Sylvia Chibuye1,3*, Panji Nkhoma1, Marah Simakando1, Jacob Ndhlovu1,4, Sumbukeni Kowa1,2 and Bellington Vwalika1,2
1The University of Zambia, School of Medicine, P.O Box 50110,10101 Lusaka, Zambia
2The University Teaching Hospital, Private Bag RW1X,Ridgeway, Nationalist road, Lusaka, Zambia
3Evelyn Hone College, School of Medicine, P.O Box 30029, Lusaka, Zambia
4Eden University, School of Medicine and Health Sciences, P.O Box 37727,Lusaka, Zambiap
- *Corresponding Author:
- Sylvia Chibuye
The University of Zambia, School of Medicine, P.O Box 50110, 10101 Lusaka, Zambia
Tel: +260968760070
E-mail: mwenyachibuye@yahoo.com
Received Date: February 05, 2021; Accepted Date: February 18, 2021; Published Date: February 24, 2021
Citation: Chibuye S, Nkhoma P, Simakando M, Ndhlovu J, Kowa S, Vwalika B (2021) Circulating Micro particles: a Risk Factor for Recurrent Abortion in Women at the University Teaching Hospital, Lusaka, Zambia. Health Sci J. 15 No. 1: 803.
Keywords
Circulating micro particles; Recurrentabortion; Women
List of abbreviations: CI: Confidence Interval; FACS: Fluorescence Activated Cell Sorter; FITC: Fluorescein Isothiocyanate; MP: Micro particles; SD: Standard Deviation
Introduction
Spontaneous abortion is the most common complication of early pregnancy [1-4]. The American Society for Reproductive Medicine (2008) defines recurrent abortions as two or more failed pregnancies prior to 20 or even 28 weeks of pregnancy as it currently is in Zambia, the pregnancy loss should have been documented by either ultrasound and/or histopathological examination [5]. Scientists have hypothesised that some cases of recurrent abortion are due to defective maternal haemostatic response leading to thrombosis in the uteroplacental bed thereby leading to placental insufficiency and ultimately fetal loss [6]. Various pregnancy complications, including pregnancy loss, may be associated with procoagulant changes in general, rather than congenital or acquired thrombophilias in particular [5].
Circulating micro particles are a heterogeneous group of small membrane-coated vesicles, released from cell membranes upon activation or apoptosis leading to externalisation of phospholipids such as phosphatidylserine [7,8]. Phosphatidylserine expressed on the surfaces of microparticles amplifies the procoagulant and/ or inflammatory response on the endothelial surface by providing a catalytic surface which promotes assembly of procoagulant proteins and stimulates coagulation reactions [2].
Studies like that of Laude et al [7] have measured the total microparticles in women with a history of recurrent pregnancy loss compared with controls, and found microparticle levels to be above the upper limit of normal in 59% of patients. This study agrees with another study by Pasquier et al [9], that found a higher number of microparticles in women referred for unexplained pregnancy loss as compared to that of parous women.
The World Health Organisation has over time estimated the regional and global occurrence of miscarriages and as of the year 2000, 19 million spontaneous abortions took place. These abortions were approximate to one abortion to every 10 pregnancies [1]. The University Teaching Hospital receives approximately 500 abortion cases monthly of which more than half of these cases are unexplained pregnancy losses. This study aimed to assess the relationship of circulating microparticles in recurrently miscarrying women, compared with that of parous control women at The University Teaching Hospital in Zambia. Identifying women at risk of abortion and therefore, requiring special obstetric and gynaecology management could be a step towards curbing this problem.
Materials and Methods
Patients
Between May 2016 and July 2016, a case-control study was carried out at The University Teaching Hospital, Obstetrics and Gynecology emergency ward. A total of 18 women were recruited as cases defined as women more 18 years of age that had suffered two or more recurrent abortions with unknown possible cause attending the Obstetrics and Gynaecology emergency ward at The University Teaching Hospital. Only women whose pregnancy loss had no known cause after laboratory investigations were included in this study. Hospital based controls were drawn from women more than 18years of age having at least two live births and no history of pregnancy loss. In total 55 controls were enrolled.
The University of Zambia Biomedical Research Committee review board approved the study.
Laboratory testing
Circulating microparticles were measured in platelet poor plasma, 48 hours after the previous abortion. 3ml of blood was collected from both cases and controls and gently mixed in a sodium citrate vacutainer. The blood samples were isolated by a two cycle centrifugation process, the first centrifugation cycle was for 10 minutes at 1500rpm and the second was at 1300rpm for 5 minutes. The platelet poor plasma was stored at -35oC until analysis and the remaining sample was discarded.
The reagents were brought to room temperature before the procedure. Aliquots of 30μl platelet poor plasma were incubated for 30 minutes at room temperature in the dark with 10 μl Annexin V Fluorescein Isothiocyanate (FITC). After incubation was complete, samples were diluted in 500 μl of annexin V binding buffer solution (1:10 in distilled water). In order to express microparticle counts as absolute numbers per microliter of plasma, 30 μl of counting beads with an established concentration close to 1000 beads/μl was added to each sample (Count Bright™ absolute counting beads, Life Technologies, Canada). The sample was vortexed at a low frequency for 10 seconds and the number of fluorescence-positive microparticles in the stained samples quantified by the Becton Dickinson FACS Calibur (Fluorescence Activated Cell Sorter) after 10, 000 events.
Statistical analysis
An increased level of MPs in both cases and controls was defined as a level >2 standard deviation (SD) from the mean of control women [10]. MP levels in cases were compared with controls using the unpaired t-test, where statistical significance was assumed at P?0.05, 95% confidence interval (CI).
Data was analysed using SPSS version 16 software.
Results and Discussions
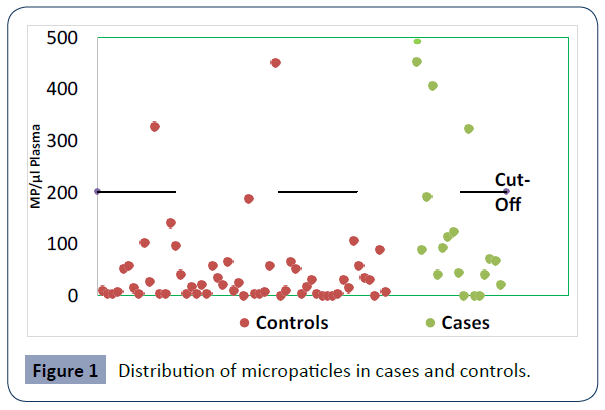
Microparticle distribution in the peripheral blood of both cases and controls was parametric, ranging from 0 to 495/μl in cases and 0 to 451/μl in controls. Levels >2 SD from the mean of control parous women were considered to be abnormal. The cut-off value was found to be at 202MPs/μl. Four of the 18 cases had an increased number of MPs 22(%) as compared to 2/55 controls 4(%) (P=0.022). A scatter plot of MP levels in both cases and controls is demonstrated in Figure 1. A larger proportion of cases with recurrent abortion had raised microparticle levels as compared to controls.
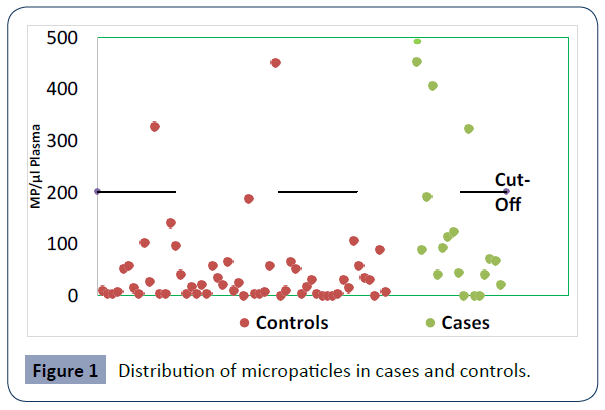
Figure 1 Distribution of micropaticles in cases and controls.
MP=Microparticles
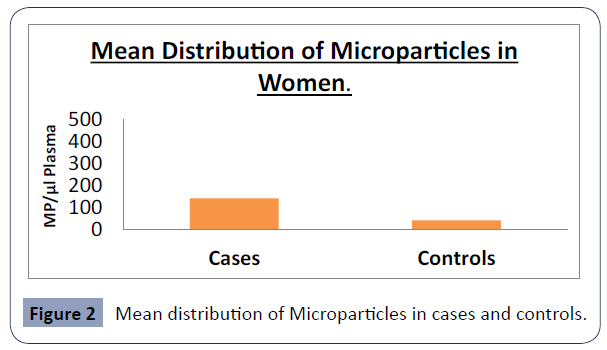
Among women at the University Teaching Hospital (Total=73) there was a statistical significance between the two groups of women, Cases (mean=142.94, SD=162.594) and controls (mean=43.80, SD=78.977), t(20)=2.49, P=0.022, 95% CI 182.20- 16.09. This is demonstrated in Figure 2.
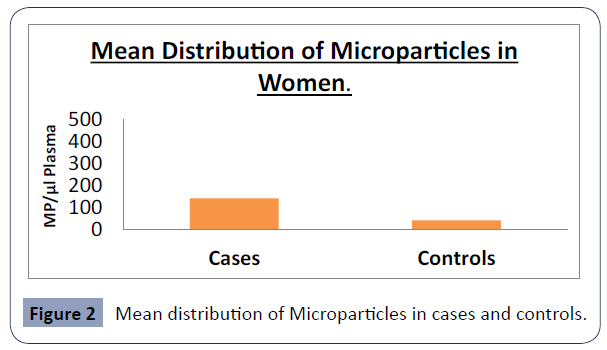
Figure 2 Mean distribution of Microparticles in cases and controls.
Discussion
Findings in this study showed that women with two or more pregnancy losses had a higher number of microparticles (22%) as opposed to control women (4%) who had two or more live births, indicating that microparticles are associated with pregnancy loss P=0.022.
Findings from this study were similar to a study by Carp et al (2004) where cases (12.5%) had a higher number of microparticles than controls (2.2%). Similarly, a study by Pasquier et al [9] compared microparticle levels of women referred for unexplained pregnancy loss with those of parous women. This study like previous studies that focused on annexin V-FITC positive microparticles also found higher levels of microparticles in women with recurrent abortions as compared to parous women. Laude et al[7]carried out a study to investigate the relationship between microparticles and women with unexplained pregnancy losses. A total of 74 women with recurrent abortions were sampled and phosphatidylserine-positive microparticles measured using annexin V-FITC. Forty-one of the 74 women had increased levels of microparticles, with 29 (59%) being associated with early pregnancy loss. The lower prevalence in the current study (22%) than that of the study by Laude et al [7] may be due to assessing microparticles in women 24hrs after either an abortion or a live birth, rather than 3 months after either a spontaneous abortion or a live birth. This study concentrated on assessing microparticles also immediately after the occurrence in order to investigate the plausibility of measuring microparticle quantity in these women for diagnostic purposes given microparticles are associated with unexplained pregnancy loss.
Haemostatic changes that occur after pregnancy loss tend to normalise 3 to 4 weeks after the event and as such microparticles have been suspected to also normalise. Also, due to the highly thrombogenic nature of microparticles, they tend to get consumed through the processes of excessive clotting initiation and activation in the placental bed and thus a majority of the microparticles would be trapped in fibrin deposits explaining the lower prevalence of microparticles assessed at the time of diagnosis. Alijotas Reig et al [11] assessed microparticles at the time of diagnosis and found a decreased number of endothelial microparticles in the group of pregnancy loss, which lead them to conclude that there was no association. It is important to note that this study measured total number of microparticles and not just endothelial microparticles, thus explaining why this study found increased microparticles and an association between microparticles and unexplained pregnancy loss. The ideal time for collecting samples for microparticle analysis could therefore be at least 4 weeks after pregnancy loss.
Conclusions
The results of this study suggest that that increased levels of microparticles in peripheral circulation of women with two or more unexplained pregnancy losses regardless of it being an early loss or a late loss, supports emerging evidence that microparticles have a role to play in abortion. This shows a promising approach to the use of microparticles as markers for risk of recurrent abortion.
Declarations
Ethical approval was sought from The University of Zambia – Biomedical Research Ethics Committee. Consent was granted by The University Teaching Hospital administration and permission to collect samples from the Obstetrics and Gynaecology at The University Teaching Hospital (UTH).
Ethics approval and consent to participate
Ethical approval was sought from The University of Zambia - Biomedical Research Ethics Committee under reference number 008-03-16. Consent was granted by the University Teaching Hospital administration and permission to collect samples from the Obstetrics and gynaecology wards was sought from the Head of the Department of Obstetrics and Gynaecology at the University Teaching Hospital (UTH). Written informed consent was obtained from all the participants in the study.
Consent for Publication
Not applicable
Availability of Data and Materials
All data analysed during the current study is available from the corresponding author on reasonable request.
Competing Interests
The authors declare that there have no competing interests.
Funding: Not Applicable
Authors' Contributions
The study was designed by SK and BV. The samples were run and processed by SC with TK supervising the study. The manuscript was written and edited by SC, SK, BV, TK and MS.
All authors have read and approved the final manuscript.
Acknowledgements
The authors wish to thank the Obstetrics and Gynaecology department for the help during sample collection and The University Teaching Hospital-Paediatric Centre of Excellence Laboratory staff members for providing the equipment and assistance with sample processing. And most importantly The Chibuyes’ for funding this study.
35448
References
- Alijotas-Reig J, Palacio-Garcia C, Farran-Codina I, Zarzoso C, Cabero-Roura L, et al. (2011) Circulating cell-derived microparticles in women with pregnancy loss. Am J Reprod Immunol 66: 199-208.
- Castellana D, Kunzelmann C, Freyssinet JM (2009) Pathophysiologic significance of procoagulant microvesicles in cancer disease and progression. Hamostaseologie 29:51-57.
- Carp H, Dardik R, Lubetsky A, Salomon O, Eskaraev R, et al. (2004) Prevalence of circulating procoagulant microparticles in women with recurrent miscarriage: a case–controlled study. Hum Reprod 19:191-195.
- Doubilet PM, Benson CB, Bourne T, Blaivas M (2013) Diagnostic criteria for non-viable pregnancy early in the first trimester. N Engl J Med 369:1443.
- Greer IA (2001) Thrombosis in pregnancy: maternal and fetal issues. Lancet 353: 1258-1265.
- Jy W, Horstman LL, Ahn YS (2010) Microparticle size and its relation to composition, functional activity, and clinical significance. Semin Thrombi Hemostat 36: 876-880.
- Laude I, Rongieres-Bertrand C, Boyer-NeumannC, Wolf M, Mairovtz V, et al. (2001) Circulating procoagulantmicroparticles in women with unexplained pregnancy loss: a new insight. Thrombi Haemostat 85: 18-21.
- Mause SF, Weber C (2010) Microparticles: protagonists of a novel communication network for intercellular information exchange. Circ Res 107:1047-1057.
- Pasquier E, Martin L, Bohec C, Collet M, George FD, et al. (2013) Unexplained pregnancy loss: a marker of basal endothelial dysfunction. Fertil Steril 100:1013-1017.
- Patil R, Ghosh K, Satoskar P, Shetty S (2013) Elevated Procoagulant Endothelial and Tissue Factor Expressing Microparticles in Women with Recurrent Pregnancy Loss. PLoS ONE.
- Robertson L, Wu O, Langhorne P, Twaddle S, Clark P, et al. (2006) The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) Study. Thrombophilia in pregnancy: a systematic review. Br J Haematol 132:171-196.