Abstract
Teenagers' gynecomastia is becoming a significant cosmetic and physiological problem, particularly in the context of obesity, abrupt weight reduction following surgery, and other endocrine disorders. Surgery may involve nipple-conserving subcutaneous mastectomies with liposuction, power- or ultrasound-assisted mastectomies, or nipple transpositions using a variety of methods. In order to address the persistent problem of unsightly scarring, which manifests as obvious scar hypertrophy and nipple necrosis, various methods of nipple transposition have been developed, ranging from free grafts to pedicled flaps. In this case report, we call attention to an antiquated procedure that was used mostly for reduction mammoplasty on female patients back in the day and was first published by Passot in 1925. We would like to emphasise that this technique is still not utilised in gynecomastia surgery as commonly as the Wise pattern mastopexy procedure. That by employing this method and avoiding a vertical scar, patients with Simon IIB/III and ptotic gynecomastia would have superior cosmetic results.
Keywords
Reduction mammoplasty; Gynecomastia; Inferior pedicle;
Nipple transposition
INTRODUCTION
The abnormal or physiological expansion of the male breast
tissue is known as gynecomastia. Based on the
preponderance of glandular and fibro-fatty tissue,
respectively, it is classified as a true disease and a false
disease. Many classification schemes have been developed,
but the formerly subjective Simon1 and the more modern,
relatively objective Rohrich classifications have gained the
most traction. Surgery, medicinal therapy for the underlying
endocrine causes, and observation are all forms of
treatment. Additionally, there are a variety of surgical
procedures available, from liposuction to more invasive
excisions and mastectomies. Patients with little glandular
hypertrophy typically have little extra skin, making
liposuction an easy treatment option often the only option.
Power-assisted [1]. The capacity of traditional liposuction
alone to remove tissue has been improved by liposuction
and ultrasound-assisted liposuction technologies [2]. The
traditional Webster procedure4 and the bigger excisions in
the Wise pattern, Letterman, and Dufourmentel-Mouly
technique, to mention a few, are examples of excisional
operations [3]. Many of these, meanwhile, have only been
reported for reduction mastopexy in female patients,
therefore they have a number of drawbacks when used on
male patients [4]. The Wise pattern typically results in
coning of the breast and unfavourable scarring, and they
frequently leave behind too much glandular tissue [5].
There has also been a problem with the stigmatisation of
inverted "T" scars. Nipple transposition through a cephalad
buttonhole on the breast mound was reported by Passot as
having acceptable practical and aesthetic results [6]. This
method should likely be used considerably more frequently
than it is today, especially in severe cases of gynecomastia
[7]. We present a case of a kid who underwent a
subcutaneous mastectomy using the Passot technique and
had Simon 3, Rohrich IIB, and pseudo ptosis [8]. The
youngster had no immediate postoperative problems and
had an excellent cosmetic result at the future follow-up
visits [9]. A 17-year-old kid came to our outpatient
department with both breast growth and sporadic mastalgia
for five years [10]. The size of the breasts gradually rose and
stayed stable for one year. Endocrine and other underlying
conditions had been ruled out following a thorough
evaluation of the man. He was found to have bilateral
Simon III gynecomastia with pseudoptosis after evaluation.
He underwent a complete evaluation, which included a
general anaesthesia preoperative work-up. He underwent measurements and markings, then a subcutaneous
mastectomy with a Transposition of the inferior-pedicled,
de-epithelialized nipple flap. For nipple-areola-skin-saving
mastectomies, elliptical incisions based on the
inframammary groove on both sides were employed. After
the bilateral mastectomies, the new nipple sites were
indicated intraoperatively rather than the customary
preoperative site markings to achieve better symmetry. The
specimens from the mastectomy were weighed individually.
In order to assure adequate vascularity of the nipple-areola
complexes, the neo-nipple areola site was designated on
both sides. An inferior-pedicled nipple flap was created
bilaterally on the inframammary fold, being careful to
retain the flaps broad-based and tapering towards the apex.
The pedicled flap was tunnelled subcutaneously to the site
of the excised skin, which had a circular skin segment
removed that was 5 mm smaller in diameter than the NAC
ipsilaterally. In order to prevent bulging and saucerization
flaws at the new site, care was made to trim the pedicle
sufficiently. Subcuticular monocryl sutures were used to
create the neo-nipple areola. The superior mastectomy flaps
were stitched to the inframammary with Jackson Pratt
drains put posterior to the flaps. Using 4-0 subcuticular
monocryl sutures at the incision site groove. On the third
postoperative day, the patient was released without
incident. At no point were any side effects like hematoma,
seroma, an infection at the surgery site, or skin necrosis
identified. On the fifth postoperative day, during the
outpatient visit, both drains were taken out. A follow-up
visit was scheduled for every two, four, three, and six weeks.
There was no discernible constriction at the new nippleareola
location. The availability of multiple surgical
treatments for the treatment of severe gynecomastia shows
that no single option has been proven to be the most
effective. The options are mostly determined by the
surgeon's preferences, and each method has advantages and
disadvantages of its own. The majority of treatments
provide substantial difficulties when performed on male
breasts because they have a lower breast-to-skin ratio and
varied flap vascularity. The majority of the methods were
created for reduction mastopexy of the female breast.
Treatment strategies that enable more tissue excision and
NAC repositioning should be preferred for obese patients
with pseudogynecomastia. Such patients would typically
be given the option of a NAC graft or procedures utilising
an areolar pedicle flap. Among the latter, options include
the better, worse, pedicles that are central, medial,
superolateral, 8, or super medial. Although NAC grafting
is a straightforward procedure, it is risky due to the NAC's
lack of sensitivity, the potential for graft non-integrity and
the risk of necrosis and pathological scarring, and most
importantly, the requirement for dressing and careful care
of the graft for up to two weeks after surgery. Techniques
based on pedicles typically maintain the NAC's tactile
sensitivity. Peri-areolar excisions and skin resections should
be sufficient for the majority of patients with moderate to
severe gynecomastia; however, extra-areolar incisions and
scars may be required for patients with severe gynecomastia
linked to different stages of ptotic NAC. For severe gynecomastia surgeons, wise pattern reduction has become
a crucial tool, as the vertical pattern raises several aesthetic
and scar tissue issues leading to the quest for additional
aesthetic incision placements. Passot is credited with
performing the technique utilising an inferior-pedicled flap
and publishing the first report of vertical scarless mastopexy
in 1925. Only the inferior pole of the breast was treated
with a wedge procedure to remove extra fat.10 comparable
to the Passot scar, Lalonde11 described a horizontally
oriented wedge excision with a comparable button-holing
placement of the new nipple position. The method was
designed to reduce the likelihood of scar enlargement or
keloid development over the Wise pattern scar's vertical
face in inclined populations. Similar methods were
presented by Kazzazi and Malata12. Because of the ensuing
horizontal skin flaps, large redundant and Furthermore,
this restores the masculinity of the chest with the final
positioning of the scar in the submammary fold, in the
transition between the chest and the abdomen, which
makes it aesthetically acceptable in the long run. Flaccid
tissues as they can extend to the posterior axillary line or
the back, in cases where it is associated with torsoplasty. In
particular, the scarring was barely noticeable. At any of the
surgery sites, no necrosis was seen, and no contour
abnormalities were noticed at any point throughout the
follow-up. The postoperative phase saw no change in the
nipple-areola feelings beneficial in people who have
excessive superfluous skin and pseudogynecomastia after
metabolic surgery or weight loss for other causes. There are
a number of potential problems with the Passot approach.
The vertical scar that it replaces may have the same issues as
the scar on the submammary fold. In addition, although it
is uncommon, NAC necrosis, hematoma, seroma, and
wound disintegration can still be present. By preserving a
narrow base of the flap with gradual tapering towards the
NAC and removing enough fat from the superior flap so
that the pedicle can be accommodated without unwanted
bulging and additional weight, adding to a better aesthetic
value and a lower likelihood of subsequent ptosis, the risk
of flap weight-related postoperative ptosis, addressed by
Thienot, can be managed. Most men can limit the scar's
posterolateral extension so that it rarely extends past the
mid-axillary line, which improves its overall acceptability.
The Passot approach has a unique role in the surgical care
of severe gynecomastia, depending on a variety of
circumstances, but the more traditional techniques are
sufficient for the majority of patients with lower stages of
the illness. The Passot procedure, which has no vertical scar
and NAC transposition, is efficient for treating severe
gynecomastia surgically because it permits extensive tissue
resection, has a low morbidity rate, and produces good
aesthetic and functional results.
MATERIAL AND METHODS
1. Patient selection: A 32-year-old male with severe
gynecomastia was selected for the surgical intervention
using the Passot technique.
2. Preoperative assessment: A comprehensive
preoperative evaluation was conducted, including a detailed medical history, physical examination,
hormone profile analysis, and imaging studies (e.g.,
mammography, ultrasound) to rule out underlying
pathology and determine the extent of gynecomastia.
3. Surgical technique: The Passot technique, which
combines direct glandular tissue excision and
liposuction, was employed for the surgical treatment.
The procedure involved the following steps: • Anesthesia: General anesthesia or local anesthesia
with sedation was administered based on patient and
surgeon preferences.
• Incision: A periareolar incision was made around
the lower half of the areola, providing access for both
glandular tissue excision and liposuction.
• Glandular tissue excision: Direct excision of the
glandular tissue was performed through the periareolar
incision. Careful dissection and removal of the excess
glandular tissue were carried out, ensuring preservation
of the nipple-areolar complex.
• Liposuction: Following glandular tissue excision,
liposuction was performed to address any remaining
adipose tissue and contour irregularities. Tumescent
or ultrasound-assisted liposuction techniques were
utilized as per surgeon preference.
• Hemostasis and closure: Adequate hemostasis
was achieved, and the incisions were closed using
absorbable sutures. Sterile dressings were applied.
4. Postoperative care: The patient was monitored
postoperatively and provided with appropriate pain management, antibiotics, and instructions for wound
care. Follow-up appointments were scheduled to
monitor healing, address any concerns, and assess
aesthetic outcomes.
RESULTS
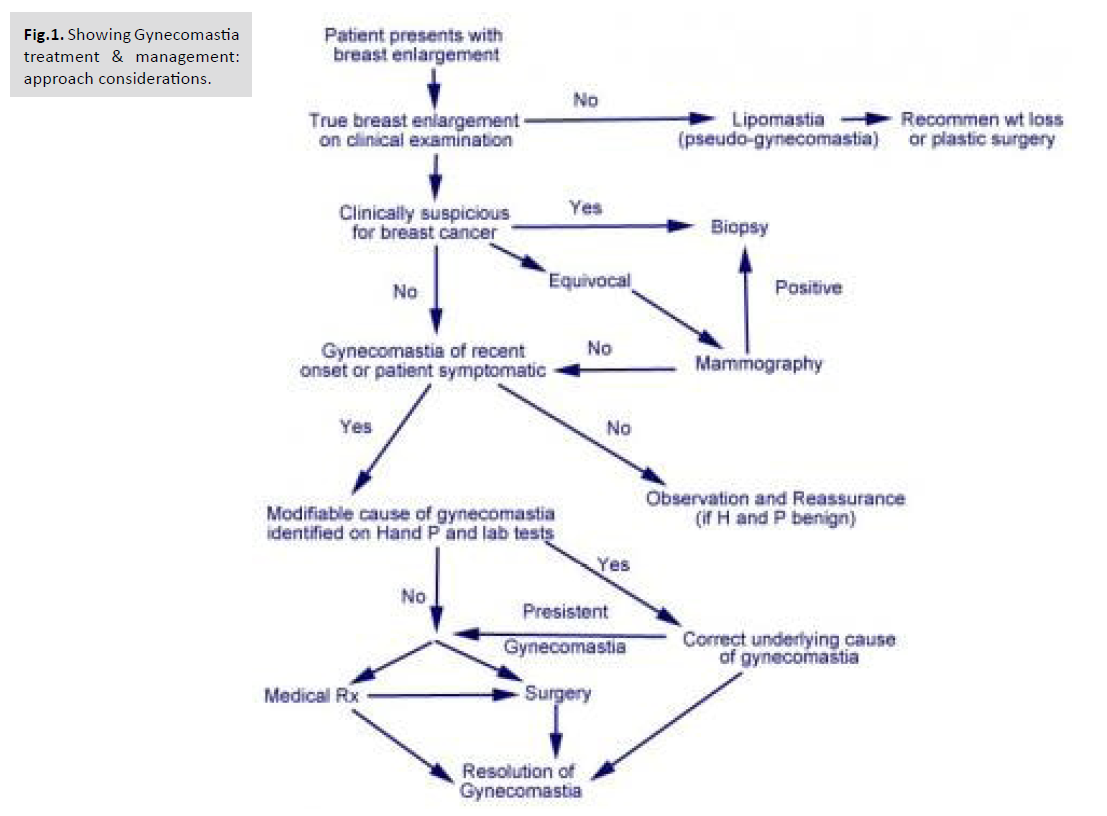
As with previous methods, the IMF and new nipple position
are marked. The new NAC is drawn as a horizontal oval ∼3
cm in diameter at the fourth intercostal space; however, the
size varies depending on the patient's overall body habitus
[Fig.1].
Fig.1. Showing Gynecomastia
treatment & management:
approach considerations.
Again, initial liposuction is performed. The incision is made
in the IMF and carried down to the level of the pectoral
fascia. The glandular tissue is then dissected off the fascia
to the level of the second intercostal space. The nipple is
removed as a full-thickness graft. The superior flap is then
pulled inferiorly to estimate and mark the excision of
excess skin and soft tissue. Although various classification
schemes have been proposed, those most often cited are
those set forth by Simon and Rohrich [Tab.1.].
The IMF incision is closed in layers over a drain. Finally,
the nipple is placed onto a de-epithelialized bed and
secured with a bolster dressing. The location of the NAC
can be estimated at the fourth intercostal space in the
midclavicular line; however, the patient should be viewed
in the upright position on the operating table to ensure
appropriate position for each patient depending on their
body habitus.
| Rohrich Classification |
| Grade I |
Minimal hypertrophy (< 250 g of breast tissue) without ptosis |
| IA |
Minimal hypertrophy—primarily glandular |
| IB |
Minimal hypertrophy—primarily fibrous |
| Grade II |
Moderate hypertrophy (250–500 g of breast tissue) without ptosis |
| IIA |
Moderate hypertrophy—primarily glandular |
| IIB |
Moderate hypertrophy—primarily fibrous |
| Grade III |
Severe hypertrophy (> 500 g of breast tissue) with grade I ptosis (glandular or fibrous) |
| Grade IV |
Severe hypertrophy with grade II or III ptosis (glandular or fibrous) |
Tab.1. Table showing classification
schemes have been proposed, those
most often cited are those set forth by
Simon and Rohrich.
DISCUSSION
Gynecomastia is a condition that can significantly impact
the physical and psychological well-being of affected
individuals. Surgical intervention is often necessary
for severe cases that do not respond to conservative
management. The Passot technique, a modified approach
to gynecomastia surgery, has gained recognition for its
effectiveness in achieving aesthetic outcomes with minimal
scarring. In this discussion, we will analyze the case report
and study review on the application of the Passot technique,
addressing its efficacy, safety, advantages, and limitations.
The case report presented a successful application of the
Passot technique in the treatment of severe gynecomastia.
The patient achieved significant improvements in breast
contour and symmetry following surgery. This case
highlights the favorable aesthetic outcomes that can be
achieved using the Passot technique. The combination of
direct glandular tissue excision and liposuction allows for
comprehensive treatment, addressing both the glandular
and fatty components of gynecomastia. The literature
review further supports the efficacy and safety of the Passot
technique. The reviewed studies consistently demonstrated
excellent aesthetic outcomes and high patient satisfaction
rates. The Passot technique proved effective in reducing
glandular tissue, contouring the chest, and minimizing the
risk of contour deformities. Furthermore, the technique
was associated with minimal scarring, which is a significant
advantage compared to traditional approaches that may
result in more visible scars. One of the notable advantages
of the Passot technique is its ability to achieve naturallooking
chest contours. By combining direct glandular
tissue excision and liposuction, the surgeon can address
both excess glandular tissue and adipose deposits, resulting
in a more aesthetically pleasing outcome. The technique
allows for individualized treatment, tailoring the procedure
to the specific needs of each patient. Additionally, the
preservation of the nipple-areolar complex helps maintain a
natural appearance. The Passot technique has demonstrated
a favorable safety profile, with low complication rates
reported in the literature. The risk of hematoma, seroma,
and infection appears to be minimal. Furthermore, the
technique has shown to be effective and safe even in severe
gynecomastia cases. However, it is important to note that
all surgical procedures carry inherent risks, and patientspecific
factors and surgical expertise also play a role in
determining outcomes.
Despite the positive findings, there are some limitations
to consider. The case report presents results from a single
patient, which restricts the generalizability of the findings.
Additionally, the literature review may be subject to
selection bias and variations in study design and reporting.
Larger-scale prospective studies with longer follow-up
periods are necessary to provide more robust evidence
on the long-term outcomes and potential complications
associated with the Passot technique. In conclusion, the
Passot technique offers a valuable surgical approach for
the treatment of severe gynecomastia, providing excellent
aesthetic outcomes and high patient satisfaction rates.
The combination of direct glandular tissue excision and
liposuction allows for comprehensive treatment and
improved chest contouring. The technique's advantages
include minimal scarring, a natural appearance, and a
favorable safety profile. However, further research is needed
to validate these findings and establish the Passot technique
as a standard surgical option for severe gynecomastia.
Surgeons should consider patient-specific factors and
weigh the benefits and risks when selecting the appropriate
surgical approach for gynecomastia treatment.
CONCLUSION
The case report and study review on applying the Passot
technique in the surgical treatment of severe gynecomastia
provide compelling evidence supporting its efficacy and
safety. The Passot technique, combining direct glandular
tissue excision and liposuction, has shown to be effective in
achieving excellent aesthetic outcomes, with high patient
satisfaction rates and minimal scarring. The technique
allows for comprehensive treatment of both glandular and
fatty components, resulting in improved chest contour and
symmetry. Despite the limitations of the case report and
the reviewed studies, the findings consistently demonstrate
the advantages of the Passot technique over traditional
approaches. It offers a natural-looking appearance,
reduced scarring, and a favorable safety profile. However,
larger-scale prospective studies with long-term followup
are needed to validate these findings and establish
the Passot technique as a standard surgical option for
severe gynecomastia. In clinical practice, surgeons should
consider patient-specific factors, such as the extent and
type of gynecomastia, as well as individual preferences,
when selecting the appropriate surgical approach. The
Passot technique should be considered as a viable option
for patients with severe gynecomastia, aiming for optimal
aesthetic outcomes and patient satisfaction. Overall, the
Passot technique represents a valuable advancement in
the surgical treatment of severe gynecomastia, providing
patients with a safe and effective solution to address their
physical and psychological concerns. Future research should focus on further validating the technique's efficacy,
assessing long-term outcomes, and comparing it with other
surgical approaches to establish evidence-based guidelines
for the management of severe gynecomastia.