Keywords
Step test; Two-minute step test; Elderly; Elderly population; Senior function test; Aerobic capacity; Elderly rehabilitation; Physical capacity and Neurological rehabilitation
Introduction
General fitness often decreases with age but it is essential for quality of life. Therefore, it becomes essential to find out a method of evaluation of individual fitness level for appropriate exercise program [1]. Physical fitness parameters such as strength, flexibility, coordination, and endurance cannot be determined using tools such as Barthel Index or Lawton scale. A key factor in preserving mobility and independence in later years is maintaining the fitness capacity (e.g., strength, endurance, agility, and balance) needed to perform normal everyday activities—to do simple housework, climb steps, lift and carry objects, get in and out of chairs or transportation vehicles, and walk far enough in and around stores, buildings, and parking lots to do one’s own shopping [2].
Currently there are various techniques used for elderly physical and aerobic capacity in this study we have tried to explore the potential usage of two-minute step test as indicator to measure the aerobic and physical capacity. We believe that endurance is important to assess in this population of older people without current acute problems living in the community for 2 reasons: (1) we believe there is a relationship between fatigue and the decline of physical function and loss of independence which is commonly seen in various neurological impairments and (2) we contend that a relationship exists among endurance decline, health status, and the of risk factors for neurological disorders.
The few studies published regarding threshold requirements for independent living primarily have involved laboratory-based measures, such as maximum oxygen uptake, peak oxygen consumption, or maximum muscle torque measures that provide important information for the scientific community but which are not well understood or easily interpreted by most health professionals, program leaders, or by older adults themselves [3,4]. The two-minute step test provides critical information regarding the response to exercise and the activity which is major part of neurological assessment and rehabilitation, Among elderly people with frailty, we suggest that an emphasis on identifying the category of response (“deconditioned,” or “conditioned”) provides more useful information about the person’s neurological risks (and physiological safety) for loss of independence and planning for rehabilitation than the person’s level of performance (number of steps).
Field test of functional fitness for older adults—the Senior Fitness Test (SFT; Rikli & Jones, 1999, 2001 in press) was the first attempt to develop criterion standards for a comprehensive fitness test battery for older adults [5,6], standards that address the key physiological variables needed for independent functioning. Although mobility and physical independence can be attained in a variety of ways (through use of assistive technologies, public transportation, etc.) and is influenced by multiple factors— cognitive, psychosocial, physical, environmental, and financial. From the Senior Fitness Test Battery two minute step test is used in this research to find out the aerobic endurance and in turn physical capacity in elderly staying at old age home.
The 6 MWT has also been used as an outcome measure for patients participating in various rehabilitation programs but it has serious limitations in this context. Although the 6 MWT is currently advocated for evaluating functional exercise capacity [7] in elderly population regardless of the setting, in reality it is not feasible in most apartments, geriatric homes, and medical offices because of its requirement for a hall that is 30 meters long. This long-standing need for a practical, effective exercise evaluation tool that is independent of the dimensions of physical space takes on even more urgent importance with the new health care mandate for improving both efficiency of, and access to, home care.
SFT which had been designed out of a need for simple, easy to use tools to assess physical fitness in older adults, the SFT has proven to be a valuable resource for health and fitness professionals looking to obtain information about the physical status for older adults, either for research purpose or for practical application. Endurance in this population may indicate the physiological capacity for participating in neurological rehabilitation and provide some indication of the capacity of the older individual to perform ADL.
By identifying the fitness category, Rikli and Jones developed a comprehensive functional fitness test battery that included normative performance standards based on a nation-wide study of 7,183 older Americans aged 60–94 years [8-10]. Functional fitness was defined as “having the physiologic capacity to perform normal everyday activities safely and independently without undue fatigue”. The SFT was called the Fullerton functional fitness test when it was originally published with its supporting reliability and validity documentation and normative standards.
Methods
The project was approved by college ethical committee and geriatric home administration and the data were collected at Little sisters of poor Mysore Department of elderly Neurological Rehabilitation.
Participants
Subject participating in the study provided informed consent. In patients who were participating in neurological rehabilitation performed a 2 MST and 6 MWT as part of their routine functional evaluation Healthy subjects were volunteers from the rehabilitation staff, and families, and provided informed consent [11,12]. Subjects with significant neuromuscular, cardiovascular or skeletal impairment were excluded from testing.
Data collection
The following variables were collected: gender, age, diagnosis, heart rate (HR), O2 saturation (O2 sat), systolic and diastolic blood pressures), and rating of perceived exertion (RPE).
Procedures
With inpatients the two-minute step test and 6 MWT were done, the order was randomized for each patient, inpatient data were collected from chart reviews [13]. Patients performed the twominute step test and 6 MWT once; with a 30-minute rest period between tests. The 6 MWT was performed in halfway adjacent to gym and the two-minute step test was performed on a step located in the rehabilitation gym, It consisted of stepping up and down one -high step as rapidly as possible for 2 minutes. One step=one bilateral step up + one bilateral step-down [14-16]. Prior to beginning a test, subjects stood quietly for 2 minutes while HR, O2 sat, BP, and RPE were recorded. The same variables were assessed again immediately at test termination [17].
Prior to beginning the test, subjects were told:
“You are now going to do a 2-minute step test. You can hold the rail for balance, but do not pull yourself up while holding the rail. You may get out of breath [18,19]. You are permitted to slow down, stop or rest as necessary, but you should resume stepping as soon as you are able.”
“As you are stepping up and down, you will be informed of the time when there is 1 minute remaining, and when there are 15 seconds remaining. You will be encouraged to do your best. Please do not talk during the test unless you have pain or dizziness. When the 2 minutes are up, I will ask you to stop. Please stop immediately.”
“Remember that the object is to step up and down as many times as you can in 2 minutes, so remember to pace yourself.
Start stepping now!”
Data analysis
Validity of the 2 MST was determined by a Pearson correlation analysis between number of steps attained during the 2 MST and distance covered during the 6 MWT collected from a chart review of subjects enrolled in inpatient neurological rehabilitation [20], Physiologic response differences to the tests were evaluated using t-test analysis on HR, O2 sat, BPs, BPd, and RPE. The sensitivity of the 2 MST was evaluated by comparing the number of steps attained respectively by inpatients, and by healthy subjects.
Results
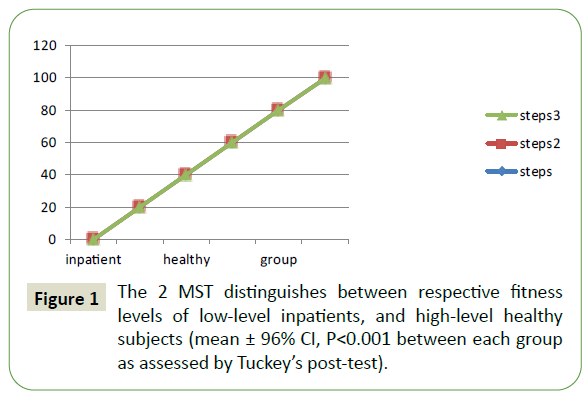
A total of 60 subjects (Table 1) were tested: 45 were inpatient neurological rehabilitation patients, and 15 were healthy volunteers. Validity was determined by comparing the basic data generated by the 2 MST and 6 MWT performed by inpatients, and by healthy subjects. The number of steps attained in the 2 MST and the distance covered in the 6 MWT were highly correlated (r=0.92, P<0.001) (Figure 1). There were no significant differences between the 2 MST and the 6 MWT in perceived exertion, oxygen saturation, or blood pressure (Table 2). Sensitivity of the 2 MST was evaluated from the ability to distinguish between different levels of function, compared the results from low-level subjects (the 60 inpatients) and healthy subjects (the 15 volunteers). Inpatients averaged 23.5 ± 11.3 steps (mean ± SD), compared to 66.4 ± 16.1 steps in the healthy population. (Figure 1).
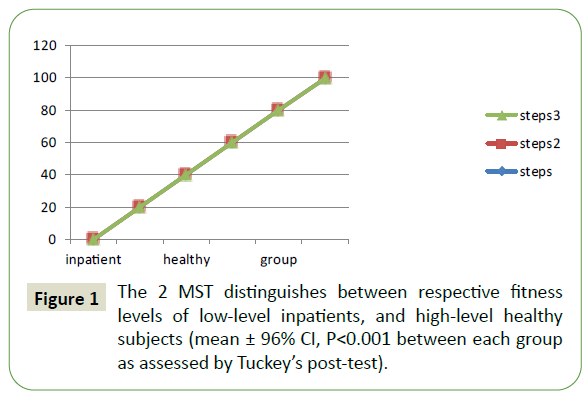
Figure 1: The 2 MST distinguishes between respective fitness levels of low-level inpatients, and high-level healthy subjects (mean ± 96% CI, P<0.001 between each group as assessed by Tuckey’s post-test).
| Variables |
N |
Age |
Height (cm) |
Weight (kg) |
| Inpatients |
Women |
32 |
77 ± 8 |
145 ± 7 |
64 ± 13 |
| Men |
13 |
75 ± 11 |
158 ± 9 |
76 ± 11 |
| Healthy |
Women |
9 |
78 ± 12 |
147 ± 8 |
61 ± 14 |
| Men |
6 |
76 ± 9 |
157 ± 7.6 |
72 ± 11 |
Table 1 Population demographics (mean ± SD).
| Variables |
2MST |
6MWT |
P-value |
| Heart Rate |
100.4 ± 25.5 |
97.6 ± 25.0 |
<0.001 |
| RPE |
13.0 ± 2.4 |
14.1 ± 6.9 |
NS |
| O2 Saturation |
95.8 ± 3.8 |
93.0 ± |
NS |
| BP sys |
130.6 ± 24.5 |
130.4 ± 25.2 |
NS |
| BPdias |
62.1 ± 12.0 |
63.2 ± 11.0 |
NS |
Table 2 Maximum heart rate (HR), perceived exertion (RPE), oxygen saturation (O2 sat), Systolic blood pressure (BPsys) and diastolic blood pressure (BPdias) attained during the 2MST and the 6MWT (mean ± SD).
Discussion
The initial population that we tested comprised patients discharged to inpatient neurological rehabilitation following acute hospitalization. They were all low-level patients with significant functional limitations. Our goal was a feasible test for aerobic assessment and neurological rehabilitation with results comparable to a known standard [21]. As shown in Table 2 peak HR, O2 saturation, and blood pressure response on the 2 MST were similar to those obtained in this low-level patient group with the 6 MWT. This similarity of physiologic variables was corroborated by the similarity in perceived exertion score. These values are similar to those observed in previous studies using the 6 MWT [22,23].
Results found in this study are similar to those in previous study for the measure of physical capacity in elderly population, major goal in this study was to observe 2 MST as predictor for the aerobic capacity in elderly population with neurological rehabilitation, as effective approaches to help older people maintain a healthy and active life are urgently needed, as the elderly have twice as many disabilities and four times as many physical limitations as people less than 60 years of age [20].
Conceptually, functional fitness [6] represents the physical capacity that is needed to undertake normal everyday activities, independently and without the early onset of fatigue, If elderly individuals do not take part in physically active lifestyles, they expose themselves to the risk of their muscle mass and joint motion reducing by 40% and 10%–40%, depending on body part, respectively, while loss of muscle strength (~30%) is related to a decrease in muscle mass [10].
Whilst research is prevalent regarding the functioning of older people generally, there are no published data regarding either aerobic capacity indicators or test markers for neurological rehabilitation of elderly people in Mysuru [8]. Like many cities, Mysuru has seen an increase in the age of its population, suggesting the need for this information. The rate of decrease of maximal oxygen consumption (VO2 max) [1] is not constant throughout life, but has been shown to accelerate significantly with each decade [11]. This decline is greater in men than women. Hawkins and Wiswell suggested that aerobic ability loss is nearly 10% per decade, which is similar to the results for the males in this study, whereas the women had almost identical aerobic abilities after 2 MST AND 6 MWT.
Weiss et al. suggested the decrease in VO2 max after 60 years of age was due to a drop in maximum cardiac output, as well as a reduction in the arterial/venous oxygen difference, which further limits their participation in various neurological rehabilitation activities or exercises. Measure of 2 MST can act as a predictor before planning the rehabilitation protocol [2] for the elderly population in need of neurological rehabilitation. These reductions in oxygen level difference take place more rapidly in men than women, although sex differences tend to vanish in the last decades of life [14].
Certain inherent factors such as patient sex, age, weight, height, muscle function could potentially influence results [16] and cannot be controlled for, Performance encouragement and familiarity with the test have been shown to increase the distance walked [17-23] using the 2 MST as an end point in an interventional investigation would require performing the test a minimum of two times prior to assessing the intervention or using 2 MST as one of indicator for planning of neurological rehabilitation protocols.
Several limitations in our study underline the need for further study to explore the sensitivity and use of 2 MST in greater detail. Because our control group was too small to distinguish between men and women, accurate normative data could not be derived [24]. A second limitation concerns the age difference between the patient groups and the healthy control group. The study thus must be repeated with an older healthy aging population.
In addition to confirming our findings, future studies are also needed to establish the minimal clinically significant performance difference in the 2 MST. Independent evaluation of predictive performance threshold values is required before these values can be used clinically with confidence. Finally, our single study assessing this new field test which could possibly be used as one of indicator for neurological rehabilitation must be followed by more to gauge the interpretability of the 2 MST and determine the degree to which change in test performance reflects clinical and functional changes
Conclusion
In conclusion, the measurement of functional status and physical capacity is an integral part of evaluating elderly fitness level and the impact of interventions such as neurological rehabilitation. The present study shows the 2 MST to be a low-cost, welltolerated, and accurate field test that can assess functional status and exercise tolerance in patients across a spectrum of fitness levels and in the limited physical space typically found in medical offices, acute care facilities, and in geriatric or old age homes.
39691
References
- Webb C, Vehrs PR, George JD, Hager R (2006) Estimating VO2 max using a personalized step test. Measurement in Physical Education and Exercise Science. 3:184-197.
- Różańska-Kirschke A, Kocur P, Małgorzata W, Dylewicz P (2006) The Fullerton Fitness Test as an index of fitness in the elderly: Medical Rehabilitation. 2: 9-16.
- Jessie Jones C, Rikli RE (2002) Measuring functional for older Adults. The Journal on Active Aging. 24-30.
- American College of Sports Medicine. (2010). ACSM’s guidelines of exercise testing and prescription Philadelphia: Lipincott Williams & Wilkins.
- Petrella RJ, Koval JJ, Cunningham DA, Paterson DH (2001) A self-paced step test to predict aerobic fitness in older adults in the primary care clinic. Journal of American Geriatrics Society. 49:632-638.
- Tuna HD, Edeer AO, Malkoc M, Aksakoglu G (2009) Effect of age and physical activity level on functional fitness in older adults. Eur Rev Aging Phys Act. 6: 99–106.
- Brach JS, FitzGerald S, Newman AB (2003) Physical activity and functional status in community-dwelling older women: a 14-year prospective study. Arch Intern Med. 163:2565–2571
- Kostić R, Pantelić S, Uzunović S, Djuraskovic R (2011) A comparative analysis of the indicators of the functional fitness of the elderly. Facta Univ Ser Phys Educ Sport. 9(2):161–171.
- Guyatt GH, Townsend M, Keller J, Singer J, Nogradi S (1991) Measuring Functional Status in Chronic Lung Disease: Conclusions from a Randomized Controlled Trial. Respiratory Medicine. 85:17-21.
- McDowell I, Newell C (1996) Mental Status Testing Measuring Health: A Guide to Rating Scales and Questionnaires. New York: Oxford University Press.
- Visser M, Goodpaster BH, Kritchevsky SB (2005) Muscle mass muscle strength and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. 60(3):324–333.
- Weiss EP, Spina RJ, Holloszy JO, Ehsani AA (2006) Gender differences in the decline in aerobic capacity and its physiological determinants during the later decades of life. J Appl Physiol. 101(3):938–944.
- Toraman N, Ayceman N, Yaman (2005) Effects of six weeks of detraining on retention of functional fitness of old people after nine weeks of multicomponent training. Br J Sports Med. 39(8):565–568.
- Brill PA (2004) Functional Fitness in Older Adults. Champaign (IL): Human Kinetics.
- Kervio G, Carre F, Vile NS (2003) Reliability and Intensity of the Six-Minute Walk Test in Healthy Elderly Subjects. Medecine Science Sports Exercise. 35:169-174.
- Seynnes, O, Fiatarone, S, Hue O, Pras P, Legros P, et al. (2004) Low-Moderate versus High-Intensity Progressive Resistance Training in Frail Elders. Journal Gerontology, 59:503-509.
- Westerterp KR (2000) Daily physical activity and ageing. Curr Opin Clin Nutr Metab Care. 3(6):485–488.
- García-Hermoso A, Cavero-Redondo I, Ramírez-Vélez R, Ruiz JR, Ortega FB, et al. (2018) Muscular strength as a predictor of all-cause mortality in an apparently healthy population: A systematic review and meta-analysis of data from approximately 2 million men and women. Arch. Phys. Med. Rehabil. 99:2100–2113.
- Sawada SS, Lee IM, Naito H, Kakigi R, Goto S, et al. (2014) cardiorespiratory fitness, body mass index, and cancer mortality: A cohort study of Japanese men. BMC Public Health. 14:1012.
- Bouchard C, Shephard RJ, Stephens T, Sutton JR, McPherson BD (1990) Exercise, Fitness, and Health: A Consensus of Current Knowledge. Human Kinetics.
- Astrand PO (1956) Human physical fitness with special reference to sex and age. Physiol. 36:307–335.
- Rikli RE, Jones CJ (2012) Development and Validation of Criterion-Referenced Clinically Relevant Fitness Standards for Maintaining Physical Independence in Late Years. Gerontologist. 53:255–267.
- Strassmann A, Steurer-Stey C, Lana KD, Zoller M, Turk AJ, Suter P, et al. (2013) Population-based reference values for 1-min sit-to-stand test. Int. J. Public Health. 58:949–953.
- Rikli RE, Jones CJ (2001) Senior Fitness Test Manual. Human Kineties. Exercises and multifunctional fitness on functional performance of elderly women from the community. J Nutr Health Aging 20 (4): 376 - 382.