Abstract
Dependence on out-of-pocket payment (OPP) for healthcare may lead poor households to undertake catastrophic health expenditure; millions of people suffer and die because they do not have the money to pay for healthcare. Worldwide about 44 million households face financial problems due to healthcare expenditure; more than 40% of African nations’ health expenditure comes from out-of-pocket payments making a scarcity of funds for health, and lowincome groups make health payments by borrowing or selling property. Therefore, an agenda for developing a system of healthcare financing is common for all nations toward universal health coverage (UHC), using the emerging concept of community-based health insurance (CBHI) as a potential strategy to achieve universal health coverage in developing countries by discussing the problem of healthcare financing in low-income countries (LIC), helping to raise revenue, and narrowing the financial gaps of health sectors providing universal health coverage. Despite great efforts to improve accessibility to modern healthcare services in the past two decades, utilization of healthcare services in Ethiopia has remained very low. However, the functions of pooling funds and organizing them are critical for countries’ progress toward UHC.
Objective: This study aimed to assess willingness to pay, explore the mechanism of financial pooling for community-based health insurance, and identify factors associated with households in the Tigray Region, Northern Ethiopia, in 2020.
Method: A community-based, quantitative and qualitative cross-sectional study was conducted from September to October 2020 in Tigray, Ethiopia. The sample size was determined using a single population proportion formula. Multi-stage cluster sampling was used to select 845study participants and 10 KII and 4FGDs were selected using a purposive sampling technique. Data were collected using an interviewer-administered questionnaire that was managed and analyzed using Epi-data Version 3.5.1 and SPSS Version 21.Theinterview guide used Atlas-ti software for qualitative data.
Results: Based on 845 households surveyed, more than half of respondents, 483 (57.2%), were female. The majority of the respondents, 743(87.9%), knew the current premium and registration fee of community-based health insurance (CBHI), with more than 90 percent, 790(93.5%), planning to renew/enroll their membership in CBHI, with the mean premium per household head they were willing to pay being 396 ETB (SD=±216) and 310 ETB (SD=±115) per household annually for urban and rural, respectively. In addition, six out of ten (62%) urban dwellers and five out of ten (52%) rural dwellers wanted to pay an additional amount of money to the current governmental premium threshold (which is 240 ETB for rural and 350 ETB for urban).
Conclusion: Community-based health insurance is an effective means of increasing the utilization of healthcare services and providing a scheme for member households with a pool mechanism situated at the district level, enabling districts to own the scheme, a decentralized health system, and decentralized decisions, ensuring equity. To alleviate deficits and make CBHI increases in the annual premium and enrollment of the community to CBHI sustainable, budget subsidization by the government to reverse the ruin, increased community awareness, and continuing the current pooling mechanism at the district level, but establishing or revising a department at the health office that controls the process of CBHI, are recommended.
Keywords
Community-based health insurance; Healthcare utilization; Healthcare financing
universal health coverage; Financial pooling
Abbreviations
ANC: Ante-Natal Care; CBHI: Community-Based Health Insurance;
ETB: Ethiopian Birr; EPSA: Ethiopian Pharmaceutical Supply
Agency; FGD: Focus Group Discussion; HEP: Health Extension
Programme; HEW: Health Extension Workers; KII: Key Informant
Interview; LIC: Low Income Country; MOU: Memorandum of
Understanding ; OOP: Out of Pocket; OPP: Out of Pocket Payment;
SD: Standard Deviation; UHC: Universal Health Coverage; USD:United States Dollar; WIP: Willingness to Pay
Background
Globally, approximately 44 million households (more than
150 million people) face financial problems due to healthcare
expenditure [1]. In the majority of African countries, more than
40% of the total health expenditure is by out-of-pocket payment
(OPP), which results in a scarcity of funds for health [2]. More
than 90% of healthcare financing problems have been reported
in sub-Saharan African countries, where resources are limited
[3,4].The economic burden of direct payments worsens among
people in lower income groups because healthcare demands outof-
pocket payments by borrowing or selling property [5,6]. As
a result, developing healthcare financing systems is a common
agenda and key area for health system actions toward universal
health coverage (UHC) [3] for all countries [3,4-7]. Community-
Based Health Insurance (CBHI) is an emerging concept for
providing financial protection to healthcare financing problems
in low-income countries that involves the mobilization of
resources for the health sector (revenue raising),accumulation
and management of prepaid financial resources(pooling), and
allocation of pooled funds (purchasing) [3,8]. Among others,
South Korea, Ghana, and Rwanda are the best examples of lessons
learned from developing countries, while South Korea is often
cited as a success story for its rapid achievement of universal
health coverage through community-based health insurance
[1,3]. However, in most African countries, healthcare financing
covers almost exclusively the formal sector and achieves no more
than 10 percent of population coverage [3,9].
Pooling arrangements and their potential to contribute to
progress toward UHC have received much less attention.
However, the function of pooling and the different ways in which
countries organize this is critical for their progress toward UHC
[10,11]. According to evidence from [13], fragmentation in pooling
is a particular challenge for UHC objectives. Pools are fragmented
when barriers exist in the redistribution of prepaid funds. This results
inefficiency in the healthcare system, as it typically implies duplication
(or multiplication) in the number of agencies required to manage
pools (and, usually, purchasing as well) [11,12]. Low adhesion rates,
limited resource mobilization, and poor sustainability have been the
challenges to in effective implementation of the CBHI scheme in
some sub-Saharan African countries [9].
The government of Ethiopia has introduced community-based
health insurance (CBHI) as a strategy for reducing catastrophic
financial shocks in our country, and it has been piloted in 13 selected
districts in Amhara, Oromia, Southern Nations, Nationalities,
and Peoples (SNNP), and Tigray [11,12]. Community-based
health insurance benefit packages are available for all services in
health centers and hospitals, excluding tooth implantation and
eyeglasses, with a provider payment mechanism making an effort
to remove financial risk through the expansion of CBHI [14-16].
According to the Health Sector Financing Reform (HSFR) project
report, the overall enrollment was 48% [12]. However, evidence
has shown that utilization of the scheme was affected by different
socio demographic, economic, and health-related factors,
including the study region in Tigray, northern Ethiopia [12,13].
Understanding the CBHI pooling setup and the community’s
willingness to pay (WTP), determining the amount of money, and
exploring facilitators and barriers while implementing the scheme
are necessary for policy makers to redesign and reform options,
and to expand the program regionally. Therefore, the objective
of this study was to assess the CBHI pooling setup, WTP for CBHI,
and associated factors among rural and urban households in the
Tigray region of Northern Ethiopia.
Methods
A community-based, quantitative and qualitative cross-sectional
study design was employed from September 1 to October 20,
2020 in an urban-rural community of selected districts in Tigray
Region, which is located in northern Ethiopia, hosting seven zones
(one special zone), 93 districts (71 rural and 22 urban) with 814
kebeles (the smallest administrative unit) and a total projected
population of 6,960,000 (CSA 2007 census projected for 2015),
with 90% overall health service coverage of the region [15,16].
All urban-rural households in the districts that had (not yet)
established the CBHI scheme were the source population,
whereas the study population comprised sampled households in
the selected districts. Household heads that had lived for more
than six months in the kebele and who were ≥18 years of age
were included in the study. Respondents who were working in
the formal sector or unable to participate in the interview due
to health conditions were excluded from the study. Respondents
working as focal persons of CBHI in regional health bureaus,
district health offices, and health insurance agencies, zonal
coordinators, district and kebele administrators, representatives
of the kebele’s cabinet, and health extension workers were
eligible for the qualitative study.
The sample size was calculated using a single-population
proportion formula with the assumption of proportion of
willingness to pay (WTP) for CBHI (p=80%) in Fogera District,
Ethiopia [17] using the95% confidence interval (Z=1.96) and a 4%
margin of error. After considering a design effect of 2 and adding 10% for a potential non-response rate, the final sample size was
845 households. For the qualitative part, 10 KI and 4 FGD were
interviewed with key actors of health insurance representatives
at each selected district and kebele.
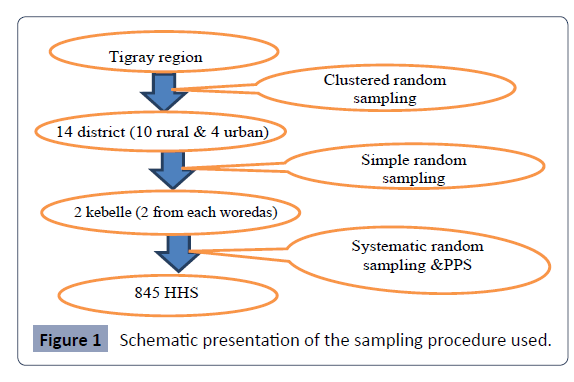
A multistage sampling technique was used to select the study
participants. To reach the final sample size, the first 14 districts
out of the seven zones were selected using cluster sampling and
then 2 kebeles from each district using simple random sampling,
and finally the households’ proportion to size was sampled using
systematic random sampling from each kebele. In the first stage
of sampling, 28 kebeles from 14 districts were randomly selected
from the region. In the second stage, households were selected
from these by systematic random sampling and probability
proportionate to size (PPS), for which a purposive sampling
technique was used.
The dependent variables are willingness to pay and the financial
pooling mechanism for CBHI. Willingness to pay means the
maximum (non-zero) amount that households are willing to
pay for the insurance scheme, elicited through a double-bound
contingent valuation method specifically by applying a bidding
game. Independent variables, such as socio demographic
characteristics (age, sex, marital status, educational status, family
size, religion, and ethnicity), economic factors (wealth index
and occupation), environmental factors (distance from health
institution in walking time), health and health-related factors
(health condition of illness, chronic illness and disability, medical
treatment for the recent episode, healthcare cost of the recent
treatment, perceived quality of the healthcare service in the
area), and knowledge-related factors(awareness of CBHI and
social trust) were independent variables in the study (Figure 1).
Figure 1: Schematic presentation of the sampling procedure used.
The wealth index questionnaire was adapted from the Ethiopian
Health Insurance Agency for the number and types of consumer
goods owned, housing characteristics, and availability of basic
amenities for residents. From these, scores were derived using
principal component analysis and classified into five quintiles.
Quantitative data were collected from selected CBHI members
and non-member households using pre-tested intervieweradministered
structured questionnaires adopted from other
studies conducted in similar areas. The survey questionnaires were
developed to elucidate information on the basic demographic
and socioeconomic characteristics of the households, incidence of illness, and subsequent choice of health providers, and the
amounts and sources of money used to finance healthcare
services for illness for themselves and family members. The survey
questionnaire was administered in Tigrgna, the working language
of the state which most study area residents adequately listened
to and spoke. Fifteen trained data collection teams were used for
data collection, and each team comprised three data collectors
and one field supervisor. Supervisors spot-checked the quality of
data collection and ensured the questionnaires were completed
daily. The qualitative study respondents purposively selected
included board members and general congress, the Agency of
CBHI, the Zonal Administration, the Woreda Health Office, the
Woreda Administration, and the Regional Health Bureau. Ten key
informant interviews were conducted in each woreda with four
focus group discussions, one in each of the selected woredas,
with eight participants in each group.
An effort was made to include participants with a range of
characteristics in order to obtain a broad representation of
CBHI management and budget administration. Data were
gathered using a prepared FGD guide that was introduced to
the participants, describing the objective of the study, and was
followed by open questions cantering on the CBHI and the sum
of money made available for the purpose of the scheme. Trained
moderators facilitated all FGDs, with discussion notes taken and
audio recordings made.
Contingent valuation was used to elicit WTP for oneself, for other
members of the household, and also for altruism (for poor and
impoverished people in the community) using only the bidding
game technique (Dong et al. 2005). Three iterations were used
in the bidding game depending on the answer to the starting
bid. The final response was a continuous quantitative amount
that indicated respondents’ maximum WTP. A brief introductory
explanation and scenario regarding health insurance was provided
to the respondents before determining their WTP for the scheme.
The concept of CBHI and its attributes were explained before
starting the bidding game.
Quantitative data were analyzed using Epi-data Version 3.5.1,
and SPSS Version 21. Frequencies and proportions were used
to describe categorical variables using cross-tabulation. Factors
associated with the outcome variable with P<0.20 in the bivariate
analysis were included in the multivariable logistic regression,
data from focus group discussions and KII were transcribed, and
responses were classified into general categories identified in the
discussion and interview guide using Atlas-ti software. A common
theme was identified, inferences were made from each theme,
and conclusions were drawn.
Ethical clearance was obtained from the IRB of the Tigray Health
Research Institute. Support letters were obtained from the
Tigray Regional Health Bureau, and Health Office permission was
obtained from the kebeles’ administration prior to conducting the
study. Written consent was obtained from the respondents prior
to the interview by explaining the purpose of the study as the IRB of
the THRI had already accepted and approved it. The confidentiality
of their information was assured using a coding system and by
removing any personal identifiers. Respondents’ right to refuse to
answer several or all of the questions was respected.
Results
Description of study participants
Of 845 sampled respondents, more than half, 483 (57.2%), were
female. A total of 810(95.9%) were Christian Orthodox, followed
by 35(4.1%) Muslim/Catholic; 840 (99.4%) were Tigrayan, the
majority of them, 607(72%), rural dwellers; and 267(31.6%) were
between the ages of 29 and 39 years. Among them, 581 (68.8%)
were married, followed by 116(13.7%) divorced/separated,
75(8.9%) single and 73(8.6%) widowed, respectively. More than
half of the respondents, 500(59.2%), had family size less than or
equal to five, whereas 345(40.8%) had family size greater than
five.
In total, 554 (65.6%) had two or more, 169 (20%) exactly one,
and 112 (14.4%) no family members of age 18 years or older
currently living with them. The majority of the respondents,
385 (45.6%), have no family members younger than 5 years
old, whereas 110 (13%) and 350 (41.4%) had two or more and
exactly one, respectively. Similarly, of the total respondents only
89 (10.5%) had one or more family member age 65 years and
older. Of the respondents, 440(52.1%) and 141(16.7%) were
farmers and daily laborers, respectively followed by merchants,
93 (11%), housewives, 89 (10.5%), and others, 82 (9.7%). Looking
at the educational background of respondents, 309 (36.6%), 135
(16%), 252 (29.8%), 139 (16.4%), and 10 (1.2%) were unable to
read and write, could read and write, had primary school, had
secondary school, and had college or above. In total, 329 (38.9%)
of the respondents’ wealth indices were below the median level
and are poor and poorest, whereas 342 (40.5%) were above the
median level and are rich and richest (Table 1).
| Characteristics |
Number |
Percentage |
| Sex of respondent |
|
|
| Male |
363 |
42.7 |
| Female |
482 |
57.3 |
| Age of respondents |
|
|
| <=29 years |
172 |
20.3 |
| 30-39 years |
267 |
31.6 |
| 40-49 years |
171 |
20.2 |
| 50-59 years |
112 |
13.3 |
| >=60 years |
123 |
14.6 |
| Religion |
|
|
| Orthodox |
810 |
95.9 |
| Muslim/Catholic |
35 |
4.1 |
| Ethnicity |
|
|
| Tigrain |
840 |
99.4 |
| Amhara |
5 |
0.6 |
| Marital status of respondents |
|
|
| Single |
75 |
8.9 |
| Married |
581 |
68.8 |
| Widowed |
73 |
8.6 |
| Divorced/Separated |
116 |
13.7 |
| Residence of the respondent |
|
|
| Rural |
607 |
71.8 |
| Urban |
238 |
28.2 |
| Household/family size |
|
|
| Greater than 5 |
345 |
40.8 |
| Less than or equal to 5 |
500 |
59.2 |
| Household having member ≥18 years old |
|
|
| No having ≥18 years old |
122 |
14.4 |
| Having one |
169 |
20 |
| Having two or above |
554 |
65.6 |
| Household members younger than 5 years old |
|
|
| No child |
385 |
45.6 |
| Having one child |
350 |
41.4 |
| Two or above |
110 |
13 |
| Household members older than age 65 years |
|
|
| No older age |
756 |
89.5 |
| One or above |
89 |
10.5 |
| Occupation of the respondent |
|
|
| Farmer |
440 |
52.1 |
| Housewife |
89 |
10.5 |
| Merchant |
93 |
11 |
| Daily laborer |
141 |
16.7 |
| Others |
82 |
9.7 |
| Educational status of the respondent |
|
|
| Unable to read and write |
309 |
36.6 |
| Read and write |
135 |
16 |
| Primary school |
252 |
29.8 |
| Secondary school |
139 |
16.4 |
| College or above |
10 |
1.2 |
| Wealth Index |
|
|
| Poorest (1st quintile) |
164 |
19.4 |
| Poor (2nd quintile) |
165 |
19.5 |
| Medium (3rd quintile) |
174 |
20.6 |
| Rich (4th quintile) |
180 |
21.3 |
| Richest (5th quintile) |
162 |
19.2 |
Table 1. Demographic and socioeconomic characteristics of the study participants in Tigray Region, Northern Ethiopia, 2020 (N = 845).
Health and health-related characteristics
Out of the total sample size, 84 (9.9%) respondents had a history
of chronic illness, and of the total respondents 250(29.5%) had at
least one episode of acute illness in the last six months and almost
all (92%) of them sought treatment for their recent episodes,
with 136(59.4%), 70(30.6%), and 23(10%) in public health
centers, hospitals, and private health facilities, respectively. Of
the total participants, 611(72.3%) lived close to health centers
and 234(27.7%) to hospitals (Table 2).
Characteristics |
Number |
Percentage |
| Have history of chronic illness |
|
|
| Yes |
84 |
9.9 |
| No |
761 |
90.1 |
| Encountered any illness during the last 6 months in the family |
|
|
| Yes |
250 |
29.6 |
| No |
595 |
70.4 |
| Have sought and received medical care (n=250) |
|
|
| Yes |
229 |
27.1 |
| No |
21 |
2.5 |
| Place where you receive treatment (n=250) |
|
|
| Public health center |
136 |
59.4 |
| Private health facility |
23 |
10 |
| Public hospital |
70 |
30.6 |
| Nearest health facility to your home |
|
|
| Hospital |
234 |
27.7 |
| Health center |
611 |
72.3 |
Table 2. Health and health-related situations of participants in Tigray Region, Northern Ethiopia, 2020 (N=845).
Awareness of head of household
The results revealed that the majority of respondents, 796
(94.2%), had heard about community-based health insurance
(CBHI). Nearly two-thirds of the respondents received CBHI
information from health extension workers and were aware
that CBHI is not like a saving scheme; that is, they will not earn
interest in their premium payment, nor will the premium be
returned even if they do not use health services, but rather that
the premium is a payment to finance future health costs. Besides,
more than 70% of the households had information that not only
the poor are members of the CBHI.
Practice of household heads toward CBHI
Of the total 845 household members covered in this survey,
433 (51.2%) were insured with the scheme through their own
contributions. More than half of the surveyed households had less than or equal to two years of enrolment. More than two-thirds of
the members paid a premium at the Kebele administration office.
Members were asked why they joined the CBHI scheme; around
one-quarter clarified that they did not know enough about the
CBHI scheme (Table 3).
Characteristics |
Number |
Percentage |
| Insurance status |
|
|
| Insured |
433 |
51.2 |
| Not insured |
399 |
47.2 |
| Insured but not renewed |
13 |
1.5 |
| Length of enrollment |
|
|
| Less than/equal to 2 years |
241 |
54 |
| Greater than 2 years |
205 |
46 |
| Time taken, after payment of registration fee and premium, to start utilizing health services(n=446) |
|
|
| Greater than 30 days |
286 |
64.1 |
| Less than 30 days |
160 |
35.9 |
| Where do you pay the premium |
|
|
| At the CBHI office |
76 |
17 |
| At kebele administration office |
309 |
69.3 |
| Official comes and collects |
61 |
13.7 |
| Why did you decide to enrolling CBHI (n=699) |
|
|
| Illness and/or injury occurs frequently in our household |
163 |
23.3 |
| To finance healthcare expenditure |
271 |
38.8 |
| Premium is low compared to the user fee price to obtain medical treatment |
224 |
32.04 |
| Pressure from other family members/community |
10 |
1.43 |
| Pressure from the CBHI office |
31 |
4.43 |
| Why did you decide not to enroll in CBHI (n=404) Number percentage |
|
|
| Illness and injury does not occur frequently in our household |
48 |
11.88 |
| The registration fee and premiums are not affordable |
77 |
19.06 |
| Want to wait in order to confirm the benefits of the scheme from others |
57 |
14.11 |
| We do not know enough about the CBHI scheme |
93 |
23.02 |
| There is limited availability of health services |
36 |
8.91 |
| The quality of healthcare services is low |
36 |
8.91 |
| The benefit package does not meet our needs |
31 |
7.67 |
| CBHI management staff are not trustworthy |
13 |
3.22 |
| Waiting time to access services is longer for CBHI members |
13 |
3.22 |
Table 3. Practice of household head toward CBHI in Tigray Region, Northern Ethiopia, 2020 (N=845).
Household head’s knowledge of CBHI benefit packages: The
majority of the households, 805(95.3%), thought regarding health
and health-related expenditure that CBHI is good way of helping
clients with health expenditures. In addition, approximately 80
percent, 672(79.5%), of household heads knew that CBHI covers
only care within the country. Similarly, 91.8% of respondents
knew that CBHI covers for both outpatient and inpatient
health expenditure. On the other hand, about 324(38.3%) and
235(27.8%) of household heads did not know that CBHI does not
cover medical care for cosmetic values and transportation fees,
respectively. Generally, in this study, the overall knowledge status
of respondents regarding what CBHI is, how it works, and its
concepts and purpose was 521(61.7%) respondents.
Willingness to pay: In this study, the majority of the respondents,
743(87.9%) know the current premium and registration fee
of community-based health insurance (CBHI) and 790(93.5%)
plan to renew/enrolled their membership of CBHI. However,
267(36.7%) respondents felt that the premium for CBHI per
household is inadequate. Hence, greater than 60%, 121(62.7%)
respondents were urban communities and about 279 (52%) from
rural communities suggested to increase the current premium
for CBHI. The mean annual amount of money (premium) per
household head they were willing to pay was 396 ETB (SD=±216)
for urban and310 ETB (SD=±115) for rural areas per household
annually. Similarly, the average amount of money they were
willing to pay for registration fees for CBHI was 18.9 (SD=±12.5)
(in Birr).
Benefit of CBHI among households: Of the total CBHI members,384(86.1%) respondents were assured that they benefitted
from the CBHI. Reduced costs of healthcare for 237(61.7%)
respondents were among the dominant benefits they received.
Of the respondents, 62(13.9%) believed that they did not benefit
from CBHI, and none of their HH members visited HFs for 41
(66.1%) respondents, paying additional costs for treatment for
17(27.4%) respondents, poor quality service for CBHI members
for 14(22.6%) respondents, and delay in issuing and distribution
of CBHI ID cards for 13(21%) respondents were some drawbacks
of CBHI.
Level of satisfaction of respondents toward the
quality of health services
Household satisfaction with the CBHI scheme was rated using
17 items, each having a 5-point scale from strongly disagree
to strongly agree. During the last six months, the number of
household heads visiting a health facility was 250(29.6%), of which
140(16.6%) visited health centers, 49(5.8%) both a hospital and
health center, and 61(7.2%) a hospital only, respectively. Those
who visited HFs more than once was 140 (56%) respondents,
while only once was 110 (44%) respondents.
Household heads dissatisfied with the quality of health services
showed an average 1.6 decrease compared to household heads
who were satisfied, which was 58.6;24(9.6%) household heads
responded they were strongly satisfied with cleanliness of
the health facility while25/111(22.5%)household heads were
dissatisfied with attentiveness and adequate follow up by nursing
staff. Household heads who was satisfied with quality of health
services was 58.6% greater as compared to household heads
who were dissatisfied. Household heads who were satisfied with
availability of drugs/medical supplies (56.8%) and diagnostic
facilities (60.4%) increased as compared dissatisfied household
heads. Household head satisfaction with confidentiality and
service provider attitudes toward explaining health problems was
68.8% and 64%, respectively. Household heads who were neutral
for satisfaction with waiting time and waiting time between
services had a 19.8% increase as compared to household heads
who were satisfied.
Household heads who were strongly dissatisfied with service
provider friendliness were 11.2%, while those strongly satisfied
with respect to the service provider were 8%. Similarly, 8.3%
of household heads were satisfied with the members’ card
collection process. The overall score for household satisfaction
with the CBHI scheme was 75.6 (Table 4).
| Characteristics |
Number |
Percentage |
| Have you visited a health facility during the last 6 months |
|
|
| Yes |
250 |
29.6 |
| No |
595 |
70.4 |
| Frequency of health facility visiting |
|
|
| Once |
110 |
44 |
| Greater than once |
140 |
56 |
| Health institution/facility visited |
|
|
| Only hospital |
61 |
7.2 |
| Both hospital and health center |
49 |
5.8 |
| Only health center |
140 |
16.6 |
| Satisfied with the service you received during your visit/stay |
|
|
| Very dissatisfied |
13 |
5.2 |
| Dissatisfied |
44 |
17.6 |
| Neutral |
31 |
12.4 |
| Satisfied |
147 |
58.9 |
| Very satisfied |
15 |
6 |
| Satisfied with overall quality of service |
|
|
| Very dissatisfied |
4 |
1.6 |
| Dissatisfied |
39 |
15.6 |
| Neutral |
58 |
23.2 |
| Satisfied |
142 |
56.8 |
| Very satisfied |
7 |
2.8 |
| Availability of drugs/medical supplies |
|
|
| Very dissatisfied |
9 |
3.6 |
| Dissatisfied |
57 |
22.8 |
| Neutral |
42 |
16.8 |
| Satisfied |
126 |
50.4 |
| Very satisfied |
16 |
6.4 |
| Availability of diagnostic facilities |
|
|
| Very dissatisfied |
6 |
2.4 |
| Dissatisfied |
35 |
14 |
| Neutral |
58 |
23.2 |
| Satisfied |
129 |
51.6 |
| Very satisfied |
22 |
8.8 |
| Cleanliness of the facility |
|
|
| Very dissatisfied |
5 |
2 |
| Dissatisfied |
26 |
10.4 |
| Neutral |
43 |
17.2 |
| Satisfied |
152 |
60.8 |
| Very satisfied |
24 |
9.6 |
| Waiting time (from time of arrival in the health facility to seeing a health professional) |
|
|
| Very dissatisfied |
6 |
2.4 |
| Dissatisfied |
48 |
19.2 |
| Neutral |
42 |
16.8 |
| Satisfied |
145 |
58 |
| Very satisfied |
9 |
3.6 |
| Waiting time between services (e.g. between consultation and diagnosis) |
|
|
| Very dissatisfied |
5 |
2 |
| Dissatisfied |
42 |
16.8 |
| Neutral |
57 |
22.8 |
| Satisfied |
120 |
48 |
| Very satisfied |
26 |
10.4 |
| Friendliness of staff |
|
|
| Very dissatisfied |
8 |
3.2 |
| Dissatisfied |
38 |
15.2 |
| Neutral |
48 |
19.2 |
| Satisfied |
128 |
51.2 |
| Very satisfied |
28 |
11.2 |
| Respect from healthcare providers |
|
|
| Very dissatisfied |
6 |
2.4 |
| Dissatisfied |
35 |
14 |
| Neutral |
51 |
20.4 |
| Satisfied |
138 |
55.2 |
| Very satisfied |
20 |
8 |
| Attentiveness and adequate follow up by the nursing staff (inpatient only in hospitals) |
|
|
| Very dissatisfied |
8 |
7.2 |
| Dissatisfied |
17 |
15.3 |
| Neutral |
19 |
17.1 |
| Satisfied |
60 |
54.1 |
| Very satisfied |
7 |
6.3 |
| Quality of food and other inpatient amenities (inpatient only in hospitals) |
|
|
| Very dissatisfied |
3 |
2.7 |
| Dissatisfied |
22 |
19.8 |
| Neutral |
25 |
22.5 |
| Satisfied |
59 |
53.2 |
| Very satisfied |
2 |
1.8 |
| Satisfied with confidentiality |
|
|
| Very dissatisfied |
9 |
3.6 |
| Dissatisfied |
30 |
12 |
| Neutral |
39 |
15.6 |
| Satisfied |
142 |
56.8 |
| Very satisfied |
30 |
12 |
| Satisfied with service providers’ attitude toward explaining health problems |
|
|
| Very dissatisfied |
14 |
5.6 |
| Dissatisfied |
34 |
13.6 |
| Neutral |
42 |
16.8 |
| Satisfied |
137 |
54.8 |
| Very satisfied |
23 |
9.2 |
| Satisfaction with members card collection on process (only CBHI members) |
|
|
| Very dissatisfied |
35 |
7.8 |
| Dissatisfied |
71 |
15.9 |
| Neutral |
58 |
13 |
| Satisfied |
245 |
54.9 |
| Very satisfied |
37 |
8.3 |
| Overall satisfaction |
|
|
| Satisfied |
189 |
75.6 |
| Neutral |
52 |
20.8 |
| Not satisfied |
9 |
3.6 |
Table 4. Level of satisfaction of household heads toward quality of health service in Tigray Region, Northern Ethiopia, 2020 (N=845).
Factors associated with willingness to pay
To identify the factors associated with willingness to pay, bivariate
linear regression was used with the following independent
variables: sex, age of household head, marital status, residence,
household family size, occupation of respondent, educational
status of respondent, wealth index, illness in the last six months,
place receiving treatment, nearest health facility, place where
you hear about CBHI, level of awareness, length of enrolment,
knowledge status, overall satisfaction of health services, and
cumulative perceived perception of CBHI. Variables that were
associated with WTP in the bi-variable analysis (at P-value < 0.25)
were included in the multivariable linear regression model. After
adjusting for all other variables, 11 variables (age of household
head, residence, family size, occupation of respondent,
educational status of respondent, wealth index, nearest health
facility, place where you hear about CBHI, level of awareness,
knowledge status, and overall satisfaction with health services)
were identified as factors associated with willingness to pay the
CBHI schemes.
For a one-unit increase in age, i.e., when age increased,
willingness to pay increased by 0.86 (95% CI: 0.13, 1.70, P=0.009).
Changing from urban to rural regions resulted in decreased
willingness to pay by 79.6% (95% CI: -118.26,-40.85, p=0.001). A one-unit increase in family size resulted in a 5.26 point increase in
willingness to pay (95% CI: 0.16, 14.71; p=0.03), merchants were
83.4 times more willing to pay than farmers (95% CI: 8.66, 175.5;
p=0.05) whereas daily laborers decreased willingness to pay
by 68% compared to farmers (95% CI: -119.74, 16.54; p=0.01),
and changing from secondary school and above education to
unable to read and write decreased by 66% the willingness to
pay (95% CI: -71.06, 2.81;p= 0.007). When the wealth index
increased, willingness to pay increased 2.6 times (95% CI: 0.13,
14.35; p=0.009) and 12 times (95% CI: 1.21, 20.11; p=0.001)
among the rich and richest, respectively. When hospitals were
the nearest health facility, willingness to pay increased 57 times
(95% CI: 20.82, 94.43; p=0.01). The source of information on CBHI
being through neighbours, mass media, and health professionals
decreased willingness to pay by 74%, 72%, and 71%, respectively,
when compared with health extension workers. Having awareness
of CBHI was 49.18 times more willing to pay when compared with
those not aware. Those who were knowledgeable were 2.5 times
willing to pay compared with those not knowledgeable (95% CI:
0.05,10.05; p=0.03),and when compared with those not satisfied
with the service given, those who were satisfied were 27 times
willing to pay (95% CI: 3.36, 59.45; p=0.04) (Table 5).
| Characteristics |
Bivariate Analysis |
|
|
|
|
Multivariate Analysis |
|
|
|
| |
B |
95%CI |
|
P-Value |
|
B adjusted |
95%CI |
|
P-Value |
| Sex of household head |
|
|
|
|
|
|
|
|
|
| Male |
17.01 |
(-4.84, 38.87) |
|
0.13 |
|
|
|
|
NS |
| Female |
1 |
|
|
|
|
|
|
|
|
| Age of household head |
0.64 |
(-0.12,1.40) |
|
0.09 |
|
0.86 |
(0.13,1.70) |
|
0.009 |
| Religion |
|
|
|
|
|
|
|
|
|
| Orthodox |
-28.13 |
(-88.32,26.85) |
|
0.32 |
|
|
|
|
NS |
| Muslim/Catholic |
1 |
|
|
|
|
|
|
|
|
| Marital status of household head |
|
|
|
|
|
|
|
|
|
| Single |
1 |
|
|
|
|
|
|
|
|
| Married |
1.56 |
(-22.17,25.29) |
|
0.13 |
|
|
|
|
NS |
| Widowed |
2.64 |
(-37.99,43.28) |
|
0.89 |
|
|
|
|
NS |
| Divorced/separated |
-28.49 |
(-60.51,3.53) |
|
0.08 |
|
|
|
|
NS |
| Residence of household head |
|
|
|
|
|
|
|
|
|
| Rural |
-86.29 |
(-109.7,-62.85) |
|
0 |
|
-79.57 |
(-118.26,-40.85) |
|
0.001 |
| Urban |
1 |
|
|
|
|
|
|
|
|
| Household/family size |
6.75 |
(0.68,12.81) |
|
0.03 |
|
5.26 |
(0.16,14.71) |
|
0.02 |
| Household members ≥18 years old |
-2.55 |
(-11.19,6.09) |
|
0.56 |
|
|
|
|
NS |
| Household members youngerthan 5 years old |
-7.54 |
(-22.66,7.57) |
|
0.33 |
|
|
|
|
NS |
| Household members older than age 65 years |
-1.48 |
(-28.32,25.35) |
|
0.91 |
|
|
|
|
NS |
| Occupation of respondents |
|
|
|
|
|
|
|
|
|
| Farmer |
1 |
|
|
|
|
|
|
|
|
| Housewife |
14.19 |
(-20.62,49.01) |
|
0.42 |
|
|
|
|
NS |
| Merchant |
50.29 |
(15.29,85.31) |
|
0.01 |
|
83.44 |
(8.66,175.52) |
|
0.05 |
| Daily laborer |
-37.5 |
(-66.64,-8.36) |
|
0.01 |
|
-68.14 |
(-119.74,16.54) |
|
0.01 |
| Others*(petty traders, unemployed students) |
35.66 |
(-1.48,72.81) |
|
0.6 |
|
|
|
|
NS |
| Educational status of respondent |
|
|
|
|
|
|
|
|
|
| Unable to read and write |
-15.51 |
(-38.07,7.04) |
|
0.18 |
|
-34.13 |
(-71.06,2.81) |
|
0.007 |
| Read and write |
10.39 |
(-18.95,39.73) |
|
0.49 |
|
|
|
|
NS |
| Primary school |
7.71 |
(-15.94,31.35) |
|
0.52 |
|
|
|
|
NS |
| Secondary school |
1 |
|
|
|
|
|
|
|
|
| Wealth Index |
|
|
|
|
|
|
|
|
|
| Poorest (1st quintile) |
1 |
|
|
|
|
|
|
|
|
| Poor (2nd quintile) |
0.81 |
(-26.57,28.19) |
|
0.95 |
|
|
|
|
NS |
| Medium (3rd quintile) |
3.28 |
(-23.65,30.21) |
|
0.81 |
|
|
|
|
NS |
| Rich (4th quintile) |
-38.51 |
(-64.50,-12.53) |
|
0 |
|
2.6 |
(0.13,14.35) |
|
0.009 |
| Richest (5th quintile) |
37.28 |
(9.81,64.74) |
|
0.01 |
|
12.01 |
(1.21,20.11) |
|
0.001 |
| Have history of chronic illness |
|
|
|
|
|
|
|
|
|
| Yes |
-17.35 |
(-54.56,19.85) |
|
0.36 |
|
|
|
|
NS |
| No |
1 |
|
|
|
|
|
|
|
|
| |
|
|
|
|
|
|
|
|
|
| Encountered any illness during the last 6 months in the family |
|
|
|
|
|
|
|
|
|
| Yes |
14.43 |
(-9.38,38.23) |
0.23 |
|
|
|
|
NS |
|
| No |
1 |
|
|
|
|
|
|
|
|
| Have sought and received medical care |
|
|
|
|
|
|
|
|
|
| Yes |
-3.65 |
(-79.39,72.09) |
0.92 |
|
|
|
|
NS |
|
| No |
1 |
|
|
|
|
|
|
|
|
| Place where you receive treatment |
|
|
|
|
|
|
|
|
|
| Public health center |
-16.98 |
(-46.58,12.62) |
0.26 |
|
|
|
|
NS |
|
| Private health facility |
123.44 |
(59.51,187.38) |
0.001 |
|
|
|
|
NS |
|
| Public hospital |
1 |
|
|
|
|
|
|
|
|
| Nearest health facility to your home |
|
|
|
|
|
|
|
|
|
| Hospital |
72.82 |
(49.09,96.55) |
0.001 |
|
|
57.62 |
(20.82,94.43) |
0.01 |
|
| Health center |
1 |
|
|
|
|
1 |
|
|
|
| Place where you obtain information/hear about CBHI (N=796) |
|
|
|
|
|
|
|
|
|
| Neighbors/friends |
-42.22 |
(-75.00,-9.45) |
|
|
0.01 |
-74.84 |
(-129.15,-20.52) |
|
0.007 |
| CBHI officials in public meeting |
-10.86 |
(-32.92,-11.19) |
|
|
0.33 |
|
|
|
NS |
| House to house awareness creation campaign |
-27.21 |
(-6.72,-61.13) |
|
|
0.12 |
|
|
|
NS |
| Mass media: TV, radio |
-88.75 |
(-125.45,-52.04) |
|
|
0.001 |
-72.96 |
(-128.67,-17.24) |
|
0.01 |
| Professionals in health facilities |
-28.53 |
(-53.69,-3.36) |
|
|
0.03 |
-71.37 |
(-107.91,-34.83) |
|
0.001 |
| Health extension workers |
1 |
|
|
|
|
|
|
|
|
| Level of awareness |
|
|
|
|
|
|
|
|
|
| Aware |
38.15 |
(14.65, 61.65) |
|
|
0.001 |
49.18 |
(12.59,85.77) |
|
0.009 |
| Not aware |
1 |
|
|
|
|
|
|
|
|
| Length of enrollment |
|
|
|
|
|
|
|
|
|
| Less than/equal to 2 years |
-23.51 |
(-56.83,9.81) |
0.17 |
|
|
|
|
NS |
|
| Greater than 2 years |
1 |
|
|
|
|
|
|
|
|
| Time taken, after payment of registration fee and premium, to start utilizing health services |
|
|
|
|
|
|
|
|
|
| Greater than 30 days |
0.72 |
(-34.03,35.47) |
0.98 |
|
|
|
|
NS |
|
| Less than 30 days |
1 |
|
|
|
|
|
|
|
|
| Knowledge status |
|
|
|
|
|
|
|
|
|
| Knowledgeable |
1.8 |
(0.24,20.64) |
0.06 |
|
|
2.5 |
(0.05,10.05) |
0.03 |
|
| Not knowledgeable |
1 |
|
|
|
|
|
|
|
|
| Benefited from the CBHIscheme |
|
|
|
|
|
|
|
|
|
| Yes |
-25.09 |
(-74.62,24.42) |
0.32 |
|
|
|
|
NS |
|
| No |
1 |
|
|
|
|
|
|
|
|
| Overall satisfaction of health service |
|
|
|
|
|
|
|
|
|
| Satisfied |
24.64 |
(10.14,73.45) |
0.23 |
|
|
27.32 |
(3.36,59.45) |
0.04 |
|
| Not satisfied |
1 |
|
|
|
|
|
|
|
|
| Cumulative perceived perception of CBHI |
|
|
|
|
|
|
|
|
|
| High |
-19.72 |
(-41.65,2.21) |
0.09 |
|
|
|
|
NS |
|
| Low |
1 |
|
|
|
|
|
|
|
|
Table 5. Factors associated with willingness to pay of household heads toward CBHI in Tigray Region, Northern Ethiopia, 2020 (N=845)
Community awareness and perception
According to most key informants, community awareness and
perception of CBHI have increased over time, and enrollment in
the scheme has also increased. However, as the premium for the
scheme is small, this affects the perception of some community’s
on being a member as they consider that they could not receive
quality services by paying such premiums. An expert curative and
rehabilitative case-team coordinator said:
“As observations, there are wrong perceptions from some
members of the community who said that through this low
premium, CBHI could not be as much more benefited.”
Furthermore, poor interest in enrolling when they feel healthy
and want to be a member when they are sick indicates poor
awareness of the system; in line with this, if members of the
scheme were not sick in the fiscal year, they felt compunctions
for the premium they paid.
CBHI coverage and sustainability: All key informants agreed that
CBHI coverage in their respective districts increased from year
to year, ranging from 52% during Ramma to 92% during Mokoni.
In 2012, E.C. shows huge inter-district coverage differences
of CBHI and sustainability problems due to gaps in community
mobilization for enrollment. Campaign mobilization focuses on
coverage rather than convincing the community of the aim of the
scheme. In a pilot district, CBHI coverage was increased, providing
aid such as wheat for enrolment, which affected community
sustainability in the scheme of some key informants:
Due to that wrong way, some community members considered
enrolment to CBHI as a benefit of to the government not as a
benefit of themselves” (District CBHI coordinator).
Most key informants of the districts confirmed that they faced
budget discrepancies/deficits due to incomparable premium
payment amounts, and low coverage of the CBHI enrolment and continuous market inflation are among other reasons. In addition,
one participant explained that most members of the scheme
were households who repeatedly got sick, and those who had no
history of illness were not members: .
“Most member of CBHI scheme is those who usually get sick and
those who did not usually get sick are not” (district curative and
rehabilitative case team coordinator).
On the other hand, increased healthcare demand, even for
health check-ups, from the community increases the budget
deficit for CBHI. Poor preparedness of health facilities was also
mentioned as a reason for problems with CBHI. Furthermore,
most participants confirmed that less focus from different levels
of leaders affected the sustainability of the scheme:
“Even as a region, when should work more to make it more
sustainable, we are always good in starting programmers but we
are poor to make programme become sustainable”(cluster CBHI
head).
Health facilities’ preparedness and service quality: Most participants declared that health facilities tried their best to
avail drugs and supplies adequately to satisfy the community.
However, because of the absence of drugs and supplies in the
market and the Ethiopian Pharmaceutical Supply Agency (EPSA),
clients are referred to private health facilities and this creates
dissatisfaction, even if they withdraw from the scheme. On the
other hand, some clients want to be referred to private health
facilities as they thought better treatments can be find there,
which is costly ruin of CBHI is highly increased up to 100,000
birr for the reimbursement of individuals. Furthermore, due to
a lack of preparedness, CBHI is becoming a source for the lack of
good governance in some health facilities, increasing community
dissatisfaction:
“If we failed prepare the community will engulf us for our failure"
(district CBHI coordinator).
According to reflections from some participants, increasing health
service utilization following CBHI implementation is negatively
affected by the rude character of health service providers:
“When clients repeatedly visit health facilities, some health
professionals are not happy by the workload due to CBHI and
even showed a rude character for clients for their repeated visit”
(district curative and rehabilitative case team coordinator).
Some participants explained the contribution of CBHI to improving
service quality through proper referral linkage because due to
CBHI the health facilities utilize the health tier system properly.
Thus, self-referral to higher levels of health facilities decreased
as clients did not want to cover half the payment for the service
they obtained, preventing unnecessary workload in higher health
facilities and underutilizing lower-level health facilities.
Some participants mentioned a public-private partnership
as a mechanism to prevent ruins in the CBHI. Furthermore,
informants noted that regulation of exaggerated drug and supply
costs in private health facilities should be practiced, and that such
measures are the responsibility of the functional state:
“We are regulating private health facilities for their quality
service provision, having expired drugs, and practicing other
unpermitted procedures, why do not we regulate them on the
cost of the services they asked? Nothing! We can regulate them”
(cluster CBHI coordinator).
Challenges: Participants indicated resource-related challenges
in the implementation of CBHI. Most participants underlined
the structural challenges of CBHI. Even if the implementation
among districts is not standardized, some districts have a CBHI
coordinator, while others do not, and responsibility is given to
curative and rehabilitative case team coordinators.
Most informants explained that the scheme had adequate
human power and budget limitations. Furthermore, negligence
in allocating an administrative budget to the scheme was
mentioned. Some participants reflected their grievances about
the poor ownership of CBHI by different bodies at each level of
management. Thus, for most informants, especially those directly
involved in the scheme, these challenges were described as the
cause of their dissatisfaction with the scheme:
“Though CBHI is a basic scheme to help the community, giving a
due focus as of its importance has remained low” (Cluster CBHI
coordinator).
“The focus given for CBHI by mangers in each level is not
satisfactory, and I feel sorry and even I think I will leave my job
if I get another better opportunity” (district CBHI coordinator).
Due to inadequate human power, premium collection and
utilization are negatively affected. Furthermore, this also affects
health extension workers performing other routine activities
because of their engagement in collecting revenues. Additionally,
according to the informants, revenue extravagancy is also in place
because of the absence of responsible bodies in each kebele:
Theoretically, in kebele during the collection of revenue, above
2000 birr should not be wait in the hands of the collectors; it
should be deposited to the nearby bank account, but in practice,
it is common to get, up to 80,000 birr in the hands of the revenue
collectors. Therefore, our revenue collection is not immune
from extravagancy, (district curative and rehabilitative case team
coordinator).
Another challenge faced by the informants was the restructuring
of districts. As districts are separated into different administrative
units, this delays the start of the scheme among newly emerging
districts and is challenging for the continuity of the scheme.
Recommendations/the way forward
For better CBHI implementation, a robust and effective pooling
system is critically important. One of the specific objectives of
this study was to identify where the pooling system for CBHI
should be situated, as a number of newly emerged districts have
been created for administrative purposes in the current Tigray. As
a result, 86% (n=24) of the key informants recommended that the
pool for CBHI should be situated at the district level. Participants
described their arguments regarding this issue: situating the
pool at the district level enables districts to own the scheme,
decentralizes the health system and decisions, and ensures
equity.
However, among the participants, three preferred the pool to
be situated at a regional level. Their argument was based on
the importance of focusing on the scheme at the regional level
and sharing responsibilities. Additionally, they also need to lead
the program through experience sharing to achieve a balanced
performance among districts, which they considered would
be better if handled by the region. However, one participant
preferred it to be situated in both districts and regions. His
argument was that this would solve the problems of delay during
signing the MOU among district health offices and hospitals.
Accordingly, he noted that districts should make agreements
with health centers and hospitals within the region. Thus, partial
pooling in both districts and regions is an option.
Furthermore, almost all participants recommended revising the
structure of CBHI and that adequate human power should be
employed. Adequate budget allocation for the scheme was also
recommended by most informants. In line with this, more than 80%
(n=23) of the participants recommended raising premiums due to
the existence of market inflation in the cost of drugs and supplies.
On the other hand, three participants agreed on increasing the
premium but they had concern with the community’s ability
to pay, even though they reflected that members of the CBHI
scheme could fail to renew their membership. Furthermore, one
participant indicated his preference for the total involvement of
the community, even with the current premium, before rushing
to increase it. However, media coverage was also recommended
to improve community awareness. The participants also
recommended budget subsidization from the government to
reverse the ruins. However, from the reflection of the participants,
other methods of resource mobilization are poor on the ground.
Discussion
This study aimed to assess WTP for CBHI, pooling mechanisms,
and associated factors among households in Tigray Region,
Northeast Ethiopia. This study revealed that six out of ten (62%)
urban dwellers and five out of ten (52%) rural dwellers wanted to
pay an additional amount to the current governmental premium
threshold (which is 240 ETB for rural and 350 ETB for urban). As
an average amount of premiums, households were willing to pay
per annum per household 396 ETB (10.7 USD) and 310 ETB (8.4
USD) (October 2020 exchange rate) for urban and rural dwellers,
respectively. This current finding is higher than the study findings
in Fogera district (187.4 ETB) [18] and Adama district (211 ETB)
[19], but lower than the studies in Ecuador[20] and other parts
of Ethiopia [21,22] which showed WTP an average of US$30,
US$16, and US$11.12 per year, respectively. This could be due
to differences in the elicitation methods of the initial bids and
changes in the value of money over time, area, design, and
participants. Nevertheless, it is far from the 34 USD (30 USD-
40 USD) recommended by the WHO in 2001 to deliver essential
healthcare in low-income countries like Ethiopia. Based on the
2014 report, the mean medical expenditure was 28.65 USD per
capita in Ethiopia. A study conducted in Gondar indicated that
the median total cost incurred by patients was more than 22.25
USD per visit.
The results of this study revealed that age of the household head
is significantly associated with willingness to pay for CBHI, and
a similar finding in Namibia and Tanzania showed that the age
of respondents affects their interest in and WTP for the scheme.
This might be because as the age of individuals increases their
income status also increases, or because as the age of individuals
increases their health status will be decreased. This result is
consistent with a study conducted in Nigeria which indicated
that rural residents were less likely to have WTP. This implies that
raising awareness is needed, especially in rural areas, and care
must be taken to fix the premium paid by different population
groups, which suggests that premiums should be adjusted for
income and that there should be exemptions and subsidies for
the poor to increase their willingness. Study participants who had
few family members were less likely to pay for the scheme than
their counterparts. This result is supported by studies conducted
in other parts of Ethiopia Nigeria, China and India which might
be because households with lower family sizes may consider
covering the cost of medical care for their families by OOP. Again,
this study’s results show that merchants were more likely to
be willing to pay than farmers, which is consistent with studies
conducted in other parts of Ethiopia. This might be a result of
their level of earnings and ability to afford high medical expenses,
given that families who are farmers (who are most often exposed
to poverty) are less willing to pay than merchants in the private
sector; policymakers must be aware that the poorest can be
excluded from such a scheme and either subsidize or lower
their premiums. The educational level of the respondents was
found to be another factor that increased the premium they
were willing to pay for the CBHI scheme, which is consistent
with studies conducted in Nigeria, Cameron and Burkina Faso
Educated household heads have better knowledge about the
advantage of making regular insurance payments to avoid the
risk of catastrophic medical expenditures at the time of illness,
and might also have better income, access to media, and easily
understand the benefits of participating in the health insurance
scheme.
The wealth status of families was positively and significantly
associated with WTP, which is similar to other studies conducted
in other parts of Ethiopia Fogera district Nigeria China and India
A possible explanation might be that wealthier people have
more WTP than the poor, which might be due to fear of high
asset losses if unexpected events could occur, implying that the
government should implement a co-payment system to enable
poor households to meet their requirements. Households that
are closer to hospitals are more willing to pay than those near
health centers; this is an issue of quality health services, so the
government should work more to equip health centers with
medical equipment and drugs. A study conducted in Conakry and
Guinea showed that poor quality of care in healthcare services is
one of the main causes of low and even declining enrolment in
CBHI.
HEW are more successful in disseminating information to
the community regarding CBHI than other methods such as
mass media and friends, which may be because a number
of identified successes were achieved by the HEP (family
planning, immunization, ANC, malaria, TB, HIV, and community
satisfaction) in the first five years of implementation. Service
utilization, improved knowledge and care seeking, increased
latrine construction and utilization, enhanced reporting of
disease outbreaks, a high level of community satisfaction and
HEWs as the primary source of information have increased
Respondents’ awareness of the CBHI scheme has a positive and
significant association with their WTP for CBHI. This finding is
consistent with those of studies conducted in Nigeria Cameron
and Myanmar This may be due to the catastrophic effects of
health problems and the benefits of joining insurance schemes
earlier. This implies that intensive awareness creation and trustbuilding
programs are required in the community, particularly for
those who do not have formal education and those who have not
been insured before. One qualitative participant indicated that:
“The community awareness and perception on CBHI has been
increased from time to time. Thus, the interest of enrolling to the
scheme is increased. However, there are some perceptions which
hinder the enrollment of the community like they considered the
scheme as the issue of the poor and they don’t consider getting
quality service through the seated premium [21,22].
The study indicates that the knowledge of respondents regarding
CBHI is significantly associated with willingness to pay, which
shows that each level of government sectors, in collaboration with
CBHI programmers, is more aware of the community about CBHI
benefit packages and their premiums. The level of satisfaction
with health service delivery affects willingness to pay for CBHI. In
2005, the World Health Assembly called on all countries to move
toward universal health coverage, especially developing countries
with huge inequalities in health service delivery Therefore, CBHI
enhances universal health coverage (UHC) if client satisfaction is
met.
Limitations
Some district CBHI focal persons were not available during
the data collection period, and data were collected from their
representatives, which may have its own drawbacks for decisions
which could, in turn, affect the pooling mechanism of CBHI.
Conclusion
The average amount of money households were willing to pay
per annum per household for CBHI of urban dwellers was 396
ETB (10.7 USD at October 2020 exchange rate) and of rural
dwellers was 310 ETB (8.4 USD at October 2020 exchange rate.
Age of the household head, residence, family size, occupation of
the respondent, educational status, wealth index, nearest health
facility, place where they obtained information about CBHI, level
of awareness, knowledge status, and overall satisfaction with
health services were identified as independent factors associated
with willingness to pay for the CBHI schemes. Regarding the
pooling mechanism, this should be located at district level.
Participants described their arguments regarding this issue:
situating the pool at the district level enables districts to own the
scheme, decentralizes the health system, makes decentralizes
decisions, and ensures equity. To alleviate deficits or to make
CBHI sustainable, factors include increasing the annual premium
and enrollment of the community to CBHI, budget subsidization
from the government to reverse the ruin, increase communitybased
awareness creation activities, and continue with the
current pooling mechanism at the district level, but establish or
revise a department at the health office that controls the process
of CBHI. Newly emerged districts should create their own pool in
their respective district.
Conflicts of Interest
The authors declare that they have no any conflicts of interest.
Authors Contributions
All authors conceived the study, performed the analysis,
and participated in designing the data collection tools, data
management, and writing of the manuscript. The authors agree to
be accountable for all aspects of the work related to its integrity.
All authors have read and approved the manuscript.
Acknowledgments
The authors acknowledge the Tigray Health Research Institute,
Tigray Regional Health Bureau, health facilities, and study
participants for their cooperation during the study.