Keywords
Acne vulgaris; Arthritis; Isotretinoin; Sacroiliitis
Introduction
Isotretinoin (13-cis-retinoic acid) is a compound obtained from the derivation of retinoids. Having linked the target cell, acting together with the protein binding complex, retinol is oxidized to retinaldehyde by cytosolic or microsomal enzymes. Therefore, the reduction of retinaldehyde by the enzyme retinaldehyde dehydrogenase leads to the formation of retinoic acid and, originating a set of other physiologically important acids, such as tretinoin and isotretinoin. This substance is widely used by professionals and dermatologists for the control, reduction and treatment of severe acne, rosacea and resistant acne, as well as other dermatological disorders [1].
It is known that the increase in inflammatory cytokines stimulates the synthesis of matrix metalloproteinases (MMP), enzymes responsible for the breakdown of extracellular matrices in osteoarthritis and rheumatoid arthritis. Retinol and retinoic acid have been shown to induce MMP-2 activity, in which retinoic acid activity could not be reversed by antioxidants. The MMP-2 operates the type IV collagen in basement membrane degradation and, although present in low levels in healthy joint tissue is much more abundant in arthritic joints. As a derivative of retinoic acid, there is a possibility that isotretinoin stimulates MMP-2 activity and, consequently, degradation of the membrane in the joints [2,3].
The spondyloarthritis consist a group of chronic systemic inflammatory disease characterized by negativity of rheumatoid factor clinical findings such as inflammatory arthritis and enthesitis, for back pain and back pain of inflammatory nature, and is associated with the presence of human leukocyte antigen HLA B27. A arthritis it generates intense pain and discomfort at the end of the spine with gradual evolution, without specific laboratory markers that demonstrate its activity [4].
Case Report
The patient MGP, 17 years old, white, male, was admitted with a history of low back pain for 31 days with worsening in the last week, irradiation to the right thigh, with inflammatory rhythm accompanied by great difficulty in walking since the beginning of frame. He denied contact with infectious diseases, as well as a significant morbid past or current illness. He claimed to be using 40 mg of isotretinoin orally for 5 months.
On physical examination, he was in good general condition, with pale skin, fever and flushing in the facial region associated with pustules and moderate acne in the facial and thoracic region. The examination of the different devices showed no changes, except for severe pain in the right iliac fossa, with no signs of peritonism. He walked with extreme difficulty. The clinical evaluation of the right hip and lumbar spine was impaired due to the painful condition. The test Fabere and Gaenslen were positive right.
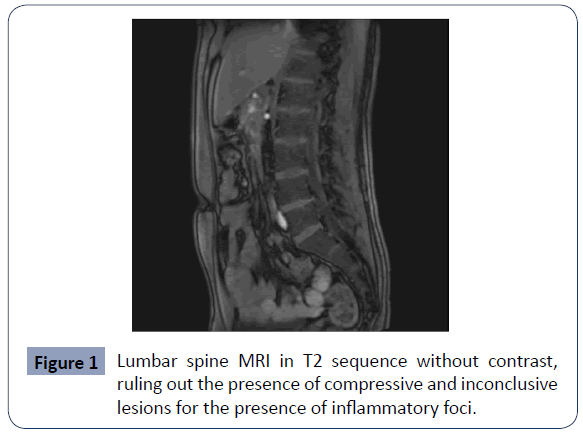
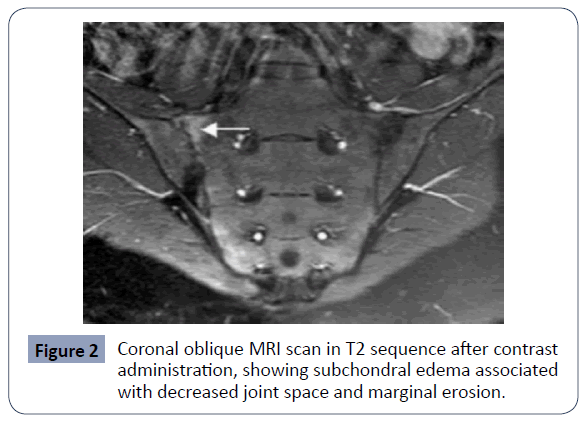
Laboratory evaluation showed normal count of leukocytes (8,490/mm3) without neutrophilia and Creative protein (PCR) 13.64 mg/l (v alues of 10 mg/L and 40 mg/L are compatible with rheumatic diseases) as well as v peed of h Emossedimentation (VHS) standard (10 mm in the 1st hour). He underwent hip radiography, ultrasound of the right hip and magnetic resonance imaging (MRI) of the lumbar spine without contrast, where no major changes were seen, including the right hip, and without evidence of collections/masses (Figure 1).
Figure 1: Lumbar spine MRI in T2 sequence without contrast, ruling out the presence of compressive and inconclusive lesions for the presence of inflammatory foci.
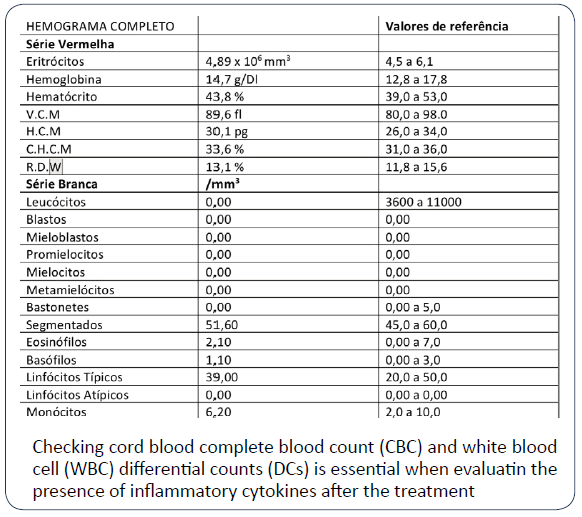
Due to the persistence of the clinical picture, without remission of pain complaints after a 24-hour surveillance period, MRI was performed with contrast of the sacroiliac region (Figure 2), where bone edema was seen on the right and left, with bulging of the anterior aspect of the synovial capsule associated with a liquid collection 5 mm in diameter, compatible with acute bilateral sacroiliitis [5].
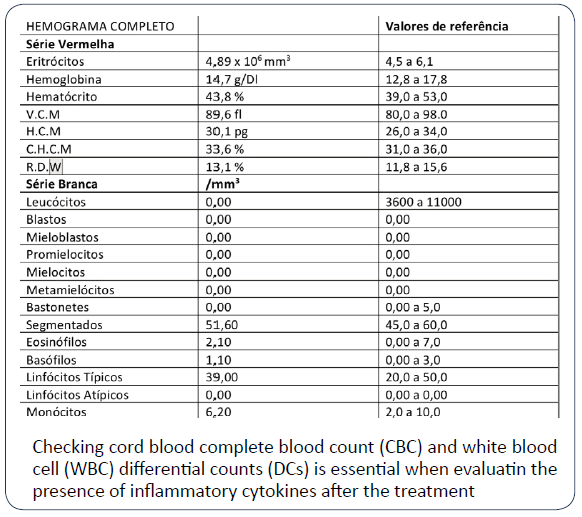
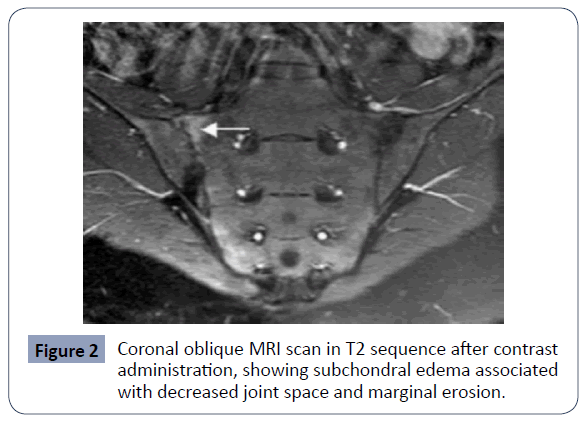
Figure 2: Coronal oblique MRI scan in T2 sequence after contrast administration, showing subchondral edema associated with decreased joint space and marginal erosion.
The patient was admitted to the rheumatology service where he started treatment with sulfasalazine 3.0 g/day, together with the immediate suspension of isotretinoin. Nimesulide 200 mg/day was administered for pain control. After 3 months of treatment, she was afebrile, still with periodic and reduced pain complaints, but with remission of the inflammatory condition from an analytical point of view (Figure 2). Currently, the patient is being followed up at the Rheumatology service, with no evidence of inflammatory recurrence or sequelae.
Discussion
Although bilateral symmetrical sacroiliitis can be seen in HLA-B27 negative patients, the presentation in this case is not characteristic of any of these disorders. The our patient did not show reactive arthritis, symptoms of inflammatory bowel disease, psoriasis, uveitis, conjunctivitis, peripheral arthritis compatible with ankylosing spondylitis, arthropathy Enteropathica or arthropathy psoriatic.
The mechanisms responsible for the induction of sacroiliitis by isotretinoin are not known. Although HLA-B27 has been proposed as a factor related to isotretinoin-induced sacroiliitis, this association has not been proven. The Our patient was negative for HLA-B27, as well as many other patients reported in the literature [6].
Arthasarathy suggested that isotretinoin is capable of altering the membrane structures of cells most susceptible to degenerative processes when exposed to mild trauma.
It is known that retinol and retinoic acid promote an increase in the activity of MMP-2, a family of Zn2+ - dependent endopeptidases, which promotes the degradation of the extracellular matrix, where the activity of retinoic acid could not be reversed by antioxidants. Desk that MMP-2 leads to type IV collagen basement membrane degradation in the cell and is normally most abundant in the joints with some form of arthritis. Being obtained from retinoic acid, there is a real possibility that the oral use of isotretinoin may stimulate MMP-2 activity and consequent degradation of the membrane of joint surfaces [2,3].
After starting treatment for analgesia and use of anti-inflammatory drugs, negative serological analysis for the presence of HLA-B27 antigen, which is present in approximately 10% of normal individuals, associated with the lack of clinical evidence to reinforce the diagnosis of ankylosing spondylitis, ruled out the diagnostic hypothesis [7,8].
Conclusion
The association between the use of isotretinoin and sacroiliitis has been previously reported by other authors (ref). In our report, we present evidence of the presence of sacroiliitis simultaneously with the use of isotretinoin, with complete resolution of the serological changes and the complete blood count after discontinuing the drug, despite persistent acne. The temporal association between treatment and symptom onset, combined with complete recovery after isotretinoin withdrawal, suggests that our patient had isotretinoin-induced sacroiliitis.
34958
References
- Costa CS , Bagatin E, Martimbianco ALC , da Silva EMK , Lúcio MM, et al. (2018) Oral isotretinoin for acne. Cochrane Database of Systematic Reviews.
- Levinson M, Gibson A, Stephenson G (2014) Sacroiliitis secondary to isotretinoin. Australas J Dermatol 53: 298-300.
- Health Surveillance Agency (2016) Roacutan :Isotretinoin. Label for Health Professionals. Laboratório Roche.
- SelçukLB, Arıca DA, Şahin HB, Yaylı S, Bahadır S (2017) The prevalence of sacroiliitis in patients with acne vulgaris using isotretinoin. Cutan Ocul Toxicol 36:176-179.
- Montandon C, Costa MAB, Carvalho TN, JúniorI MEM, Teixeira KS (2007) Sacroiliitis: imaging evaluation. Radiologia Brasileira 40: 53-60.
- Rozin AP, Kagna O, Shiller Y (2010) Sacroiliitis and severe disability due to isotretinoin therapy. Rheumatol Int 30: 985-986.
- Geller ASB, Alagia RFN (2013) Sacroiliitis after use of oral isotretinoin-association with acne fulminans or adverse effect? An Bras Dermatol 88: 193-196.
- Yılmazer B, Coşan F, Cefle A (2013) Bilateral acute sacroiliitis due to isotretinoin therapy: a case report. Int J Rheum Dis 16: 604-605.