Case Report - (2023) Volume 17, Issue 9
Botulinum Toxin as a Management for Scars after Cervical Disc Hernia Surgery
Juan Farak Gomez1*,
Jhon Fredy Bello Cordero1,
Lina Marcela Blandon Santamaria2,
Laura Margarita Viloria Gomez3,
Richard Jorge Ramos Montes4,
Laura Juliana Jaramillo Marino5,
Andriun Duarte Perez3,
Maria Jose Rivera Castillo6 and
Jaime Andres Lozano Navarro6
1Department of Emergency Medicine, Foundation University of Health Sciences, Bogota, Colombia
2Department of General Physician, Cooperative University of Colombia, Bogota, Colombia
3Department of General Physician, Sinu University, Bogota, Colombia
4Department of General Physician, Rafael Nunez University, Bogota, Colombia
5Department of General Physician, University of Santander, Bogota, Colombia
6Department of General Physician, Rosario University, Bogota, Colombia
*Correspondence:
Juan Farak Gomez, Department of Emergency Medicine, Foundation University of Health Sciences, Bogota,
Colombia,
Email:
Received: 21-Apr-2022, Manuscript No. IPHSJ-23-12739;
Editor assigned: 26-Apr-2022, Pre QC No. IPHSJ-23-12739 (PQ);
Reviewed: 10-May-2022, QC No. IPHSJ-23-12739;
Revised: 03-Oct-2023, Manuscript No. IPHSJ-23-12739 (R);
Published:
31-Oct-2023, DOI: 10.36648/1791-809X.17.9.1060
Abstract
Currently within the operating rooms of our hospitals there
are a number of patients requiring intervention for cervical
disc pathologies, which at the time of performing the
suturing process, a horizontal scar is acquired at the neck
level; an injury that after not being successful an adequate
resolution, both in the functional recovery of the entire
cervical area as well as the disappearance of the pain
suffered prior to intervention, results in serious
consequences that surely affect not only the image of the
patient but also the suffers, but also their psycho-emotional
development and their social development. Studies have
recently been published that support the use of botulinum
toxin injection in the muscular area adjacent to the wounds,
causing the immobilization of the wound and with it, a
significant improvement in the appearance of the final scar.
Keywords
Botulinum toxin; Scarring; Herniated disc;
Cervical wound; Keloid
Introduction
The keloid scars that are obtained after a surgical procedure
as a result of an unsuccessful resolution of a pathology have
represented lesions that are difficult to treat. The persistence of
an unattractive scar in an area as visible as the neck can be a
cause for concern, with a certain psychological and social
impact, it limits mobility and elasticity. Until now, there is no
treatment that has presented a 100% satisfactory effect. A
relevant factor that determines the final aesthetic appearance of
skin scars is the direction of the traction vectors of the scar skin,
so by acting on the tension of the wound edges during healing we can favor the final appearance of the scar resulting. The
injection of botulinum toxin in the muscular area adjacent to the
wounds causes the immobilization of the wound and with it, a
significant improvement in the appearance of the final scar [1].
Healing is a complex biological process that is divided into
three phases. The inflammatory phase aims to stop bleeding and
produce chemokines that attract regenerating cells. During the
second (proliferative) phase, there is a large increase in healing
mediator cells, including fibroblasts, endothelial cells and
neutrophils. At this time, angiogenesis begins to accelerate due
to the release of chemokines and angiogenic growth factors [2].
In the last phase (remodeling), the wound becomes less dense
and there are large numbers of well-differentiated
myofibroblasts, type I collagen and mature blood vessels. Any
alteration to this process triggers pathological scarring. The
tension of a wound is an important factor that determines the
degree of fibrosis and angiogenesis. From this concept the
incisions in the skin should be designed according to the lines of
relaxed tension. This dynamic stress has its effect on wounds by
producing tissue ischemia. This ischemia has been proposed as a
promoter of fibroblast migration because it is not an acceptable
environment for healing. As there is a greater proliferation of
fibroblasts, more collagen is synthesized in a disorganized way,
which develops pathological scars [3].
Studies demonstrate the effect of botulinum toxin-a on the
angiogenesis of a wound closed by first intention in the initial
stages of healing, showing an increase in the number of newly
formed blood vessels; propose that botulinum toxin-a maintains
fibroblasts in G0-G1 phases and decreases the process of mitosis
and the development of blood vessels [4].
Cervical disc herniation is defined as the exit of the nucleus
pulposus through the fibrous ring, due to an injury to the
intervertebral disc, generally resulting in a neurological clinical picture due to compression of the nerve roots of the affected
vertebral segment. The objective of surgery in cervical disc
herniations is the exeresis of the herniated disc and the
decompression of the nerve structures, as well as a successful
aesthetic resolution of the scar obtained [5].
Case Presentation
The study design is adapted to a systematic review of the evidence present in the scientific literature on the relevance of the application of botulinum toxin injection as a management for scars after cervical disc herniation surgery [6].
The literature search took place between 1997-2021, delving into various bibliographic databases in order to obtain information and review previous studies on the exposed topic. The keywords and Boolean operators used were "botulinum toxin", "healing", "herniated disc", "cervical injury", "keloid". Described through DeCS. In order to obtain a greater update on the subject, the articles published in the last 30 years were set as a temporary filter for the search [7].
Cervical disc herniation is defined as the exit of the nucleus pulposus through the fibrous ring, due to an injury to the intervertebral disc, generally resulting in a neurological clinical picture due to compression of the nerve roots of the affected vertebral segment. Considering symptomatic cervical hernias, those that present with radiculopathy, cervical disc herniations are more frequent in the 4th and 5th decades of life (45%) and the most frequent location is at the C6-C7 level (60%) followed by C5-C6 (20%) and C4-C5; being the root C7 the most affected. In a population study in Rochester, Minnesota, USA, the prevalence of cervical radiculopathy was 107.3 men and 63.5 women per 100,000 inhabitants, of which 5.5% were due to cervical disc herniations [8]. Currently, the intervention of cervical disc pathologies can be carried out in several ways, however, all of them lead to a closure by first intention, with the subsequent appearance of a scar at that level. Obviously, the first objective of this surgery is success in terms of resolving the pathology that affects the patient, both in the functional recovery of the entire cervical area, as well as the disappearance of the pain that he suffered prior to the intervention and not less the aesthetic part is important with adequate healing; otherwise, it can be a cause for concern, with a certain psychological and social impact. This is further aggravated if the evolution of the scar is not as expected and a hypertrophic or keloid scar appears with its bulge and on many occasions, itching and pain [9].
Studies have recently been published that support the use of botulinum toxin for the prevention of abnormal scar formation, injected around the wound. Although initially the treatment was carried out two weeks after the intervention, it has subsequently been seen that the earlier the botulinum toxin injection, the better the final result. An important goal in wound closure is to minimize scarring. Different methods have tried to address this problem, including corticosteroid injections, irradiation, the use of ultrasound, silicone applications and many others [10]. However, their effects have been unsatisfactory because they do little to alleviate the underlying disease process, which is the distraction of the effect of muscle traction on immature collagen. A relevant factor that determines the final aesthetic appearance of skin scars is the direction of the traction vectors of the scar skin, so by acting on the tension of the wound edges during healing we can favor the final appearance of the scar resulting. The injection of botulinum toxin in the muscular area adjacent to the wounds causes the immobilization of the wound and with it, a significant improvement in the appearance of the final scar [11].
The skin is a dynamic organ. It has a role of protection and metabolic exchanges, but also performs an aesthetic and social function. Any cutaneous aggression causes remodeling phenomena called "scarring", whose objective is to achieve optimal restoration of its integrity. This healing is a complex mechanism, which goes through different successive phases before producing a definitive scar in a few months. However, this scarring can be pathological (hypertrophic or keloid) or lead to a defective or "vicious" scar result. These situations give rise to great demands on the part of the patients (Figure 1).

Figure 1: Hypertrophic scar.
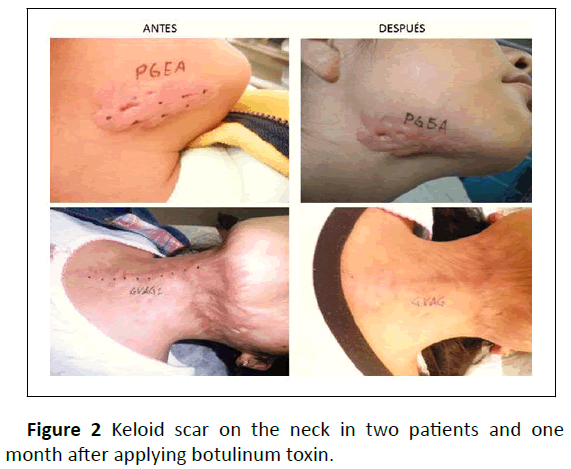
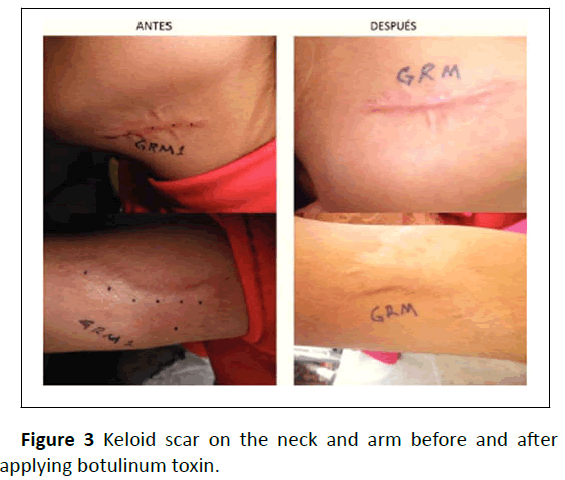
There are numerous innovative treatments, many of which are still in research protocols for the treatment of scars, such as botulinum toxin, which treats a local muscle-paralyzing substance, which has already demonstrated its effectiveness in improving scars, allowing the reduction of local tension and shear forces that maintain inflammation. The mechanisms by which botulinum toxin promotes proper wound healing are several [12]. The most obvious and well-known is the decrease in muscle contraction underlying and adjacent to the wound, thus reducing the tension that supports the scar. But there are other beneficial factors, recently discovered, such as the inhibition of fibroblast proliferation and extracellular matrix synthesis, both in animal and human models in vivo and the inhibition of sebaceous glands responsible for inflammatory responses that contribute to scar hypertrophy, among other molecular mechanisms yet to be elucidated (Figures 2 and 3).
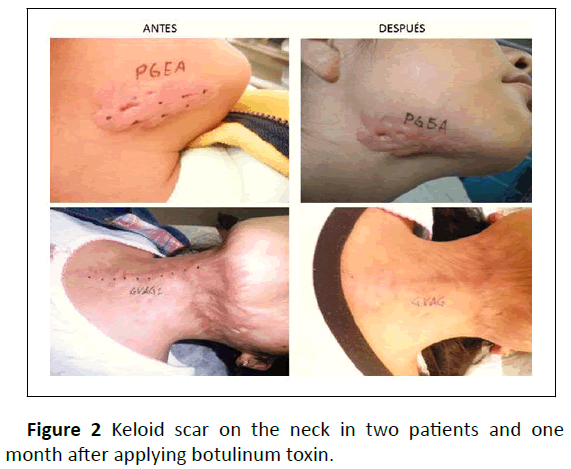
Figure 2: Keloid scar on the neck in two patients and one month after applying botulinum toxin.
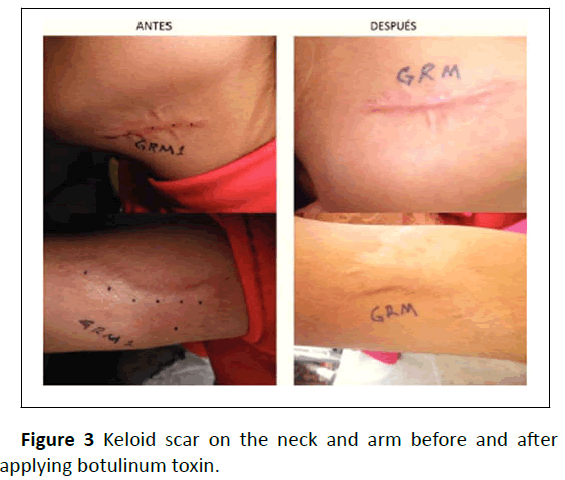
Figure 3: Keloid scar on the neck and arm before and after applying botulinum toxin.
Following the appearance of a skin wound, the physiological healing process comprises a series of overlapping phases that include inflammation, proliferation and maturation. The initial inflammatory phase begins at the very moment of the appearance of the injury, with the activation of the coagulation cascade and the release of cytokines that stimulate chemotaxis 6 of neutrophils and macrophages, responsible for the initial elimination of cellular waste and substances [13]. Exogenous to the affected area. After 48 to 72 hours, the proliferative phase begins, which lasts between 3 and 6 weeks. In it, the local recruitment of fibroblasts promotes the formation of a reparative support tissue, the extracellular matrix. This granulation tissue is made up of procollagen, elastin, proteoglycans and hyaluronic acid, which form a supporting structure to close the epidermal continuity solution and facilitate neovascularization. There is also an abundance of myofibroblasts differentiated from dermal fibroblasts in response to increased levels of Transforming Factor Beta (TGF-β), a cytokine involved in fibrosis processes in various organs. Myofibroblasts contain contractile microfilaments of muscle origin (actin) and help initiate wound reduction. During this repair period, an increase in local angiogenesis mediated by vascular endothelial growth factor is also observed [14].
When this proliferative phase ends, the scar enters a final maturation process, during which the initial extracellular matrix and immature type III collagen are gradually replaced by mature type I collagen, so that the progressive slowing of the initial healing processes lead to the formation of definitive, organized and functional scars [15].
It is known that various clinical variables influence the healing capacity of each patient, such as fertile women who heal worse than postmenopausal women and men, due to the influence of estrogens (mediated by an increase in TGF-β1); anatomical location, sex, age, negroid and mongoloid race heal worse than caucasians, size of the wound and local contamination.
Results and Discussion
Disc herniation is the exit of material from the nucleus
pulposus through the ruptured annulus fibrosus. Surgical
treatment is currently more clearly defined (cervical
microdiscectomy and laminectomy) and reserved for those few
patients who persist with increasing pain, progressive root injury
and spinal cord injury. As a general rule, the results of
interventions for disc herniation or extrusion have excellent or
good results in more than 90% of cases and are performed in the
anterior and lateral neck area. The skin incision is made
following a skin fold (to reduce the scar as much as possible). It
is rare that, as a consequence of the surgical intervention, due
to a complication, there are permanent neurological sequelae. It
can range from a clear increase in the loss of sensitivity and
strength in the area that hurt, to a permanent partial or total
spinal cord injury. At the level of cervical spine surgery, it may
happen that, despite a properly indicated and performed
intervention, pain persists that disables the person to carry out
their usual life. The causes of this post-surgical cervical pain
syndrome are very varied. They range from the entrapment of
the nerve root due to abnormal scarring, to psychological
phenomena or “rental neurosis” that make it impossible for the
person who works for someone else to resume their normal
working life. Healing has represented a challenge for medical
science, so far there is no therapeutic method that guarantees
100% scar removal, preventive management being the best
method to improve it. This study aims to find out that the
application of botulinum toxin in keloid scars can produce an
improvement in the functionality and aesthetics of the area
affected by the keloid scar.
Muscles can repeatedly distort wounds in the healing phase.
Botulinum toxin A chemoimmobilization is an ideal biochemical
agent that allows almost total elimination of muscle pull in the
healing wound. The goal of chemoimmobilization of skin
wounds is to eliminate dynamic stress on healing tissues to
improve and minimize stress for optimal cosmetic results.
However, the wound healing process is influenced by factors
other than muscle traction, such as skin phototype, the extent
and depth of the wound, its location and the direction of the
wound.
Botulinum toxin A has demonstrated its usefulness as a
treatment for multiple diseases, including blepharospasm,
spasmodic torticollis, dystonia and axillary and palmar
hyperhidrosis, among others. Its main indication and use is to
reduce glabellar and frontal expression lines in the aesthetic
field. However, in the last 10 years, the use of botulinum toxin A
to diminish the appearance of scars has grown considerably. The
justification for this is the decrease in the surface tension of the
wounds, which decreases ischemia at the edges and promotes a
better microenvironment (decreasing hypoxia and ischemia).
The improvement of the scars is due to an inhibition of the
contraction of the musculature below the wound, which
improves the microenvironment due to the decrease in wound
tension and less hypoxia. In addition, botulinum toxin A
increases the synthesis of blood Vessel Growth Factor (VEGF),
substance P and calcitonin release regulator gene (GRLC), which
stimulate the development of blood vessels.
Conclusion
It can be concluded from this research that healing
abnormalities are a health problem of great concern to surgeons
and their patients. Currently, there are numerous treatments
under development, such as botulinum toxin, considered an
effective therapeutic method in managing of scarring; provides
aesthetic and functional benefits in a scar after a surgical
procedure for cervical disc herniation based on the premise that
the wound healing process is influenced by the distraction of
muscle traction on immature collagen, so the application of this
muscle-paralyzing substance modulates the initial stages of the
wound-healing process by decreasing fibroblast proliferation
and inflammatory cell migration, while increasing angiogenesis.
References
- Hernandez U, Arellano AJ, Zaragoza AC, Flores HN, Juarez GZ, et al. (2014) Use of botulinum toxin in keloid scar. Surg Gen 36: 76-81.
[Google Scholar]
- Quintero-Larrovere MC, Flores-Sanchez E, Soto-Montenegro AE (2018) Effects of perilesional muscle relaxation with botulinum toxin type A on the healing of post-traumatic facial wounds. Cir Plast 44: 203-215.
[Google Scholar]
- Lebeda FJ, Dembek ZF, Adler M (2012) Kinetic and reaction pathway analysis in the application of botulinum toxin A for wound healing. J Toxicol 2012: 159726.
[Crossref] [Google Scholar] [PubMed]
- Kim YS, Roh TS, Lee WJ, Yoo WM, Tark KC (2009) The effect of botulinum toxin a on skin flap survival in rats. Wound Repair Regen 17: 411-417.
[Crossref] [Google Scholar] [PubMed]
- Osuna IB, Gonzalez RR, Alfonso MAM, Leon TG, Gonzalez JB, et al. (2013) Diagnostic evaluation in the postgraduate programs of the national center for minimum access surgery. Rev Cuba de Educ Medica Super 27: 46-53.
[Google Scholar]
- Valencia MR, Perez AM (2010) Cervical disc herniation. Rev Esp Cir Ortop Traumatol 54: 314-320.
[Google Scholar]
- Gutierrez AP, Bascones MG, Gutierrez RP, Jimenez MD (2019) Subcutaneous botulinum toxin in the treatment of peripheral neuropathic pain. Rehabilitacion 53: 131-135.
[Crossref] [Google Scholar]
- Ziade M, Domergue S, Batifol D, Jreige R, Sebbane M, et al. (2013) Use of botulinum toxin type A to improve treatment of facial wounds: A prospective randomised study. J Plast Recons Aesth Surg 66: 209-214.
[Crossref] [Google Scholar] [PubMed]
- Gassner HG, Sherris DA (2003) Chemoimmobilization: Improving predictability in the treatment of facial scars. Plast Recons Surg 112: 1464-1466.
[Crossref] [Google Scholar] [PubMed]
- Zhibo X, Miaobo Z (2009) Intralesional botulinum toxin type A injection as a new treatment measure for keloids. Plast Recons Surg 124: 275-277.
[Crossref] [Google Scholar] [PubMed]
- Beanes SR, Dang C, Soo C, Ting K (2003) Skin repair and scar formation: The central role of TGF-β. Expert Rev Mol Med 5: 1-22.
[Google Scholar] [PubMed]
- Colwell AS, Beanes SR, Soo C, Dang C, Ting K, et al. (2005) Increased angiogenesis and expression of vascular endothelial growth factor during scarless repair. Plast Reconstr Surg 115: 204-212.
[Google Scholar] [PubMed]
- Niessen FB, Spauwen PH, Schalkwijk J, Kon M (1999) On the nature of hypertrophic scars and keloids: A review. Plast Recons Surg 104: 1435-1458.
[Crossref] [Google Scholar] [PubMed]
- Strauch B, Herman C, Dabb R, Ignarro LJ, Pilla AA (2009) Evidence-based use of pulsed electromagnetic field therapy in clinical plastic surgery. Aesth Surg J 29: 135-143.
[Crossref] [Google Scholar] [PubMed]
- Ashcroft GS, Dodsworth J, Boxtel EV, Tarnuzzer RW, Horan MA, et al. (1997) Estrogen accelerates cutaneous wound healing associated with an increase in TGF-β1 levels. Nat Med 3: 1209-1215.
[Crossref] [Google Scholar] [PubMed]
Citation: Gomez JF, Cordero BJF, Santamaria LMB, Gomez LMV, Montes RJR, et al. (2023) Botulinum Toxin as a Management for Scars after Cervical
Disc Hernia Surgery. Health Sci J. Vol. 17 No. 9: 1060.