Keywords
Tuberculosis; NTP; Pulmonary TB; Bacteriologically confirmed PTB; Treatment success rate
Introduction
Background
Libya is Located in Northern Africa; It is the fourth largest country in Africa, and the seventeenth largest country in the world. Libya covers 1759540 square kilometers, but has one of the world’s lowest population densitie-3.6 people per every square kilometer [1]. The last nationwide census was in 2006, it was confirmed that 5,298,000 people were living in the country, females to male ratio is almost 2:1 with an annual population growth rate of 1.02% [2].
Libya is a middle burden TB country, based on the recent Annual 2018 Global Report, the total number of newly notified TB cases in 2017 was estimated at 2500, CNR at 40 cases per 100,000 populations, but registered cases were only 1363 through passive diagnosis by the Libyan NTP, 59% of these cases were pulmonary TB cases, 64% of them were bacteriologically confirmed pulmonary TB cases, incidence of occurrence MDR-RR TB cases was estimated as 1.8 per 100,000 populations. Treatment success rate was 59% [3].
TB control in Libya is a vertical program under the umbrella of National Center of Diseases NCDC. It oversees 31 NTP branches and 5 hospitals distributed all over the country. TB detection in Libya is based mainly on passive case finding, providing care to symptomatic patients referred to NTP health facilities. Under the Libyan National Tuberculosis Program, there are four Regional Tuberculosis and Chest Centers, Tripoli in the Western Region, Misurata in the Middle region, Benghazi in the Eastern Region and Sabha in the Southern Region.
The country's political situation has affected its health infrastructure tremendously, in Early 2011, amid a wave of popular protest in countries throughout the Middle East and North Africa, largely peaceful demonstrations against entrenched regimes brought quick transfers of power in Egypt and Tunisia. In Libya, however, an uprising against the fourdecade rule of Muammar al-Qaddafi led to civil war and international military intervention [4]. Nevertheless Libya's problems are far from over.
Methods
This study was carried out to describe the epidemiology of TB in focusing mainly on bacteriologically confirmed PTB in Libya. Retrospective analysis of data was carried out using data from the TB registry of NTP from 2007-2014 using WHO’s framework for TB case definitions and reporting 2013, Comparisons were made using different variants such as TB case notification rates, clinical presentation, and treatment outcome. This study was conducted using data collected by the NTP branches. New notified TB cases and treatment outcome are collected from different NTP branches scattered across the country.
Data Collection
The data is collected and processed and disaggregated according to demographic and clinical characteristics of the disease, at first data is collected using standardized paperbased patient charts, these forms are then transferred to the NTP monitoring and evaluation unit to be processed, aggregated surveillance data are then entered quarterly into an electronic database using Windows Excel spreadsheet by the statistical unit of the NTP which enters and processes this data.
Data Analysis
Descriptive statistics such as tables, graphs and charts were used to analyze the data. Important markers were also identified such as the case notification rates and ratios and percentages.
Case definitions
• A bacteriologically confirmed TB case is one from whom a biological specimen is positive by smear microscopy, culture or WRD (such as Xpert MTB/RIF). All such cases should be notified, regardless of whether TB treatment has started.
• A clinically diagnosed TB case is one who does not fulfill the criteria for bacteriological confirmation but has been diagnosed with active TB by a clinician or other medical practitioner who has decided to give the patient a full course of TB treatment. This definition includes cases diagnosed on the basis of X-ray abnormalities or suggestive histology and extra-pulmonary cases without laboratory confirmation.
• Classification based on anatomical site of disease
• Pulmonary tuberculosis (PTB) refers to any bacteriologically confirmed or clinically diagnosed case of TB involving the lung parenchyma or the tracheobronchial tree.
• Extra-pulmonary tuberculosis (EPTB) refers to any bacteriologically confirmed or clinically diagnosed case of TB involving organs other than the lungs, e.g. pleura, lymph nodes, abdomen, genitourinary tract, skin, joints and bones, meninges [5].
• Once evaluated patients are assigned one of these treatment outcomes:
• Cured a pulmonary TB patient with bacteriologically confirmed TB at the beginning of treatment who was smear- or culture-negative in the last month of treatment and on at least one previous occasion.
• Treatment completed a TB patient who completed treatment without evidence of failure BUT with no record to show that sputum smear or culture results in the last month of treatment and on at least one previous occasion were negative, either because tests were not done or because results are unavailable.
• Treatment failed a TB patient whose sputum smear or culture is positive at month 5 or later during treatment.
• Died a TB patient who dies for any reason before starting or during the course of treatment.
• Lost to follow-up a TB patient who did not start treatment or whose treatment was interrupted for 2 consecutive months or more.
• Not evaluated a TB patient for whom no treatment outcome is assigned. This includes cases “transferred out” to another treatment unit as well as cases for whom the treatment outcome is unknown to the reporting unit [5].
Results
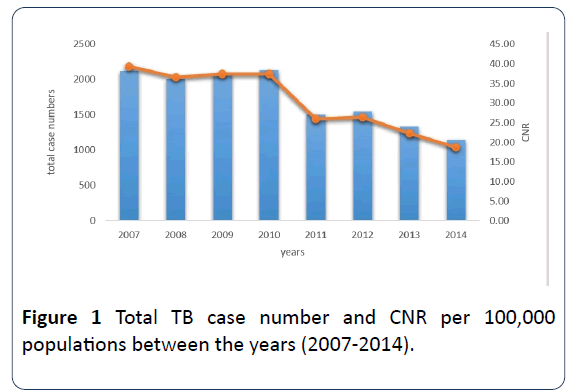
TB case detection in Libya is mainly done passively; patients seeking medical attention who are presumed to have TB are referred to one of our NTP branches for further investigation, branches use chest x-rays, sputum microcopy and culture to diagnose the patient. Throughout the study period the annual TB CNR has drastically decreased for all TB forms, beginning at 40 annual CNR per 100,000 populations in the year 2007 up to 19 per 100,000 populations at 2014. Clearly, these setbacks are however rather understandable considering the unprecedented circumstances the country has witnessed, since 2011 Libya has been dealing with a difficult turmoil; the country has been in chaos since the overthrow of Gaddafi regime in October 2011 which took a toll on the country's infrastructure (Figures 1-3).
Figure 1: Total TB case number and CNR per 100,000 populations between the years (2007-2014).
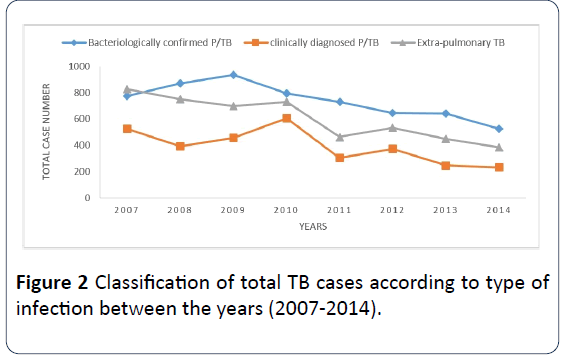
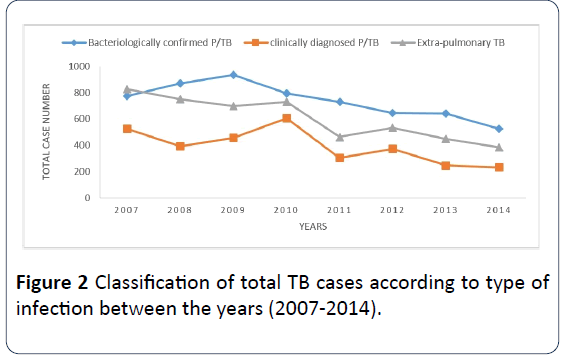
Figure 2: Classification of total TB cases according to type of infection between the years (2007-2014).
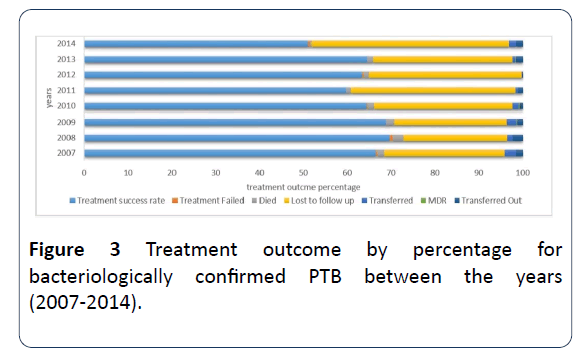
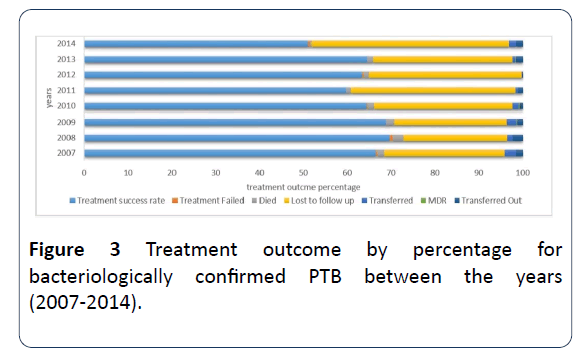
Figure 3: Treatment outcome by percentage for bacteriologically confirmed PTB between the years (2007-2014).
Since the end of the 2011 Libyan Civil War, which overthrew former leader Muammar Gaddafi, there has been violence involving various militias and the new state security forces. The violence has escalated into the current War. Clearly there are 2 setbacks in case notification that follow these political conditions. The first in 2011 with the Libyan uprising against former political regime, CNR were about 26 per 100,000 populations. Following 2010 that was the year with highest recorded CNR of 37 per 100,000 populations. The second decline was in 2014 when a civil war broke in the country's largest cities Tripoli and Benghazi. It was the lowest numbers to be observed throughout the study period, where the total number of notified cases was only 1142 nearly half of that of 2010 the case notification rate was only about 19 per 100,000 per population (Table 1).
Table 1: Treatment outcome results for total case numbers of bacteriologically confirmed pulmonary TB cases between the years (2007-2014).
| Treatment outcome |
Year |
| 2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
2013 |
2014 |
| Treatment Completed |
182 |
151 |
200 |
163 |
122 |
175 |
193 |
151 |
| Cured |
331 |
456 |
441 |
344 |
309 |
229 |
219 |
92 |
| Treatment Failed |
2 |
5 |
0 |
2 |
0 |
2 |
0 |
2 |
| Died |
12 |
22 |
18 |
12 |
8 |
9 |
7 |
2 |
| Lost to follow up |
212 |
206 |
239 |
249 |
271 |
222 |
115 |
214 |
| Transferred |
20 |
11 |
2 |
11 |
5 |
1 |
4 |
8 |
| MDR |
0 |
0 |
2 |
2 |
0 |
0 |
1 |
0 |
| Transferred out |
12 |
20 |
12 |
5 |
7 |
1 |
10 |
7 |
| Total treatment outcome |
771 |
871 |
914 |
788 |
722 |
639 |
549 |
476 |
Throughout these aggregated records it’s clear that PTB is the highest detected form of TB to be identified throughout these 8 years, being double or more that of EPTB, also within the PTB, bacteriologically confirmed PTB is the most prevalent type.
For bacteriologically confirmed PTB The highest number to be recorded was 936 in 2009, while the lowest being that of 2014 where only 526 cases were registered.
Unfortunately, a decrease in the total number of cured and treatment completed individuals is also evident, at the beginning, the numbers started to rise reaching their highest at 2009, but to plummet drastically throughout the following years.
Mortality rates however are low, only a small number of patients have died during the recorded period, 22 patients were recorded in 2008 which is the highest number to be recorded; in contrast, the least number is only 2 patients which were recorded in 2014.
Treatment success which is the addition of cured and treatment completed individuals is an important indicator for NTP success. TSR is an indicator of the performance of national tuberculosis control program. In addition to the obvious benefit to individual patients, successful treatment of infectious cases of TB is essential to prevent the spread of the infection. Detecting and successfully treating a large proportion of TB cases should have an immediate impact on TB prevalence and mortality. By reducing transmission, successfully treating the majority of cases will also affect, with some delay, the incidence of disease [6].
TSR records were rising in the first 3 years, reaching 70% in the year 2009, eventually, these numbers decreased reaching the lowest recorded percentage 51% in the year 2014.
Moreover, lost to follow up is the criteria which seems to be most problematic, since the beginning of the Libyan conflict numbers started rising, reaching the highest recorded percentage of 45% in the year 2014. In contrast to the first 3 years mentioned in the report, where the numbers remained somehow consistently below 28%.
Discussion
As the events of the Arab Spring unfolded in Libya in February 2011, it has led to an ongoing war. The civil war's aftermath and proliferation of armed groups led to violence and instability across the country, which erupted into renewed civil war in 2014. Prior to the 2011, Libya had a functioning healthcare system that could fairly support its nation’s citizens. Post-2011, the complete division of the country into multiple governments left the healthcare system extremely underfunded [7].
Treatment success is an indicator of the performance of national tuberculosis control program. In addition to the obvious benefit to individual patients, successful treatment of infectious cases of TB is essential to prevent the spread of the infection. Detecting and successfully treating a large proportion of TB cases should have an immediate impact on TB prevalence and mortality. By reducing transmission, successfully treating the majority of cases will also affect, with some delay, the incidence of disease [6].
An issue that is quite visible in our annual report is the decrease in the number of TSR, adding to that there is an increase in patients that are registered positive but fail to return to follow up visits and complete their treatment course. There are certainly a number of reasons why patients are lost in our system, one key issue is interrupted anti-drug supply, however, some factors are associated with patients themselves, such as socioeconomic factors, dissatisfaction with health services, patient mobility, poor drug tolerability. Also a deficiency in the country’s health information system, has led to inappropriate sporadic recording especially in conflict areas.
These recent years there has been an increasing number of displaced individuals and refugees especially from sub-Saharan Africa in the country which pass through the country un route to Europe mainly through illegal immigration. The association between poverty and TB is well established. TB infection is transmitted more readily in the environmental conditions of poverty: overcrowding, inadequate ventilation and malnutrition [8]. These minorities have a high tendency for treatment failure and follow up interruption due to their displacement and unstable living conditions and poverty.
Furthermore, communication is an important factor; presence of a qualified TB health educator is necessary in all health facilities providing care to TB patients. Patients should have adequate information about treatment compliance, possible side effects of the drugs, and the effects of treatment interruption, such as possible physical complications, treatment failure, multidrug resistant TB and extensively drug resistant TB. Presence of TB health educators in our national program might be of value for increasing patient's knowledge and understanding of the disease nature and eventually increase compliance to treatment.
Additionally, health services quality must be assessed, TB providing centers with impaired infrastructure, lack of adequate staff members, might be a challenge in some TB program branches and may apprehend patients from using these services.
Conclusion
The Libyan health system like many other services in the country has been adversely affected by ongoing conflict and political unrest. The inadequate health information system, shortages of medical supplies and technology, loss of health staff, damage to infrastructure and lack of sufficient funds pose serious challenges to public health.
Unfortunately, over these past 8 years, the country has witnessed a decline in TB CNR, and a decrease in treatment success rate and increase in the number of patients who are lost to follow up. Measures must be taken to ensure that TB prevention, care and control services are developed, maintained and strengthened as specified in the WHO End TB Strategy, the Regional Strategic Plan and The Guide for TB Control in Complex Emergencies [9]. However, during the acute phase of complex emergencies, the priority must focus on ensuring the availability of efficient treatment services for TB patients, the interruption of drug supplies often results in irregular intake of the necessary medicines by patients. This leads to an increase in treatment failure, low cure rate, higher numbers of patients with relapse, and increased risk of developing drug- resistant TB [9].
Furthermore, government commitment plays a key role in the fight against TB, Political commitment begins with the government deciding to make TB control a high priority and a core activity of the primary health care network. To have an impact, political commitment must translate into policy formulation, resource mobilization and program implementation. Policymakers must draft and disseminate a national policy document that outlines the control strategy, followed by operational guidelines that describe the practical steps to implementation, including national and local plans. These guidelines explain how to integrate DOTS within a country’s existing general health services. Once this groundwork has been laid, financial resources and trained staff are needed to put the program into action.
Acknowledgment
I would like to express my deepest appreciation to all those who provided me the possibility to complete this research. First of all My gratitude extends to the general manager of the NCDC /Libya Professor Badereddin B. Annajar for his continues support for the national TB program in Libya.
Additionally, I am sincerely grateful to the director of the TB and Leprosy control administration, NTP/Libya Dr. Mohamed Alfurjani for his patience, advice and critical insight.
Also, gratitude is given to all the exceptional colleagues and healthcare workers in various branches of the NTP across the country, for their continuous data recording and reporting amid difficult conditions. My deepest gratitude to my family for their love and support.
Funding
The research was self-funded by the authors.
Authors’ Contributions
Mawaheb Shelli designed and conducted the study and analysis, Mohamed Alfurjani contributed in paper revision. Fatima Almhalhel aided in data entry and analysis. All authors read and agreed to the final manuscript.
24356
References
- NCDC Documentation and Information Center (2018) National Libyan estimated population (2006-2017), pp: 1-10.
- Adam A, Patricia B, Brian D, Alison E, Erik G, et al. (2018) Libya Revolt of 2011.
- WHO (2013) Definitions and reporting framework for tuberculosis, pp: 1-40.
- World Health Organization (2015) Regional office for the Eastern Mediterranean. Libya Health Profile 2015: 1-4.
- World Health Organization (2015) Tuberculosis control in complex emergencies. Regional officer for the Eastern Mediterranean 34: 1-39.