Keywords
Disability; Maternity care; Pregnancy; Birth; Maternity survey
Introduction
According to Kenya’s Persons with Disabilities Act of 2003, "disability" means a physical, sensory, mental or other impairment, including any visual, hearing, learning or physical incapability, which impacts adversely on social, economic or environmental participation. Other types of disabilities are albinism and autism (Republic of Kenya, 2010). The results from the 2009 Census (KNBS, 2010), indicate that the number of people with disabilities in Kenya at the time was 647,689 (3.4%) males and 682,623 (3.5%) females. The study by [1] indicated that approximately 7% of women in Rhode Island reported a disability. Women living with disabilities reported significant disparities in their health care utilization, health behaviours and health status before and during pregnancy and during the postpartum period. Compared to able bodied women, they were significantly more likely to report stressful life events and medical complications during their most recent pregnancy, were less likely to receive prenatal care in the first trimester, and more likely to have preterm births compared to able bodied women. As for pregnancy experiences, women living with disabilities were over twice more likely to report a health complication during pregnancy compared to able bodied women. Women living with disabilities were more likely to report experiencing stressful life events and physical abuse during pregnancy, and over twice as likely to report feeling unsafe in their neighbourhood than able bodied women. Nearly 84% of able-bodied women received prenatal care in their first trimester, compared with approximately 78% of WLWD. Women living with disabilities were nearly twice as likely to begin prenatal care after their first trimester, and more likely to report inadequate prenatal care and were less likely to report having a postpartum check-up within six weeks of birth. This may be due to movement challenges, language barriers and other in accessibilities. Findings from this study also suggested that recent WLWD have lower levels of education, are less likely to be married, and more likely to be receiving public insurance and have lower household income.
This study also highlights significant disparities in their prepregnancy, pregnancy-related and postpartum health status, health behaviours, health care utilization, and in adverse birth outcomes between women with and without disabilities. They also reported higher rates of physical abuse from a current or former partner during their pregnancy and reported receiving less social support following delivery. The additional medical complications of pregnancy among women living with disabilities compounded by the high levels of financial, partner-related, traumatic, and emotional stress and the lack of perceived social support could potentially further compromise their health and the health of their babies. The delay in accessing health care could be partly because of bad experiences of women living with disabilities with their health care providers. Women with disabilities often reported that their health care providers are not able to manage their pregnancies effectively, possess negative stereotypes about their sexuality, disapprove of their pregnancy, and question their ability to parenting. These negative and humiliating experiences with health care providers could potentially prevent women with disabilities from seeking timely prenatal and postpartum care. Pre-pregnancy differences in the health of women with disabilities in this study, including a significantly an increased likelihood of unplanned pregnancy, have implications for clinicians caring for women with living with disabilities during their childbearing years. Delayed prenatal care increases the likelihood that these health problems may result in poor maternal and neonatal outcomes, including delayed recovery of women with disabilities during the postpartum period. The increased likelihood of poor infant outcomes in women living with disabilities necessitates greater attention of healthcare providers to the health of women with disabilities before and during pregnancy.
Findings by [2] indicated that although women living with disability do want to receive institutional maternal healthcare, their disability often made it difficult for such women to travel to access skilled health care, as well as gain access to unfriendly physical health infrastructure. Other related access challenges include: healthcare providers’ insensitivity and lack of knowledge about the maternity care needs of WLWD, negative attitudes of service providers, the perception from society that women with disability should be asexual and health information that lacks specificity in terms of addressing the special maternity care needs of women with disability. This study gives insight to why WLWD have poor accessibility to health care institutions and their inability to access professional care. Therefore, the purpose of this study was to assess the maternal and child health outcomes of pregnant women living with and without disability in Kakamega County, Kenya [3-12].
Theoretical Framework
Critical disability theory (CDT)
This study was guided by the critical disability theory (CDT) which was propounded by Michael Oliver [13]. This is an emerging theoretical framework for the study and analysis of disability issues. This theory evolved from the work of scholars who formed the Frankfurt School, a term which refers to a group of Western Marxist social researchers and philosophers originally working in Frankfurt, Germany [10]. Critical theory sees problems of PWDs explicitly as the product of an unequal society. It ties the solutions to social action and change. Notions of disability as social oppression mean that prejudice and discrimination disable and restrict people's lives much more than impairments do. For example, the problem with public transport is not the inability of some people to walk but that buses are not designed to take wheelchairs. Such a problem can be “cured” by spending money to ensure that public transport is designed in such a way that it becomes accessible to persons with disabilities [4]. The impact of this critical theory on healthcare and research has tended to be indirect. It has raised political awareness, helped with the collective empowerment of PWDs and publicized their critical views on healthcare. It has criticized the medical control exerted over the lives of PWDs, such as repeated and unnecessary visits to clinics for impairments that do not change and are not illnesses in need of treatment. Finally, it suggests a more appropriate societal framework for providing health services to PWDs [4]. This radically different view is called the social model of disability, or social oppression theory. While respecting the value of scientifically based medical research, this approach calls for more research based on social theories of disability if research is to improve the quality of lives of the people with disabilities. The theory views the problems of people with disabilities explicitly as products of an unequal society. The discrimination aspects in the theory helped to explain the experiences of women with physical disabilities in accessing and utilizing healthcare services. This theory finds relevance in the factors that hinder women with physical disabilities from accessing and utilizing health services from public facilities.
Materials and Methods
The study adopted quantitative methods. This was community based Prospective case control study. Data was collected using a structured interview method, observational schedule and focused group discussions. The study targeted a sample of 196 women living with disability who are confirmed pregnant. The sample size determination was based on the fisher`s method which focused on the level of precision attached to the expected results, the confidence level and the error time margin to be allowed in the results. The study used a multistage probability sampling design to identify the sub counties that would be case and control groups and purposeful and snow balling sampling technique to identify the pregnant women living with disability who in turn identified an able bodied pregnant woman that she is accessible to. Convenience sampling was used to establish age categories for respondents to the semi-structured interviews and focus group discussions. Household survey were done using structured questionnaires Ten enumerators who were all Community Health Volunteers with previous experience on similar research were recruited and trained by the researcher for two days on how to use the research instrument and the easier way to collect data from the respondents. The inclusion criteria was all pregnant women in their first and second trimester age between15-49 years and live in Kakamega County. Approval to carry out the study was obtained from Kakamega central sub county Health Management Team. Only those mothers, who met the study requirements, verbally consented and voluntarily signed the consent forms were enrolled into the study. Participants who could not write indicated their consent by a fingerprint. All mothers were assured for confidentiality [14,15].
Statistical analyses
Schlomer et al [16] outlined guidelines for best practices regarding the handling and reporting of missing data within research. Visual inspection of the data illustrated that missing data appeared to be missing at random. After visual inspection, in order to further examine the pattern of missing data. Data collected using the questionnaire was checked for consistency and accuracy of the responses, coded and analyzed using the version 23 of the SPSS statistical programme. Socio-demographic characteristics of both disabled and non-disabled women of reproductive age in Kakamega Central Sub county, Kenya was analyzed through descriptive characteristic in which central tendencies and Chisquare tests of significance, extent of data dispassion and variability were calculated and presented on bar graphs and pie charts. Women who did not complete the questions in the survey relating to disability were excluded. For all comparisons between a specific disability group and non-disabled women the statistical significance level was set at p = <0.01 Cross tabulations were undertaken to establish linkages between different variables.
Results
This chapter is the summary of the findings of the study based on the objective of the study. A total of 117comprising of 93 pregnant women living with disability and 24 able bodied pregnant women who reside within the twelve sub counties of Kakamega County, Kenya. Maternal factors that were observed during pregnancy included; virginal bleeding, fits, severe abdominal pains, paleness, Severe headache, foul smell, any abnormal virginal discharges, pain while passing urine, reduced or no kicking by the baby, Blurred vision fast or difficulty in breathing, Unusual swelling or face and legs, Sleeping under LLMTN and nutritional status. Additional maternal outcomes observed at birth included hand washing technique, breast feeding technique, any other illness, advise on family planning, number of ANC visits, any treatment given during pregnancy, method of delivery, place of delivery and PNC visit. Child outcomes includes weight of the baby at birth, condition of the baby at birth(alive/dead), health status of the baby at birth, Fever, Fast or difficulty in breathing, Unable to breastfeed, Chest in drawing, unconsciousness, unusually sleepy or drowsy, lack of energy or weakness, feeling very cold, redness of the umbilical cord, pus from the umbilical cord, stiffness of the neck, yellow soles, any congenital abnormalities detected, any other signs of sickness/Local infection, Immunization of BCG and Polio. It also tested the difference of the outcome between the women living with disability and able-bodied women.
Before birth maternal outcomes
Before birth maternal outcomes were analyzed based on the period of observation. The results were presented in three periods; 12 weeks, 13-28 weeks into pregnancy and 29-onset of labor.
Maternal outcomes observations for 12weeks into pregnancy
The study found that majority of the able-bodied (91.2%, n=31) and the disabled women (95.1%, n=98) did not have any vaginal bleeding, did not have severe abdominal pains (76.5%, n=26 and 84.5%, n=87), did not have paleness (94.1%, n=32 and 91.3%, n=94), neither severe headache or foul smell (88.2%, n=30 and 83.5%, n=94). The findings also revealed that 85.3% (n=29) of the able-bodied women did not report abnormal vaginal discharges or pain while passing urine (91.2%, n=32). A few in the able-bodied (17.6%, n=6) and disabled women (8.7%, n=9) reported blurred vision and difficulty in breathing. 85.3% of the able-bodied women and 89.3% of women with a disability did not experience unusual swelling of face and legs. Only 38.2% of the able-bodied women and 21.4% of the disabled women had a written birth plan. This indicates that birth plan is still a major problem for pregnant women and more emphasis should be put in health education on birth plan. In addition, 88.2% (n=30) of the able-bodied women and 71.8% (n=74) of the disabled women did not have any other illness.
Maternal outcomes observations for 13-28 weeks into pregnancy
Results from maternal outcome observations for 13-28 weeks showed that that majority of the able-bodied (91.2%, n=31) and the disabled women (95.1%, n=98) did not have any vaginal bleeding, did not have severe abdominal pains (79.4%, n=27 and 79.6%, n=82), did not have paleness (94.1%, n=32 and 88.3%, n=91), neither severe headache(88.2%,n=30 and 84.5%,n=87) or foul smell (88.2%, n=30 and 92.2%, n=95). The findings also revealed that 85.3% (n=29) of the able-bodied women and 81.6% (n=84) disabled women did not report abnormal vaginal discharges or pain while passing urine (91.2%, n=32 and 97.1%, n=100). A few in the able-bodied (14.7%, n=5) and disabled women (9.7%, n=10) reported blurred vision and difficulty in breathing. 85.3% (n=29) of the able-bodied women and 87.4% (n=90) of women with a disability did not experience unusual swelling of face and legs. Only 38.2% (n=13) of the able-bodied women and 22.3% (n=23) of the disabled women had a written birth plan. In addition, 88.2% (n=30) of the able-bodied women and 70.9% (n=73) of the disabled women did not have any other illness. It is also of importance to note that by 13-28 weeks into the pregnancy only one disabled woman lost her pregnancy (1%, n=1).
Maternal outcomes observations for 29 weeksonsets of labor weeks into pregnancy
Results from maternal outcome observations for 29 weeks to onset of labor showed that that majority of the able-bodied (91.2%, n=31) and the disabled women (93.2%, n=96) did not have any vaginal bleeding, did not have severe abdominal pains (76.5%, n=26 and 82.5%, n=85), did not have paleness (94.1%, n=32 and 85.4%, n=88), neither severe headache (88.2%, n=30 and 82.5%, n=85) or foul smell (88.2%, n=30 and 90.3%, n=93). The findings also revealed that 85.3% (n=29) of the able-bodied women and 80.6% (n=83) of the disabled women did not report abnormal vaginal discharges or pain while passing urine (91.2%, n=31 and 94.2%, n=97). A few in the able-bodied (14.7%, n=5) and disabled women (11.7%, n=12) reported blurred vision and difficulty in breathing. 88.2% (n=30) of the able-bodied women and 85.4% (n=88) of women with a disability did not experience unusual swelling of face and legs. Only 38.2% (n=13) of the ablebodied women and 22.3% (n=23) of the disabled women had a written birth plan. In addition, 88.2% (n=30) of the able-bodied women and 70.9% (n=73) of the disabled women did not have any other illness. It is also of importance to note that by 29-38th weeks into the pregnancy only two disabled women lost their pregnancy (1.9%, n=2).
After birth maternal and child outcomes
Maternal outcomes observations for Mother at Birth: Results from maternal outcome observations after birth showed that that majority of the able-bodied (97.1%, n=33) and the disabled women (86.4%, n=89) did not have any vaginal bleeding, did not have severe abdominal pains (94.1%, n=32 and 77.7%, n=80), did not have paleness (100%, n=34 and 90.3%, n=93), neither severe headache(94.1%,n=32 and 84.5%,n=87) or foul smell (100%, n=34 and 92.2%, n=95). The findings also revealed that 100 %(n=34) of the able-bodied women and 88.3%(n=91) of the disabled women did not report abnormal vaginal discharges or pain while passing urine (91.2%, n=31 and 90.3%, n=93). A few in the able-bodied (5.9%, n=2) and disabled women (6.8%, n=7) reported blurred vision and difficulty in breathing. 97.1% (n=33) of the ablebodied women and 88.3% (n=91) of women with a disability did not experience unusual swelling of face and legs. 64.7% (n=22) of the able-bodied women and 59.2% (n=61) of the disabled women attended ANC clinic 4 or more times. In addition, 73.5% (n=25) of the able-bodied women and 46.6% (n=48) of the disabled women received advice on family planning. With regards to method of delivery 91.2% (n=31) of able-bodied women and 97.1% (n=100) of disabled women delivered through SVD and majority delivered at the hospital (97.1%, n=33 and 94.2%, n=97).
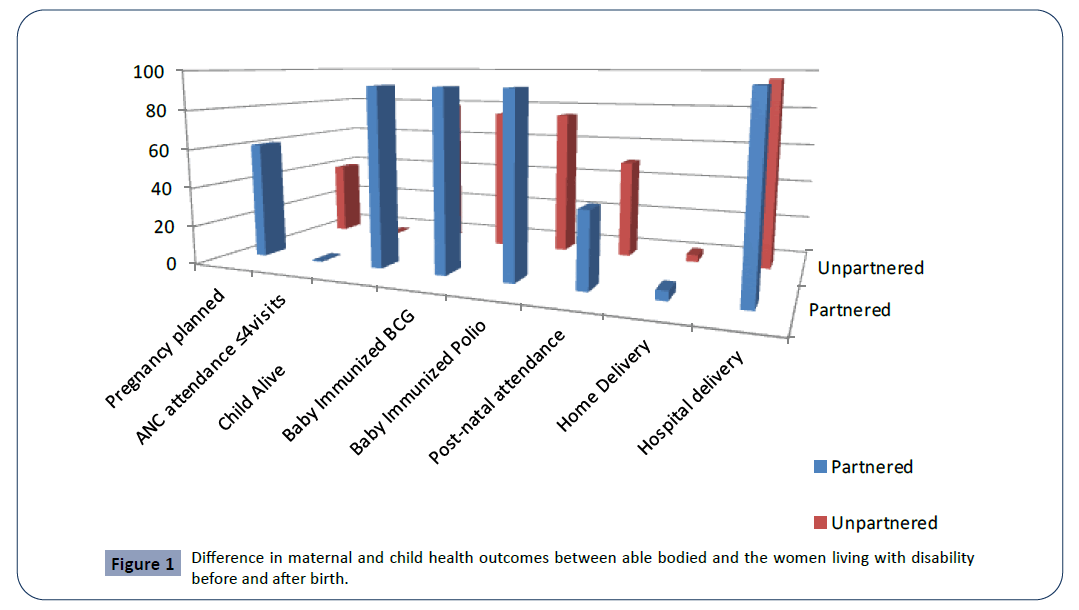
Child outcome observations at birth: Results from child outcome observations showed that that majority of the able-bodied children (100%, n=34) and the disabled women’s children (83.5%, n=86) were alive, Were of good health (97.1%, n=33 and 83.3%, n=85), did not have baby fever (100%, n=34 and 86.4%, n=89), neither did they have fast or difficult breathing (97.1%,n=33 and 85.4%,n=88), majority were able to breastfeed (97.1%, n=33 and 84.5%, n=87). The findings also revealed that 100% (n=34) of the able-bodied women’s children and 86.4% (n=89) of the disabled women’s children did not have chest in drawing nor experience unusual sleep (100%, n=31 and 84.5%, n=87). A few in the able-bodied women’s children (8.8%, n=3) and disabled women’s children (3.9%, n=4) experienced yellow sole. 91.2% (n=31) of the able-bodied women’s children and 81.6% (n=84) of the children women living with disability did not experience congenital abnormalities. Table 1 above shows a summary of the findings (Figure 1).
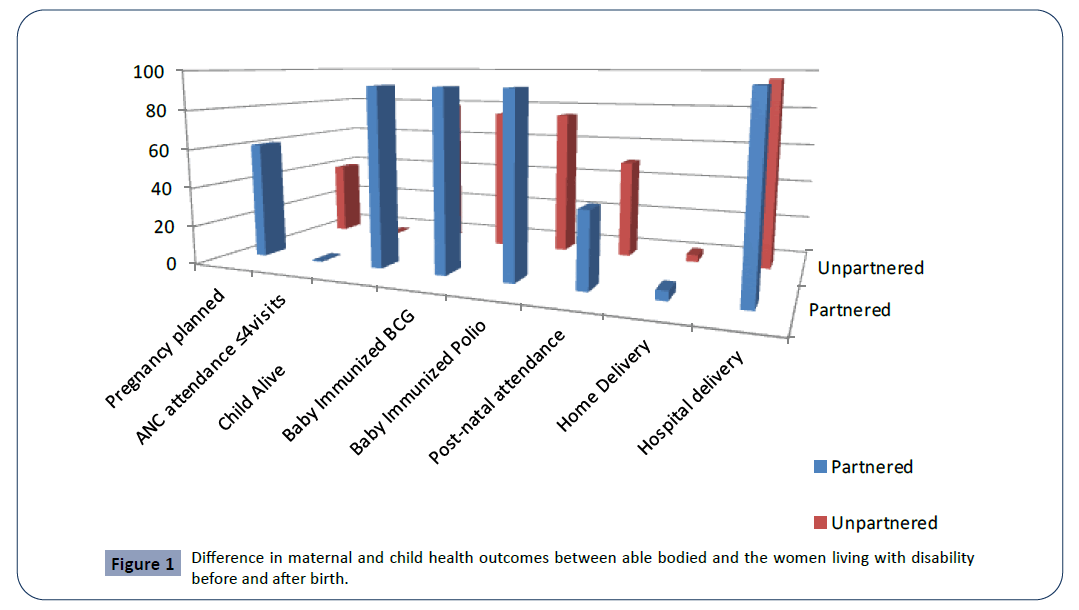
Figure 1: Difference in maternal and child health outcomes between able bodied and the women living with disability before and after birth./p>
Table 1. Difference in maternal and child health outcomes between able bodied and the women living with disability before and after birth.
| |
Able bodied women (%) |
WLWD (%) |
| Pregnancy planned |
58.8 |
32 |
| Not Pregnancy planned |
41.2 |
68 |
| ANC attendance ≤4visits |
64.70% |
59.20% |
| Child Alive |
100 |
85.4 |
| Child Lost pregnancy |
0 |
1.9 |
| Child Died at birth |
0 |
11.2 |
| Child Died postnatally |
0 |
2.9 |
| Baby congenital abnormalities |
0 |
7.8 |
| Baby Immunized |
100 |
97 |
| Baby Not Immunized |
3 |
3 |
| Post-natal attendance |
73.7 |
54.9 |
| Home Delivery |
2.9 |
4.9 |
| Hospital delivery |
97.1 |
95.1 |
Maternal outcomes observations for mother 4-6 weeks after birth: Results from maternal outcome observations 4-6 weeks after birth showed that that majority of the able-bodied (97.1%, n=33) and the disabled women (88.3%, n=91) did not have any vaginal bleeding, did not have severe abdominal pains (94.1%, n=32 and 80.6%, n=83), did not have paleness (100%, n=34 and 88.3%, n=91), neither severe headache(94.1%,n=32 and 86.4%,n=89) or foul smell (100%, n=34 and 92.2%, n=95). The findings also revealed that 97.1% (n=33) of the able-bodied women and 88.3% (n=91) of the WLWD did not report abnormal vaginal discharges or pain while passing urine (97.1%, n=33 and 92.2%, n=95). A few in the able-bodied (2.9%, n=1) and WLWD (2.9%, n=3) reported blurred vision and difficulty in breathing. 100% (n=33) of the able-bodied women and 89.3% (n=92) of WLWD did not experience unusual swelling of face and legs. 64.7% (n=22) of the able-bodied women and 61.8% (n=61) of the WLWD attended ANC clinic 4 or more times. In addition, 73.5% (n=25) of the able-bodied women and 45.6% (n=47) of the WLWD received advice on family planning. With regards to breastfeeding technique 85.3% (n=29) of able-bodied women and 68% (n=70) of WLWD used the proper technique. Table 1 below shows a summary of the findings.
Child observations for 4-6 weeks after birth: Results from child outcome observations after 4-6 weeks showed that that majority of the able-bodied children (100%, n=34) and the WLWD’s children (89.2%, n=91) had a weight of 2.5 and above, Were of good health (100%, n=34 and 85.3%, n=87), did not have baby fever (100%, n=34 and 83.3%, n=85), neither did they have fast or difficult breathing (100%,n=34 and 82.4%,n=84), majority were able to breastfeed (100%, n=34 and 83.3%, n=85). The findings also revealed that 100% (n=34) of the able-bodied women’s children and 86.4% (n=89) of the WLWD’s children did not have chest in drawing nor experience unusual sleep (100%, n=34 and 84.3%, n=86). Most of the able-bodied women’s children (100%, n=34) and WLWD’s children (84.3%, n=86) did not pus from umbilical cord. 100% (n=34) of the able-bodied women’s children and 77.5% (n=79) of the children WLWD did not experience congenital abnormalities. Table 1 above shows a summary of the findings.
Tests of within-between groups Differences in Maternal outcomes before Birth with disability status as a between groups factor: The test of differences in maternal outcomes before birth was done using repeated measure ANOVA with withinbetween subject effects. The between subjects’ factor was able bodied and WLWD. The overall scores for schedule one to three were converted to z-scores before the repeated measures were done. The Mauchly’s test of sphericity indicated (0.783, p<0.01) that the differences of the variances of all possible pairs within groups in the maternal outcomes were not equal hence the researcher used Greenhouse-Geisser for epsilon correction. The Levene test of homogeneity was done and the results showed homoscedasticity of variances based on means (Observation schedule one f (1,135) =0.069, p=.793, Observation schedule two f (1,135) =00.135, p=783, observation schedule three f (1,135) =0.030, p=862). Repeated measure ANOVA results are presented in Table 2 below. As Table 2 indicates, a repeated measures ANOVA of maternal outcome scores (Time(observation schedules over time) × Able bodied group/Disabled group) indicated a non-significant main effect for maternal outcomes change over time(Greenhouse-Geisser 1.634, 270 =.119,p=863, ?2=0.001), a non-significant main effect for disability status groups (f (1,135) =.256, p=.614,?2=0.002) and a non-significant Time × Group interaction effect (Greenhouse-Geisser 1.643, 270=.470, p=.622,?2=0.003) .The Bonferroni post hoc test for within subject effect was not done because there were no significant within subjects effects. This means there was no significant differences in maternal outcomes amongst schedules one, two and three. Moreover, there were no significant differences between the able bodied and disabled women in a linear combination of all the maternal outcomes in the three time periods.
Tests of within-between groups differences in maternal outcomes before birth with disability status as a between groups factor: The test of differences in maternal outcomes before birth was done using repeated measure ANOVA with within-between subject effects. The between subjects’ factor was able-bodied and disabled women. The overall scores for schedule one to three were converted to z-scores before the repeated measures were done. The Mauchly’s test of sphericity indicated (0.783, p<0.01) that the differences of the variances of all possible pairs within groups in the maternal outcomes were not equal hence the researcher used Greenhouse-Geisser for epsilon correction. The Levene test of homogeneity was done and the results showed homoscedasticity of variances based on means (Observation schedule one f (1,135) =0.069, p=.793, Observation schedule two f (1,135) =00.135, p=783, observation schedule three f (1,135) =0.030, p=862). Repeated measure ANOVA results are presented in Table 2 below. As Table 2 indicates, a repeated measures ANOVA of maternal outcome scores (Time observation schedules over time) × Able-bodied group/Disabled group) indicated a non-significant main effect for maternal outcomes change over time(Greenhouse-Geisser1.634, 270 =.119,p=863, ?2=0.001), a non-significant main effect for disability status groups (f (1,135) =.256, p=.614,?2=0.002) and a non-significant Time × Group interaction effect (Greenhouse-Geisser 1.643, 270 =.470, p=.622,?2=0.003) .The Bonferroni post hoc test within-subject effect was not done because there were no significant withinsubjects effects. This means there were no significant differences in maternal outcomes amongst schedules one, two and three. Moreover, there were no significant differences between the able-bodied and disabled women in a linear combination of all the maternal outcomes in the three time periods.
Table 2. Tests of Within-Subjects/between subject Effects.
| Source |
Type III Sum of Squares |
Df |
Mean Square |
F |
Sig. |
Partial Eta Squared |
| Time |
Greenhouse-Geisser |
.119 |
1.643 |
.073 |
.105 |
.863 |
.001 |
| Disability Status |
|
.480 |
1 |
.480 |
.256 |
.614 |
.002 |
| Disability Status * Time |
Greenhouse- Geisser |
.470 |
1.643 |
.286 |
.412 |
.622 |
.003 |
Tests of within-between groups Differences in Maternal outcomes after Birth with Disability status as a between groups factor: The test of differences in maternal outcomes after birth was done using repeated measures ANOVA with within-between subject effects. The between subjects’ factor was disability status of women. The overall scores for schedule four and five were converted to z-scores before the repeated measures were done. The Mauchly’s test of sphericity was not computed because of presence of only two within subjects’ factors. The Levene test of homogeneity was done and the results showed homoscedasticity of variances based on means (Observation schedule four f (1,134) =2.406, p=.123, Observation schedule five f (1,134) =1.943, p=.166. As Table 3 indicates, a repeated measures ANOVA of maternal outcome scores (Time (observation schedules over time) × able bodied women group / disabled women group) indicated a significant main effect for maternal outcomes change over time (Greenhouse-Geisser 1, 133 =.117, p=0.03, ?2=0.246), a significant main effect for disability status (f (1,134) =.111, p=.001,?2=0.176) and a significant Time × Group interaction effect (Greenhouse-Geisser 1, 133 =1.527, p=.02, ?2=0.17). This shows there were significant differences between the able bodied and WLWD in a linear combination of maternal outcome observations from birth up to six weeks after delivery. Table 3 gives a summary of the descriptive statistics.
Table 3. Tests of Within-Subjects/between subject Effects.
| Source |
Type III Sum of Squares |
Df |
Mean Square |
F |
Sig. |
Partial Eta Squared |
| Time |
Greenhouse-Geisser |
.115 |
1 |
.068 |
.117 |
.03 |
.246 |
| Status |
|
.480 |
1 |
.480 |
.111 |
.001 |
.176 |
| Time * Status |
Greenhouse-Geisser |
.470 |
1 |
.286 |
1.527 |
.02 |
.017 |
Tests of within-between groups differences in child outcomes with disability status as a between groups factor: The test of differences in child outcomes after birth was done using repeated measures ANOVA with within-between subject effects. The between subjects’ factor was disability status of women. The overall scores for schedule four and five were converted to z-scores before the repeated measures were done. This was done to cater for inconsistencies as a result of additional measures used in the different observations. The Mauchly’s test of sphericity was not computed because of presence of only two within subjects’ factors. The Levene test of homogeneity was done and the results showed homoscedasticity of variances based on means (Observation schedule four f (1,133) =19.03, p=.034, Observation schedule five f (1,133) =11.45, p=.266. As Table 4 indicates, a repeated measures ANOVA of child outcome scores (Time (observation schedules over time) × able bodied women group/disabled women group) indicated a significant main effect for child outcomes change over time (Greenhouse- Geisser 1, 133 =188.06, p<0.01, ?2=0.046), a significant main effect for disability status (f (1,133) =7.183, p=.008,?2=0.076) and a non-significant Time × Group interaction effect (Greenhouse- Geisser 1,133 =1.714, p=.193, ?2=0.017). These shows there were significant differences between the able bodied and disabled women in a linear combination of child outcome observations from birth up to six weeks after birth. Table 4 gives a summary of the descriptive statistics.
Table 4. Descriptive Statistics of maternal outcomes.
| |
Status |
Mean |
Std. Deviation |
N |
| Observation 4 |
able bodied |
11.90 |
2.700 |
34 |
| Disabled |
11.44 |
7.678 |
102 |
| Total |
11.67 |
6.775 |
136 |
| Observation 5 |
able bodied |
11.96 |
2.699 |
34 |
| Disabled |
11.13 |
7.274 |
102 |
| Total |
11.55 |
6.433 |
136 |
Discussion
The objective of this study was to assess the maternal and child health outcomes of pregnant women living with and without disability in Kakamega County, Kenya. Women living with disability carry a more complex burden of health conditions than do the able-bodied pregnant women. Maternal factors that were observed during pregnancy included; vaginal bleeding, fits, severe abdominal pains, paleness, Severe headache, foul smell, any abnormal vaginal discharges, pain while passing urine, reduced or no kicking by the baby, Blurred vision fast or difficulty in breathing, Unusual swelling or face and legs, Sleeping under LLMTN and nutritional status.
Additional maternal outcomes observed at birth included hand washing technique, breast feeding technique, any other illness, advise on family planning, number of antenatal (ANC) visits, any treatment given during pregnancy, method of delivery, place of delivery and PNC visit. Child outcomes includes weight of the baby at birth, condition of the baby at birth(alive/dead), health status of the baby at birth, Fever, Fast or difficulty in breathing, Unable to breastfeed, Chest in drawing, unconsciousness, unusually sleepy or drowsy, lack of energy or weakness, feeling very cold, redness of the umbilical cord, pus from the umbilical cord, stiffness of the neck, yellow soles, any congenital abnormalities detected, any other signs of sickness/Local infection, Immunization of BCG and Polio.
It was observed that the pregnancy outcomes and complications among women living with disability were significantly higher compared to majority of the able bodied. This is because the disability status predisposes them to high health risks during pregnancy period. This finding was similar to [9] who found out that regardless of pregnancy, women with chronic physical disabilities (CPD) are significantly more likely to report fair or poor general health than are other women: 35.0% versus 4.6%.
Findings from maternal outcome observations for 13-28 weeks in table 5 showed that majority of the able-bodied and the women living with disability did not have maternal complications during pregnancy though more of the women living with disability had some complications compared to the able bodied ones. However, a few in the able-bodied and disabled women reported blurred vision and difficulty in breathing. Only 38.2% of the able-bodied women and 22.3% of the disabled women had a written birth plan. The government needs to put more emphasis on birth plan for all pregnant women. Health education on importance of a birth plan is very important for preparation and improvement of maternal and child outcomes. It is also of importance to note that by 13-28 weeks into the pregnancy only one woman living with disability lost her pregnancy. This was similar to a study by [9] where interview with 22 women living with mobility disabilities who had delivered babies within the prior 10 years identified complications during pregnancy that appeared to be related to their underlying disability. They often experience certain similar problems during pregnancy: shortness of breath, urinary tract difficulties (urinary frequency, Urinary tractinfections (UTIs)), and bowel management problems. However this was not the case with experiences of able bodied pregnant women.
Table 5. Tests of Within-Subjects/between subject Effects.
| Source |
Type III Sum of Squares |
df |
Mean Square |
F |
Sig. |
Partial Eta Squared |
| Time |
Greenhouse-Geisser |
1536.25 |
1 |
1536.25 |
188.1 |
.000 |
.046 |
| Status |
|
1045.25 |
1 |
1045.25 |
7.183 |
.008 |
.076 |
| Time * Status |
Greenhouse-Geisser |
14.001 |
1 |
14.001 |
1.714 |
.193 |
.017 |
Maternal observations as the women approached delivery were consistent for both women living with disability able bodied women. Findings from maternal outcome observations for 29- 38 weeks showed that that majority of the able-bodied and the disabled women did not have complications. It was also of importance to note that by 29 weeks to onset of labor, two women living with disability women lost their pregnancy yet none among the able bodied women. This was similar to [1] with respect to pregnancy characteristics and experiences, women living with disabilities were over twice as more likely to report a medical complication during pregnancy compared able bodied women. Specific health problems more common among women living with disabilities included vaginal bleeding, kidney/bladder infections, nausea, injury due to a car crash, preterm labor, and premature rupture of membranes.
This study found out that there were no significant differences in maternal outcomes amongst schedules one, two and three. Moreover, there were no significant differences between the able bodied and women living with disability in a linear combination of all the maternal outcomes in the three time periods. In Kenya ANC services is well utilized and therefore pregnancy complications are dealt with early. Also, antenatal services are free therefore affordable for all women. The few women living with disability who experienced some complications were likely be due to accessibility issues. Was unlike the findings by [1] in which women living with disabilities compared to their ablebodied peers were more likely to report medical complications and stressful life events during pregnancy. In addition, women living with disabilities were at greater risk of stressful life events during their pregnancy. This was similar to a study by [9] where interview with 22 women living with mobility disabilities who had delivered babies within the prior 10 years identified complications during pregnancy that appeared to be related to their underlying disability. They often experience certain similar problems during pregnancy: shortness of breath, urinary tract difficulties (urinary frequency, UTIs), and bowel management problems. However, this was not the case with experiences of able bodied pregnant women. ANC services have greatly improved Maternal and child indicators in Kenya and once the health facilities make provisions for the women living with disabilities, the indicators with further improve.
Majority of women delivered at the hospital and by SVD deliveries at while only 2.9% had CS deliveries with positive maternal and child outcomes. This means Hospital delivery is well utilized in Kakamega County because of Oparanya care model, free delivery creed by the president, availability of maternity wards up to the level of dispensaries and health centres, beyond zero campaigns by the first lady, availability of ambulance services by Kakamega County in conjunction with red cross, improved roads in the county and increase of health facility Results from maternal outcome observations after birth showed that majority of the able-bodied and the women living with disability maternal complications. Both the able-bodied women and the women living with disability attended ANC clinic 4 or more times however findings of this study suggests that more able bodied women than women living with disability attended ANC four times and over. This is due to accessibility issues and high poverty amongst the women living with disability unlike the able bodied women. This is consistent with a study in USA by [12] which found out that across all women, regardless of pregnancy, women living with disability are significantly more likely to report fair or poor general health than are able bodied women: 35.0% versus 4.6%. In agreement, astudy by [1] revealed that women living with disabilities reported significant differences in their health care utilization, health behaviors and health status before pregnancy, during pregnancy and during the postpartum period. Compared to the able bodied women, they were significantly more likely to report stressful life events and health complications during their most recent pregnancy, were less likely to receive antenatal care in the first trimester, and more likely to have preterm births compared to the able bodied women and low birth weight babies in comparison to the able bodied. In agreement also, is a study by [3] which showed that all women living with experience a lot of challenges of giving birth to a child or children.
Child health outcomes are normally highly related to maternal factors; her health during pregnancy, place and method of delivery. Results from child health outcomes observations showed that majority of babies of the able-bodied women and the babies of women living with disability were alive, though all the children who died were from the women living with disability while none of the able-bodied women lost a child. The children were of good health with very few having health issues. The findings also revealed that of the able-bodied women’s children and of the children of WLWD did not experience congenital abnormalities. As noted in this study WLWD are highly likely to give birth to children with congenital abnormalities unlike the able bodied women because some disabilities are genetically acquired [15]. This findings were unlike [1] which found out that over 10% of women living with disabilities had a low birth weight infant and over 13% preterm birth, compared with 7% and 9%, respectively, among women living without disabilities. Women living with disabilities were more likely to have a long hospital stay, an infant in nursery and to have had an infant who died than their able bodied peers but it was similar to studies which have found that Increased risks of instrumental delivery and adverse pregnancy outcomes have been reported in women with physical disabilities and longstanding conditions [17]. Health challenges faced by women living with disabilities impact greatly to negative child outcomes.
Findings from maternal outcome observations up to six weeks after birth indicated that majority of the able-bodied and the disabled women did not have major complications. This can be due to the fact that most of them delivered in the hospital where they received good care. However postnatal care visit was poorly attended. There is need to educate and reemphasis on importance of postnatal care visit. PNC reduces maternal neonatal complications and the mother receives more advice on how to care for herself and the baby. This study is alike [1] whereby women living with disabilities were more likely to delay prenatal care until after the first trimester, report inadequate prenatal care, and were less likely to report having a postpartum check-up within six weeks of birth. The delay in accessing health care could be partly attributed to the negative experiences of women living with disabilities with their health care providers. In addition, the able-bodied women and of the WLWD received advice on family planning. With regards to breastfeeding technique both able-bodied women of WLWD used the proper breast-feeding technique. Table 6 shows a summary of the findings. This was unlike [1] where by 84% of able-bodied women received prenatal care in their first trimester, compared with approximately 78% of women with disabilities.
Table 6. Descriptive Statistics for child outcomes.
| |
Status |
Mean |
Std. Deviation |
N |
| Observation 4 |
able bodied |
1.82 |
1.167 |
34 |
| disabled |
5.83 |
9.960 |
101 |
| Total |
4.82 |
8.799 |
135 |
| Observation 5 |
able bodied |
6.79 |
.946 |
34 |
| disabled |
11.85 |
10.220 |
101 |
| Total |
10.58 |
9.112 |
135 |
In this study, 17 babies died; 2 were lost pregnancies, 12 died at birth and 3 died during postnatal period. All of them were from women living with disability. However results from child outcome observations after 4-6 weeks showed that all the able-bodied children and majority of the women living with disability’s children had a weight of 2.5kg and above and were of good health. Proper ANC and hospital delivery definitely lead to positive child outcomes. Though unlike all the children of able bodied women were healthy, few children from women living with disability experienced health problems this was similar to a study by [14] where an estimated 20.6 million deliveries identified between 2007-2011 data 10,275 occurred in women with Intellectual and Development Disability(IDD). In adjusted regression analyses, women with IDD compared to those without IDD were significantly more likely to have preterm birth, low birth weight and stillbirth.
The test of differences in maternal outcomes after birth was done using repeated measures ANOVA with within-between subject effects. There were significant differences between the able bodied and disabled women in a linear combination of maternal health outcome observations after birth and four to six weeks after birth. Disability status on its own is a health risk factor. It interferes with health facility accessibility and usability. Health facility needs to cater for the unique needs of women living with disability otherwise will continue having negative indicators among women living with disability unlike the able-bodied women and will generally lead to negative maternal indicators. This was alike study by [18] found out difference in pregnancy complications of matched women with and without a diagnosis of Multiple Sclerosis who had a live birth. There was a statistically significantly higher proportion of women with a live birth with MS who had a claim for premature labor (p = 0.005), infection in pregnancy (p=0.016), maternal cardiovascular disease (p=0.028), anaemia or acquired coagulation disorder (p=0.007), neurologic complications in pregnancy (p=0.005), and sexually transmitted diseases in pregnancy (p=0.045) compared with women with a live birth without MS. Women with a live birth without MS had a higher rate of post term pregnancy (p<0.001) compared with women with a live birth with MS.
The test of differences in child outcomes after birth was done using repeated measures ANOVA with within-between subject effects. These shows there were significant differences between the able bodied and disabled women in a linear combination of child outcome observations after birth up to six weeks after birth. This can be attributed to women living with disability having delayed to start their ANC visits and some having maternal complications during pregnancy. High illiteracy level among them which makes it hard to follow instructions on how to take care of their babies, lack of spouse to assist and also lack of a source of income may have contributed to these differences. [1] found out that compared to the able bodied women, WLWD were more likely to have preterm births and low birth weight babies compared to those of able bodied women. This was similar to the study by [18,19]. where a higher proportion of women with multiple sclerosis(MS) than those without had claims for premature labor (31.4% vs. 27.4%; p=0.005), infection (13.3% vs. 10.9%; p=0.016), cardiovascular disease (3.0% vs. 1.9%; p=0.028), anemia/acquired coagulation disorders (2.5% vs. 1.3%; p=0.007), neurologic complications (1.6% vs. 0.6%; p=0.005), sexually transmitted diseases (0.4% vs. 0.1%; p=0.045), acquired fetal damage (27.8% vs. 23.5%; p=0.002), and congenital fetal malformations (13.2% vs. 10.3%; p=0.004).
This was also similar to the findings of the study by [3] show that all women living with disability who have had the experience of giving birth to a child or children faced immense challenges in childbearing. The example in the study, Rudo lives on her own in an urban area, and in some instances, she stays in her rural home, she is deaf, partially blind, divorced, childless, 50 years old and formally unemployed. She claimed that all her babies died because the doctors and nurses could not use sign language.
Conclusion and Recommendation
The study found out that maternal healthcare services lacked the flexibility and responsiveness to meet the unique maternity care needs of WLWD. Women living with disabilities had poor maternal and child health outcomes. The findings will contribute to maternity services more satisfactorily pinpointing the required actions in caring for pregnant women with different types of disability and in training staff to support women with a wide range of conditions. The findings from this study may enable maternity service providers to more satisfactorily pinpoint the required actions in caring for pregnant women with disability. Further research should target the experience, use of services and needs of women with different and multiple disabilities from diverse groups, using qualitative as well as quantitative methodologies.
29795
References
- Canti V, Castiglioni MT, Rosa S, Franchini S, Sabbadini MG, et al. (2012) Pregnancy outcomes in patients with systemic autoimmunity. Autoimmunity 45: 169–175.
- Chen YH, Lin HL, Lin HC (2009) Does multiple sclerosis increase risk of adverse pregnancy outcomes? A population-based study. Mult Scler 15: 606–612.
- Christiana RT, Hunter CL, Dibley MJ, Heywood P (2010) Why do some women still prefer traditional birth attendants and home delivery? A qualitative study on delivery care services in West Java Province, Indonesia. BMC Pregnancy and Childbirth 10.
- Pothier D, Devlin R (2005) Critical Disability Theory: Essays in Philosophy, Politics, Policy, and Law. UBC Press, Vancouver.
- Franklin PA (1977) Impact of Disability on the Family Structure. Social Security Bulletin 40: 3-18.
- Gabrysch S, Campbell OM (2009) Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy and Childbirth 9: 34.
- Gavin NI, Benedict MB, Adams EK (2006) Health service use and outcomes among disabled Medicaid pregnant women. Womens Health Issues 16: 313–322.
- Grue L, Laerum KT (2002) Doing motherhood: some experiences of mothers with physical disabilities. Disabil Soc 17: 671–683.
- Murthy GVS, John N, Sagar J (2014) Reproductive health of women with and without disabilities in South India, the SIDE study (South India Disability Evidence) study: a case control study. BMC Womens Health 14: 146.
- Hosking DL (2008) Critical disability theory. A paper presented at the 4th Biennial Disability Studies Conference at Lancaster University, UK.
- Ganle JK, Otupiri E, Obeng B, Edusie AK, Ankomah A, et al. (2016) Challenges Women with Disability Face in Accessing and Using Maternal Healthcare Services in Ghana: A Qualitative Study. PLoS One 11: e0158361.
- Shadow Report (2004) On the implementation of CEDAW and women’s human rights in Bosnia and Herzegovina.
- Oliver M (1996) Understanding disability: From theory to practice. The Journal of Sociology & Social Welfare 23: 24.
- Olsen BE, Hinderaker SG, Bergsjø P, Lie RT, Olsen O, et al. (2002) Causes and characteristics of maternal deaths in rural northern Tanzania. Acta Obstetrician et Gynecologica Scandinavica 81: 1101-1109.
- Schlomer GL, Bauman S, Card NA (2010) Best practices for missing data management in counseling psychology. J Couns Psychol 57: 1-10.
- Signore C, Spong CY, Krotoski D, Shinowara NL, Blackwell SC (2011) Pregnancy in women with physical disabilities. Obstet Gynecol 117: 935–947.