Harutyunyan L, Meliksetyan
K, Oganesyan A, Oseyan
H, Khachatryan H and
Hakobyan Y**
Department of Hematology and
Transfusion Medicine, National Institute
of Health, Yerevan 0051, Armenia
- *Corresponding Author:
- Hakobyan Y
Department of Hematology and Transfusion
Medicine, National Institute of Health,
Yerevan 0051, Armenia
Tel: +37477450683
E-mail: yero75@yahoo.com
Received Date: October 11, 2021; Accepted Date: October 23, 2021; Published Date: October 29, 2021
Citation: Harutyunyan L, Meliksetyan K,
Oganesyan A, Oseyan H, Khachatryan H,
et al. (2021) Case Report: LDAC for the
Treatment of Post-Splenectomy Newly
Diagnosed PMF Patent with Oral Treatment
Inability. Health Sci J. 15 No. 10: 889.
Keywords
Myelofibrosis; Splenectomy; Thrombosis; Cytarabine; Treatment
Abbreviations: AML: Acute Myeloid Leukemia, CBC: Complete Blood Count; ESR: Erythrocyte Sedimentation Rate; HGB: Hemoglobin; HMA: Hypomethylating Agent; LDAC: Low Dose Cytarabine; LDH: Lactate Dehydrogenase; MPN: Myeloproliferative Neoplasms; RBC: Red Blood Cells; PLT: Platelets; PMF: Primary Myelofibrosis; WBC: White Blood Cells
Introduction
Primary myelofibrosis (PMF) is a hematologic malignancy belonging to Ph negative myeloproliferative neoplasms (MPN), and it is commonly characterized by a higher risk of acute myeloid leukemia (AML) transformation [1]. According to NCCN Guidelines 2021, if disease progression to an advanced phase or AML occurs, treatment for non-transplant candidates includes three main options: hypomethylating agent (HMA) with or without JAK inhibitors, low-intensity chemotherapy, or a clinical trial with novel agents [2].
Case Report
A 65-year-old man was admitted to the hematology center on 09.04.2021 with complaints of abdominal pain on the upper left side and sweating. His medical history was significant for femoral endarterectomy and left leg amputation due to severe venous thrombosis 5 years ago. On the admission day, ultrasound and CBC revealed splenomegaly (37 × 19 cm with splenic vein of 1.9 cm), normochromic anemia (HGB=89g/L, RBC=2.95×1012/L), mild leukocytosis (WBC=14,820, neutrophils 13.31 × 109/L, myelocytes=2%, metamyelocytes=4%, bands=12%, segmented neutrophils=70%, lymphocytes=4%, and monocytes=8%) with normal PLT (199 × 109/L), and elevated ESH (32mm/h), respectively. Deficiency anemias were subsequently excluded. Physical examination showed paleness of the skin and mucous membranes with palpable edges of the spleen and liver. The biochemical evaluation found elevated levels of LDH (590U/L) and uric acid (8.4mg/dL). Coagulation tests, urinalysis, and testing for common infections (e.g., HBV, HBC, HIV, brucellosis, syphilis) were normal.
Prior to hematologic follow-up, the patient was sent to the Hepatobiliary department for a consultation, and an urgent splenectomy was indicated by a surgeon based on a significantly enlarged spleen, which was performed on 06.05.2021. Based on two pathohistological analyses of the liver, spleen, and adjacent lymph node biopsy materials, the patient was diagnosed with liver cirrhosis and PMF, MF-3. BCR/ABL1 was negative with PCR, while JAK2 V617F, CALR, and MPL mutations were planned but still not performed because of the patient’s financial constraints [3].
On 25.05.2021, the patient presented to the hematology center with swelling and pain in the amputated leg. Duplex ultrasound scan showed thrombosis in vena cava inferior, with elevated levels of D-dimer (2.37 mcg/mL), ATIII (117%) homo cysteine (19.99 umol/L). Medical treatment started with daily doses of hydroxyurea 1000 mg, allopurinol 300mg, nadroparin 0.6mL × 2x, aspirin 100 mg, amoxicillin-clavulanate 1000mg × 2x for 3 weeks, and vaccinations recommended for patients following splenectomy [4,5]. Hyperhomo cysteinemia was managed with vitamin complex therapy. After 7 days of treatment, no changes in CBC were observed; however, D-dimer decreased to 1.56 mcg/ mL. The dose of hydroxyurea was adjusted to 2000mg daily, while other medications remained with the same dose.
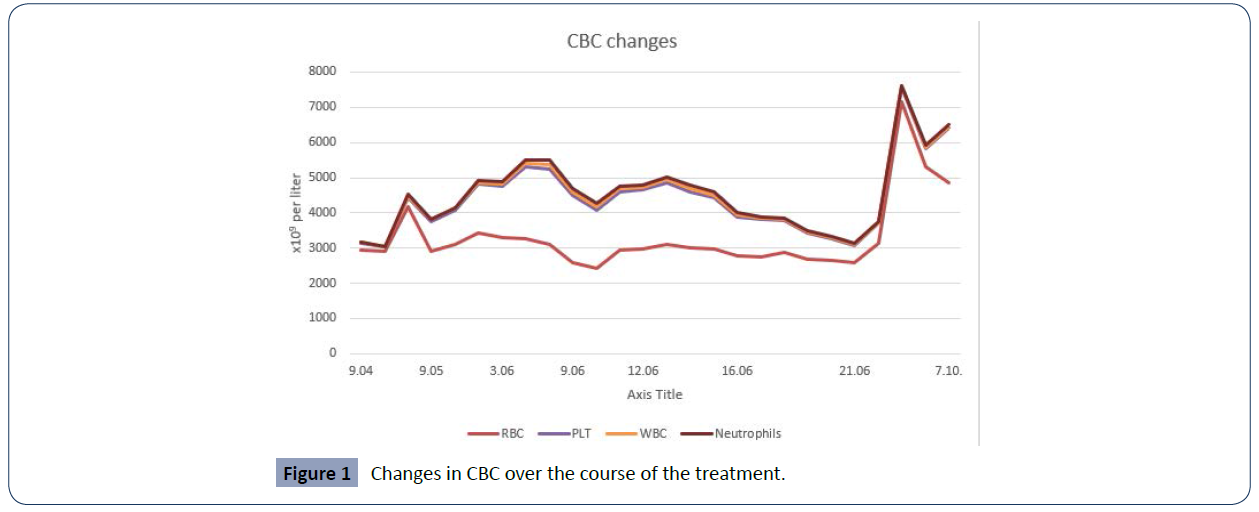
On 07.06.2021 the patient was brought to the ICU of the hematology center with complications of severe pneumonia, uncontrolled leukocytosis (WBC=101.74 × 109/L with 95% of neutrophils) and thrombocytosis (PLT=2,036 × 109/L), renal failure (Creatinine=218 mc mol/L, BUN=22 mmol/L), vomiting, and melena. Aspirin was discontinued and nadroparin 0.6 × 2 was combined with plasma transfusions. Abdominal CT scan demonstrated intestinal obstruction of an adhesive character with a transudate in perihepatic, post-splenectomy parts, abdominal lymphadenopathy, flush-fill liver hemangioma in the S7 segment. Esophagogastroduodenoscopy showed hyperemic prepyloric parts with solitary erosions of 0.1-0.2 cm but no obstruction. Barium contrast X-Ray: no intestinal obstruction. The surgeon considered a dynamic intestinal obstruction and advised symptomatic treatment. Chest CT scan was significant for left lung discoid atelectasis in the postero dorsal segment, right side minimal hydrothorax accompanied with passive atelectasis, and patterns of pulmonary aspergillosis. Repeated duplex ultrasound demonstrated that thrombosis remained in the common iliac vein bilaterally (Figure 1).
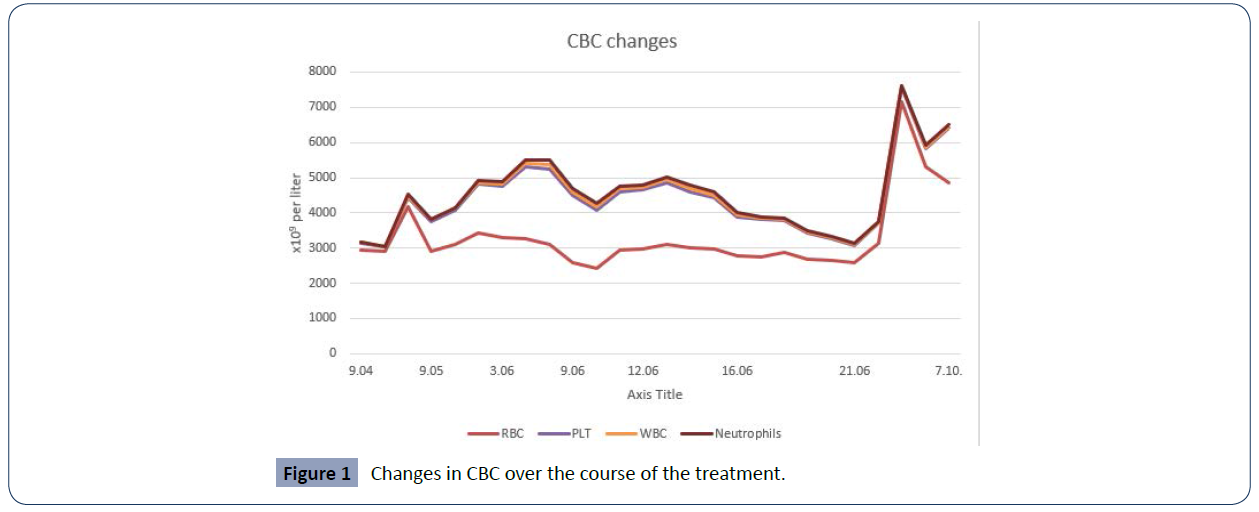
Figure 1 Changes in CBC over the course of the treatment.
Due to severe vomiting, oral supplementation medication intake became impossible. Thus, along with a supportive treatment for bronchopneumonia, including voriconazole and antibiotics, intestinal obstruction, and renal failure, the decision was made to start a low dose cytarabine (LDAC) therapy (20mg cytarabine every 12 hours for 10 days, intracutaneous administration), considering abnormal levels of PLT (1893 × 109/L) and WBC (107.32 × 109/L). Treatment response was observed already on day 5 since the initiation of the therapy, and by the time of patient discharge, both PLT (491 × 109/L) and WBC (22.83 × 109/L) were remarkably reduced and remained stable for the next three months. Currently, the patient receives hydroxyurea (2000 mg/ day) and 100 mg/day aspirin and remains under ambulatory supervision. The JAK2 V617F mutation is positive, and the addition of Ruxolitnib to the treatment plan is currently underway.
Conclusion
LDAC may be considered a good choice for the management of PMF patients after splenectomy in which oral intake is compromised regardless of disease transformation and in the context of posts plenectomy. Future large-scale studies are required to confirm these findings. Figure 1 Changes in CBC over the course of the treatment.
40911
References
- Iurlo A, Cattaneo D, Gianelli U (2019) Blast Transformation in Myeloproliferative Neoplasms: Risk Factors, Biological Findings, and Targeted Therapeutic Options. Int J Mol Sci 20: 1839.
- Mesa RA, U, Shammo JM, Vachhani P, Verstovsek S (2021) Recent Updates to NCCN Guidelines on MF Treatment. OncLive eNewsletter.
- Szuber N, Tefferi A (2018) Driver mutations in primary myelofibrosis and their implications. Curr Opin Hematol 25: 129-135.
- Bonanni P, Grazzini M, Niccolai G, Paolini D, Varone O, et al. (2017) Recommended vaccinations for asplenic and hyposplenic adult patients. Hum Vaccin Immunother 13: 359-368.
- Gill H, Leung GMK, Yim R, Lee P, Pang HH, et al. (2020) Myeloproliferative neoplasms treated with hydroxyurea, pegylated interferon alpha-2A or ruxolitinib: clinicohematologic responses, quality-of-life changes and safety in the real-world setting. Hematology 25: 247-257.