M. Malarvizhi1*, B. Hariprasad2 and M. Bhavani3
1Department of Nursing, SRU, Porur, Chennai, India
2Department of Chest and T.B., SRMC 7 RI, Chennai, India
3Depatment of Human Genetics, SRU, India
- *Corresponding Author:
- M. Malarvizhi
Lecturer, Faculty of Nursing, SRU, Porur, Chennai, India
E-mail: malarvizhi23@gmail.com
Received Date: 14.06.2016; Accepted Date: 09.08.2016; Published Date: 16.08.2016
Introduction
Asthma is a long term health problem affects 300 million people worldwide and 15 million people in India. It accounts for 0.5% of national burden and 0.2% of death. It is considered to be a prototype of psychosomatic illness. The various triggers for asthma includes, allergic, infective, climatic and emotional factors.
Background of the Study
The theme for world Asthma day, 2011 is you can control your Asthma' as framed by Global Initiatives for asthma (GINA) in order to create awareness and control asthma. It’s like an iceberg, that only 11% asthma patients are being identified and remaining 89% are either not or wrongly diagnosed. Hence, necessary measures to be taken to cure it before it becomes fatal condition. However, yoga can increase fitness and reduce stress, which may help control asthma. Hence the level of control needs to be identified and measures to be initiated as earlier.
Need for the Study
Education seems to be a positive predictor of physical and mental health among patients with chronic illness. Research suggests that social support and education on control measures by the health care professionals is advantageous for promoting their quality of life.
Objectives
1. To determine the level of asthma control among patients with bronchial asthma.
2. To associate the level of asthma control with the selected demographic variables among patients with bronchial asthma.
Methodology
Research Design : Evaluative approach
Sample : Patients with bronchial asthma
Sample size : 60
Setting : Chest OPD, Sri Ramachandra Hospital
Sampling technique : Random sampling
Tool : Pharmacy Asthma Control Screening Tool (PACS)
Tool description
Ask the patient if he/ she has experienced any of the following in the last month (Tick) (Table 1).
Table 1 Tool description.
| Criterion |
Never |
Once a week or less |
More than once a week |
Not sure |
| Symptoms of asthma, cough, wheeze, shortness of breath |
|
|
|
|
| Waking at night because of asthma |
|
|
|
|
| Chest tightness on walking |
|
|
|
|
| Difficulty in performing vigorous activity like running, lifting heavy objects, exercise |
|
|
|
|
| Difficulty in performing moderate activities like vacuuming, climbing flights of stairs |
|
|
|
|
| Asthma Control |
Good |
Partial |
Poor |
Not sure |
Note: Well controlled= good or partial, Poorly controlled = poor
Data analysis: Descriptive and Inferential statistics, Results: The major findings of the study are depicted below in tables and graphs.
Table 2 and 3 depicts the frequency and percentage distribution of the demographic variables of patients with bronchial asthma. Among which 23 (38%) belongs to the age group of 20-30 years and 36 (60%) of them are male patients, and majority 33 (55%) had primary education, 27 (18%) are unskilled labors with the income of Rs. 10,001 to 15,000 are 16 (27%), 28 (47%) are living in the semi-urban areas, 35 (58%) are non smokers, 32 (54%) had family history of asthma in their first degree relative, 18 ( 30%) had comorbid illness of hypertension.
Table 2 Frequency and percentage distribution of the demographic variables among patients with bronchial asthma.
| Demographic Variables |
N=60 |
| No. |
% |
| 1. |
Age (in yrs) |
|
|
| a. |
20-39 |
23 |
38 |
| b. |
40-59 |
22 |
37 |
| c. |
59-60 |
15 |
25 |
| d. |
>60 |
- |
- |
| 2. |
Gender |
|
|
| a. |
Male |
36 |
60 |
| b. |
Female |
24 |
40 |
| 3. |
Educational status |
|
|
| a. |
No formal education |
12 |
20 |
| b. |
Primary school |
33 |
55 |
| c. |
High school |
15 |
25 |
| d. |
Higher secondary |
- |
- |
| e. |
Degree |
- |
- |
| 4. |
Marital status |
|
|
| a. |
Married |
10 |
17 |
| b. |
Unmarried |
23 |
38 |
| c. |
Divorced |
- |
- |
| d. |
Widow |
27 |
45 |
| 5. |
Occupation |
|
|
| a. |
Coolie |
10 |
25 |
| b. |
unskilled |
27 |
18 |
| c. |
Skilled |
12 |
30 |
| d. |
Professional |
11 |
27 |
| 6. |
Income (inRs) per month |
|
|
| a. |
≤ 5000 |
5 |
8 |
| b. |
5001-10,000 |
15 |
25 |
| c. |
10,001-15,0000 |
16 |
27 |
| d. |
15,001-20,000 |
12 |
20 |
| e. |
>20,001 |
12 |
20 |
| 7. |
Residence |
|
|
a. |
Rural |
12 |
20 |
| b. |
Semi-urban |
28 |
47 |
| c. |
Urban |
20 |
33 |
| 8. |
Type of family |
|
|
| a. |
Joint |
23 |
38 |
| b. |
Nuclear |
22 |
37 |
| c. |
Extended |
15 |
25 |
| 9. |
Smoking habit |
|
|
| a. |
Non smoker |
35 |
58 |
| b. |
Cigaratte smoker |
25 |
42 |
| 10. |
Duration of asthma(yrs) |
|
|
| a. |
<6 months |
23 |
38 |
| b. |
≤ 1 |
12 |
20 |
| c. |
1-5 |
25 |
42 |
| 11. |
Family history of asthma |
|
|
| a. |
First degree relative |
32 |
54 |
| b. |
No First degree relative |
28 |
46 |
| 12. |
Presence of co-morbid medical illness |
|
|
| a. |
Diabetes mellitus |
16 |
27 |
| b. |
Hypertension |
18 |
30 |
| c. |
Cardiac disease |
10 |
17 |
| d. |
Bone disease |
- |
- |
| e. |
Gastro-intestinal disease |
16 |
26 |
Table 3 Overall mean and standard deviation of level of asthma control among patients with asthma (N=60).
| Mean |
Standard deviation |
| 10.9 |
4.38 |
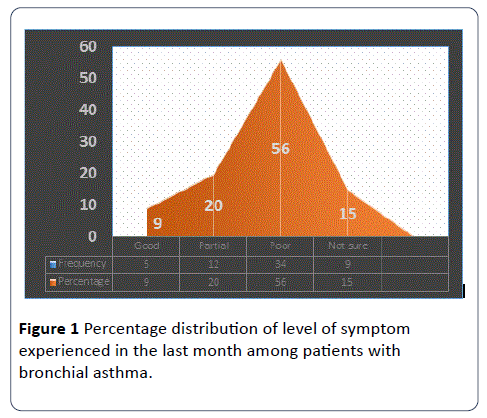
Figure 1 depicts the percentage distribution of the asthma symptom experienced by the patients in the last month. Overall it showed that 56% of them are in the poor state of asthma control, 20% of them have partial control and 15% are not sure about their asthma control.
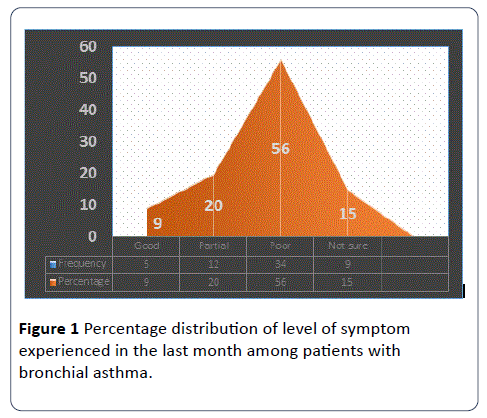
Figure 1: Percentage distribution of level of symptom experienced in the last month among patients with bronchial asthma.
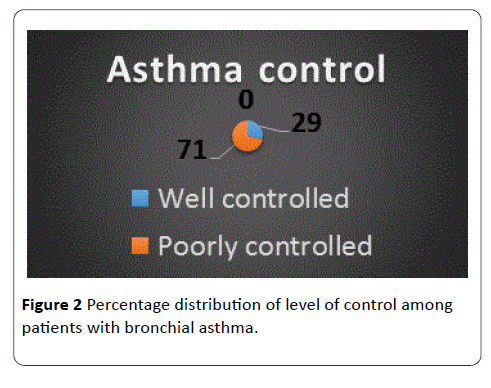
Figure 2 depicts that asthma control was classified into two categories which includes well controlled as good or partial experience of symptoms and poorly controlled as poor way of experiencing the symptom control in the last month (PACS). The analysis shows that 71% of them are in the poorly controlled state of their asthma severity.
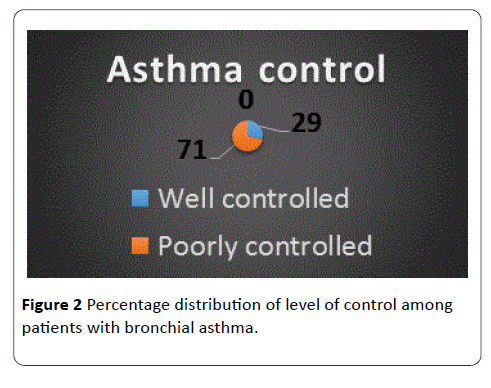
Figure 2: Percentage distribution of level of control among patients with bronchial asthma.
There was an significant association between asthma control with the age, duration of illness.
Conclusion
Prevention from the complications is an essential key in the asthma management. Collaborative management is essential to improve their quality of life and prevent from deterioration of lung function. Nurses can implement the protocols/policies to motivate patients to improve their adherence with poor disease control.
Holistic Nursing should focus on health care sector in which the care of individuals, families and communities to maintain optimal health and quality of life.
Effective asthma management requires routinely tracking symptoms and measuring how well lungs are functioning.
11310
References
- Bender BG, Bender SE (2005) Patient-identified barriers to asthma treatment adherence: responses to interviews, focus groups, and questionnaires. Immunol Allergy Clin North America 25: 107.
- Charlton I, Charlton G, Broomfieldsss J, Mark AM (1990) Cramer “Evaluation of peak flow and symptom only self-management plans for control of asthma in general practice”. BMJ 301: 1355-1359.
- Jones KP, Mullee MA,Middleton M, Chapman E, Holgate ST, et al. (1995) “Peak flow based asthma self-management: a randomized controlled study in general practice”. Thorax 50: 851-857.
- Lahdensuo (1995) Randomised comparison of guided self-management and traditional treatment of asthma over one year. BMJ 312: 748.
- Horne R (2006) “Compliance, adherence, and concordance: implications for asthma treatment” Chest 130: 1.
- National Asthma Council Australia (2006) Asthma Management Handbook Melbourne, Australia.