Omer Othman Abdullah*
Vitreoretinal Surgeon and Medical Retina Specialist, Ibin Sina Modern Eye and Retina Center, Ministry of Health, Erbil, Iraq
*Corresponding Author:
Omer Othman Abdullah
Vitreoretinal Surgeon and Medical Retina Specialist
ibinsina Modern Eye and Retina Center
Ministry of Health, Erbil, Iraq
Tel: +9647501206673
E-mail: omer@ibinsina.org
Received Date: August 10, 2020; Accepted Date: August 25, 2020; Published Date: August 31, 2020
Citation: Abdullah OO (2020) Diabetic Retinopathy Health Crises in Kurdistan Governorate-Iraq/Erbil. Health Sci J. 14 No. 5: 749.
DOI: 10.36648/1791-809X.14.5.749
Objective: To find out the incidence of blindness among the diabetic population in the lack of anti-vascular endothelial growth factor (VEGF) and to assess patient's knowledge about their illness.
Introduction: The diabetic blindness can be prevented by up to 90%, in the early stages of the disease. At the time of diagnosing type two, 21% of them have retinopathy. After 20 years of diabetes; the retinopathy affects 60% of type 2 and approximately all of type 1 diabetic population.
Subject and method: This retrospective study comprised of 1784 diabetic patients. Their vision assessed according to the international classification of controlling blindness as legally blind (visual acuity=< 20/200) or socially blind. For this purpose, the Snellen Eye Chart used at a fixed distance of 20 feet. Patients were checked regularly when checkup missed; excluded from the study.
Result: About 46% of the diabetic population did not know when their diabetes started with a p-value 0.000, which is a very highly significant correlation. Regarding patients information how to control their diabetes; 82% of them did not know how to handle the illness, and 76% did not know the dietary restrictions with a very highly significant p-value, the correlation between them and legal blindness.
About 84.1% presented with legal blindness. After many interventions, 37.9% remained legal blindness, but 62.1 improved. While 6% became socially blinded.
Around 43.9% were unable to buy the anti-vascular endothelial growth factor drugs, with a p-value=0.000.
About 87.2% of patients did not perform HbA1C two times per year with very highly significant with the legally blind.
Conclusion: We can emphasize that the lack of education program, patient's information about the disease, non-referrals, economic crisis and the unavailability of the anti-vascular endothelial growth factor; all collectively created a blinded diabetic population.
Keywords
Anti-vascular endothelial growth factor; Diabetic retinopathy; Legal blindness; Health crises
Introduction
The devastating ocular complication in diabetes is blindness; most of the diabetic population know that or have seen the same complication from other persons; still they do not control their hyperglycemic states well [1].
The diabetic blindness can be prevented up to 90%, if the treatment is given adequately and the patient consulted in the early stages of the disease, to prevent progression or blindness [2].
Retinopathy affects type 1 and type 2. At the time of diagnosing type 2 and 21% of them have retinopathy because they do not know that they have diabetes [3]. After 20 years of diabetes; the retinopathy affects 60% of type 2 and approximately all of type 1 diabetic population [3]. Therefore, we can emphasize that the duration and the glycemic control directly related to the retinopathy and blindness, which occurs slowly and silently [4]. It is expected by 2030 to have more than 190 million vision loss from diabetic retinopathy by different mechanisms which directly related to the poor blood sugar controlling [5].
Materials and Methods
This retrospective study comprised of 1784 diabetic patients who attended our clinic from Jan. 2nd 2019 to Jan. 2nd 2020. The same vitreoretinal specialist performed all the assessments for all the patients. The patient's visual acuity assessed according to the international classification of controlling blindness as legally blind, if the visual acuity (VA)=< 20/20 or socially blind when he was unable to do his daily tasks [1]. For this purpose, the Snellen Eye Chart used at a fixed distance of 20 feet.Every patient, according to his eye situation whether underwent a single or combining two or more interventions like argon laser, intravitreal anti-VEGF, cataract surgery or pars planavitrectomy. Patients were checked up for one year according to the schedule given, and any patient missed from the checkup had been excluded from the data collection.
Result
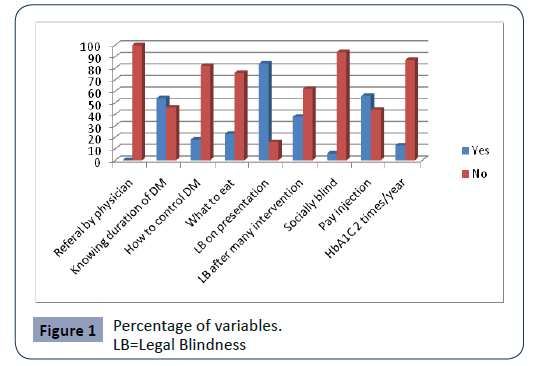
The data analyzed using SPSS version 27, ANOVA and regression used, any variable < 0.05 regarded as significant statistically. All the frequencies illustrated in Figure 1.
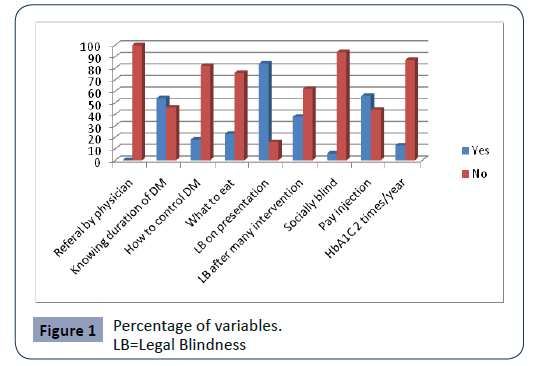
Figure 1: Percentage of variables.
There was no referral of diabetic patients by physician 100%, and it is correlation with the legal blindness (LB) was very highly significant (VHS). Nearly 46% of the diabetic population unaware about the start of their illness with a p-value 0.000, which is a VHS correlation. Regarding patients information how to control their diabetes; 82% of them did not know; how to handle this illness, and 76% did not know how to manage dietary regimen with a VHS p-value 0.000 correlation between them and LB. On presentation, 84.1% were legally blinded, and after many interventions, 37.9% remained LB, i.e. their vision stabilized, but around 62.1 got a better vision. But 6% of them became socially blind.
Concerning the financial issues for buying the injection, 43.9% were unable to pay for the anti-VEGF drugs, and it is p-value=0.000 VHS.
The patients care regarding their regular checkup for HbA1C; 87.2% were not performing the test even two times per year, and it is correlation with the LB was VHS, p-value=0.000.
Discussion
Diabetic retinopathy in the early stages is asymptomatic, and the visual symptoms make the patient consult; therefore, there should be a robust screening program to identify new diabetes cases before the patients can detect their illness, visually based [5]. The diabetic retinal changes can be detected before the visual symptoms to appear by electroretinogram (ERG), which detects the functional changes and also measuring the calliper of the retinal vasculature [5].
The duration of diabetes considered as a significant risk factor, after 20-30 years 77% of the diabetic population develops diabetic retinopathy [6], but in our region 46%, they do not know the onset and duration of diabetes.
The diabetes-related legally blindness on 3.6% for type 1 and 1.6 for type 2 for the proliferative stage and [3], while, legally blind on presentation accounts for 26.1% for proliferative diabetic retinopathy for and 25.8% for macular edema [7] but in this study, 84% were legally blind on presentation, however, after multi interventions like argon laser and pars planavitrectomy 38% remained legally blind but their vision stabilized. Due to total lack of quality controlled anti-VEGF; no one received the injection at our side which is a crucial step in treating diabetic retinopathy as it reduces the incidence of diabetes-related blindness by 75% [8,9].
The incidence of global visually handicapped from diabetic retinopathy is 1% [10], while in our region is 6%. The correlation between duration and each of the legally blind on presentation, legally blind after many interventions and visually handicapped, was very highly significant; p-value 0.00.
The incidence of the lack of patients' knowledge to control diabetes was 82% which is the primary step in managing diabetes [11]. About 23.9% did not believe that dietary restriction impacts on their eye health, which is a building block in treating diabetes [12], and the most critical point to focus, here, is no one had been informed to check his eyes by their physician [13].
Regarding regular HbA1c testing, which is a significant risk factor for the diabetic blindness, 87% did not perform the test two times per year which is a crucial marker for the diabetic control in preventing blindness [14].
Another point was unavailability of the anti-VEGF, although, directly the patient been asked whether able to pay for the injection if it became available; 43.9% were not able to pay; therefore, the economic crises adds another burden to worsen the situation [15].
Conclusion
This study emphasizes the lack of education program, patient's information about the disease, non-referrals, economic crisis and the unavailability of the anti-VEGF; all collectively created a Figure 1 blinded diabetic population.
Acknowledgements
Special thanks to both ibinsina modern eye and retina center and LaylaQasim diabetic center for referring diabetic cases.
Declarations
Funding: None
Conflict of interest: None declared
30951
References
- Vashist P, Senjam S, Gupta V, Gupta N, Kumar A (2017) Definition of blindness under National Programme for Control of Blindness: Do we need to revise it? Indian J Ophthalmol 65: 92-96.
- Aiello LP, Gardner TW, King GL, Blankenship G, Cavallerano JD, et al. (1998) Diabetic Retinopathy. Diabetes Care 21: 143-156.
- Fong DS, Aiello L, Gardner TW, King GL, Blankenship G, et al. (2004) Retinopathy in Diabetes. Diabetes Care 27: s84-s7.
- Ramanathan RS (2017) Correlation of duration, hypertension and glycemic control with microvascular complications of diabetes mellitus at a tertiary care hospital. Integr Mol Med.
- Lechner J, O'Leary OE, Stitt AW (2017) The pathology associated with diabetic retinopathy. Vision Res 139: 7-14.
- Klein R, Klein BE, Moss SE, Davis MD, DeMets DL (1984) The Wisconsin epidemiologic study of diabetic retinopathy. III. Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years. Arch Ophthalmol 102: 527-532.
- Jeppesen P, Bek T (2004) The occurrence and causes of registered blindness in diabetes patients in Århus County, Denmark. Acta ophthalmologica Scandinavica 82: 526-530.
- Varma R, Bressler NM, Doan QV, Danese M, Dolan CM, et al. (2015) Visual Impairment and Blindness Avoided with Ranibizumab in Hispanic and Non-Hispanic Whites with Diabetic Macular Edema in the United States. Ophthalmology 122: 82-89.
- Zhao Y, Singh RP (2018) The role of anti-vascular endothelial growth factor (anti-VEGF) in the management of proliferative diabetic retinopathy. Drugs Context 7: 212532.
- ÃÂÃÂââ¾ÃÂâÂÂÃÂ
þahlÃÂÃÂââ¬Ã
¾ÃÂâÂÂÃÂñ E, ÃÂÃÂââ¬Ã
¾ÃÂâÂÂÃÂðdil A (2019) A Common Approach to Low Vision: Examination and Rehabilitation of the Patient with Low Vision. Turk J Ophthalmol 49: 89-98.
- Beaser RS, Turell WA, Howson A (2018) Strategies to Improve Prevention and Management in Diabetic Retinopathy: Qualitative Insights from a Mixed-Methods Study. Diabetes Spectr 31: 65-74.
- Wong MYZ, Man REK, Fenwick EK, Gupta P, Li LJ, et al. (2018) Dietary intake and diabetic retinopathy: A systematic review. PLoS One 13: e0186582-e.
- Saleem M (2017) The impact of delay in diabetic patient's referral for diabetic retinopathy screening on the level of retinopathy detected in adult Sudanese diabetic Sudanese patients. Al-Basar International Journal of Ophthalmology 4: 49-53.
- Khan H, Sherwani S, Ekhzaimy A, Masood A, Sakharkar M (2016) Significance of HbA1c Test in Diagnosis and Prognosis of Diabetic Patients. Biomarker Insights 11: 95-104.
- Low L, Law JP, Hodson J, McAlpine R, O'Colmain U, et al. (2015) Impact of socioeconomic deprivation on the development of diabetic retinopathy: a population-based, cross-sectional and longitudinal study over 12 years. BMJ Open 5: e007290-e.