Case Report - (2022) Volume 13, Issue 1
Uveitis and Acute Myelitis after COVID-19
Narjes Gouta*,
Mariem Mhiri,
Rihab Ben Dhia,
Mouna Aissi and
Mahbouba Frih-Ayed
Department of Neurology, Fattouma Bourguiba Hospital, Monastir, Tunisia
*Correspondence:
Narjes Gouta, Department of Neurology, Fattouma Bourguiba Hospital, Monastir,
Tunisia,
Tel: +21695034905,
Email:
Received: 16-Jan-2022, Manuscript No. ipjnn-22-12328;
Editor assigned: 18-Jan-2022, Pre QC No. P-12328;
Reviewed: 13-Feb-2022, QC No. Q-12328;
Revised: 16-Feb-2022, Manuscript No. R-12328;
Published:
23-Feb-2022
Abstract
A number of neurological disorders have been reported to be associated with the novel corona virus (COVID-19) including acute stroke, encephalitis, convulsions, peripheral neuropathy and rarely myelitis. Multiple other symptoms have been reported such as uveitis. In this article we presented the case of a 32-year-oldwoman who was presented to hospital with proprioceptive ataxic walking, progressive lower limb weakness, urinary retention and visual blur. She had been diagnosed with COVID-19 four days before the appearance of symptoms. Clinical examination showed weakness, hyporeflexia, hypoaesthesia of both lower limbs and intermediate uveitis. The evolution was marked by the total regression of the motor deficit and partial regression of the visual blur after treatment with intravenous methylprednisone. It is important to recognize potential neurologic manifestations and complications of the noval corona virus especially when some of which can be rapidly progressing and require urgent intervention.
Keywords
COVID-19; Myelitis; Uveitis
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease
caused by a recently discovered coronavirus. The majority
of people with COVID-19 experience only mild or moderate
symptoms and recover without special treatment. Neurological
manifestations and complications of acute and post COVID-19
are common, ranging from mild nonspecific symptoms to severe
manifestations such as encephalopathy and myelitis [1]. Acute
myelitis is an acute inflammation of gray and white matter leading
to muscle weakness and paralysis. In the medical literature only
few cases of acute myelitis associated with COVID-19 infection
are reported. Uveitis after COVID-19 disease is rarely reported.
In this paper, we report the case of acute myelitis associated
with uveitis occurring after COVID-19 infection. Mechanism and
treatment of neurologic manifestations are discussed.
Case Report
A 32-year-old woman was admitted for gait disorder, vesicosphincter
disorder and visual blurring evolving for 2 weeks.
These symptoms appeared four days after PCR proven infection
with coronavirus 19. The evolution was marked by progressive
worsening of walking, becoming ataxic and unstable, confining
the patient to bed. On the other hand, the visual blur has
gradually regressed spontaneously. The patient was admitted in the neurologic unit and the clinical examination showed ataxic
walking, unstable standing position, motor deficit and hypoestesis
in both lower limbs. Reflexes are abolished and there is a
suspended sensory level at C2- C3 to superficial tact and pinprick
testing. Otherwise, there is no cerebellar syndrome or cranial
nerves damage. The patient reported also urinary retention
but the perineal examination was without abnormalities.
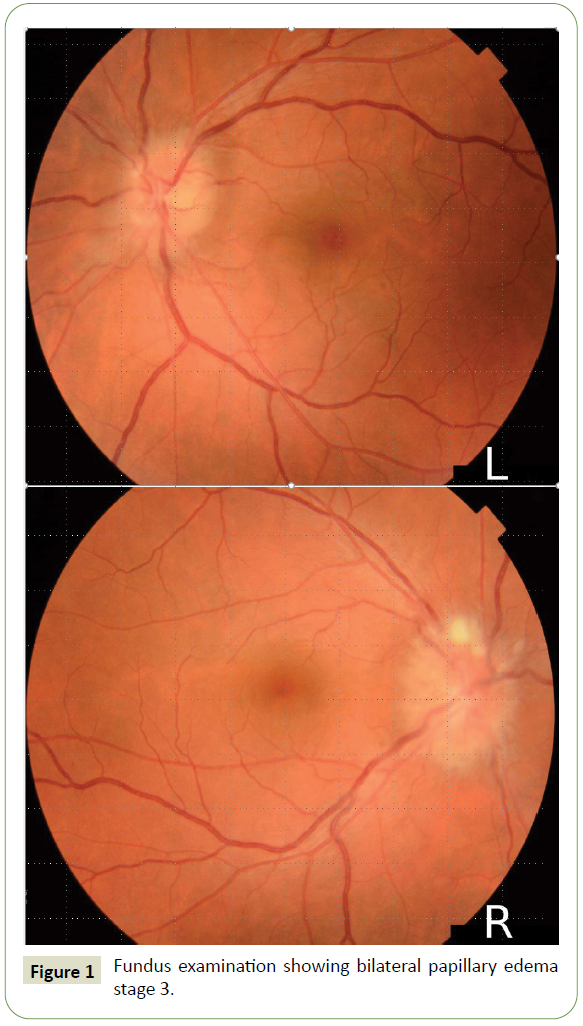
Ophthalmologic examination found bilateral papilledema stage 2
and intermediate uveitis (Figure 1). The Cerebrospinal Fluid (CSF)
analysis was normal. The serological testing of herpes simplex
virus (type 1 and 2), Epstein Barr virus, cytomegalovirus, human
immunodeficiency virus and hepatitis was negative.
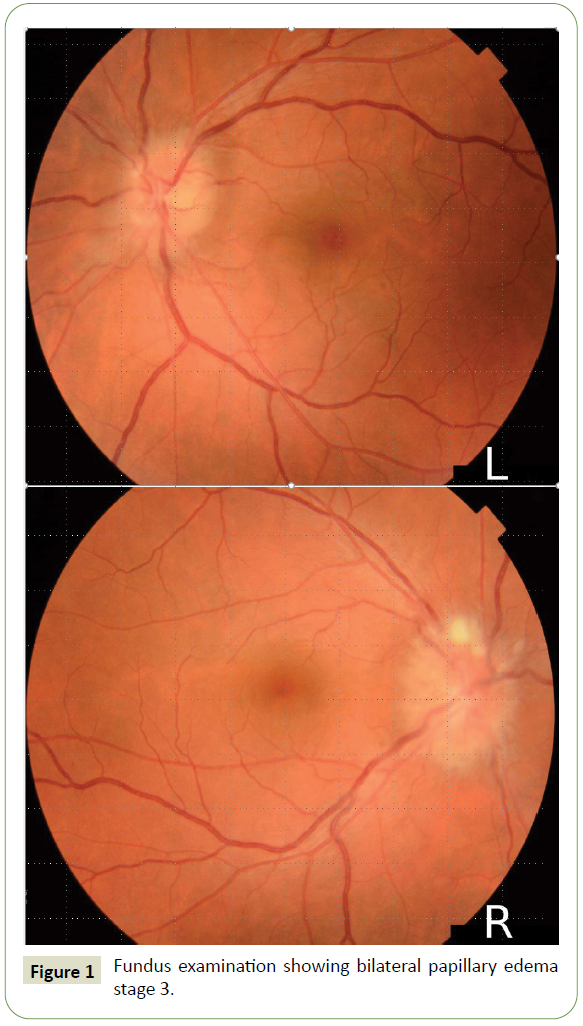
Figure 1: Fundus examination showing bilateral papillary edema stage 3.
Autoimmune tests were negative especially antinuclear,
aquaporin 4 antibodies and anti-Myelin oligodentrocytes
glycoprotein (MOG). The diagnosis of myelitis post COVID-19 was
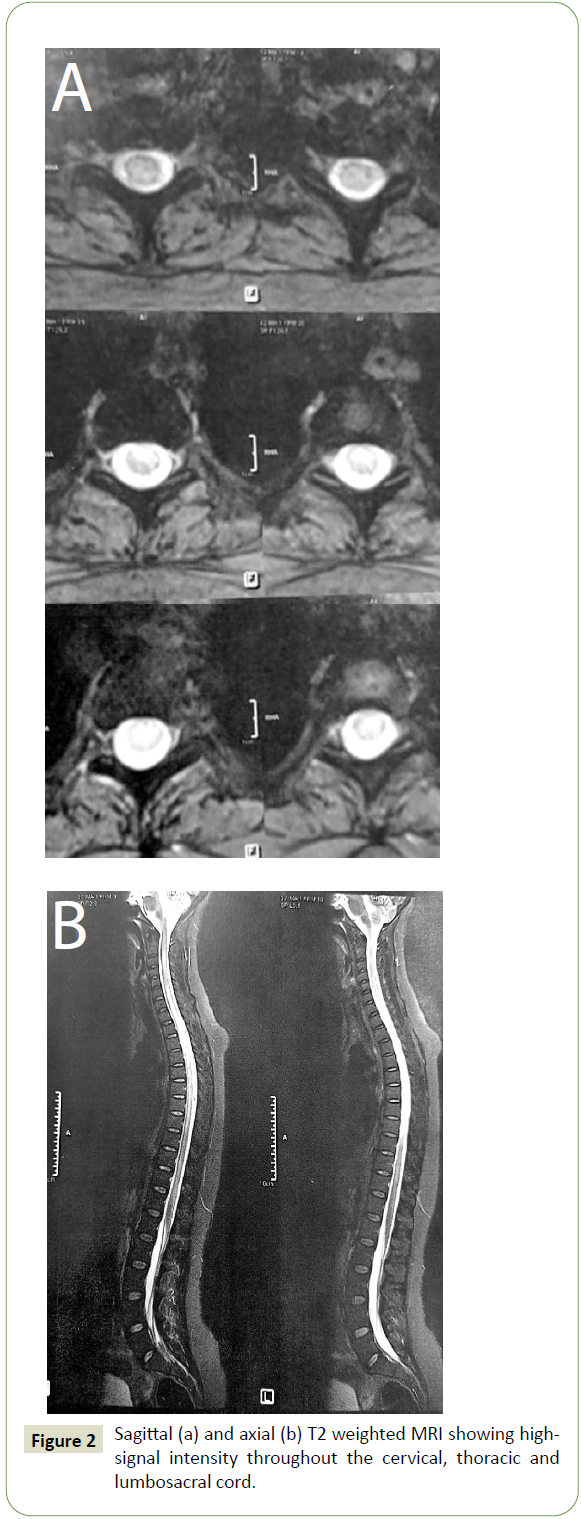
highly suggested. Brain MRI was normal and spinal MRI showed
diffuse high T2 signal throughout the cervical, thoracic, and
lumbosacral cord (Figure 2A). After gadolinium injection there is
enhancement of the entire spinal cord (Figure 2B). The patient
was treated with intravenous methylprednisolone (MP) 1 gram
per day for 5 days and then full dose oral corticosteroid therapy
with gradual reduction. The evolution was marked by the total
regression of the motor deficit and the visual blur after 2 months.
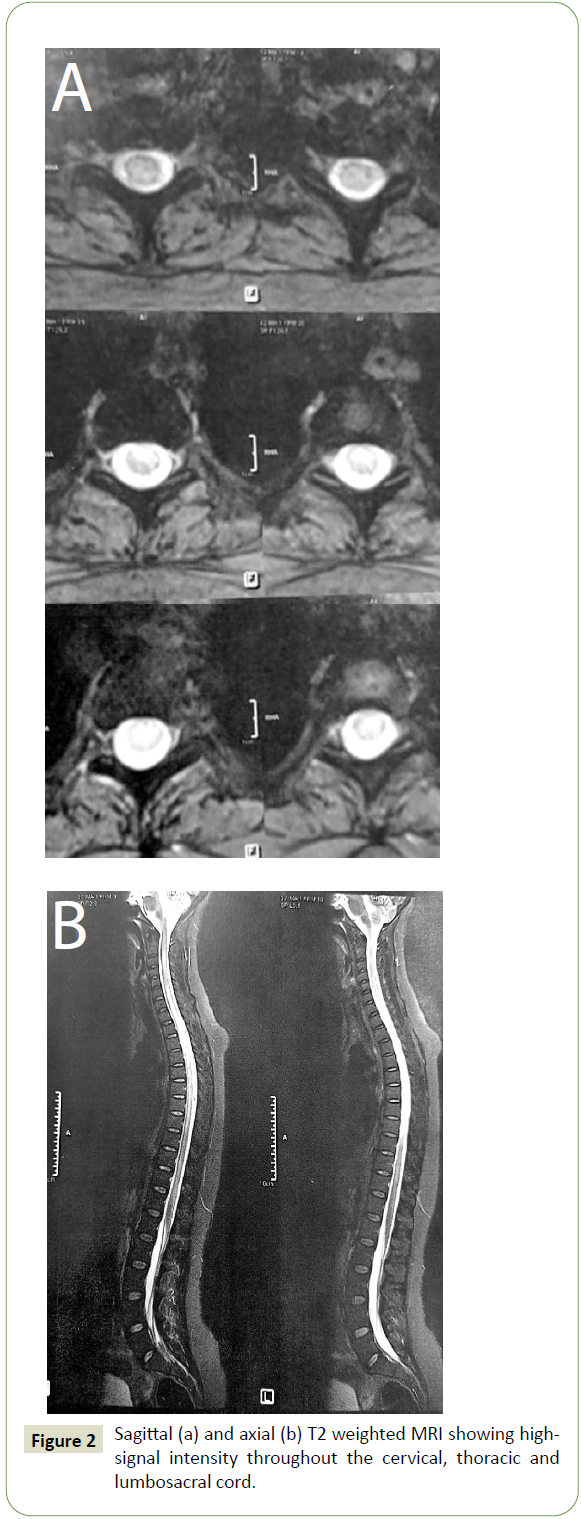
Figure 2: Sagittal (a) and axial (b) T2 weighted MRI showing highsignal intensity throughout the cervical, thoracic and lumbosacral cord.
The repeated ophthalmologic examination showed a regression
of the papillary edema passing to stage 1.
Discussion
In this paper we have presented a case of acute myelitis associated
with uveitis after recent COVID-19 infection. It is well known that
SARS-CoV-2 has a neurotropism with commonly nonspecific
neurologic complications as headache, myalgia, fatigue and
vomiting. Severe neurologic symptoms are rarely reported.
Among the Central Nervous System (CNS) features, acute stroke
is most frequently reported. Seizures, encephalitis and myelitis
are less described but being increasingly documented. Among
the peripheral nervous system Guillain Barre syndrome has
mostly been seen [1,2].
A Houston Methodist-led team of researchers have found
COVID-19 can result in an unexpectedly frequent occurrence of
Acute Transverse Myelitis (ATM), a rare but often devastating spinal cord disorder. The team's study of documented pandemic
cases found that 43 ATM involved an inflammation of the spinal
cord that prevents sensory and motor information from flowing
to the brain and the rest of the body. The cases occurred in both
developed and underdeveloped countries [3].
Several possible mechanisms exist by which SARS-CoV-2 could
lead to spinal cord manifestations. Coronaviruses have been
shown to be both neuroinvasive and neurovirulent and can lead
to demyelination and as well as an inflammatory response [4].
Since we did not detect SARS- CoV-2 RNA in the CSF of our patient,
we postulate that it would likely due to an immune- mediated
inflammatory process rather than direct invasion of SARS- CoV-
2 into the CNS. There are papers that emphasize a positive RTPCR
test for SARS-CoV-2 in CSF in the context of encephalitis,
which is not a common finding in other COVID-19 neurological
manifestations. These results highly suggest that there should be
other explanations for neurological symptoms associated with
COVID-19 disease [5,6].
To our knowledge, there is no evidence-based treatment
guidelines available for para-infectious ATM. If a para or
post-infectious pathogenesis is corroborated, intravenous
immunoglobulins (IVIG) may be another treatment option [4].
Concerning our patient, a spectacular improvement was the rule
under corticosteroid therapy.
Coronaviruses are known to cause various ocular infections in
animals such as conjunctivitis, anterior uveitis, retinitis, and
optic neuritis. Bettach E et al. [7] presented recently a case of
COVID-19 that presented initially to ophthalmology clinic with keratoconjunctivitis with small pseudo dendrite and small
subepithelial infiltrates in the cornea. It is well known that SARSCoV-
2 induces conjunctivitis. A study conducted on 38 COVID-19
infected patients showed that 5% of them had virus-positive
conjunctivitis and 32% had conjunctivitis. Moreover, retinal
hemorrhages, central retinal vein occlusion and other retinal
thrombotic complications have been observed in COVID-19
patients [8]. Intermediate post COVID-19 uveitis is very rarely
described in the literature so far. The stasis papillary edema would
be due to viral infection and not by intracranial hypertension
since the opening pressure at the lumbar puncture was normal as
well as the cerebral MRI. The improvement of edema and uveitis
by corticosteroid therapy supports this argument.
All physicians should keep in mind the possibility of uveitis in
the differential diagnosis when dealing with patients who had
previous viral prodromal symptoms up to a few weeks prior to
presenting with uveitis [8,9]. To the best of our knowledge, no
case of myelitis associated with post-COVID-19 intermediate
uveitis has been reported before.
Conclusion
Coronavirus remains a virus like all viruses that can cause postinfectious
myelitis but the prevalence, severity and prognosis of
post-COVID-19 myelitis remains to be determined. Thus, it is of
major importance to remain cognizant of the atypical and lessprevalent
sequelae of viral infections in patients with recent
COVID-19 infection, as prompt recognition and management are
important to prevent significant morbidity.
REFERENCES
- Yavarpour-Bali H, Ghasemi-Kasman M (2020) Update on neurological manifestations of COVID-19. Life Sci 15: 118063.
Google Scholar, Crossref, Indexed at
- Nepal G, Rehrig JH, Shrestha GS, Shing YK, Yadav JK, et al. (2020) Neurological manifestations of COVID 19: a systematic review. Crit Care 13: 421.
Google Scholar, Crossref, Indexed at
- Román GC, Gracia F, Torres A, Palacios A, Gracia K, et al. (2021) Acute Transverse Myelitis (ATM): Clinical Review of 43 Patients With COVID-19-Associated ATM and 3 Post-Vaccination ATM Serious Adverse Events With the ChAdOx1 nCoV-19 Vaccine (AZD1222). Front Immunol 12: 653786.
Google Scholar, Crossref, Indexed at
- Schulte EC, Hauer L, Kunz AB, Sellner J (2021) Systematic review of cases of acute myelitis in individuals with COVID-19. Eur J Neurol 28: 3230-3244.
Google Scholar, Crossref, Indexed at
- Águila-Gordo D, Flores-Barragán JM, Ferragut-Lloret F, Portela-Gutierrez J, LaRosa-Salas B, et al. (2020) Acute myelitis and SARS-CoV-2 infection. A new etiology of myelitis? J Clin Neurosci 80: 280-281.
Google Scholar, Crossref, Indexed at
- Munz M, Wessendorf S, Koretsis G, Tewald F, Baegi R, et al. (2020) Acute transverse myelitis after COVID-19 pneumonia. J Neurol 267: 2196-2197.
Google Scholar, Crossref, Indexed at
- Bettach E, Zadok D, Weill Y, Brosh K, Hanhart J (2021) Bilateral anterior uveitis as a part of a multisystem inflammatory syndrome secondary to COVID‐19 infection. J Med Virol 93: 139-140.
Google Scholar, Crossref, Indexed at
- Iriqat S, Yousef Q, Ereqat S (2021) Clinical Profile of COVID-19 Patients Presenting with Uveitis. A Short Case Series. Int Med Case Rep J 14: 421-427.
Google Scholar, Crossref, Indexed at
- Hung JCH, Li KKW (2020) Implications of COVID-19 for uveitis patients: perspectives from Hong Kong. Eye (Lond) 34: 1163-1164.
Google Scholar, Crossref, Indexed at
Citation: Gouta N, Mhiri M, Dhia RB, Aissi M, Frih-Ayed M (2022) Uveitis and Acute Myelitis after COVID-19. J Neurol Neurosci Vol.13 No.1:409