Ana-Maria Dumitrescu1, Anca Sava1*, Dana Mihaela Turliuc1, Andrei Ionut Cucu2, Roxana Sufaru1, Ioan Gotca3, Irena Cristina Grierosu1 and Serban Turliuc4
1Grigore T. Popa, University of Medicine and Pharmacy, Iași, Romania
2Prof. dr. N Oblu, Emergency Clinical Hospital, Iași, Romania
3Dr. Ghelerter, Mental Health Center, Iași, Romania
4Socola, Institute of Psychiatry, Iași, Romania
- *Corresponding Author:
- Anca Sava
Discipline of Anatomy and Embryology, Morphofunctional Department, “Grigore T. Popa” University of Medicine and Pharmacy, 16 Universitaţii Street, 700115 Iași, Romania
Tel: +40744303678
Fax: +40232301633
E-mail: dr_anca_sava@yahoo.com
Received Date: December 28, 2020; Accepted Date: January 11, 2021; Published Date: January 15, 2021
Citation: Dumitrescu AM, Sava A, Turliuc DM, Cucu AI, Sufaru R, et al. (2021) An Autopsic Study on Bilateral Hypoplasia of the Posterior Communicating Arteries in Cerebrovascular Diseases. Health Sci J. 15 No. 1: 784.
Keywords
Posterior communicating artery; Bilateral hypoplasia; Autopsy
Introduction
Circle of Willis (CW) or circulus anteriosus cerebriis an anastomotic arterial structure located at the base of the brain, around the optic chiasm and other structures of the interpeduncular fossa.
The posterior communicating artery (PcoA) has its origin in the intradural part of the internal carotid artery (ICA), below the point of emergence of the anterior choroidal artery and it follows a posterolateral path, above the oculomotor nerve, to join the posterior cerebral artery, which is a branch of the basilar trunk. PCoA serves as an anastomotic channel between the anterior and posterior cerebral circulation as it extends posteriorly and join the primary segment of the ipsilateral Posterior Cerebral Artery, thus completing the circle of Willis. In its path, PCoA sends branches that irrigate the optic tract, optic chiasm, posterior hypothalamus, the pituitary stalk, the anterior and ventral nuclei of the thalamus [1].
Therefore, this artery provides a major blood supply to the ipsilateral cerebral hemisphere if there is a hypoplasia or an obstruction of the ICA, basilar artery or vertebral arteries.
On the other hand, occlusion, aplasia, or hypoplasia of the ACoP can significantly compromise brain irrigation, which can lead to the development of a stroke.
In the literature, autopsic reports of hypoplastic PCoAs are quite rare, but articles with bilateral hypoplasias are even rarer, either as isolated cases [2] or as a number of cases included in a large series of anatomical variants of CW [3]. So far, only 24 studies have been published. However, there are articles on this issue, but they were realized as angiographic studies [4].
The aim of our research was to identify the clinical consequences of bilateral hypoplasia of the posterior communicating arteries (PCoAs) in order to provide a clue to neurosurgeons and neurologists in their work to diagnose and treat patients with stroke symptoms.
Materials and Methods
This research was done in the Department of Pathology, "Prof. dr. N. Oblu” Emergency Clinical Hospital, Iasi, Romania, mentioning the fact that this represents the main neurological and neuro-surgical healthcare Centre in the region of north-eastern Romania.
The study was started by undertaking the institutional ethical approval. We performed an anatomical retrospective study on gross morphology of 98 circles of Willis that were identified at the time of the autopsies, which were performed at the request of the attending physician to establish the diagnosis of death in patients who died in same hospital in a three years period (January 1, 2013-December 31, 2015). At the time of the each autopsy, the pathologist (AS) carefully separated CW from brain tissue for better view. The pathologist (AS), assisted by two neurosurgeons (DMT and AIC), made detailed morphological and morphometric analysis of each circle of Willis.All constituting arteries of the CW were observed, measuring the outer diameter that was and note in a autopsy register. Gross morphological variations of CW were photographed and later archived.
We included in this study only those circles of Willis with bilateral hypoplasia (less than 0.5mm in the outer diameter) of the posterior communicating arteries (PCoAs) [2] and without any other associated anatomical abnormalities. The circles of Willis that showed normal anatomy or other gross morphological variations were excluded from the study. Any vessel with an outer diameter less than 0.5 mm was considered hypoplastic.
We recorded from the register of the Pathology Department of the same hospital the following data: age and gender of each deceased patient, the outer diameters of both PCoAs (left and right) for each circle of Willis, which were measured with a ruler and recorded during the autopsy by the pathologist, but also the medical cause of the death for these patients. All demographical data and autopsic findings were recorded in the patient data sheet.
Results
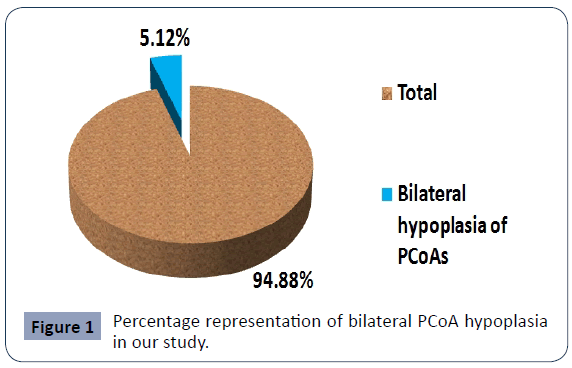
Of the 98 deceased who were autopsied in the hospital Prosecutor's Office during the three years studied period, only in 5 cases (5.12%) we identified bilateral hypoplasia of the PCoAs (Figure 1).
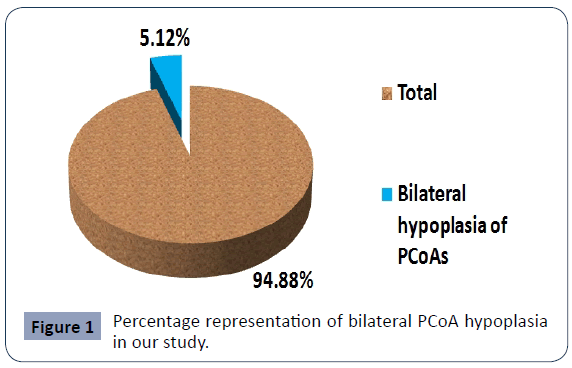
Figure 1 Percentage representation of bilateral PCoA hypoplasia in our study.
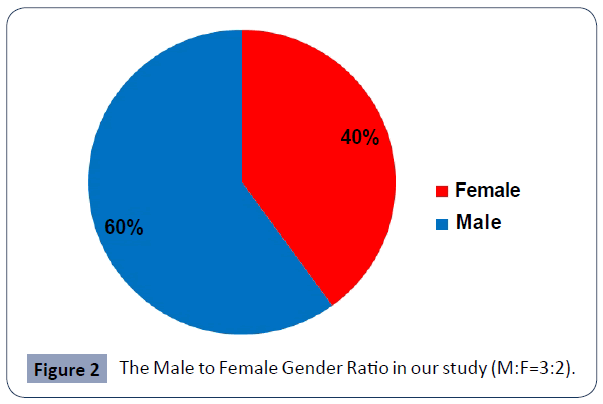
Of these 5 cases, three were male and two were female (Male- Female Ratio=3:2) (Figure 2). The average age of the deceased patients that were included in our study was 63.5 years.
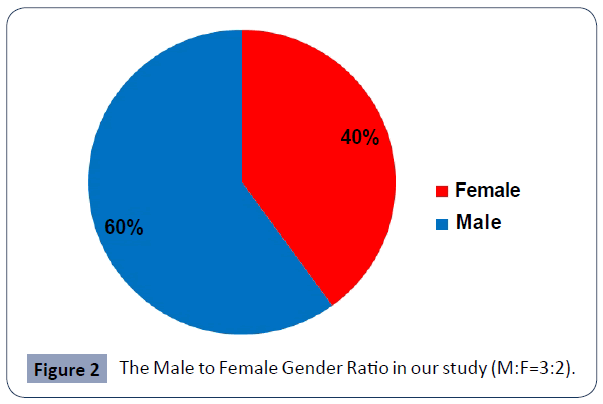
Figure 2 The Male to Female Gender Ratio in our study (M:F=3:2)..
Table 1 highlights the variety of causes of death in bilateral hypoplasia/aplasia of PcoAs. Most of the cases (4/5 cases) revealed a stroke located either supratentorially, in the frontal or fronto-parietal area, or in the brainstem, and manifested as hematoma, hemorrhage or infarction. However, in each case, other causes of death were associated, such as hypertension or systemic atherosclerosis. Only one case died of non-neurological causes (Table 2).
| No. |
Gender/Age |
Right PCoA |
Left PCoA |
Medical Cause of Death |
| 1 |
M/50 |
Aplasia |
Hypoplasia |
Right fronto-parietal hemorrhagic infarction Oclusion of right ICA Systemic hypertension |
| 2 |
F/71 |
Hypoplasia |
Hypoplasia |
Ponto-mesencephalic hemorrhage Systemic atherosclerosis Arterial hypertension |
| 3 |
M/76 |
Hypoplasia |
Aplasia |
Left F hematoma Oclusion of left ICA Systemic atherosclerosis |
| 4. |
M/40 |
Hypoplasia |
Hypoplasia |
Bulbar and pontine infarction Oclusion of basilar trunk Arterial hypertension |
| 5 |
M/67 |
Hypoplasia |
Hypoplasia |
Acute myocardial infarction of the left ventricle |
PCoA=Posterior Communicating Artery; ICA=Internal Carotid Artery; F=Frontal; P=Parietal; T=Temporal; IV=intraventricular
Table 1 Demographic and morphological characteristics of our cases.
| Authors |
Country |
Material |
|
| Hypoplasia |
| Kapoor et al [9] |
India |
1000 brains |
13,2% |
| Sinha et al [10] |
India |
80 brains |
17% |
| Gunnal et al [8] |
India |
150 formalized brains |
27,33% |
| Siddiqi, Tahir and Lone [11] |
Pakistan |
51 fresh brains |
15,6% unilateral hypoplasia
7,8% bilateral hypoplasia |
| Macchi et al [12] |
Italia |
100 healthy patients |
21% |
| Pa?cal?u et al [13] |
Romania |
10 formalized brains with CW with anatomical variants |
41% |
| Our study |
Romania |
98 fresh brains |
5,12% (bilateral) |
Table 2 Comparison of the data obtained in our study with those from literature.
In two (40%) cases, we found a strokes in frontal lobe. In two (40%) cases, the cause of death was an ischemic stroke of the brain stem.
In only one case (20%), even in the presence of bilateral hypoplasia of PCoAs, the cause of death was non-neurological.
Discussions
Normal PCoA presents an external diameter of 1.00-1.5 mm and an average length of 1.33-1.36 cm, regardless of its origin [5].
The following anatomical variants of PCoA are described in the literature: 1). hypoplasia of one or both PcoAs (i.e. the outer diameter should be less than 0.5 mm, regardless of its length); 2). aplasia of one or both PcoAs (a complete or partial failure of the arteru to grow); 3). atresia of one or both PcoAs (i.e. the outer diameter should be less than 0.5 mmandlack of a vascular lumen),4). bilateral absence of PcoAs; 5). fenestration; 6). persistent fetal pattern [3,6-8].
In the studies published so far, there are not many reported variations of PCoAs. More over, there are very few studies on the proposed topic, usually as isolated case reports (Nagawa et al). There are also a few reports on large number of cases with hypoplasia of PcoA, bur usually they presented only the unilateral variant [3,8]. Only Gunnal et al, in India, analysing 170 human cadaveric CW, found numerous types of variations of PCoA in the form of its aplasia, unilateral or bilateral hypoplasia, fenestration, and persistent fetal pattern. From all this types of variants, unilateral and bilateral hypoplasia were identified in a quater of the cases [3].
However, all studies published until now, realized on autopsied brains or on cerebral angiographs, in Asia or Europe, showed that hypoplasia is the most common anatomical variation of PCoAs [9-13].
The reduction of the diameter of the PCoA is associated with reducing the required blood supply to the brain because the volume of blood flow is inversely proportional to the length of the artery and directly proportional to its diameter. Thus, the shorter and wider one of the PCoA, the more efficient the transmission of blood to the nervous tissue dependent of that artery will become. Conversely, the longer and narrower the lumen of one or both PCoAs, the weaker the irrigated area of the brain will be [2].
This fact explains the development of extensive stroke identified by us in bilateral hypoplasia of PCoA, especially if there is an associated systemic pathology as well as the occlusion of an important artery that ensures brain irrigation, such as ICA or basilar trunk.
Even if literature claims that PCoA hypoplasia becomes a risk factor for ischemic stroke only in the presence of ipsilateral ICA occlusion [14], in our study we found that aplasia of one of the two PCoAs associated with the hypoplasia of the controlateralPCoA causes ischemic stroke of the brainstem, revealing their role in ensuring posterior circulation in case of occlusion of the vertebro-basilar system, too.
Conclusions
We have found that the bilateral hypoplasia of the two Posterior Communicating Arteries led to a stroke, either haemorrhagic or ischemic, which ultimately caused death of that individual. Although bilateral hypoplasia of both Posterior Communicating Arteries may be asymptomatic and neurologically uncomplicated, in most cases this anatomical variant increases the risk of hemorrhagic or ischemic stroke and plays a significant role in planning neurosurgical interventions and in diagnoses of neurological diseases.
Disclosure of Conflicts of Interest
None
34940
References
- Liebeskind DS, Caplan LR (2008) Anatomy of intracranial arteries. In: Jong SK, Louis RC, Wong KSL(editors). Intracranial Atherosclerosis.
- Edith N, Mwaka ES, Sam K (2017) Bilateral Hypoplasia of the Posterior Communicating Artery: A Morphological Case Report. Anat Physiol 7:4.
- Gunnal SA, Farooqui MS, Wabale RN (2018) Anatomical Variability of the Posterior Communicating Artery. Asian J Neurosurg 13: 363-369.
- Bhanu SP, Pentyala S, Sankar DK (2020) Incidence of hypoplastic posterior communicating artery and fetal posterior cerebral artery in Andhra population of India: a retrospective 3-Tesla magnetic resonance angiographic study. Anat Cell Biol 53: 272-278.
- Hegedus K, Molnar L (1987) Anatomical patterns of hypoplastic posterior communicating arteries and their implications for cerebrovascular diseases. Eur Arch Psychiatry Clin Neurosci 236:241-246.
- Hemamalini KK, Saraswathi G (2016)Bilateral absence of posterior communicating arteries -a case report. Int J Sci Res 4.
- Rao MKG, Somayaji N, Ashwini LS, Sapna M (2014) Incomplete circle of Willis due to the bilateral abnormal origin of posterior cerebral arteries and bilateral absence of posterior communicating arteries. Saudi J Health Sci 3:40-42.
- Gunnal SA, Farooqui MS, Wabale RN (2014) Anatomical variations of the circulus arteriosus in cadaveric human brains. Neurol Res Int 2014: 687281.
- Kapoor K, Singh B, Dewan IJ (2008) Variations in the configuration of the circle of Willis. Anat SciInt 83:96-106.
- Sinha I, Ghosal AK, Basu R, Dutta I (2014)Variation in the pattern of circle of Willis in human brain – A morphological study and review. Al Ameen J Med Sci 7:13-19.
- Siddiqi H, Tahir M, Lone KP (2013) Variations in cerebral arterial circle of Willis in adult Pakistani population. J Coll Phys Surg Pak 23: 615-619.
- Macchi C, Catini C, Federico C, Gulisano M, Pacini P, et al. (1996) Magnetic resonance angiographic evaluation of circulus arteriosus cerebri (circle of Willis): a morphologic study in 100 human healthy subjects. Ital J Anat Embryol 101:115-123.
- Pascalau R, Padurean VA, Bartos D, Adrian B, Szabo BA (2019)The Geometry of the Circle of Willis Anatomical Variants as a Potential Cerebrovascular Risk Factor. Turk Neurosurg 29:151-158.
- Chuang YM, Liu CY, Pan PJ, Lin CP (2008) Posterior communicating artery hypoplasia as a risk factor for acute ischemic stroke in the absence of carotid artery occlusion. J Clin Neurosci 15:1376-1381.