientificapproach to cancer control. CA Cancer J Clin 34: 328-332.
- Lim JN, Ojo AA (2016) Barriers to utilisation of cervical cancer screening in Sub Sahara Africa: A systematicreview. EurJ Cancers Care 26.
- Sedigheh SS (2012) Predictors of cervical cancer screening : An application of healthbelief model. InTopics on cervical cancer with an advocacy for prevention. InTech.
- Nwobodo H, Ba-Break M (2015) Analysis of the determinants of low cervical cancer screening uptakeamongNigerianwomen. J Public HealthAfr6:12-19.
- Arulogun OS, Maxwell OO (2012) Perception and utilisation of cervical cancer screening services amongfemale nurses in UniversityCollege Hospital, Ibadan, Nigeria. Pan Afr Med J 11.
- Gebreegziabher M, Asefa NG, Berhe S (2016) Factorsaffecting the practices of cervical cancer screening amongfemale nurses at public health institutions in Mekelle Town, NorthernEthiopia, 2014: A Cross-Sectional Study. J Cancer Res 2016 : 7.
- Anantharaman VV, Sudharshini S, Chitra A (2013) A cross-sectional study on knowledge, attitude, and practice on cervical cancer and screening amongfemalehealth care providers of Chennai Corporation. JAcad Med Sci2:124-128.
- Thippeveeranna C, Mohan SS, Singh LR, Singh NN (2013) Knowledge, attitude and practice of the pap smear as a screening procedureamong nurses in a tertiaryhospital in northeasternIndia. Asian Pacific J Cancer Prev14: 849-852.
- Mutyaba T, Mmiro FA, Weiderpass E (2006) Knowledge, attitudes and practices on cervical cancer screening among the medicalworkers of Mulago Hospital, Uganda. BMC BMC Med Edu6: 13.
- Al-Meer FM, Aseel MT, Al-Khalaf J, Al-Kuwari MG, Ismail MF (2011) Knowledge, attitude and practices regarding cervical cancer and screening amongwomenvisitingprimaryhealth care in Qatar. East MediterrHealth J 17: 855.
- Rashied AM, Abbas I (2014) Barriers for up taking the Pap smearamong Nurse- Midwives in Baghdad City Hospitals. Kufa J Nursing Sci4.
- Kerim DB (2011) Knowledge and applications of midwife and nurses at educationalhospitals on the early diagnose of cervical cancer. Asian Pacific J Cancer Prev12: 481-485.
- Urasa M, Darj E (2011) Knowledge of cervical cancer and screening practices of nurses at a regionalhospital in Tanzania. AfricanHealthSci11: 48-57.
- Ibekew RU (2015) A comparative assessment of knowledge, attitude and practice of cervical cancer and its screening amongclinicalstudents in south Nigeria. Nigeria Health J 15:55-61.
- Adanu RM (2002) Cervical cancer knowledge and screening in Accra, Ghana. J Womens Health Gender-Based Med 11: 487-488.
- Swapnajaswanth M, Suman G, Suryanarayana SP, Murthy NS (2014) Perception and practices on screening and vaccination for carcinoma cervix amongfemalehealthcareprofessional in tertiary care hospitals in Bangalore, India. Asian Pac J Cancer Prev15: 6095-6098.
- Oche MO, Kaoje AU, Gana G, Ango JT (2013) Cancer of the cervix and cervical screening:Currentknowledge, attitude and practices of femalehealthworkers in Sokoto, Nigeria. Int J Med 5: 184-150.