Keywords
Coronavirus disease; Morbidity; Mortality; New york city
Background
Since the first laboratory confirmed Coronavirus Disease 2019 (COVID-19) –related death on March 11, 2020 [1], COVID-19 has triggered significant social, political, and economic upheaval in the lives of people who live, work, and play in NYC. As of May 25, 2020, over 196,098 persons have been infected, resulting in 51,197 hospitalization and 16,482 laboratory-confirmed deaths [2]. According to the New York City Department of Health and Mental Hygiene [2] data, the city’s poor and vulnerable communities experienced exceedingly high rates of morbidity and mortality due to the pandemic.While COVID-19 infection rates among the 44+ age group in NYC were similar, there was a significant disparity in mortality rates, 184 per 100,000 in adults ages 44-64 vs. 1,055 per 100,000 in adults ages 65 and older [2]. Similarly, mortality rates were disproportionately higher among men at 255 per 100,000 compared to women at 155 per 100,000. Mortality rates were higher among people who identify as Latinx (230 per 100,000) and Black (218 per 100,000), compared to White (109 per 100,000) and Asian (102 per 100,000). There was a steady increase in COVID-19 cases, hospitalization, and death rates associated with incremental, increased poverty levels [3].
There are two community districts in Queens that have faced alarming COVID-19 incidence and mortality. District 4, specifically Corona, had the highest rate of COVID-19 infections in the borough and New York City, accounting for an average rate of 4895 cases per 100,000. As of June 11, 2020, the average mortality rate was 442 per 100,000. District 14, specifically Far Rockaway, accounted for an average rate of 2535 cases per 100,000, considerably less than District 4, and an average mortality rate of 476 per 100,000, the highest in the borough and the city [3]. We know that severe illness and deaths due to COVID-19 are caused mainly by underlying medical conditions such as heart disease, lung disease, cancer, diabetes, immunodeficiency, kidney disease, and liver disease [3]. However, it is unclear why District 4 had the greatest number of COVID-19 cases, and District 14 had the highest rate of deaths in the city. This study examines and compares underlying community-level factors of these two districts, such as demographics, health status, access to healthcare, socioeconomic conditions, and environmental characteristics.
Methods
We conducted a descriptive cross-sectional study. The data collected were retrieved from NYCDOHMH and aggregated by Community Districts, which encompass multiple towns. In this case, District 4 includes Corona and Elmhurst. District 14 includes Far Rockaway, Arverne, Edgemere, Broad Channel, and Breezy Point. Therefore, the data was retrieved using zip codes that were matched to each District.
Districts 4 and 14 were examined using public data extracted from the NYCDOHMH Community Health Profiles and New York University (NYU) Furman Center on June 11, 2020. The data from the NYCDOHMH Community Health Profiles contain information on health status, access to healthcare, and socio-economic conditions such as poverty, unemployment, and education [4,5].
Health status was defined using self-reported health status, obesity, diabetes, hypertension, avoidable hospitalizations (from diseases that could be addressed in primary care), and psychiatric hospitalizations. Premature deaths from 2011-2015 were also included as the health status of the Districts. Access to healthcare was defined based on residents’ health insurance status. Poverty, unemployment, and education were used to measure socioeconomic status. Poverty was defined as the total pre-taxed income for a family that falls below the government threshold. Unemployment was defined as whether a person is employed in the last week.
We collected information on environmental characteristics such as housing units, rent burden, and severe overcrowding from NYU Furman Center, which uses data from the American Community Survey (ACS) and defined communities by districts. Severe overcrowding was defined as more than 1.5 household members in each room per unit.Rent burden referred to the rent in households whose gross rent (including electricity and heating fuel costs) was equivalent to at least 50 percent of their income. Housing units referred to the number of housing units as separate living quarters.
We conducted a descriptive analysis using all variables in the study. NYCDOHMY had already performed bivariate data analysis using a t-test comparing the rates of each community district. The difference in the variables was considered statistically significant if p-values were ≤ 0.05.
Results
Table 1 displays the public data from NYCDOHMH and NYU Furman Center, providing descriptive statistics for Districts 4 and 14 with regards to community-level indicators such as health status, access to healthcare, socioeconomic status, and environmental characteristics.
| |
District 14 |
District 4 |
| Demographics |
% |
% |
| Population |
n=114390 |
n=188107 |
| Foreign born |
26% |
63% |
| Limited English Proficiency |
13% |
51% |
| Race* |
| Asian |
3% |
36% |
| Black |
40% |
5% |
| Latinx |
22% |
51% |
| White |
33% |
6% |
| Other |
2% |
1% |
| Age* |
| 0-17 |
26% |
21% |
| 18-24 |
8% |
9% |
| 25-44 |
25% |
33% |
| 45-64 |
26% |
25% |
| 65 and older |
14% |
11% |
| COVID-19 Characteristics |
| COVID-19 incidence |
2535/100000 |
4895/100000 |
| COVID Deaths |
476/100000 |
442/100000 |
| Health Status |
| Good, Better, Very Good or Excellent |
75% |
68% |
| Obesity |
32% |
19% |
| Diabetes |
15% |
11% |
| Hypertension |
34% |
23% |
| Avoidable Hospitalization |
1345/100000 |
892/100000 |
| Psychiatric Hospitalization |
1158/100,000 |
440/100,000 |
| |
| Access to Healthcare Characteristics |
| Uninsured |
11% |
25% |
| |
| Mortality Characteristics |
| Premature Mortality |
269/100,000 |
105/100,000 |
| Heart Disease |
75/100,000 |
16/100,000 |
| Cancer |
57/100,00 |
35/100,000 |
| Diabetes |
- |
3/100,000 |
| Suicide |
- |
4.4/100,000 |
| Drug-related Conditions |
12.4/100,000 |
- |
| Life Expectancy (years) |
77 |
86 |
| Socioeconomic characteristics |
| Poverty |
18% |
27% |
| Unemployment |
8% |
6% |
| Education |
|
|
| Less than High School Diploma |
22% |
30% |
| High School and Some College |
43% |
42% |
| College Degree |
35% |
28% |
| |
| Environmental characteristics |
| Severe crowding rate |
3% |
12% |
| Rent Burden |
26% |
35% |
| # of Housing units |
n=46,463 |
n=48,857 |
*Note: Percentages may not sum up to 100% due to rounding.
Table 1 Descriptive statistics including demographics, COVID-19 cases, health status, access to healthcare, mortality, socioeconomic and environmental characteristics across two districts in Queens, NY.
Demographics
District 4 is majority Latinx, representing 51% of the population, followed by Asians at 36%, Whites at 6%, and Blacks at 5%.Foreign-born represented 63%, 51% experienced limited English proficiency, and 30% of residents have less than a high school diploma.In District 14, Blacks represented 40% Whites 33%, Latinx 22%, and Asian 3%. Foreign-born represented 26%, 22% of residents have less than a high school diploma, and 13% have limited English proficiency. Furthermore, there were no evident differences in age distribution between the two districts.
Health status/access to healthcare characteristics
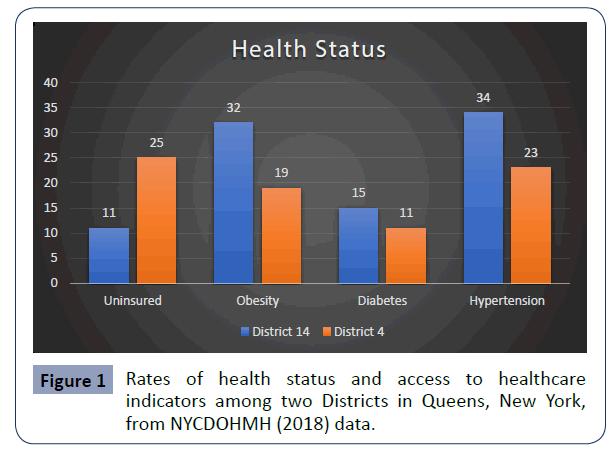
Self-reported physical and mental health status (using these responses: “Good,” “Very Good,” or “Excellent”) was different in District 4 than in District 14 at 68% and 75%, respectively. Avoidable hospitalizations were more frequent in District 14 with rates of 1,345 per 100,000 than in District 4 with rates of 892 per 100,000. Similarly, significant health disparities were found in the rate of psychiatric hospitalizations in District 14 at 1,158 per 100,000 compared to District 4’s rate of 440 per 100,000. Furthermore, there were differences found among preexisting conditions directly associated with COVID-19 deaths, as shown in Figure 1. For example, about 32% of District 14 inhabitants were found to be obese compared to 19% in District 4. The occurrence of hypertension (34% vs. 23%)and diabetes (15% vs. 11%) was more frequent in District 14 than District 4 (Figure 1).
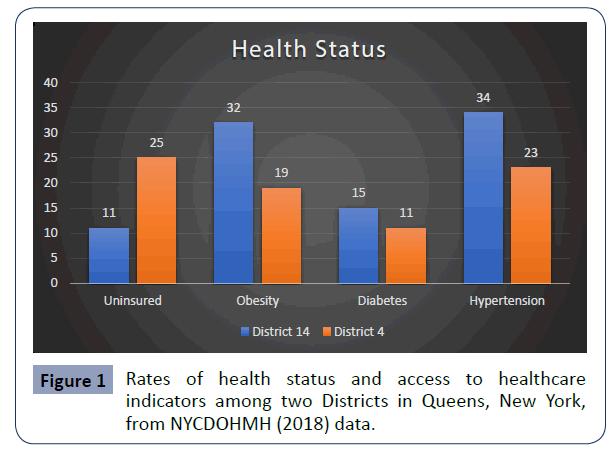
Figure 1 Rates of health status and access to healthcare indicators among two Districts in Queens, New York, from NYCDOHMH (2018) data.
Other health metrics, however, show greater differences. The premature mortality rate in District 14 (269 per 100,000) was twice that in District 4 (105 per 100,000). District 14 also had higher mortality rates due to heart diseases (75 per 100,000 vs. 16 per 100,000) and cancer (57 per 100000 vs. 35 per 100000) than District 4. Lastly, the average life expectancy in District 14 was 77 years compared to 86 years in District 4.
Socioeconomic characteristics
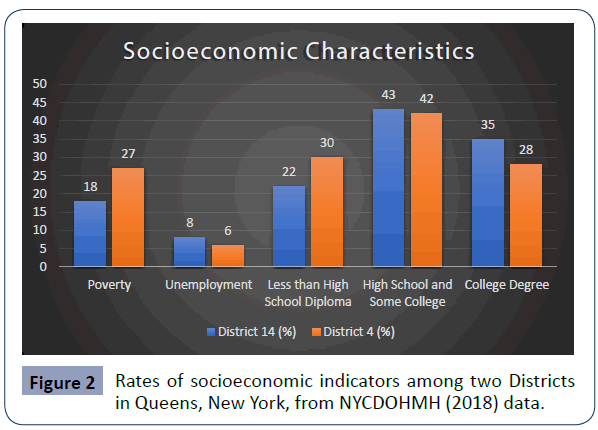
Based on NYCDOHMH Community District Health Profile, 30% of residents in District 4 have less than a high school diploma, which is almost 30% greater than District 14, as shown in Figure 2. Conversely, District 14 has slightly more college-educated residents than District 4. Regarding poverty, District 4 is 33% more impoverished than District 14. However, the incarceration rate among residents 16 years and older was disproportionately higher in District 14 than District 4 at 824 per 100,000 and 227 per 100,000 (Figure 2).
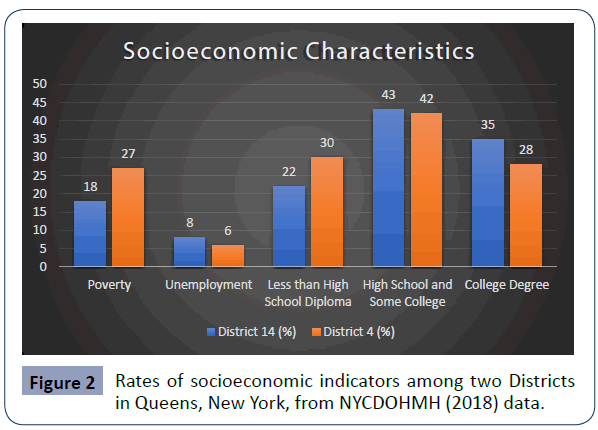
Figure 2 Rates of socioeconomic indicators among two Districts in Queens, New York, from NYCDOHMH (2018) data.
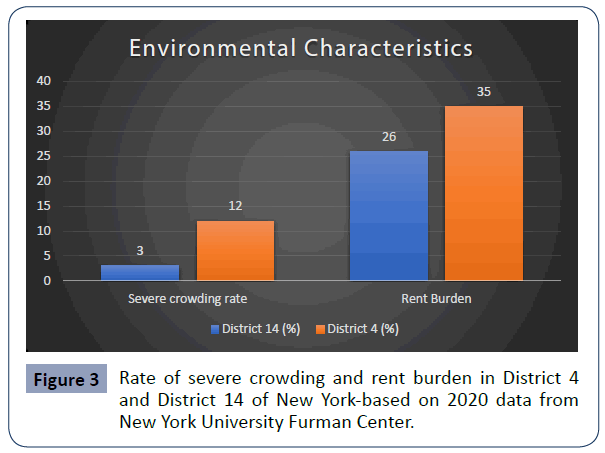
Environmental characteristics
Districts 14 & 4 have comparable housing units, 46,463 and 48,857, respectively. While District 4 reporteda 12% severe overcrowding rate (based on the five-year American Community Survey estimates) than District 14 (3%), as shown in Figure 3 [5]. Furthermore, the rent burden was greater in District 4 (35% vs. 26%). District 14 lacks healthcare facilities and resources and is considered a medically underserved community after the closing of Peninsula Hospital in 2012 [6] (Figure 3).
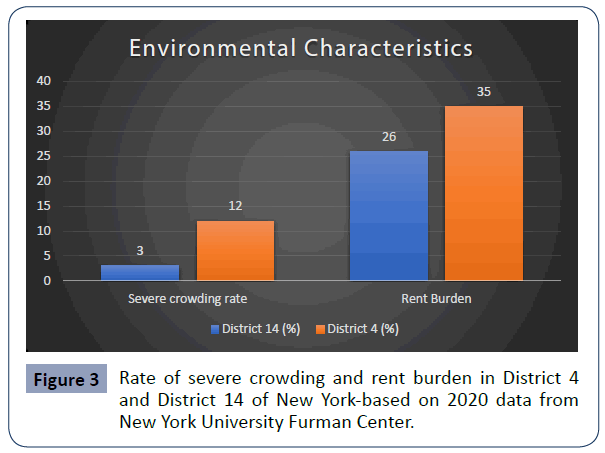
Figure 3 Rate of severe crowding and rent burden in District 4 and District 14 of New York-based on 2020 data from New York University Furman Center.
Discussion
This study provided insight into the health status, access to healthcare, socioeconomic, and environmental factors that put the residents of District 4 and District 14 at heightened risk for COVID-19 incidence or mortality. There are distinctive characteristics in each community that make them more susceptible to either infection or death. Although the District 4 residents have poorer access to healthcare, and a larger immigrant population than does District 14, the self-reported health status of District 4 residents is significantly better. This finding is consistent with other studies highlighting that immigrant children and adults have better health and lower mortality rates than US-born individuals [7-15]. Moreover, Singh et al study indicated immigrants (like foreign-born) have less access to healthcare, similar to the residents in District 4, a densely populated immigrant community [16].
High COVID-19 mortality in district 14
District 14 had certain characteristics at a community level that may have led to disproportionate deaths due to COVID-19. For instance, the rate of premature mortality inDistrict 14 is 2.5 times that of District 4. The mortality rate of heart disease in District 14 is almost five times that found in District 4. Additionally, cancer mortality is almost two times greater in District 14, andlife expectancy is approximately ten years shorter in District 14. Regarding existing chronic conditions, obesity and hypertension are also found in higher proportions, suggesting that residents of District 14 are at increased risk of death due to COVID-19. Previous studies show that these conditions are associated with death from COVID-19 [17]. Compounding the issue further, residents of District 14 had almost double the number of avoidable hospitalizations than District 4. Furthermore, high avoidable hospitalization rates suggest that residents are not getting adequate access to primary healthcare or preventive programs to manage disease conditions.
The disproportionate rate of poor health outcomes found in District 14 suggests a profound lack of access to quality healthcare services. One of the reasons is that the area is deemed a medically underserved community in NYC [18]. According to Health Resources and Services Administration, medically underserved areas are areas or populations designated as having very limited primary care providers and increased infant mortality, poverty, or an elderly population (HRSA-MUA FIND, 2020). Other reasons for poor health outcomes in District 14 are the long wait times, inconvenient hours, and significant geographic distance, as documented in a Doctors of the World (2014) report.
High COVID-19 morbidity in district 4
As noted earlier, District 4 has the highest number of COVID-19 cases in Queens and the city. One distinguishing characteristic of District 4 that separates it from District 14 is the built environment. The built environment in this study refers to housing conditions and limited affordable housing. According to the NYU Furman Community Health Profile report, District 4 is four times more severely overcrowded than District 14 [15]. In 2018, the number of housing units in District 4 was 48,857, only 5% greater than Far Rockway, 46, 463 [14]. However, District 4 is 39% more populous than District 14, reinforcing the severity of crowding in District 4.Studies have found that residents in crowded and poor housing conditions are 50% greater risk for COVID-19 infection and 42% at risk for COVID-19 mortality [19].
The ripple effect of socioeconomic factors increases the risk of infection among District 4 residents. One of the main reasons for overcrowding may be due to poverty. District 4 has a 27% greater poverty level compared to District 14. Even though District 4 has a slightly lower unemployment rate than District 14, it seems likely that the income disparities influence the way people live. The lack of affordable housing and the high cost of living in NYC leaves families with no alternative but to share rooms and reside in crowded spaces.
Racial/ethnic enclaves
Apart from the health status, access to healthcare, socioeconomic, and environmental conditions affecting the health outcomes, it is vital to highlight the difference in the racial and ethnic composition between the two communities, each with distinct differences in health outcomes. As discussed earlier, District 14 experienced significant mortality due to COVID-19. Concerning the racial composition, Blacks represented the largest racial group in District 14 (40%) followed by Whites (33%). However, Blacks account for substantially more COVID-19 cases than Whites. Blacks reside in areas of the district where there is the most significant number of COVID-19 cases. Blacks were also significantly more concentrated and marginalized in specific areas in District 14, subjecting them to astronomical health disparities.
District 4, on the other hand, has a different racial composition compared to District 14. There are significantly more Latinx in District 4 than District 14. Even though they have better health outcomes than those in District 14, socioeconomic and environmental conditions may heighten the risk for COVID-19 infection. The dense concentration of impoverished foreign-born residents in District 4 seems like the perfect breeding ground for COVID-19. These racial and housing disparities seem consistent with other research. Urbanization (the movement of migrants to urban areas) may have led to substandard housing and sanitary conditions that put new migrants at increased risk for infectious diseases [2].
Conclusion
Our findings in this study highlight the distinct demographic, health status, socioeconomic, and environmental factors in two communities that make them more susceptible to COVID-19 infection (in District 4) or death from COVID-19 (District 14). Severe overcrowding places individuals at heightened risk for COVID-19 in District 4, Queens. Other factors, including the type of employment, low wages, and access to food, laundry, and other essential supplies that were not included in this study, may compound the issue further. Disproportionate preexisting health conditionsin District 14 increase individuals’ risk for mortality due to COVID-19 despite having health insurance. To that end, this study underscores the underlying community-level factors that are to be considered when planning COVID-19 prevention efforts, specifically severe crowding and low English language proficiency in District 4 and existing health disparities and access to quality healthcare in District 14.
34691
References
- Ahmad K, Erqou S, Shah N, Nazir U, Morrison A, et al. (2020) Association of poor housing conditions with COVID-19 incidence and mortality across US counties. Plos One 15: e0241327.
- Neiderud CJ (2015) How urbanization affects the epidemiology of emerging infectious diseases. Infect Ecol Epidemiol 5: 27060.
- CDC COVID-19 Response Team (2020) Severe outcomes among patients with District 4virus disease 2019 (COVID-19) – United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep 69: 343-346.
- Docherty AB (2020) Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ 369.
- Morbidity and Mortality Weekly Report (2020) Preliminary Estimate of Excess Mortality During the COVID-19 Outbreak — New York City, March 11–May 2, 2020. Weekly 69: 603–605.
- New York City Department of Health and Mental Health (2020) COVID-19: Data.
- NYCDOHMH (2018) Community Health Profiles, Queens Community District 14.
- NYCDOHMH (2018) Community Health Profiles, Queens Community District 4.
- NYCDOHMH (2018) Community Health Profiles, Queens Community District 7.
- New York State, Office of the State Comptroller (2018) An economic snapshot of the Rockaways.
- Noonan A, Velasco HE, Primm A, Sydnor KD, Amen-Ra N, et al. (2011) Access to effective behavioral health services for insured minority populations: what works?Aetna.
- Singh GK, Rodriguez-Lainz A, Kogan MD (2013) Immigrant Health Inequalities in the United States: Use of Eight Major National Data Systems. Sci World J 2013: 512313.
- Substance Abuse and Mental Health Services Administration (2014) Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings.NSDUH Series H-48. Rockville.
- U.S. Department of Health and Human Services (2001)Mental health: Culture, Race, And Ethnicity—A Supplement To Mental Health: A Report Of The Surgeon General. Rockville.
- U.S. Department of Health and Human Services (1999) Mental Health: A Report of the Surgeon General. Rockville.