Keywords
Health Professionals’ Inoculation, Vaccines, Immunization
Introduction
Vaccines work best when most members of a community are vaccinated - the more people are vaccinated, the lower the possible risk of anyone's exposure to vaccine-preventable diseases. Because vaccines must be safe for use by as many people as possible, vaccines are developed in accordance with the highest standards of safety. Years of testing are required by law before a vaccine is licensed and distributed. Once in use, vaccines are continually monitored for safety and efficacy. However, as with any medical procedure, vaccination has some risks as well as substantial, proven benefits. Individuals react differently to vaccines, and there is no way to absolutely predict the reaction of a specific individual to a particular vaccine. Anyone who takes a vaccine should be fully informed about both the benefits and the risks of vaccination [1].
The significance of applying a full-inoculation program to health professionals leads to a substantial decrease in the morbidity rate of infectious diseases between patients and employees.
The recommendations concerning the vaccines are based on the characteristics of the immunologic factors, on the scientific knowledge of the principles of active and passive immunization, on the epidemiology and the characteristics of diseases (e.g. morbidity, mortality, therapeutic cost and productivity loss), on the estimation of vaccine safety, on the cost analysis of the preventive measures, on the published and unpublished studies and finally on the public health specialists’ views over Clinical and Preventive Medicine. The benefits and the risks of vaccines are closely related with all immunologic factors (e.g. antigenic substance or antibody drug) [1].
The heath-care professionals due to their contact with patients or patients’ contagious materials are in constant exposure risk and potential disease transmission, which obviously can be prevented by an inoculation program. For this reason, the immunological conservation is considered an extremely crucial part of the preventive programs and infection control of the health-care professionals. The proper use of the immunologic factors secures the health-care professionals and furthermore protects the patients against an infection, preventing the contagious risk from the health-care professionals to the patients [2].
The continuous immunization programs could substantially reduce the number of infections met among health-care professionals working at general hospitals and the accompanying risk of transmitting the diseases, which may be prevented through inoculation in other employees and patients. Every Service or Department, which provides health services to patients, should be encouraged to practice a concise immunologic policy on all health-care professionals. The American Hospital Association [3] has confirmed immunologic programs for the hospital’s employees as well as the patients. The immunologic recommendations of the Advisory Committee on Immunization Practices (ACIP) [4] for health-care professionals should be taken into account for the development of the particular policy.
Purpose: The aim of the present study was to record and evaluate the immunization levels of the health-care professionals in the General Hospital of Korinth.
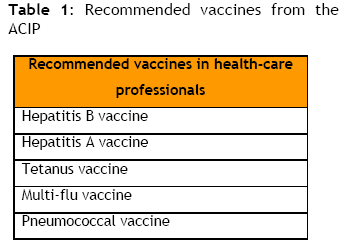
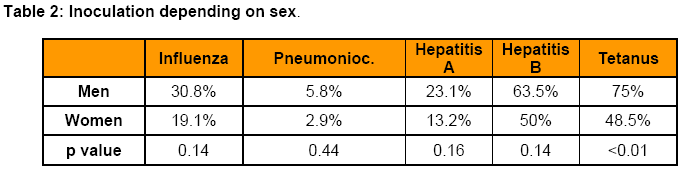
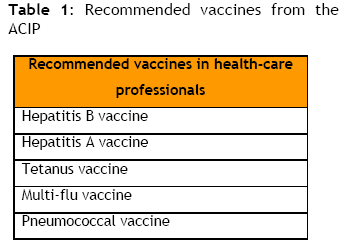
Method and material: We have conducted a descriptive, cohort study of correlation. The screening survey was performed from January 2007 – March 2007 in health-care professionals of the General Hospital of Korinth. Health-care professionals included were only of medical and nursing staff of the hospital. Data collection was based on an anonymous questionnaire designed for the purpose of the present study, according to the bibliographic references and the inoculation recommendations, the Advisory Committee on Immunization Practices (ACIP) [4], the Centers for Disease Control and Prevention (CDC) [1,2] and the Greek Department of CDC. (K.E.E.L.P.Ν.Ο.). Health-care professionals were asked whether they had been inoculated with one of the following vaccines (Hepatitis A, Hepatitis B, Tetanus, Multi-flu and Pneumococcal vaccine) which are described on Table 1.
In total, 250 questionnaires were distributed, of which 233 were filled in, 17 were lost and 20 were excluded due to incomplete filling. The total samples of our study were consisted of 213 correct filled in questionnaires.
Statistical analysis: The statistical analysis was conducted using the statistical program SPSS 13. Quantitative variables were examined, in order to ascertain normal distribution, according to Kolmogorov-Smirnof criterion. X2 test and Fishers’ exact test were used to compare proportions.
A probability value (P value < 0,5) was considered to indicate statistical significance. Quantitative variables are depicted by mean value ± standard deviation.
Reliability and validity: The internal consistency reliability of our study was examined with coefficient alfa (Cronbach’s a), which was equal to 0,71. If the coefficient alfa >0.70 the reliability of the questionnaire is valid.
Results
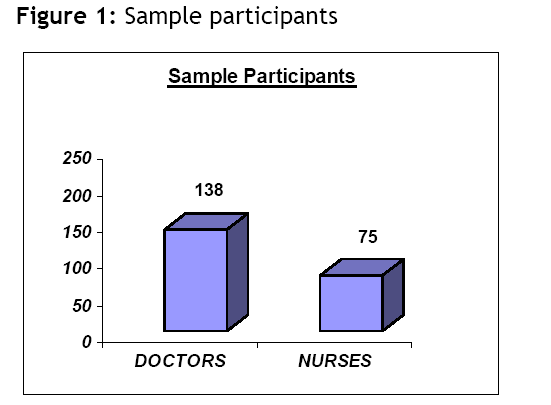
Sample participants were 138 Doctors and 75 Nurses (Figure 1). The mean age of the participants in the study was 35,7 years old, with a standard deviation of 9,6 years (SD±9,6).
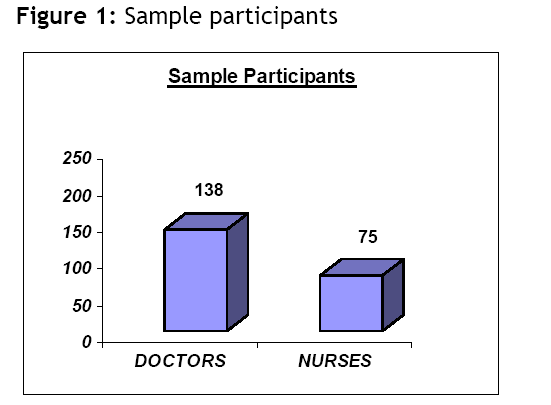
Figure 1: Sample participants
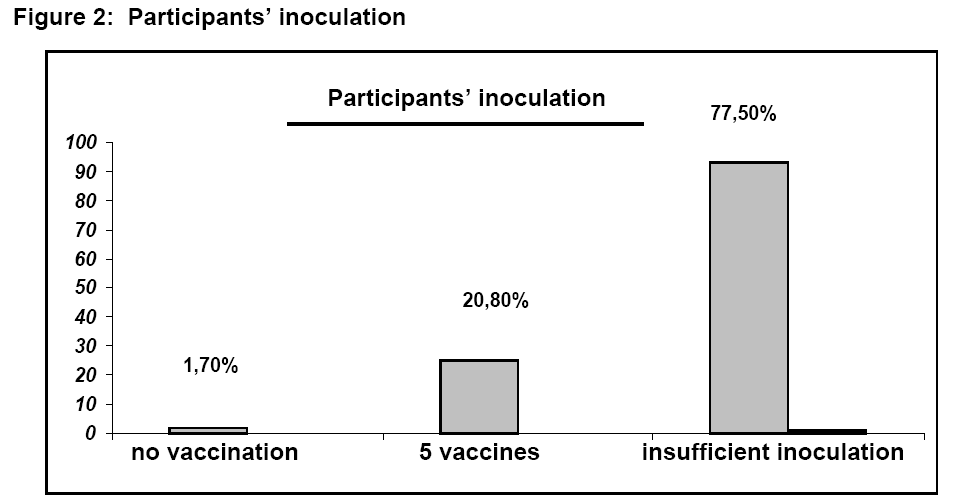
The results of the study have shown that only two (2) of the health-care professionals (1,7%) had not been inoculated with any of the five vaccines, which are mentioned in Table 1. Moreover, 25 employees (20.8%), reported full inoculation, that is, all five vaccines which are mentioned in Figure 2.
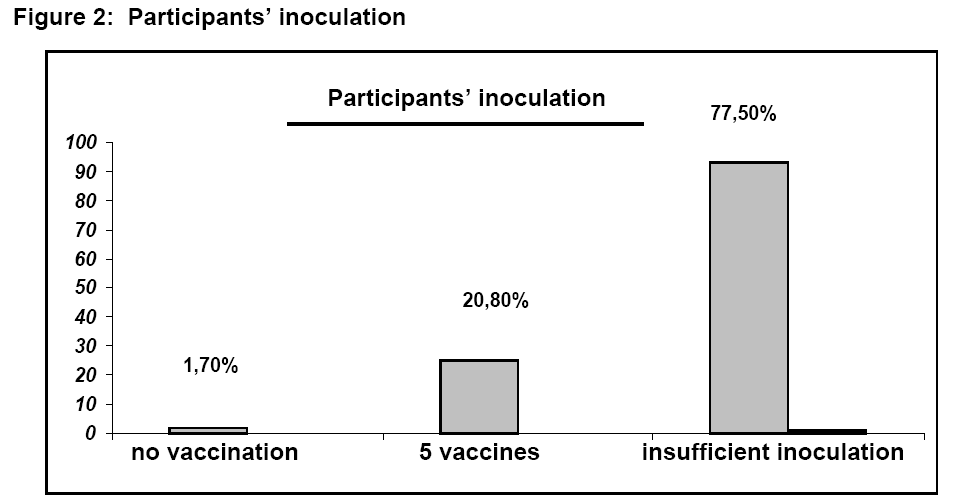
Figure 2: Participants’ inoculation
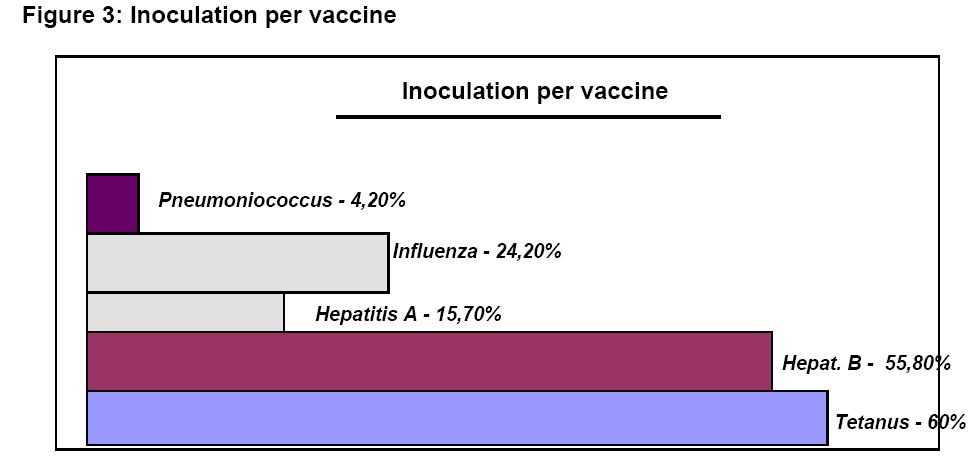
The aforementioned inoculation mainly involved Tetanus (60%), Hepatitis B (55.8%) and Hepatitis A (15.7%). Lastly, the Multi-flu vaccine (24.2%) and the Pneumococcal vaccine (4.2%) (Figure 3).
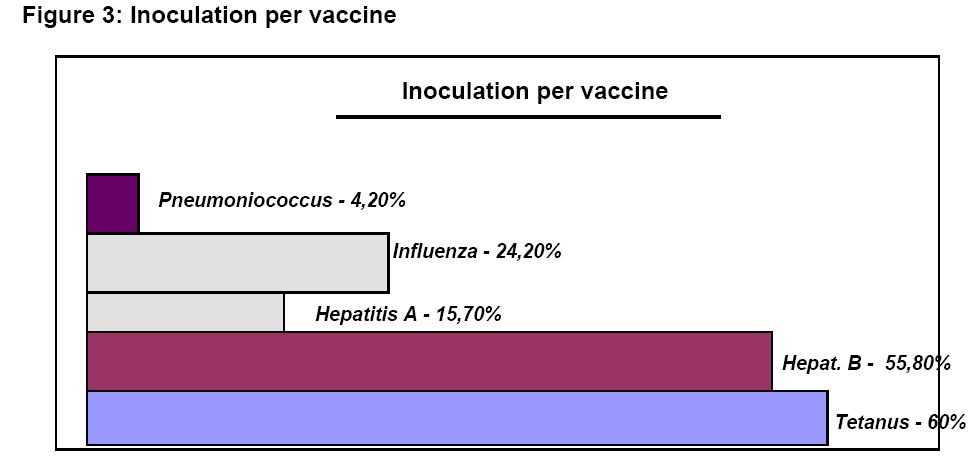
Figure 3: Inoculation per vaccine
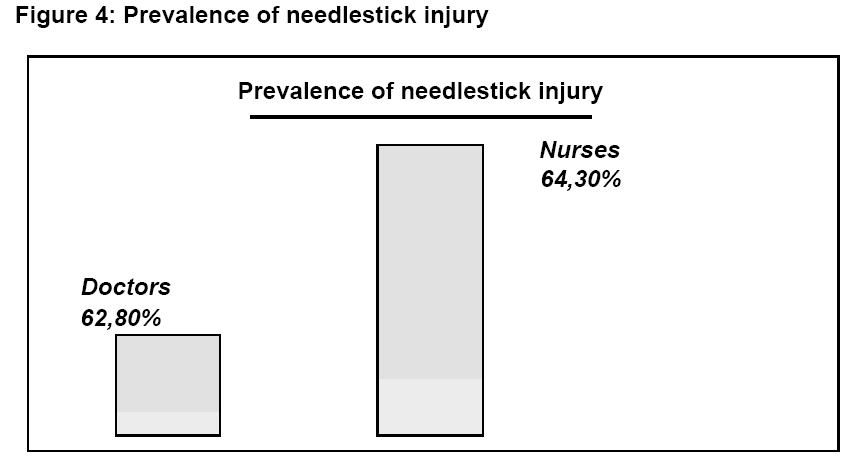
A high percentage 63.3% (n=76) of the health-care professionals reported that they suffered at least one needlestick injury during the past year.
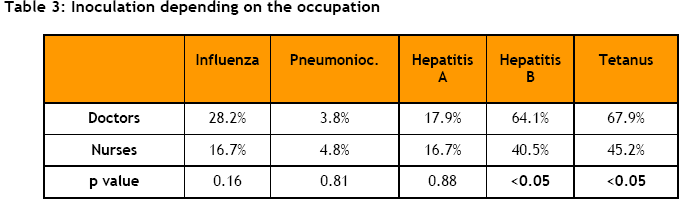
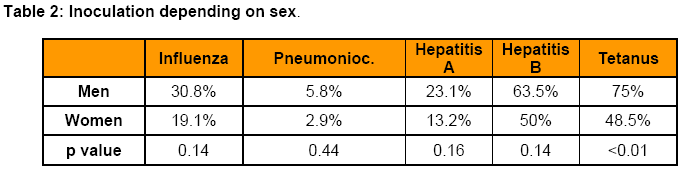
Correlations: Men report that they have been inoculated more frequently than women health-care professionals, with a higher statistical significant difference p<0.01 being observed in Tetanus inoculation (Table 2). In particular, men had been inoculated against Influenza in a percentage of 30.8%, against Pneumoniococcus 5.8%, against Hepatitis A 23.1%, against Hepatitis B 63.5% and against Tetanus 75%. On the contrary, women report that they have been inoculated against Influenza in a percentage of 19.1%, against pneumoniococcus 2.9%, against Hepatitis A 13.2%, against Hepatitis B 50% and against Tetanus 48.5%.
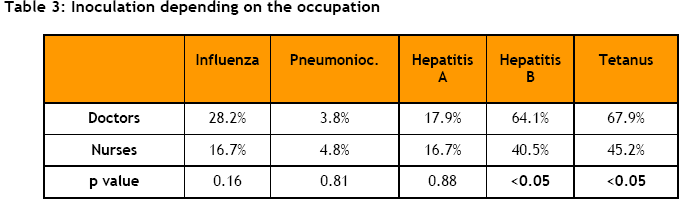
Correlating the participants with their occupation (Doctors – Nurses), it is observed that Doctors were more frequently inoculated than Nurses (28.3% vs. 16.7%), with a higher statistical significant difference being observed in Hepatitis B (64.1% vs. 40.5%) and Tetanus inoculation (67.9% vs. 45.2%), (p<0.05) (Table 3).
The prevalence of needlestick injury does not show any kind of statistical significant difference between Doctors (62.8%) and Nurses (64.3%) (Figure 4).
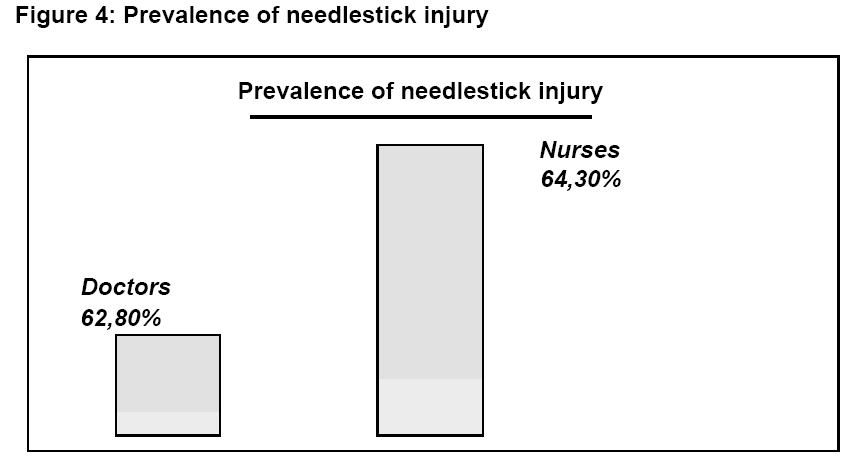
Figure 4: Prevalence of needlestick injury
According to their working domain (chirurgical-pathological), it was observed that the health-care professionals of the chirurgical department had a better immunologic profile and were more consistent with their inoculation program than the health-care professionals of the pathological department. Statistical significant difference was observed in the aforementioned groups especially as far as the Influenza (51.9% vs. 22.7%) p<0.01 and Hepatitis A inoculation (37% vs. 13.6%) p<0.05 is concerned. Non-statistical significant difference was observed in Pneumoniococcus, Hepatitis B and Tetanus inoculation; nevertheless healthcare workers in the Chirurgical department seem to have substantially higher rates of inoculation than those of the Pathological department (Table 4).

The age of the participants did not seem to affect the inoculation status. Moreover, judging from the results, no statistical significant difference was observed between the inoculation status and the post that the doctors held at the hospital (specialized and specializing doctors).
Lastly, it is worth mentioning that the health-care professionals who mentioned a needlestick injury more frequently, are the ones who either have been inoculated or were inoculated immediately after the injury (for Hepatitis B), than those who had never been exposed to such risk (63.2% vs. 43.2%, p< 0.05).
Discussion
The current study was conducted in a rural hospital and involved medical and nursing staff. In the hospital there are a great number of health care professionals (except for doctors and nurses) who ought to be inoculated according to the international guidelines. Nevertheless, our research focused on medical and nursing staff that is most certainly at a higher risk of infectious disease transmission.
From the demographic data of our sample the mean age of the participants in the study was 35.7 years old, a fact which is in agreement with several similar studies from the international bibliography [6,7].
Most of the participants note that they have been inoculated with Tetanus vaccine at a percentage of 60% and secondly with Hepatitis B vaccine at a percentage of 55.8%, percentage rates which emphasize that the health-care professionals are either not updated or they are extremely negligent.
The inoculation rate of Hepatitis B of the present study was 55,8%, a fact which is by far lower than the one mentioned in Robyn R. M. Gershon et al.,8 study, in which the full inoculation rate was at a percentage of 64%.
The full inoculation percentage in several studies fluctuates from 71%- 81% [9,10,11] while in other studies the percentages are much lower (40%-53%) [7,12,13,14], especially in countries with a high prevalence of the disease such as Nigeria [14].
The male doctors seem to have higher immunization percentages for Tetanus and Hepatitis B than female nurses. Similar correlations appear in other international studies, [7,15] while some researchers do not report correlations between inoculation and demographic data [16,11].
The percentage of the inoculated employees with multi-flu vaccine appears to be ominously low (24.2%). This result is in accordance with other studies results which detect extremely low percentages of anti-flu inoculation (19.6% and 20.6%) as in the studies of Gil H et al., [17] and R. Jimet et al. [18] Similarly, other studies appear to have extremely low percentages of anti-flu inoculation, up to 28% [15,19,20].
On the contrary, inoculation rates from 35%-62% are detected in several other studies [15,21,22], with the higher rates appearing in the studies of Nichol KL et al., [22] and Ohrt C.K et al., [23] in which the inoculation rate was between 61%-62%. It is worth mentioning that the latest researches have been conducted in the U.S.A. where all health-care professionals are familiar with antiflu vaccination.
According to a large number of studies [17,18,19], it is evident that the awareness, the broad knowledge and the accessibility to the vaccine constitute a crucial factor, which will contribute to the continuous increase of the anti-flu vaccine inoculation rate.
The decreased immunization rates of health-care professionals in our study, as far as Hepatitis A (15.7%) is concerned, are not consistent with the results of international studies [24,25], in which the immunization rates are over 50%. It is worth noting that the aforementioned results come from studies conducted not only in the USA but also in other European countries such as Belgium and Spain, in which the Hepatitis A vaccination is part of the obligatory inoculation. In Greece, Hepatitis A vaccination became mandatory in 1998.
The overall percentage of professional exposure (needlestick injuries) in the current study is approximately 63.3%, which is considered as a rather huge percentage rate. Similar studies report that professional exposures of all types are at a percentage rate of 45%- 93% [8,19,11]. The difference in the percentage rates of transdermal traumatism with a needlestick in our study, in contrast to other studies, could be attributed not only to new safety apparatus, which are applied in other countries, but also to the continuous education of the employees.
No statistical significant difference was detected, as far as the accident percentage rates between Doctors and Nurses (62.8% vs. 64.3%) is concerned. The substantially high accident rate should form the basis for new informational programs concerning safety measures in medical and nursing practice.
Finally, the unanticipated decreased inoculation levels 20,8%, with all of the five internationally recommended vaccines, is a great problem that we should all take serious thought of. Indeed inoculation with Tetanus vaccine shows satisfactory results not only for the employees of the Chirurgical (74.1%) but also of the Pathological Department (65.9%). In addition, inoculation with Hepatitis B vaccine shows increased but still not satisfactory rates both in the Chirurgical and Pathological Department (59.3% vs. 47.7%). On the contrary, inoculation with Hepatitis A, Pneumoniococcus and Influenza present discouraging results. Inoculation with Pneumoniococcus vaccine displays the worst results, 11.1% in the Chirurgical Department and 4.5% in the Pathological Department.
A series of published studies [13,14,18,20], have investigated the causes of success or failure of the inoculation programs of Health Services as well as the attitudes and beliefs of health care professionals. The main obstacles are lack of knowledge, the fear of side-effects, negligence and sometimes vaccines’ access difficulties.
Conclusions
The immunization rate of health-care professionals in our study depicts the alarming decreased levels of immunization. Nevertheless, we shouldn’t be comforted by the fact that such results appear in other countries’ studies, too. Despite inoculation campaigns and continuous education, the knowledge of the recommended vaccines and the preventive measures are still at an extremely low rate.
Although we are aware that inoculation of health care professionals is considered a personal right, we strongly support the idea that inoculation with certain vaccines should be mandatory (as it is constituted in USA and other European countries such as Great Britain).
In order to avoid the aforementioned causes of inoculation programs’ failure and increase the inoculation rates, we should carefully design inoculation programs which take into account the particular needs in every field of the health care system.
The application of an inoculation protocol at every hospital, the continuous and intensive attempts for further education and knowledge, the establishment and control of immunization data for all health-care professionals are some of the measures that would most certainly aid the increase of the inoculation rate, as well as the decrease in the transmission of infectious diseases, for the benefit of the health-care professionals and the patients.
3637
References
- CDC. Update: vaccine side effects, adverse reactions, contraindications, and precautions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 1996;45(No. RR-12).
- CDC. Guidelines for prevention of transmission of human immunodeficiency virus and hepatitis B virus to health-care and public-safety workers: a response to P. L. 100–607, The Health. Omnibus Programs Extension Act of 1988. Atlanta, GA.: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control.1989; 1–45.
- American Hospital Association. Immunization: management advisory on health care delivery. American Hospital Association. 1992: Chicago, Illinois.
- CDC. Guidelines for prevention of transmission of human immunodeficiency virus and hepatitis B virus to health-care and public-safety workers: a response to P. L. 100–607, The Health. Omnibus Programs Extension Act of 1988. Atlanta, GA.: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control.1989;1–45.
- American Hospital Association. Immunization: management advisory on health care delivery. American Hospital Association. 1992, Chicago, Illinois.
- LaVela SL, Smith B, Weaver FM, Legro MW, Goldstein B, Nichol K. Attitudes and practices regarding influenza vaccination among healthcare workers providing services to individuals with spinal cord injuries and disorders. Infect Control Hosp Epidemiol. 2004;25:933–940.
- Dannetun E, Tegnell A, Torner A, Giesecke J. Coverage of hepatitis B vaccination in Swedish healthcare workers. J Hosp Infect.2006;63(2):201-4.
- Gershon RR, Mitchell C, Sherman MF, Vlahov D, Lears MK, Felknor S,et al. Hepatitis B vaccination in correctional health care workers. Am J Infect Control. 2005;33(9):510-8.
- King WD, Woolhandler STJ, Brown AF, Jiang L, Kevorkian K, Himmelstein DU, et al. J GEN INTERN MED 2006; 21:181–184.
- Cronbach LJ (1990). Essentials of Psychological Testing, 5th edn. Harper Collins, New York.
- Manso VF, Castro KF, Matos SM, Junqueira AL, Souza SB, Sousa MM, et al. Compliance with hepatitis B virus vaccination and risk of occupational exposure to blood and other body fluids in intensive care department personnel in Brazil. Am J Infect Control. 2003 Nov;31(7):431-4.
- Louther J, Feldman J, Rivera P, Villa N, DeHovitz J, Sepkowitz KA. Hepatitis B vaccination program at a New York City hospital: seroprevalence, seroconversion, and declination. Am J Infect Control. 1998;26(4):423-7.
- Spence MR, Dash GP. Hepatitis B: perceptions, knowledge and vaccine acceptance among registered nurses in high- risk occupations in a university hospital. Infect Control Hosp Epidemiol 1990; 11(3): 129-33
- Fatusi AO, Fatusi OA, Esimai AO, Onayade AA, Ojo OS. Acceptance of hepatitis B vaccine by workers in a Nigerian teaching hospital. East Afr Med J. 2000;77(11):608-12.
- Mah MW, Hagen NA, Pauling-Shepard K, Hawthorne JS, Mysak M, Lye T, Understanding influenza vaccination attitudes at a Canadian cancer center. Am J. Infect Control 2005; 33:243-50.
- Nakayama T, Aizawa C, Kuno-Sakai H. A clinical analysis of gelatin allergy and determination of its causal relationship to the previous administration of gelatin containing acellular pertussis vaccine combined with diphtheria and tetanus toxoids. J Allergy Clin Immunol 1999; 103:321–5.
- Gil H, Bailly P, Meaux-Ruault N, Clement I, Floret N, Guiot A, Manteaux C, et al. Influenza vaccination among health-care workers. Vaccination rates in universitary hospital of Besançon, winter 2003-2004. Rev Med Interne. 2006;27(1):5-9.
- Jiménez-García R, Hernández-Barrera V, Carrasco-Garrido P, Sierra-Moros MJ, Martinez-Hernandez D, de Miguel AG. Influenza vaccination coverages among Spanish children, adults and health care workers. Infection. 2006;34(3):135-41.
- Mc Ewen M, Farren E. Actions and beliefs related to hepatitis B and influenza immunization among registered nurses in Texas. Publ Health Nurs 2005;22(3): 230-9.
- Qureshi AM, Hughes NJ, Murphy E, Primrose WR. Factors influencing uptake of influenza vaccination among hospital-based health care workers. Occup Med (Lond). 2004;54(3):197-201.
- Murray SB, Skull SA. Poor health care vaccination coverage and knowledge of vaccination recommendations in a tertiary Australia hospital. Aust N Z J Public Health. 2002; 26(1): 65-8.
- Nichol KL, Hauge M. Influenza vaccination of healthcare workers. Infection Control Hosp. Epidemiol. 1997;18(3):189-94.
- Ohrt C.K, McKinney W.P. Achieving compliance with influenza immunization of medical house staff and students. A randomized controlled trial. The journal of the American Medical Association. 1992;Vol :267, No: 10.
- Smith S, Weber S, Wiblin T, Nettleman M. Cost-effectiveness of hepatitis A vaccination in healthcare workers. Infection control and hospital epidemiology. 1997;Vol. 18, (10), pp: 688-691.
- Thoelen S, Van Damme P, Leentvaar-Kuypers A, Leroux-Roels G, Bruguera M, Frei PC, et al. The first combined vaccine against hepatitis A and B: an overview. Vaccine. 1999;17(13-14):1657-62.