Case Report - (2022) Volume 0, Issue 0
Acute Appendicitis in Situs Inversus Totalis: A Case Report and Literature Review
Rafael Arraut Gamez1*,
Jesus Gomez Barrios1,
Darith Molinares Perez1,
María Torres de Franca2,
Juan Esteban Tafur Delgado3 and
Laura Valencia Zapata4
1General Surgery Resident, Universidad Libre seccional Barranquilla, Colombia
2General Physician, Universidad Metropolitana de Barranquilla, Colombia
3Pediatric Resident, Universidad del Sinu, Colombia
4Emergency Medicine Resident, Universidad Cooperativa de Medellin, Colombia
*Correspondence:
Rafael Arraut Gamez, General Surgery Resident, Universidad Libre seccional Barranquilla,
Colombia,
Email:
Received: 22-Apr-2022, Manuscript No. Iphsj-22-12748;
Editor assigned: 24-Apr-2022, Pre QC No. Iphsj-22-12748 (PQ);
Reviewed: 27-May-2022, QC No. QC No. Iphsj-22-12748;;
Revised: 01-Jun-2022
Published:
09-Jun-2022, DOI: 10.36648/1791-809X.16.S7.950
Abstract
Situs inversus is a rare condition caused by a congenital anomaly that consists of the inverted position of thoracic or abdominal organs with respect to the sagittal plane, with a low incidence in the general population and usually incidental finding. On the other hand, acute appendicitis is the acute inflammation of the vermiform appendix, being the most common abdominal surgical pathology in the world. We report the case of a 43-year-old female patient with no medical history, who comes to a hospital in the course of abdominal pain of onset in the epigastrium with subsequent migration of the mesogastrium and right iliac fossa, associated with SIRS, anorexia and signs of irritation. Peritoneal, in whom an open appendectomy was performed with the particularity of showing in the intraoperative ileocecal complex with macroscopic inflammatory characteristics of the left location and inverted position of the rest of the intra-abdominal organs, constituting a rare case of acute appendicitis in complete situs in versus.
Keywords
Acute appendicitis; Situs in versus; Congenital anomaly
Introduction
Situs inversus is a rare condition caused by an autosomal recessive
congenital anomaly caused by mutations located on the long arm
of chromosome 14 and deletions that affect chromosomes 7 or
8. Classically, two types of presentations are described, sites in
versus totals or complete, the most usual form, characterized by
the mirror image location of intra-abdominal and thoracic organs
including the heart, or partial or incomplete situs inversus, with a
prevalence of 1:22,000 births, determined by the mirror image of
the organs intra-abdominal and thoracic, but the heart in normal
disposition [1].
Acute appendicitis is one of the most common intra-abdominal
diseases and the main abdominal surgical emergency. It accounts
for approximately 5% of all emergency department visits
for patients under 65 years of age and 30% of acute surgical
abdominal emergencies in patients fewer than 50 years of age
worldwide [1]. Acute appendicitis with situs invesrus totals is
reported between 0.016 and 0.024%, becoming a true diagnostic
dilemma due to the abnormal position of the appendix and the
inconsistency with clinical signs and symptoms. In this article we
report a case of acute appendicitis with complete situs inversus.
Case presentation
We present the case of a 43-year-old female patient. She went to the emergency room due to a clinical picture of 28 hours
of evolution at admission, characterized by predominantly
epigastric abdominal pain with migration to the mesogastrium
and later to the hypogastrium with lateralization to the right iliac
fossa. Associated with quantified thermal increases, anorexia
and intolerance to the oral route. Within her personal history,
she denies pathological, toxic, and allergic components, but she
states that she had performed a caesarean section 8 years ago.
In her initial assessment, a patient was found to be in fair general
condition, algid, with vital signs (TA 110/80 mmHG, HR 110
L*m, RR 18 R*m, T 38.5°c, So2 96%), with data from systemic
inflammatory response (SIRS)
On physical examination she has clear signs of peritoneal irritation
(blumberg, psoas, obturator, dunphy positive), without pain on movement of the cervix or pathological genital discharge. Blood
chemistry is performed with evidence of normochromic anaemia,
normocytic WHO GI. Marked leucocytosis at the expense of
neutrophilia, with elevated CRP-type acute phase reactant,
negative BHCG and coagulation times within normal limits.
Given the manifestations described above and a high-risk
Alvarado score for acute appendicitis, it was decided to transfer
to the operating room to perform an open appendectomy. Prior
administration of prophylactic antibiotics and optimization of
medical management.
Initially, a Rocky-Davis-type incision was made, dissecting by
planes until reaching the abdominal cavity without showing
evidence of an ileocecal-appendicular complex after an
exhaustive search. For this reason, an infraumbilical medial
approach was performed, requiring blunt digital adherenciolysis
due to established Zuhlke grade III omentum-parietal adhesions,
drainage of peritoneal reaction fluid. It is evidenced with the
ileocecal complex of the left location. An appendectomy was
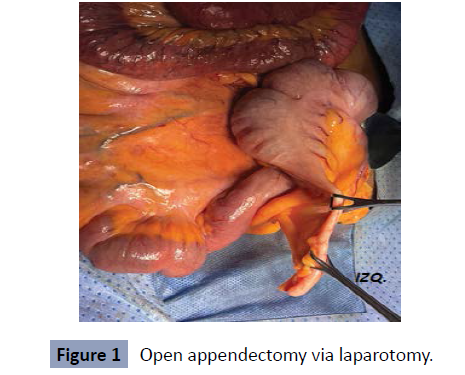
performed with extraction of the surgical piece (image 1) with
management of the appendicle stump with 2.0 Pouchet-type
silk and a systematic review of the abdominal cavity showing the
spleen, stomach, Treitz ligament on the right side and second
portion of the duodenum, liver together with the gallbladder,
ascending colon on the left side without concomitant injuries.
Haemostasis is verified, the parabolic slides and the pelvic cavity
are cleaned. We proceed to perform closure by planes, up to the
skin. With completed surgical procedure, without immediate
complications (Figure 1).
Figure 1: Open appendectomy via laparotomy.
In his postoperative period he evolves satisfactorily, returning
positive and effective intestinal transit, with resumption of
the oral route early. Thoracoabdominal tomography Figure 2 is performed, showing dextrocardia, confirming sites inversus
totals (Figure 2).
Figure 2: (a) Thoracoabdominal CT in coronal view, showing
inversion of the position of the thoracic and abdominal
organs. (b) Chest CT showing dextrocardia.
Patient currently without late postoperative complications,
without hospital readmissions during the first 30 days.
Literature review
Acute appendicitis is an extremely common abdominal disease or
surgical pathology worldwide, which represents one of the main causes of emergency abdominal surgery. It has been reported
that its highest incidence is among the population between
20 and 30 years old, emphasizing that this pathology does not
show gender predominance; although in some reports certain
percentages are shown. In addition, its clinical manifestation
is versatile on certain occasions; therefore the use of imaging
studies must be used to establish an effective diagnosis in this
way. Similarly, it should be noted that the treatment by which
acute appendicitis is managed is surgery with a laparoscopic or
open approach [2].
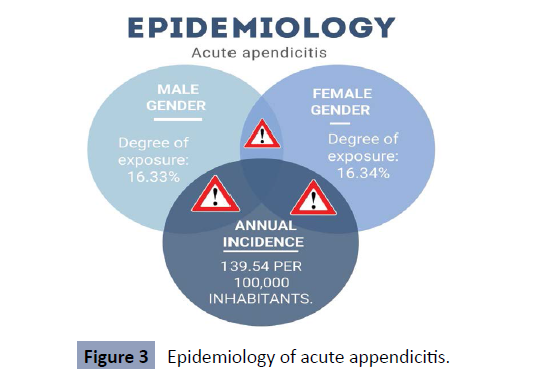
Epidemiology
Acute appendicitis is the most common cause in emergency nontraumatic
abdominal surgery, as mentioned above. This presents
a degree of exposure of 16.33% in males and 16.34 in females. Its
annual incidence is 139.54 per 100,000 inhabitants (Figure 3) [8].
Clinical manifestations
Figure 3: Epidemiology of acute appendicitis.
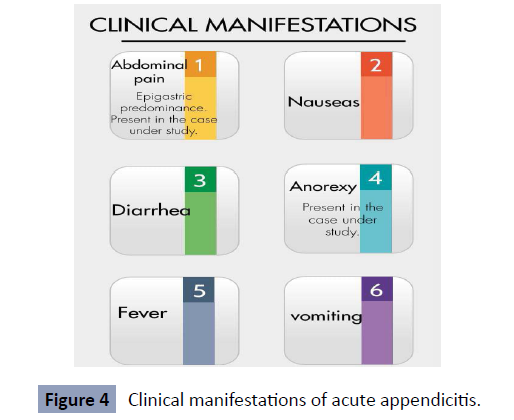
Abdominal pain is the most common symptom manifested in
patients, although we can also find other signs such as: nausea,
anorexia, diarrhoea and fever. It is necessary to mention that
this pain is per umbilical and epigastric, and then expands to
the lower right quadrant; however this is a classic symptom that
occurs only in 50 to 60% of patients.
The manifestation of nausea and vomiting usually occurs after
the onset of pain, pyrexia becomes apparent after six hours
of the clinical picture. But to a certain extent these clinical
manifestations can change from one person to another [3].
In the physical examination of patients with this pathology,
vital signs are usually taken, where we can find a temperature
greater than 38°C, heart rate above 100, that is, tachycardia and/
or in some cases tachypnea also occurs. On the other hand, it is
essential to bear in mind that the first signs and symptoms of acute
appendicitis are nonspecific, but that through the irradiation that
occurs in the lower right quadrant, it is detectable to a certain
extent on physical examination, but they must perform certain
studies to corroborate their diagnosis [4].
The maximum point of pain in the abdomen almost always
corresponds to McBurney's point, which is located two-thirds of
the way from the umbilicus on a line drawn from the umbilicus to
the right anterior superior iliac spine [5] (Figure 4).
Figure 4: Clinical manifestations of acute appendicitis.
Diagnosis
To establish an effective diagnosis of acute appendicitis, it is
necessary or relevant to take into account certain criteria, such
as the physical examination of the patient, the results of relevant
studies (laboratories, images, among others) and findings
obtained in the interview. Likewise, it should be clarified that
through the physical examination a judgment of said pathology
can be obtained, but this depends on the experience of the
health personnel who carry it out, therefore the importance
of carrying out a whole study together and in this way offer an
accurate diagnosis [6].
Situs inversus total’s (SIT)
Situs inversus total’s is a rare congenital malformation, which
involves the transposition of thoracic and abdominal organs;
which in turn complicates the diagnosis and management of the
acute abdomen. The presence of and ITS does not mean a serious
risk to health, but its early detection is essential, especially when
we are facing certain pathologies that require immediate surgical
intervention [7].
Discussion
Acute appendicitis is one of the most frequent intra-abdominal
diseases and the main abdominal surgical emergency. It accounts for approximately 5% of all emergency department visits
for patients under 65 years of age and 30% of acute surgical
abdominal emergencies in patients under 50 years of age
worldwide [8].
Appendicitis accounted for 318,000 hospital admissions in the
US in 2006, and has an overall incidence of approximately 82 to
110/100,000 populations in North America. The lifetime risk of
appendicitis is 8.6% for men and 6.7% for women in Western
countries. And may be double this risk in Asia [9].
It usually presents clinically as a dull epigastric or periumbilical
pain, accompanied by nausea or emesis, fever, and hyporexia.
Hours later, it radiates and is located in the lower right quadrant
[1]. However, its presentation in the left lower quadrant is
infrequent, and may be due to congenital or anatomical causes.
Four disorders can cause the appendix to be left-sided, and in
order of frequency they are: 1.) visceral transposition (situs
inversus), 2.) Intestinal malrotation, 3.) Wandering cecum with a
long mesentery, and 4.) Appendage of excessive length, crossing
the midline [3]. For reasons of the present case, we will focus on
the first note.
Situs inversus is a rare condition caused by an autosomal recessive
gene with incomplete penetrance and occurs in 1/10,000 to
1/35,000 live births [4, 5].
This condition can be complete when both the thoracic and
abdominal organs are transposed, or partial when only one of
these cavities is affected [5].
The incidence of situs inversus total’s reported in the literature
varies from 0.001 to 0.01% in the general population (5,6);
however, the incidence of acute appendicitis with situs invesrus
total’s is reported between 0.016 and 0.024% (6). According
to reports published in the literature, acute appendicitis in
situs inversus occurs between 8 and 63 years of age and is 1.5
times more frequent in men. In a study in the World Journal of
Gastroenterology, it was found that the average age was 29.3 ±
16.1 years and the male-female ratio was 1.5:1 [1].
Acute appendicitis in situs inversus is a true diagnostic dilemma
due to the abnormal position of the appendix. It is assumed that
although the viscera are transposed, the nervous system may not
show the corresponding transposition, which results in confusion
of signs and symptoms [9]. Thus, in about 18.4 to 31% of patients
with situs inversus and intestinal malrotation, the pain caused
by acute left appendicitis has been reported in the right lower
quadrant [1, 7].
In general, the diagnosis of surgical diseases in these patients
is delayed due to low clinical suspicion, so these patients are
usually diagnosed in advanced stages of the disease [5].
Diagnosis of acute appendicitis in situs inversus is generally Trans
operative motivated by the clinical picture of acute abdomen.
In some cases, the imaging diagnosis evidenced by contrastenhanced
abdominal CT is documented, and in some population
groups where tomography is contraindicated, another viable
option would be MRI [7].
The tomographic findings evidenced would emanate the situs inversus of the intra-abdominal organs, in addition to the findings
already described by the appendicular inflammatory process.
Conclusions
It is extremely important to know the different existing differential
diagnoses of acute abdominal pain in the lower right quadrant,
since many of these pathologies can cause referred pain with
completely different clinical presentation and surgical findings,
at the time of performing the operative approach.
Acute left appendicitis, as a rare clinical entity, should not be
underestimated and as an aetiology of acute abdomen, its
diagnosis and possible treatment should not be delayed as long as
possible. With the aim of avoiding life-threatening complications
for this small population group. The obvious shortcomings in our
health system, especially in the public network. As well as the
non-availability of immunological diagnostic aids and minimally
invasive or laparoscopic equipment, clinical suspicion should not be delayed or diminished, especially in this entity, and the
surgical approach should be carried out according to the devices
or instruments available in each service.
Imaging research and multidisciplinary follow-up, after the
generally intraoperative diagnosis of situs inversus, is essential,
in order to evaluate possible complications in other organs or
systems.
Compliance with ethical standards
Informed consent
Informed consent from the patient in reference to the case was
obtained with extensive and extensive prior information.
Interest conflict
The authors declare that they have no conflict of interest with
respect to the publication of this document.
REFERENCES
- Mark L, Kovler MD, David J, Hackam MD PhD (2021) Apendicitis Terapias quirúrgicas actuales cap 53:284-289.
Google Scholar
- Frederick H, Millham (2021) Dolor abdominal agudo Enfermedad gastrointestinal hepatica de Sleisenger Fordtran 1:144-157.
Google Scholar
- Apendice L J, Skandalaskis G L, Colborn T A, Weidman J E (2021) Skandalaskis Cirugía bases de la anatomia quirurgica de Skandalaskis Cap 17:648-661.
Indexed at, Google Scholar
- Contini S, Dalla Valle R, Zinicola R (1998) Suspected appendicitis in situs inversus totalis. Surg Laparosc Endosc 8:393-394.
Indexed at, Google Scholar
- Vicente de Jesus Aljure Reales, Gloria Camila Alvarez Gallego, Nasly Consuelo Avila Espitia (2017) Situs inversus totalis topic review approach to Genetics and case report. Rev Colomb cardiol 24:1.
Google Scholar, Crossref
- Golash V (2006) Laparoscopic management of acute appendicitis in situs inversus. J Minim Access Surg 2:220-221.
Indexed at, Google Scholar, Crossref
- Juan David Zuluaga-Restrepo, Maria del mar Meza (2012) Acute appendicitis in situs inversus totalis: a case report. Isabel cristina Herrera-Moncada CES Med 26:2.
Indexed at, Google Scholar, Crossref
- Hernandez-Cortez Jorge, Leon-Rendon Jorge Luis De, Martinez-Luna Martha Silvia, Guzman-Ortiz Jesus David, Palomeque-Lopez Antonio, Cruz-Lopez Nestor etal. (2019) Apendicitis aguda revision de la literatura. Cir gen 41:33-38.
Google Scholar
- Aljure Reales Vicente de Jesus, Alvarez Gallego Gloria Camila, Avila Espitia Nasly Consuelo, Arrieta Coley Alexandra, Angel Suarez Orlando (2017) Germany Situs inversus totalis: revision de tema con aproximacion a la genetica y reporte de casos. Revista Colombiana de Cardiologia 24:40-47.
Indexed at, Google Scholar, Crossref
Citation: Gamez RA, Barrios JG, Molinares
Perez D, Thorne Velez H, Caballero T, et al.
(2022) Acute Appendicitis in Situs Inversus
Totalis: A Case Report and Literature Review.
Health Sci J. Vol. 16 No. S7: 950.