Keywords
Blood donation; Knowledge; Attitude; Practice
Introduction
Blood is a body fluid in animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells. Blood transfusion is the injection of a volume of blood obtained from a healthy person (a donor) in to the circulation of the patient (the recipient) whose blood is deficient in quantity or quality through accident or disease [1]. There is shortage of active blood donors to meet the increased demands of blood in addition to limited supply, the issue of safety especially with regard to the risk of transfusion transmissible infection is also an issue of most concern especially in the developing countries [2].
Globally total safe blood supply is obtained from blood donors i.e., voluntary donors, replacement donors and paid donors. Voluntary non remunerated blood donors is a person who gives blood and receive no payment for it either in cash or in any kind that could a substitute for money. A replacement donor is also a non-remunerated donor who donates blood for a particular patient in an emergency. And are usually family members, colleagues or friends of concerned patient. Paid or professional donors received momentary payment for blood donation [3].
Blood transfusion is a vital component of the health care delivery system of every country. Though it is often delegated to a non-governmental organization, it is the responsibility of government to ensure adequate, safe supplies of blood, blood products and services to meet the needs of all patients in a timely, cost effective and efficient manner. Donor blood procurement from voluntary non remunerated donor has been considered the safest source of blood [4]. The demand for blood and blood products in most countries continues to increase because of the rise in human life expectancy and the implementation of new and aggressive surgical and therapeutic methods requiring large quantities of blood and blood products [5,6]. Blood can save millions of life, and voluntary donors are the only source of a safe blood supply in the world. Many efforts have been done to achieve this reality, however, both developed and developing countries have problems with the non-remunerated blood donation system [7]. World Health Organization (WHO) has adopted a policy aimed at 100% voluntary non-remunerated donor blood procurement by the year 2020 [8-10]. According to report of Namibian national blood policy in 2011 about 107 million blood donations are collected worldwide almost half of them are collected in high income countries from 15% of world population. There is marked difference in the level of access to safe blood between high and low income countries [8]. Various researches indicate that among the different types of blood donors the safest blood comes from voluntary blood donors that donate blood purely out of altruism. In Ethiopia, however, largest proportion (76.6%) of blood is obtained by hospital based replacement donation [9].
It has been estimated that 67% of men and 55% of women are eligible to give blood in the US, only 8% actually donate in any given year. Moreover, most blood is given by a relatively small number of repeat donors. This shortage has undoubtedly become more alarming amidst the transfusion- related tragedies and scandals associated with the AIDS pandemic. Consequently, there is a need to recruit and retain more blood donors [7]. Study done among university students in Bangladesh shows only 16% of respondents donate blood voluntarily [10]. This is also true for study among tertiary institution in Nigeria in which less than 2/3 of total respondents had good knowledge of blood donation, however 85% of them had never donated blood. Annual national blood demand is about 60,000-80,000 units [11].
Annual blood collection at a national level in Ethiopia is only 43% (of which 8.84% collected from voluntary nonremunerated in the Ethiopian contexts’, and achievements so far relating to blood safety, voluntary blood donation and its impact on maternal survival were discussed with members of the media present at the world blood donor day conference on 14 June 2014. It was underscored that ensuring available of safe blood at all health facilities would contribute to meet MDG 5 relating to the redaction of maternal death by ensuring that the lives of expecting mothers will not be endangered in case of emergencies for lack of blood for life saving transfusion. Although the country needs 200,000 units of blood annually, the National Blood bank of Ethiopia disclosed. The shortage has put a huge strain on caring for patients in desperate need of blood transfusions. The bank has managed to meet all its needs by gathering blood units from volunteers. However, 24 banks scattered across the country have not started operations with their full capacities, limiting the amount of blood donated [12]. So, substantial data regarding practice and their attitude of BD is relevant for policy makers and health care authorities to make decision towards it. It can be also used as source for those who are interested to conduct any further study. All the above facts along with the absence of any prior research in the study area make this study significant. So, this study aimed at to assess knowledge, attitude and practice of voluntary blood donation among residents of Aman sub-city.
Methods
The study was conducted in Aman town which is found in BMZ. It is 581 km from Addis Ababa. There are 3,455 households and17,714 total populations in the town. Among this 8,838 are males and 8876 are females. There is one teaching Hospital, 2 H/post, five private clinics and twelve pharmacies in the town. Community based descriptive cross sectional study was conducted from June 1-15/2015 G.C.
The source populations of the study were all the residents who lived in Aman town at least for 6 months. While the study populations was all the residents who lived in selected Keble of Aman. All residents who were in the age group between 18 and 65 years were included in this study whereas, residents with mental diseases and who had hearing and talking trouble were excluded. Knowledge was 98.9% whereas positive attitude and practice was 10%.
Sample was calculated by using single population proportion formula by using the following assumption. the prevalence of attitude ‘p’, 82% which is done in Addis Ababa , 95% confidence interval, 5%, and non-response rate of 10% which yields sample size of 250 [13]. After sample size was proportionally allotted for each Keble, we used systematic sampling technique to select the households. The K value was obtained by dividing total households of the Keble to proportionally allotted sample size. The questionnaire was adapted from related studies. The data collection instruments were first prepared in English and then translated to Amharic. To check consistency of the translation; back translation to English was done by another person. Then the questionnaire was pre-tested on 5% of the sample in a similar population with the same context. Based on the findings of the pretest, questions were modified. Data were collected using a structured questionnaire. Data collectors were five public heath graduate students. Training on interview techniques were given to data collectors for two consecutive days.
Data entry and cleaning were done using Epi Info version 3.5.1. Cleaned data were exported to SPSS Version 21 for analysis. Statistical analyses were done by univariate method .and the result finally presented by graph, table and summery note.
Operational definitions: - Ten questions were prepared to assess the knowledge of study participants regarding blood donation and they had categorized as following. Poor knowledge-an individual who could answer
Good knowledge- an individual who could answer 7-10 questions out of 10, whereas, the Attitude was assessed by six questions. Then those who had scored above the median were categorized as positive and those who scored below median as negative attitude. On the subject of to practice those who had history of blood donation in his /her lifetime is considered as she/he had practice of blood donation. Ethical clearance was sought from the Research Ethics Committee College of Health Sciences in Mizan-Tepi University. Oral informed consent was obtained from each study participant prior to data collection. Privacy of respondents and confidentiality of information were kept throughout the study.
Result
Among study subjects, 129(51.6%) of them were males. 180(72%) were married 46(18.4%) were single 17(6.8%) were divorced and 7(2.8%) were widowed. Most our study participants, 163(65%) were in the age range of 18-35 years followed by in 36-45 years range. Regarding to their ethnicity, 90(36%) were bench followed by kefa 67(26.8%) on the subject of to their occupation; 80(32%) were merchants (Table 1).
Table 1 Socio-demographic characteristics of respondents on blood donation in Aman sub city, southwest, Ethiopia, 2015.
| Variables |
Frequency |
Percent (%) |
| Age |
18-35 |
163 |
65.2 |
| 36-45 |
55 |
22 |
| 46-65 |
32 |
12.8 |
| Sex |
Males |
129 |
51.6 |
| Females |
121 |
48.4 |
| Ethnicity |
Bench |
90 |
36 |
| Kefa |
67 |
26.8 |
| Amhara |
59 |
23.6 |
| Oromo |
24 |
9.6 |
| Others |
10 |
4 |
| Religion |
Orthodox |
113 |
45.2 |
| Protestant |
107 |
42.8 |
| Muslim |
30 |
12 |
| Educational level |
No education |
42 |
16.8 |
| Primary |
75 |
30 |
| Secondary |
92 |
36.8 |
| Tertiary |
41 |
16.4 |
| Occupation |
Employer |
55 |
22 |
| Merchant |
80 |
32 |
| Farmers |
38 |
15.2 |
| House wife |
43 |
17.2 |
| Students |
34 |
13.6 |
Knowledge
Among the total respondents, 226(90.4%) knew about blood donation (BD); from those respondents 190(76%) had good knowledge, while, 35(14%) and 25(10%) had poor and fair knowledge respectively. regarding to, the source of information for BD, most of, 88(38.94%) had heard from mass media and followed by health professionals 63(27.87%). Most of the study participants 122(48.8%) knew the common blood group (BG). From those who know the common BGs only 117(46.8%) had known their BGs. Most of the respondents 194(88.9%) had said blood is taken from arm during BD (Table 2). Most of this study participants, 200(88.5%) said that screening should be done for donors before donation, some said contract for business and the rest didn’t know what things should be done. After donation most respondents 100(44.25%) said donors should be resuscitated and 86(38.05%) of the respondents said bed rest could be enough for donors while the rest said nothing and we didn’t know. Regarding to complications of BD; infection 90(39.8%), temporary weakness 22(9.74%) and being sick 16(7.08%) were the most common. Among those who mentioned infections as complication HIV/AIDS 132(52.8%), hepatitis 40(16%), and malaria 21(8.4%) were the commonest. Pertaining to the time of donation, Most 70(31%) of respondents thought that 3 months gap was enough to donate again, While, The rest supposed 2months and above could be enough.
Table 2 Shows the knowledge of respondent on blood donation in Aman sub city, southwest, Ethiopia, 2015.
| Variables |
Category |
Frequency |
Percent (%) |
| Do you know your blood groups? |
Yes |
A |
Males |
13 |
5.2 |
| Females |
9 |
3.6 |
| B |
Males |
9 |
3.6 |
| Females |
17 |
6.8 |
| AB |
Males |
12 |
4.8 |
| Females |
9 |
3.6 |
| O |
Males |
34 |
13.6 |
| Females |
13 |
5.2 |
| No |
Males |
21 |
8.4 |
| Females |
112 |
45 |
| Did you know BD |
Yes |
Males |
138 |
55.2 |
| Females |
88 |
35.2 |
| No |
Males |
7 |
2.8 |
| Females |
17 |
6.8 |
| Source of information about BD |
Mass media |
88 |
38.94 |
| Health professionals |
63 |
27.87 |
| Schools |
55 |
24.34 |
| Red cross |
17 |
7.5 |
| Different literatures |
3 |
1.33 |
| Blood is taken from |
Arm |
194 |
85.9 |
| Other sites |
9 |
3.99 |
| I didn’t know |
23 |
9.99 |
| Knowledge of the respondents about BD |
Good knowledge |
190 |
76 |
| Fairknowledge |
25 |
10 |
| Poor knowledge |
35 |
14 |
Attitude
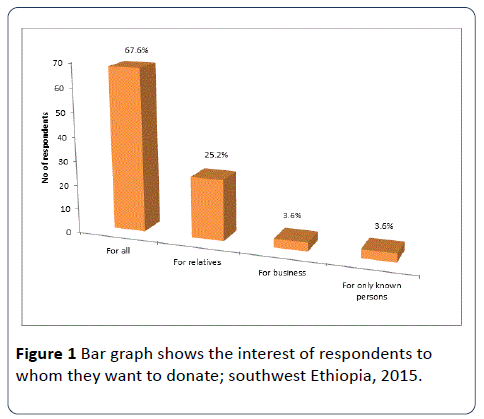
More than 2/3 of our respondents 222(93.8%) had positive attitude whereas, the rest had unfavorable attitude almost all, 220(90%) of respondents mentioned that volunteers Donors are source of blood donation, While, the rest said self-donors are the source. The reasons for those donors who were interested to donate only for relatives/friends and known persons were to save life 42(58.33%) and 28(38.9%) were frequently mentioned reasons. Most, 137(54.8%) of respondents believed patient relatives should be asked before donation, while, 113(45.2%) alleged shouldn’t be asked (Figure 1).
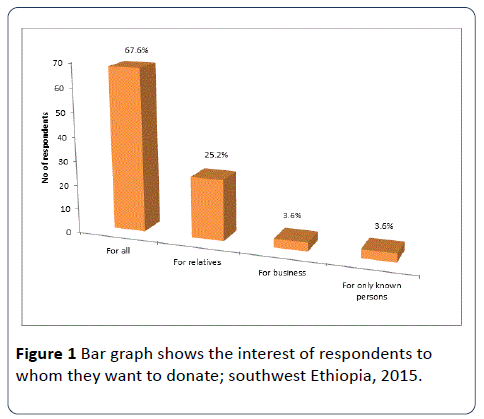
Figure 1: Bar graph shows the interest of respondents to whom they want to donate; southwest Ethiopia, 2015.
Practice
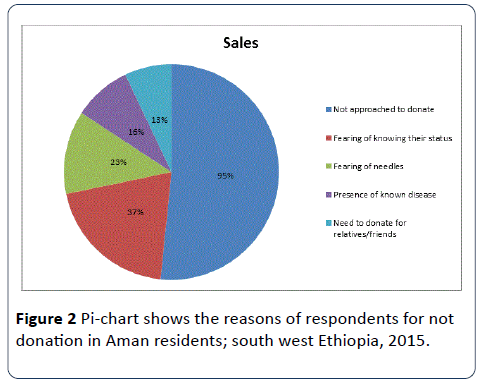
Even though most of the respondents have good knowledge and positive attitude only 66(26.4%) of study subjects have ever donated blood in their life time of these, 34(51.2%), and 30(45.5%) have donated blood 3 times and when needed in their life time respectively. The majority, 25(37.9%) of them donated for their relatives/friends as a replacement donor, while only 18(27.3%) donated voluntarily; the rest had donated for remuneration of which, 50(75.8%) of the respondents said that they could donate blood at any time, if they are called up to do so. However, 84(73.6%) of the respondents haven’t ever donated blood in their life time. Of which, 95(51.2%), 37(20.1%), and 23(11.4%) respondents didn’t donate blood due to not approached to donate, frustration of knowing their status during screening, and fearing of needles (Figure 2).
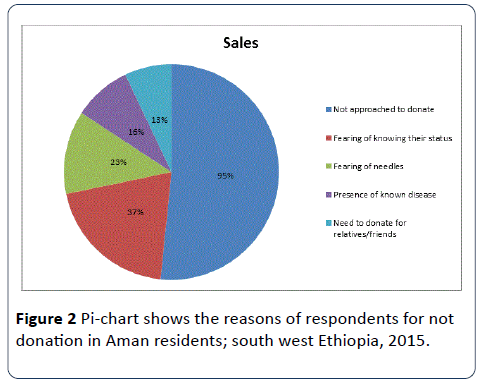
Figure 2: Pi-chart shows the reasons of respondents for not donation in Aman residents; south west Ethiopia, 2015.
Discussion
The findings of this study showed that, 190(76%) of the respondents had good knowledge, while the rest had poor and fair knowledge. This is in line with study done in Thai university students which showed 80% of the participants had good knowledge about blood donation [13]. However this is relatively higher than the findings of descriptive cross sectional study done in university of south India; that showed relatively high knowledge status as they had observed as good (42.7%), average (43.9%), and poor knowledge (13.4%) [14,15]. And less than descriptive study that was done in Addis Ababa which 98% of them had good and average knowledge [12]. It showed that male had better awareness than female. This is also true for study done in India in which (39.2%, 44.7%) good, (48.4%, 41.2%) average and (12.4%, 14%) had poor knowledge for male and female respectively.
Regarding the attitude, 212(93.8%) of our study participants had positive attitude toward blood donation. This is in line with the study done in Addis Ababa and Nigeria which is 81.6% [12,15] but, this was higher when compared with the study done in Chennai, India [7] which showed that 74% of respondents had positive perception regarding blood donation. In this study voluntary and replacement donation was accepted as the best source of blood donors by 220(90%) and 28(8.9%) respectively. This was comparable with the findings of the study that was done in Nigeria, which was 71.2% and 6.7% respectively.
The proportion of participants in the current study who practiced blood donation was 66(26.4%). This level was higher than the study held in Uttarakhand, India on KAP of people towards blood donation [16]. Even this was higher when compared with a cross sectional study on KAP of high school students in Addis Ababa, in which (10%) of the respondents donate blood [12,16]. The present study results also relatively higher when compared with study conducted in Sikkim India on behavioural disparities towards blood donation, in which 12.7% of the respondents donate blood [5,17]. This might be due to difference of awareness and attitude towards blood donation.
Among the donors in this study, 30(45.5%) of them donated for their relatives/friends as a replacement donor while only 18(27.3%) donated voluntarily; the rest had donated for remuneration and also 50(75.8%) of the respondents answered that they would donate at any time if they are called up to do so again. This result was lower than study conducted on KAP of voluntary blood donation among health care workers in which (41.7%) were voluntary, and (52.8%) donate to a friend or relatives in need of blood [15,18,19].
Around 2/3 and above of the respondents 184(73.6%) didn’t practiced BD; the reasons were not approached to donate 95(51.2%), fearing of knowing their status during screening 37(20.1%), fearing of needles 23(11.4%), presence of known disease 16(8.7%) and need to donate for relatives/friends for future 13(7.1%). These results were higher than the study conducted on KAP of voluntary blood donation among health care workers at the university of Benin city, Nigeria in which the reasons for non-donation by those who haven’t donated include nobody approached them for donation (25.2%), un fit to donate (16.5%), need to donate for a friend or relatives in future (19.7%), fear of needle (6.3%), fear of knowing their screening status (3.1%) [15,20]. This might be other reasons rather than being not approached to donate.
Conclusion and Recommendation
The study participants had good awareness about BD. Similarly, most of the respondents had positive attitude towards BD and accepted voluntary donation as the best source of donor. However, they had low practice of donation. Ministry of health and Red Cross association have to work in strengthen manner to improve the practice of blood donation. Health professionals shall disseminate information on BD by using local languages as blood donation is life saving charity with no harm. Zonal health office should have blood bank and encourage the community to donate blood.
Competing interests
We declare that we do not have any conflict of interests. This study was funded by Mizan-Tepi University.
Authors' contributions
Kebadnew MT, Addisu Y and Bezuayehu T conceived the study, involved in the study design, data analysis, drafting the manuscript and critically reviewing the manuscript. All authors read and approved the final manuscript.
Authors' information
KM is academicians and he has MPH in Epidemiology and Biostatics and all others are BSc in public health and they are working in health facility.
Acknowledgements
We are grateful to Mizan-Tepi University for funding the study and other supports. We would also like to express our deepest gratitude to data collectors and study participates for their hard work and sincere contribution.
18309
References
- Gillespie TW, Hillier CD (2002) Blood donors and factors impacting the blood donationdecision; national blood policy of Namibia. Transfuse Med Rev 16: 115-130.
- Maqbuole A, Bourhane E, Dine M (2003) Knowledge, attitude and practice regardingblood donation among Saudi population.Saudi Med J 25: 318-321.
- Giles M, Cairns E (1999) Blood donation and Ajzen’s theory of planned behaviour: an examination of perceived behavioral control. Br J Social Psycho Nigeria 34: 173-188.
- Shenga N, Pal R, Sengupta S (2008) Behavior disparities towards blood donation Sikkim, India. Asian J TransfusSci2: 56-60.
- Riley W, Schwei M, McCullough J (2007) The United States' potential blood donor pool: estimating the prevalence of donor-exclusion factors on the pool of potential donors.Transfusion 47: 1180-1188.
- Nwogoh B, Aigberadion U, NwannadiI K, Alexander A (2012) Knowledge, attitude and practice of voluntary blood donation among physicians in a tertiary health facility of a developing country. University of Benin Teaching Hospital, Benin City, Nigeria.
- https://apps.who.int/bloodsafety/transfusion_services/NBPolicyNamibiaApril09.pdf
- Uma S, Arun R, Arumugam P (2013)The knowledge, attitude and practice towards blood donation among voluntary blood donorsin Chennai, India. J ClinDiagn Res 7: 1043-1046.
- Hosain GM (1997) Knowledge, attitude and practice on blood donation among Dhaka university students in Bangladesh.East Afr Med J 74: 549-553.
- Shang B (2011) Knowledge, attitude and practice on blood donation among health science students in a university campus, South India.Int J Health Allied Sci 10: 1-3.
- Daniel N (2008) Willingness to voluntarily donate blood among high school students in Addis Ababa; Ethiopia.
- Woluannikit V (2000) A study on attitude towards blood donation among people in a rural district; in Thailand, Southeast Asia and Europe. Med Pub Health 609: 11.
- No Authors Lisyed(2010) Annual CMIS Bulletin by National AIDS Control Organization. Ministry of Health and Family Welfare. Government of India, New Delhi.
- Anju D, Atul S, Rahul C, Rajendra C, Sanjay G (2010) Knowledge, attitude and beliefs of people in North India regarding blood donation. Postgraduate Institute of Medical Sciences, Lucknow, India.
- Maharashtra K (2011) Toassess the knowledge of blood donation among voluntary blood donors at blood bank. Krishna Hospital Karad, Maharashtra, India.
- Amit A (2013) Knowledge, attitude and practices of people towards voluntary blood donation in Uttarakhand.Asian J TransfusSci 7: 59-62.
- Salaudeen A, Musa O, Awoyemi A, Bolarinwa A, Adegboye A, et al. (2012) Community survey on blood donation practices; Department of Epidemiology and Community Health, in northern state of Nigeria,University of Ilorin, Ilorin.
- Hossein S, Nasim P,Batool M (2013) University Students Awarenessand Attitude towards Blood Donation in Kerman City.
- Mousalvi F, Tavabi A,Golestan B, Ammar-Saeedi E, Kashani H, et al.(2011)Knowledge, attitude and practice towards blood donation in Iranian population. Transfuse Med 21: 308-317.