Key words
Medication errors, contributing/etiologic/risk factors, nurses, nursing
Introduction
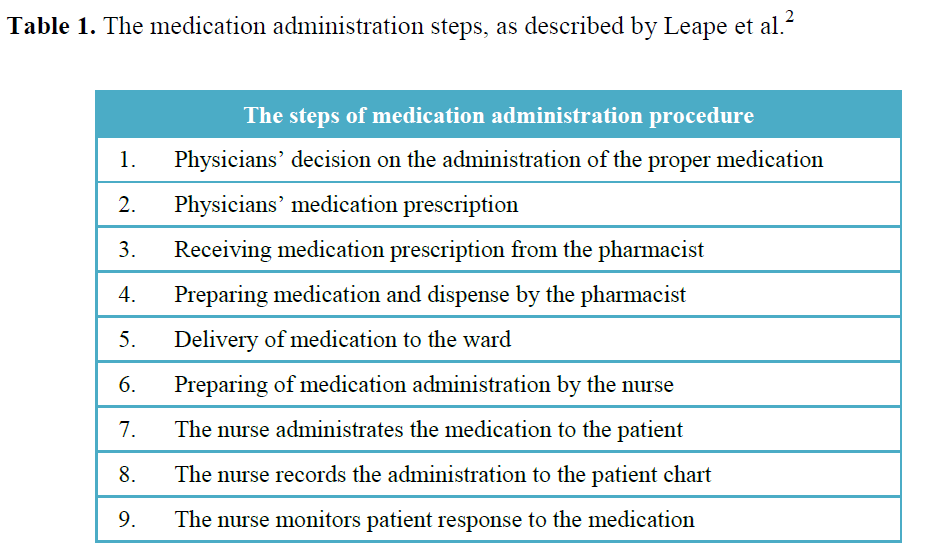
The implementation of medication process requires the cooperation of various healthcare professionals like physicians, pharmacists and nurses. The medication process starts with the physicians’ decision about the administration of the proper medicine to a patient and finishes with the medication administration to him/her and their monitoring of response to the medicine. Nurses participate in the latest steps of the medication process and are ultimately responsible for the medication administration to the patient. [1] The medication administration procedures’ steps, as described by Leape et al., [2] are presented in the Table 1.
As the United Kingdom’s Nursing and Midwifery Council underlines, medication administration requires scientific judgment, knowledge and skills application. [3] The time period spent by nurses on each shift to deal with themes related with medicines comes up to 40% of their working time. [4] Thus, it is more likely for front-line healthcare professionals of the medication process (nurses) to be blamed for when a medication error happened. Indeed, nurses are at the "sharp end" of this procedure. [5] It is useful to mention the medication error definition. A systematic review of 45 articles had been conducted to record the definitions of medication errors. Results from this study showed inconsistency in defining medication errors. Also, Lisby et al., [6] have defined the medication error according to their preferences and the needs of their research.
However, for the purpose of this study, a definition from the American National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) will be used:
"A medication error is any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the healthcare professional, patient, or consumer. Such events may be related to professional practice, healthcare products, procedures, and systems, including prescribing, order communication, product labeling, packaging, nomenclature, compounding, dispensing, distribution, administration, education, monitoring and use". [7]
A fundamental report to medication errors research area was reported by Kohn et al. [8] The authors in this report pointed out the significance of medical errors and also mentioned that medication errors in 1993 resulted in 7.391 deaths, compared to 2.876 deaths in 1983. In another report by the World Health Organization (WHO 2009) entitled "Improving medication safety", is reported that when medication errors happen, healthcare professionals should "look for all the contributing factors", making clear by this phrase that medication errors is a multifactorial problem. [9]
According to Evans [10] , there have been research efforts documenting the sources or the situations that medication errors took place. Once the etiology factors for medication errors have been identified and detected, the application of proper measures is essential for the error prevention and consequently the reduction of medication errors incidence by nurses. Certainly, since the healthcare field is under constant development (technological and pharmaceutical), medication errors remain a challenge.
This theoretical model of the "Swiss cheese" model describes the way that leads to the occurrence of an accident. In health, it has been firstly described by Reason in 1977 and it is not used only in the healthcare area, but also in other scientific areas. [11] The interpretation of this model has a symbolic-representative character. Each slice of cheese represents a defense, barrier or safeguard against error. Ideally all the defenses should be intact, but in reality the layers are full of holes. So, when an error passes through the defenses, perhaps it will stop in another defense (that means medication procedure) or it will go on, resulting in the increasing likelihood of the risk or the error or the accident. In the case of well designed health systems the error would rarely be able to pass through the defenses and cause harm. [12,13]
This is what happens in the healthcare system. The errors and the deficiencies are results of unsafe practices by humans that work in a healthcare system (e.g. the omission of re-check of the medication order by doctor), while latent conditions (like lack of communication between the primary care and secondary care services) are reflecting the faulty system structure or healthcare agency. [13]
Aim
The aim of the present review was to review the current literature related to the individual and the organizational factors that contribute to the occurrence of medication errors in clinical nursing practice.
Material and Method
A search of the relevant literature has been conducted in Pubmed electronic database, using the following search terms: medication errors, contributing/etiologic/risk factors, nurses, nursing. Studies that were taken into account were having the following inclusion criteria: published in English the period between January 1990-December 2012, with free full text provision, original research articles (qualitative, quantitative or mixed methodological design), using in the study sample nursing students or/and nurses working primarily in hospital settings, examined purely the spectrum of the contributing factors to medication errors or this theme was a part of their research study (i.e. examined also other factors; reporting and preventive strategies of medication errors). In line with these criteria, the studies that focused to the contribution of an individual factor to medication errors were not examined. References from the studies were assessed also and were taken into account if they met the inclusion criteria.
A total number of 45 articles was identified. After assessing the retrieved titles and abstracts, were rejected: 11 articles that were not original research papers, 24 articles were irrelevant and 10 were potential relevant with the aim of the present review. From the potential relevant articles, three articles’ full text provision was not given. From the rest papers (7), their full text was found. After the full text assessing only 3 were included. Also, additional sources (10) were emerged from secondary search through the evaluation of studies’ references found initially.
Results
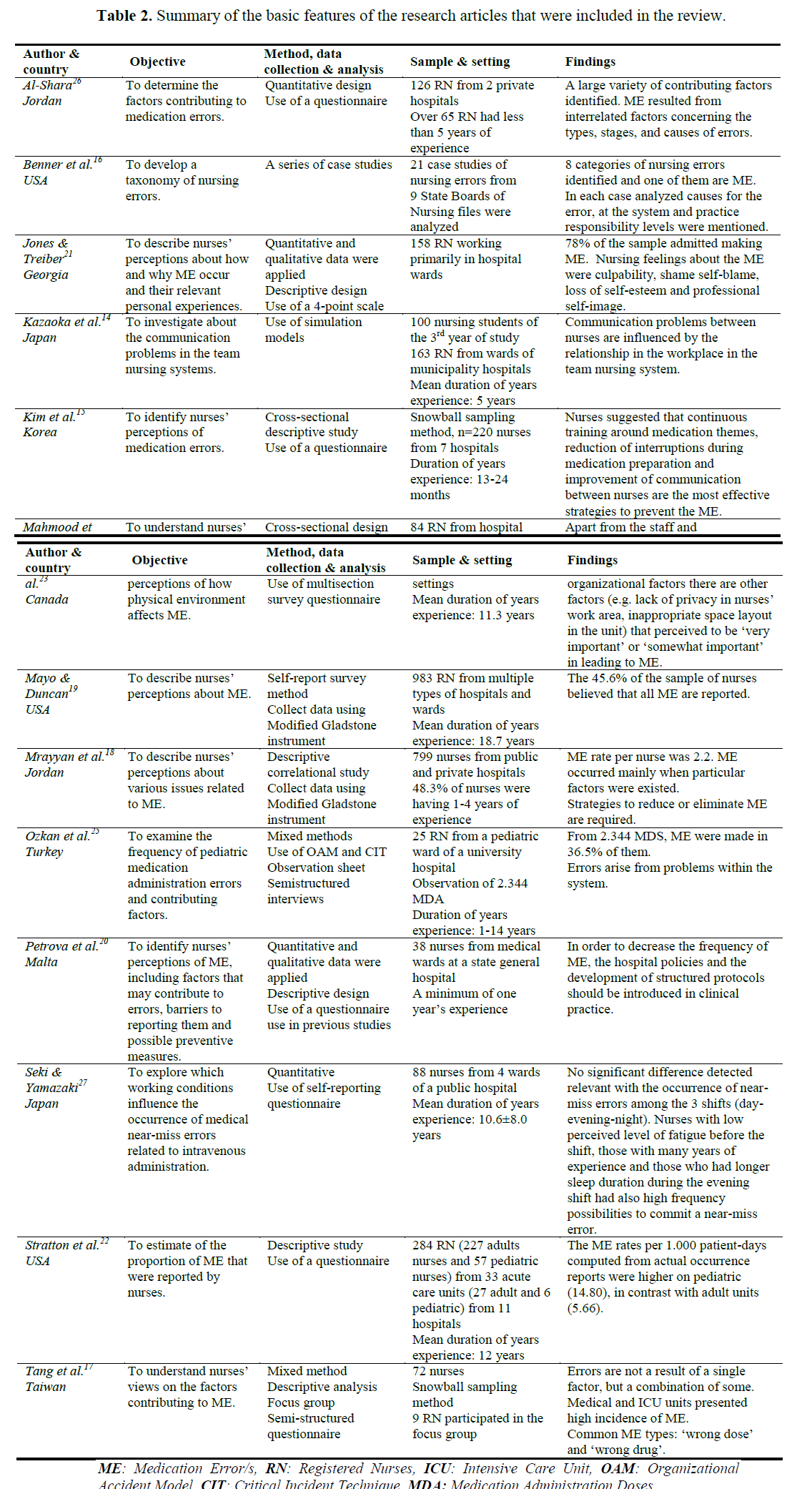
Thirteen research studies were found to meet the inclusion criteria. Table 2, outlines the basic features of the research articles that were included in the review. Three studies originated from USA, 2 from Japan and Jordan, and one from Taiwan, Malta, Turkey, Korea, Georgia and Canada respectively. The methodological approaches used by researchers were quantitative [15,18,19,22,23,26,27] or mixed. [17,20,21,25] A research paper describing a series of case studies and another one in which have been applied simulation models, were concluded in the present review. [14,16] The size of nurses’ sample participated in the studies was varying from 25 to 158 [16,17,20,21,23,25-27] and 159-284. [14,15,22] Two studies used large sample of nurses (79918 and 98319).
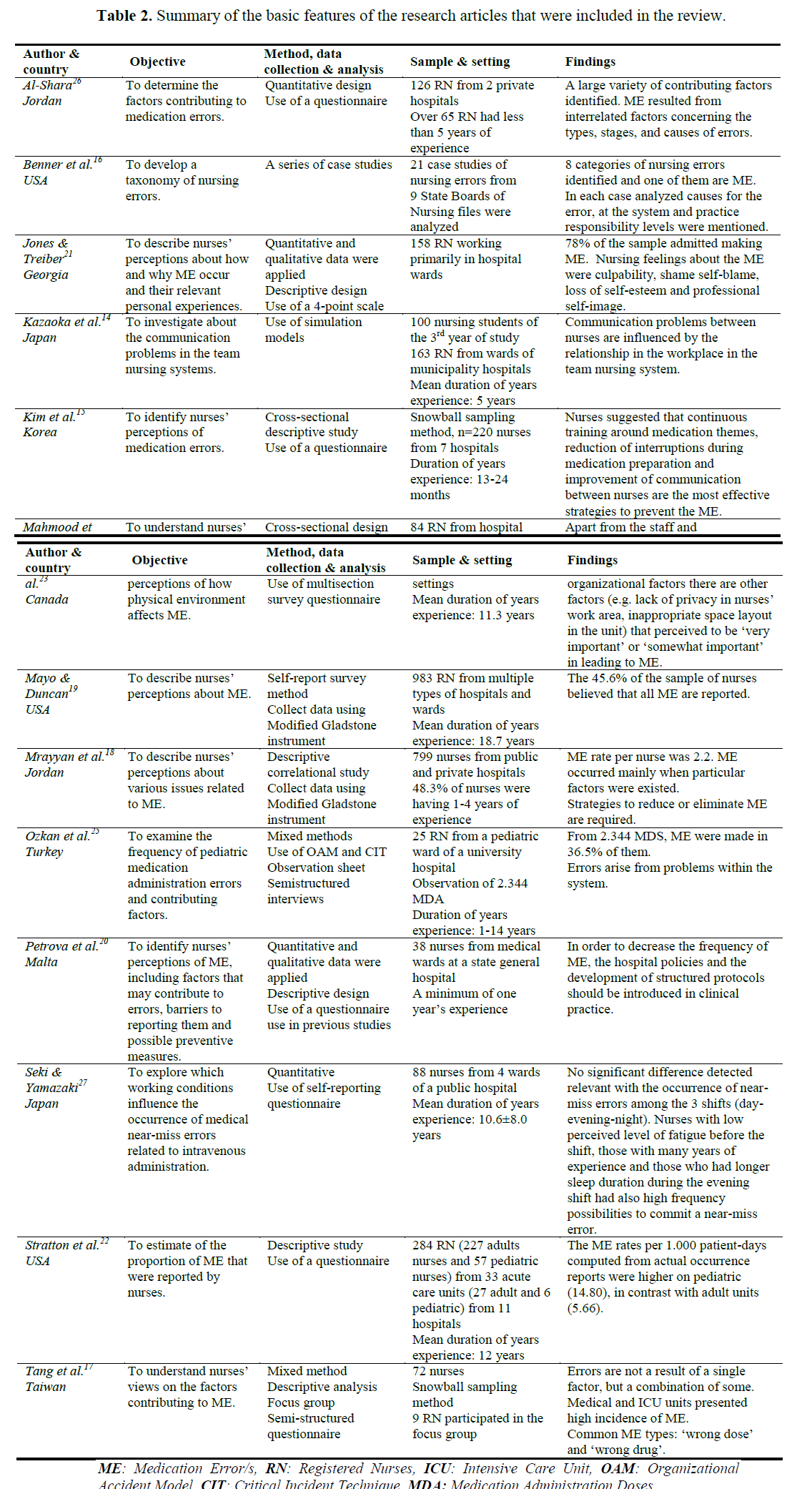
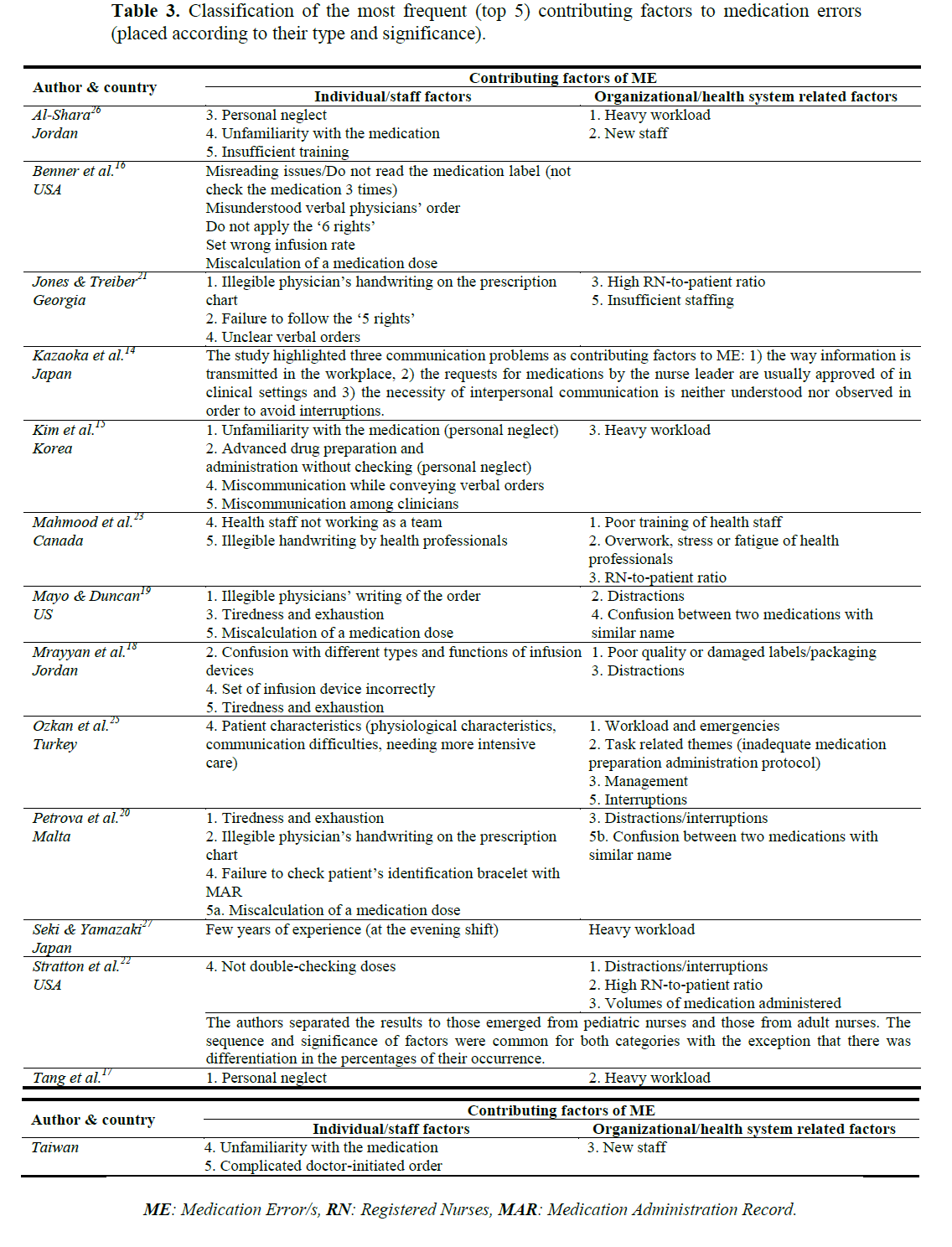
Table 3, presents a taxonomy between the most frequent (top five) contributing factors to medication errors, labeled as individual or organizational factors. By retrieving data from up to date nursing literature, the existing review article points out which individual and organizational factors may be responsible for medication errors’ occurrence. It is evident that both individual and organizational factors contribute almost the same to the medication errors occurrence. Worth mentioning is that in the present review (Table 3) individual outnumbered organizational factors. Furthermore, findings of previous literature reviews support that medication errors are a result of both categories’ factors, whereas other emphasized the contribution of health systems’ related factors. [29-31]
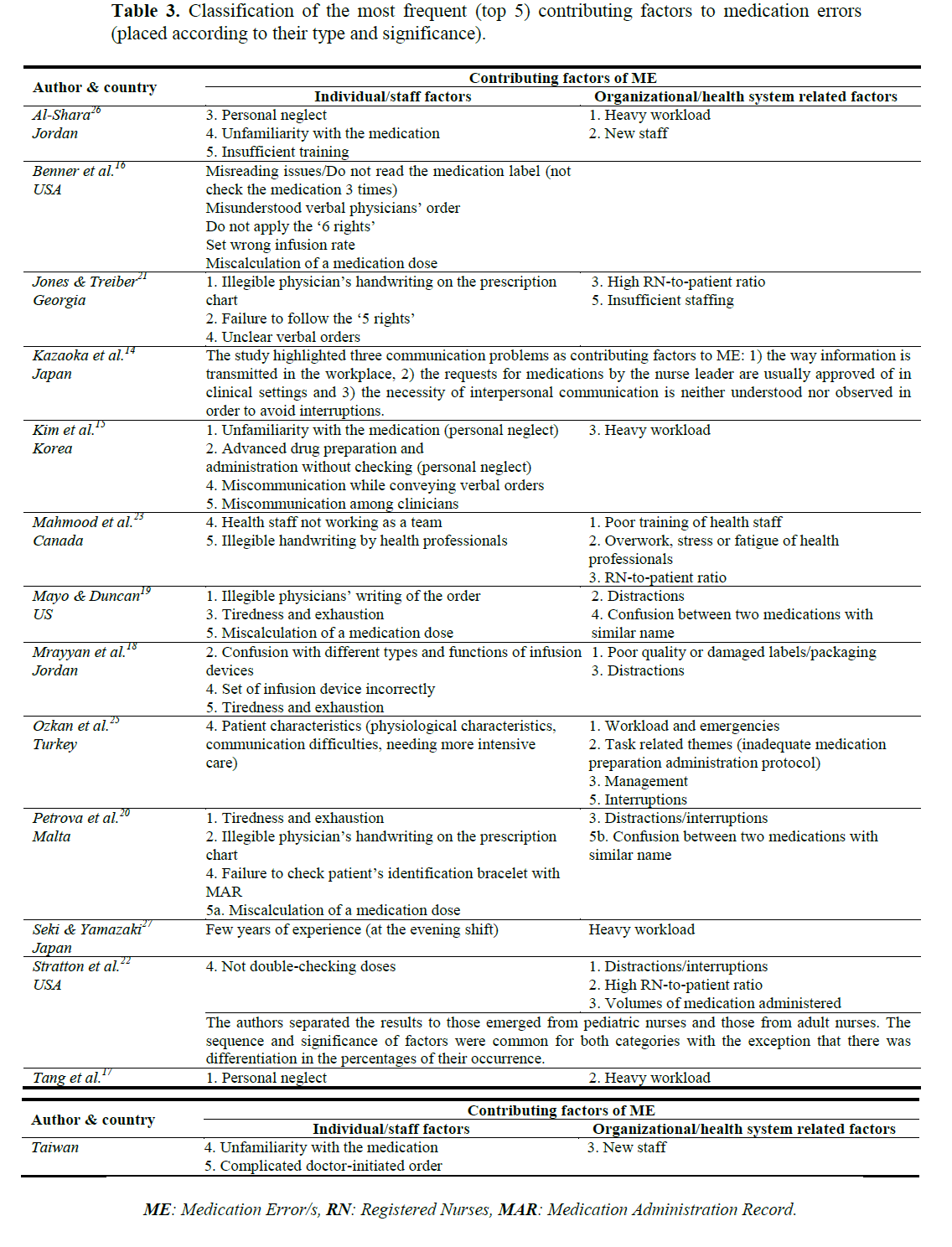
Individual factors
Humans are fallible and errors inevitable. Two issues are always topical and should not be ignored: even the best people are error prone and errors fall into concurrent patterns. [13] Doing errors is part of human nature, but so is the finding of ways to face and limit medication errors.8 The category of this approach concentrates on the interpretation of individual nurses’ factors and their relationship with the medication error. Subcategories of these factors involve: miscommunication factors, medication package labeling misreading, medication dosology miscalculation, non-adherence of the proper steps of medication preparation (checking-rechecking, application of the five rights which includes the right patient, right drug, right route, right time, right dose), personal neglect, difficulties in using infusion devices, nurses’ physical exhaustion, and problems with physicians’ prescription (illegible handwriting, unclear verbal orders).
The explanation, confirmation and generally the communication among clinicians about medication administration details are important components of the medication procedure. [14,15] Also, nurses’ clinical experience is considered to play an important role in the adherence of every step for a successful medication administration. Kazaoka and colleagues [14] stated that miscommunication factors (such as no explanation between the nurse and the nurse manager about medication errors’ subjects) are responsible for the medication errors. Nurses who participated in the study (100 out of 163) and had <5 years of experience were characterized by a low level of awareness relevant with the explanation and confirmation of medication information. [14] Miscommunication, however, can appear not only between nurses, but among clinicians in general. [15]
Benner et al., [16] examined 21 cases of nursing errors and their taxonomy revealed 8 categories, with medication errors among them. The fact that in 8 out of 21 patients’ cases died as a direct result of medication errors is important. The authors did not rank the risk factor of medication errors. A few causes of medication errors were: failing to follow a step of the medication procedure, misunderstanding of verbal order by telephone and pharmacy error.
Three studies mentioned the variable "personal neglect" in top five contributing factors of medication errors. In the first study, a high percentage (86.1%) of nurses considers so. [17] In the second one, it was observed as the third factor of error causality. Concerning the third study, two items, this of "unfamiliarity with the medication" and "advanced medication preparation and administration without checking", fall under the category of personal neglect. Nurses ranked the above factor as the leading risk factors of medication error, receiving the first factor 45.5% and the second one 45%. [15]
Other factors related to medication issues were problems with the infusion devices, which emerged in two studies and miscalculation of the medication dose. [16,18-20] By being confused with different types and functions of the infusion devices or setting wrong infusion rate and not calculating medication dose precisely were factors considered as responsible for medication errors. Furthermore, non-adherence to the proper steps of the medication procedure, such as the failure to follow the "5 rights" and the checking-rechecking process, are also mentioned as potential risk factors. [21,22]
Another research study, which was conducted in Malta, investigated nurses’ perceptions about medication errors. Results of this study revealed that nurses (37% of the whole sample) considered the physical exhaustion/tiredness as the top source of medication errors. [20] Themes relevant with the good physical status (stress, fatigue) were also mentioned in a cross-sectional survey by Mahmood et al., [23] as a factor that may lead to medication error. In contrast, nurses having participated in a number of studies, believed that illegible handwriting of medication orders is responsible for medication error. [19,20,21,23] A USA nonprofit organization for safe medication use (Institute for Safe Medication Practices, ISMP) stated that unclear writing of prescriptions causes more than 150 million pharmacists calls to physicians for further information. [24]
Organization related factors
This type of approach offers an holistic view of the medication errors issue. It concentrates on the interpretation of a number of healthcare system factors (working environment and organizational factors), their relationship and interaction with the medication error. Subcategories of these factors include: interruptions/distractions, heavy workload, high nurse-patient ratio, new staff and medication related topics (poor labeling/packaging, similar names).
The clinical environment is characterized as busy and complex, where interruptions and distractions in workflow are constant. Various studies classified the factor "interruptions or distractions" in the top five factors contributing to medication errors. Interruptions and distractions occur when a nurse is performing an intervention and before finishing with it, another task arises. As a result, the duration of nursing tasks (scheduled and non-scheduled) increases and nurses have to manage many interventions simultaneously. [18-20,22,25]
Two studies attributed medication errors primarily to the factor "interruptions or distractions". [19,22] The sources of nurses’ distraction was other patients, coworkers or events on the unit. [19,20] Except for the events on the unit, similar sources of distractions found also in another Jordanian research study. [18] Qualitative data derived from the study of Stratton and colleagues [22] , which included adult and pediatric nurses population, found that both categories of them, considered the factor "interruptions or distractions" as the top factor of medication errors. Furthermore, in a Turkish study, interruptions were observed to cause medication calculation errors, because nurses’ attention was distracted in the preparation and administration phase of the entire medication process. [25]
Increased workload was observed in a series of studies, conducted in pediatric and other hospital settings. [15,17,23,25-27] Nurses usually are expected to fulfill many responsibilities and duties during their working shift, thus the possibility of medication errors’ occurrence is increased particularly when nursing staff shortage is dominant. Apart from the above factor, the authors found insufficient protocols regarding the working environment conditions and the late arrival of medication from pharmacy. [25] Besides the morning shift; increased workload can be observed usually in the afternoon shifts. While, another study assures that medication errors occurred usually in the day shift (43.3%) and the evening (29.7%), rather than the night one (27%). [17] The "increased workload" factor may be responsible for wrong dose medication errors. Heavy workload can be indirectly associated with medication errors, which means, that in conjunction with the busy environment, it can cause fatigue and distraction and then lead to a failure of a medication step e.g. checking-rechecking method. [15]
In a study is mentioned that the factor "increased workload" is obvious in the morning and the evening shift, when physicians give many orders and the number of nurses is decreased to 1/3 of that in the morning shift, respectively. [27] Moreover, it seems that the variables "high nurse-to-patient ratio" and "increased workload" have a similar relationship like that of cause and effect. Namely, high number of patients per nurse implies a severe consequence: when a ward is not sufficiently staffed with nurses the workload is rising. The factor "high patient to nurse ratio" was among the top three frequently contributing factors to medication errors. [21-23]
Working conditions (workload and lack of experience) influence the occurrence of medical near-miss errors related to intravenous medication in a study at a hospital in Japan. Also, the authors added that sufficient clinical experience could encourage nurses to detect errors before their occurrence. [27] Otherwise, new staff probably would miss the detect of "signs" that would lead to an error during the performance of medication procedures. [16] The factor "new staff" was emerged as medication etiology factor in two studies. [17,26] The "new staff" factor was concerning nurses that had been recently graduated or change working environment.
Among system factors the organizational and physical environmental variables should be taken into account. Physical environment variables, such as insufficient space for documentation for charting (78.6%) was perceived in leading to medication errors. In addition, staff and organizational variables include overwork and stress (70.2%). [23]
Discussion
Patient safety can be at risk anytime and by various factors. Medication errors are such a factor. Although, in whole, other health professionals (physicians, pharmacists) also participate in the medication process, nurses have an active role in the management of patients’ medication. The examination of medication errors in the clinical nursing practice is crucial, since serious patient harm is potential. Moreover, medication errors are a burden for the hospital organization and the health professionals as well. Besides, having already acknowledged the medication errors’ contributing factors, their prevention can be achieved by the implementation of relevant strategies against their occurrence. [18,28] Paparella et al., [32] proposed a combination of safety principles for the development of a medication safety plan, rather than only education measures or the composing of new policies.
The included studies stressed the significance of each category of factors. Understanding the role of both individual and organizational factors and disseminate which factors and the mode that contribute to medication errors are useful to raise nurses’ awareness and vigilance about medication errors. Although nurses participate in the steps of the medication process, they should always ensure that the previous steps have been performed correctly and finish the drug administration safely.
However, it is intriguing to ascertain the critical role of hospital management against medication errors. For example, nursing administration should foster the application of policies and guidelines during medication process, after careful assessing of the literature data, encourage medication error reporting and established a non-punitive working environment. [18] Another essential dimension for the head nurses is the determination of sufficient staffing levels in every shift (to face high RN-to-patient ratio and heavy workload) and the installation of periods of time, when medication preparation and administration are performed; during a shift that allow nurses to be concentrated in that procedures, in order to work effectively (to face interruptions). [15]
In addition, taking for granted that education is an integral part of nurses’ career and since the acknowledgement of the contributing factors to medication errors has been achieved in a several degree, it is imperative to implement respective educational strategies to impede errors’ appearance or enhance their proper management. [33] For instance, interventions with educational content deemed to be valuable. Namely, nurses can be educated and trained through lectures, projects, simulation methods, practice and other didactic measures in special medication errors’ fields (e.g. medication calculation skills, distractions/interruptions, etc) or even wider prevention issues. [34-36] Also, prevention–focused functions may contain the promptly detection of errors before they reach the patient, the analysis of cases and conditions that induce medication errors and render nurses vulnerable to commit medication errors. The ultimate goals of such interventions is nurses’ role improvement, making safer the medication process and thereby the delivery of care quality to the patients.
Conclusion
To reach a conclusion, nurses should always ensure for the best nursing care delivery to every patient and try to avoid any type of harm. Undoubtedly, medication errors put patients’ health in unnecessary risk. This literature review indicates that there are plenty of factors or situations, which "permit" medication errors to happen, derived from the hospital staff or the health system. In the end, the goal of medication errors elimination is difficult to be achieved; instead the reduction of their rate can be accomplished by giving the required attention to the risk factors and applying the suitable preventive measures.
Implications for further research
Jordan stated clearly that nurses should proceed in the direction of changes in the nursing field and expecting a little information emerged from research papers. [37] Since the assessment of the majority of the contributing factors to medication error had been done, the application of relevant measures is crucial. To prevent the occurrence of any medication error type, future interventional studies should target in the direction of testing strategies which might have an effect in the reduction of medication error incidence. [24,37] Additionally, when healthcare organizations promote adjustments in patient care procedures, the estimation of their impact (positive or negative) both for patients and the staff, is useful to be explored as well. [30] Another impetus for research is the examination of medication errors in various clinical settings. [1] .
2779
References
- Reid-Searl K, Moxham L, Walker S, Happell B. Shifting supervision: implications for safe administration of medication by nursing students. J ClinNurs 2008; 17(20): 2750-2757.
- Leape LL, Kabcenell A, Berwick DM &Roessner J. Institute for Health Care Improvement. Reducing Adverse Drug Events, Breakthrough Series Guide. Institute for Health Care Improvement, USA; 1998.
- Nmc-uk.org [homepage on the Internet] . UK, Nursing and Midwifery Council. Standards for Medicines Management. 2010. [cited 2013 December 2] . Available from: https://www.nmc-uk.org/Documents/NMC-Publications/NMC-Standards-for-medicines-management.pdf.
- Armitage G, Knapman H. Adverse events in drug administration: a literature review. J NursManag 2003; 11(2): 130-140.
- Nccmer.org [homepage on the Internet] . USA National Coordinating Council for Medication Error Reporting and Prevention. Reducing Medication Errors Associated with At-risk Behaviors by Healthcare Professionals. 2007. [cited 2012 June 22] . Available from: https://www.nccmerp.org/council/council2007-06-08.html.
- Lisby M, Nielsen LP, Brock B, Mainz J. How are medication errors defined? A systematic literature review of definitions and characteristics. Int J Qual Health Care 2010; 22(6): 507-518.
- Nccmer.org [homepage on the Internet] . USA National Coordinating Council for Medication Error Reporting and Prevention. The First Ten Years. 2005. [cited 2012 Jun 25] . Available from: https://www.nccmerp.org/pdf/reportFinal2005-11-29.pdf.
- Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Committee on Quality of Healthcare in America. Washington, DC: National Academy Press; 2000.
- Who.int [homepage on the Internet] . World Health Organisation (WHO) patient safety curriculum guide for medicals schools. Topic 11. Improving medication safety. [updated 2009, cited 2012 Jul 5] Available from: https://www.who.int/patientsafety/education/curriculum/who_mc_topic-11.pdf.
- Evans J. Prevalence, risk factors, consequences and strategies for reducing medication errors in Australian hospitals: a literature review. Contemp Nurse 2009; 31(2): 176-189.
- Reason, J. Managing the Risks of Organisational Accidents. Ashgate. Aldershot; 1997.
- Department of health.gov [homepage on the Internet] . Department of Health-UK. 2004. Building a safer NHS for patients: Improving Medication Safety. A report by the Chief Pharmaceutical Officer. [updated 2004, cited 2012 Jul 5] Available from: https://www.dh.gov.uk/en/Publicationsandstatistics/Publications/nPublicationsPolicyAndGuidance/DH_4071443.
- Department of health.gov [homepage on the Internet] . Department of Health-UK. An organisation with a memory. Report of an expert group on learning from adverse events in the NHS. [updated 2000, cited 2012 Jul 7] Available from: https://www.dh.gov.uk/en/Publicationsandstatistics/Publications/nPublicationsPolicyAndGuidance/DH_4065083.
- Kazaoka T, Ohtsuka K, Ueno K, Mori M. Why nurses make medication errors: a simulation study. Nurse Educ Today 2007; 27(4): 312-317.
- Kim KS, Kwon SH, Kim JA, Cho S. Nurses' perceptions of medication errors and their contributing factors in South Korea. J NursManag 2011; 19(3): 346-353.
- Benner P, Sheets V, Uris P, Malloch K, Schwed K, Jamison D. Individual, practice, and system causes of errors in nursing: a taxonomy. J NursAdm 2002; 32(10): 509-523.
- Tang FI, Sheu SJ, Yu S, Wei IL, Chen CH. Nurses relate the contributing factors involved in medication errors. J ClinNurs 2007; 16(3): 447-457.
- Mrayyan MT, Shishani K, Al-Faouri I. Rate, causes and reporting of medication errors in Jordan: nurses' perspectives. J NursManag 2007; 15(6): 659-670.
- Mayo AM, Duncan D. Nurse perceptions of medication errors: what we need to know for patient safety. J Nurs Care Qual 2004; 19(3): 209-217.
- Petrova E. Nurses' perceptions of medication errors in Malta. Nurs Stand 2010; 24(33): 41-48.
- Jones JH, Treiber L. When the 5 rights go wrong: medication errors from the nursing perspective. J Nurs Care Qual 2010; 25(3): 240-247.
- Stratton KM, Blegen MA, Pepper G, Vaughn T. Reporting of medication errors by pediatric nurses. J PediatrNurs 2004; 19(6): 385-392.
- Mahmood A, Chaudhury H, Valente M. Nurses' perceptions of how physical environment affects medication errors in acute care settings. ApplNurs Res 2011; 24(4): 229-237.
- Ismp.org [homepage on the Internet] . Insitute for safe medication practices (ISMP). A call to action: Eliminate handwritten prescriptions within 3 years. Electronic prescribing can reduce medication errors first in a series of white papers from the Institute for Safe Medication Practices. [updated 2000, cited 2012 Jul 9] Available from: https://www.ismp.org/newsletters/acutecare/articles/whitepaper.asp.
- Ozkan S, Kocaman G, Ozturk C, Seren S. Frequency of pediatric medication administration errors and contributing factors. J Nurs Care Qual 2011; 26(2): 136-143.
- Al-Shara M. Factors contributing to medication errors in Jordan: a nursing perspective. Iran J Nurs Midwifery Res 2011; 16(2): 158-161.
- Seki Y, Yamazaki Y. Effects of working conditions on intravenous medication errors in a Japanese hospital. J NursManag 2006; 14(2): 128-139.
- Choo J, Hutchinson A, Bucknall T. Nurses' role in medication safety. J NursManag 2010; 18(7): 853-861.
- Brady AM, Malone AM, Fleming S. A literature review of the individual and systems factors that contribute to medication errors in nursing practice. J NursManag 2009; 17(6): 679-697.
- Pape TM. Searching for the final answer: factors contributing to medication administration errors. J ContinEducNurs 2001; 32(4): 152-160.
- McBride-Henry K, Foureur M. Medication administration errors: understanding the issues. Aust J AdvNurs 2006; 23(3): 33-41.
- Paparella S. Choosing the right strategy for medication error prevention?Part II. J EmergNurs 2008; 34(3): 238-240.
- Cleary-Holdforth J, Leufer T. The strategic role of education in the prevention of medication errors in nursing: part 2. Nurse EducPract 2013; 13(3): 217-220.
- Paparella SF, Mariani BA, Layton K, Carpenter AM. Patient safety simulation: learning about safety never seemed more fun. J Nurses Staff Dev 2004; 20(6): 247-252.
- Blank FS, Tobin J, Macomber S, Jaouen M, Dinoia M, Visintainer P. A "back to basics" approach to reduce ED medication errors. J EmergNurs 2011; 37(2): 141-147.
- Sherriff K, Burston S, Wallis M. Effectiveness of a computer based medication calculation education and testing programme for nurses. Nurse Educ Today 2012; 32(1): 46-51.
- Jordan S. Signposting the causes of medication errors. IntNurs Rev 2011; 58(1): 45-46.