Keywords
Psoriasis; Inflammatory skin disease; Chronic diseases
Introduction
Psoriasis is a chronic inflammatory skin disease with increased epidermal proliferation related to dysregulation of the immune system. About 1-3% of the world population is affected by this disease [1]. It is characterized by welldemarcated, erythematous papules or plaques with silvery scales that predominantly affect the extensor surfaces, scalp and nails. In severe cases, any skin surfaces can be affected.
Although psoriasis is not generally fatal, its impact on the quality of life of patients can be profound. Patients not only experience skin discomfort and itchiness, in addition their appearance can cause embarrassment and rejection. The perceived quality of life for patients with psoriasis is lower than that of the general population [2]. Psoriasis affects physical and mental functioning as much as other chronic illnesses such as cancer, heart disease, depression, diabetes, etc. [3]. Physically, it affects the appearance of the skin, in particular when the head and neck region, hand dorsa are involved, and causes discomfort such as mild to intense itching, redness, dryness and bleeding. Sleep disturbance and restricted use of hands are also reported by patients [4]. Socially, many patients experience stigmatization, embarrassment and rejection by others [5], as there is common misunderstanding that psoriasis is contagious through body contact. Reports of public rejection, such as being required to leave a swimming pool, are common [6]. Feelings of shame and lack of self- esteem lead to significant disruption in daily life and social withdrawal [7].
Psychologically, psoriasis is a major source of stress for patients. For whom the psychological impact may be greater than the physical impact [8]. Psoriasis is found to be associated with psychological morbidities, anxiety disorder and depression, alcoholism and increased suicide ideation [9-14]. Patients with psoriasis commonly experience a complexity of feelings: anxiety regarding the prognosis of the disease, depression due to the condition’s incurability, frustration and anger regarding unexpected treatment outcome, and sadness of being discriminated against. Stress is associated with more severe and frequent psoriatic flare-ups, especially for those with more disfiguring conditions [12]. All in all, poor psychosocial well-being can in turn exacerbate the disease condition.
The illness experiences of people with chronic diseases [15] developed the illness perception framework of the Self- Regulation Model of illness behavior, which has been widely accepted by health professionals in understanding patients’ behavior. This model suggests that health threats are guided by symptom perceptions and the social messages received by patients. Coping strategies in illness management, therefore, could either be problem-focused-which refers to altering the external environment that caused the stress, or emotionfocused- which involves regulating emotional responses towards stressful events. Elwy and associates further stated that these strategies would ultimately determine a patient’s help seeking or help avoidance behavior [16].
Alongside the cognitive development in Leventhal et al. [15] Self-Regulation Model, [17] considered illness recovery as an evolution process where the patient would personify the illness in order to construct a self-identity and search for the meaning of the event. However, these researchers did not further explain the process, while they also failed clearly to describe the relationship and interaction between variables. More recently, Greenley et al. [18] also identified different determinants of help-seeking behavior including how the illness experience was recognized and the perceived severity of the impact [18].
The latest development of illness perception has focused more on the relationship between cognition and behavioral responses. Based on the social cognitive theories of [19,20] proposed another self-regulation model for chronic disease management which includes a number of feedback and reappraisal processes. However, this framework focuses more on social cognition, while the emotional responses and influences on other psychosocial factors have not been clearly explored. Despite the development of a number of models to describe illness cognition and behavior, most have focused on how one’s well-being is affected by different physical, emotional, cognitive and social variables, which were usually examined as independent and separate entities within quantitative research methodology.
However, in real life, these variables might be complementary and interdependent. The dynamic interactions and interlinkage among these variables are less well described. Based on a similar concept used in a study of arthritis patients’ emotional experiences and coping strategies, Gronning et al. [21] proposed a model of dynamic balancing process.
While the patients’ intention was to maintain a normal life style and ‘go on as usual’, deterioration of bodily functions triggered by the illness forced the person to ‘listen to the body’. The tension between the two concepts created a dynamic process and the ‘adjustment’ was the balancing state where the patient would make both physical and psychological changes, in order to accommodate the disease and to minimize its impact on their daily life. A critical element of this model was the patient’s ‘attitude towards life’ which would significantly influence the overall coping process.
The current study
The chronicity of psoriasis requires patients to undergo a lengthy treatment process; difficulties in managing the multidimensional complications in illness experience should not be understated. Existing models describing illness experience are relatively linear and may not be able to depict the interlinked strategies that people with psoriasis may adopt in managing their illnesses.
The objective of this study was to provide an in-depth account of how Chinese patients with psoriasis described and made sense of their illness experience. Their strategies in managing and the dynamic nature of physical and psychosocial factors were further explored. This can provide information of how various domains such as perception and coping interact within the illness experience. The theoretical and empirical approach of this study is based on the framework of interpretative phenomenological analysis (IPA) which aims to engage with the understandings utilized by participants to make sense of their situation, as well as consider researchers’ own conceptions, beliefs, expectations, and experiences [22].
Method
This qualitative study adopts the framework of IPA which has its origins in health psychology [23]. According to Smith, IPA is “concerned with understanding personal lived experiences and thus with exploring persons’ relatedness to, or involvement in, a particular event or process”. It emphasizes the importance of understanding informants’ lived experiences in terms of how they make sense of a particular situation or phenomenon and how they make reflective interpretations and meanings of their experiences. This method can be applied to small samples with up to ten interviewees, which facilitates the exploration of themes shared between individuals. Hence, this approach has been found useful in developing a theoretical model instead of generating in-depth description of a specific phenomenon, and involves detailed examination of the informants’ worldview and their perspectives. IPA emphasizes the dynamic and interactive nature of the research process, a process in which researchers play an active role throughout. For instance, informants are trying to make sense of their experience while the researcher is also making sense of how the informants interpret their experience. IPA has been widely used to generate in-depth descriptions of human experience, especially in the field of health and illness.
In this study, IPA was adopted in order to understand informants’ lived experiences of psoriasis and to undertake a theoretically informed analysis. Semi-structured interview is the exemplary method for IPA as it allows the researcher and informant to engage in a dialogue whereby initially set questions can be flexibly modified in response to informants’ narratives during the interviewing process.
Ethical approval for the study was given by the university that employs the research team.
Sample
Purposive sampling was used in order to achieve maximum variation regarding participants’ age, gender, education background and duration of illness. Twelve patients were recruited from the membership list of a community-based psoriasis patient group in Hong Kong. Patients were selected if the person: (1) had been diagnosed with psoriasis by a dermatologist, (2) was aged between 18 to 65, (3) Was not comorbid with any other chronic disease, and (4) was able to communicate in Cantonese-Chinese.
Data collection
Semi-structured interviews were conducted which focused on exploring the patients’ lived experience of psoriasis so as to gain insights into how they coped with and made sense of their illness experience and how the illness could be integrated into their lives and relationships with others. Each interview was conducted by a researcher following an interview schedule comprising of a set of questions which served as a framework for the interview and probes pertinent to the focus of the study. Interview questions (Table 1).
Table 1 Questions and probes in the interview schedule.
| Thematic Area and Interview Questions |
| Illness experience |
| •Could you give me a brief history of your illness (i.e., psoriasis) such as age of onset, diagnosis, prognosis and treatment history? |
| •Could you describe the symptoms that you have been experiencing? |
| •What did you do when you were diagnosed with psoriasis? |
| •How does psoriasis affect your everyday life? |
| Probe: Employment opportunities, job security, work environment, interpersonal relationships, social activities, hobbies and interests |
| •Is there any difference in your quality of life since having psoriasis? |
| Illness coping |
| •How do you deal with and manage your everyday life? |
| •How do you deal with the symptoms of psoriasis? |
| •What was your feeling towards the illness? How about your feeling at this moment? |
| •How would you understand yourself as a patient? Would you consider yourself as a chronic disease patient? |
| •Has psoriasis made a difference to how you view yourself? How did you cope with the difference? |
| •What about the way other people view and treat you? How did you manage or cope with this? |
| Illness perception |
| •How did you feel when you were diagnosed with psoriasis? Probes: Physical and emotional responses |
| •How did you think about this? How about your perception at the present moment? |
| •How much did you think about your physical well-being? How about in recent days? |
| •If you had to describe what this disease means to you, what would you say? |
| •What does psoriasis mean to you? |
| •How do you make sense of the illness? |
| •How do you perceive your future? |
Interviews were conducted in a private interview room. The medium of language was the informant’s native language, i.e., Cantonese-Chinese. Each interview lasted from 1.5 to 2 hours. With informants’ consent, all interviews were digitally audiorecorded. Interviews were transcribed verbatim and the researchers also wrote up reflexive notes.
The original questions and answers of the interviews were in Cantonese-Chinese and they were translated into English accordingly. To ensure the veracity of the translation, the translated scripts were reviewed by 4 research team members and social workers who are proficient in both English and Cantonese-Chinese.
Data analysis
The interviews were analyzed by following the IPA guidelines as described by Smith [22]. They were transcribed verbatim and imported into the NVivo10 software package. Data analysis was performed by the research team. Firstly, in order to gain familiarization with the data, each researcher read each transcript several times. Codes and themes were captured and noted in the transcript independently by each reader. Second, researchers read through and compared the transcripts as well as the codes and themes together. Preliminary themes were identified, consolidated and further discussed. Third, consensus within the research team enabled the preliminary themes to be clustered into categories which were then validated by checking back with the transcripts.
Results
Twelve patients (Male: n=7; Female: n=5) with psoriasis were interviewed. Their ages ranged from below 30 to over 60, with a mean of 48.5 years. Eight informants were married and all were living with family. Onset of the disease for six informants occurred at or before the age of 26, with the earliest onset at age 14 and the latest onset at age 56. The duration of disease varied from three to 34 years, with a mean duration of 15.3 years. Informants’ demographic data (Table 2).
Table 2 Informant’s demographic characteristics.
| Informant No. |
Age |
Gender |
Marital Status |
Education Level |
Occupation |
Living with Family? |
Age at Onset |
Duration of Disease |
| 1 |
42 |
Male |
Married |
Postgraduate |
Business analyst |
Yes |
22 |
20 |
| 2 |
52 |
Male |
Married |
Under
graduate |
Consultant |
Yes |
43 |
9 |
| 3 |
59 |
Male |
Married |
Diploma |
Retired |
Yes |
25 |
34 |
| 4 |
62 |
Male |
Married |
Under
graduate |
Not specified |
Yes |
50 |
11 |
| 5 |
59 |
Female |
Married |
Secondary |
Housewife |
Yes |
56 |
3 |
| 6 |
38 |
Male |
Single |
Secondary |
Unemployed |
Yes |
22 |
10 |
| 7 |
51 |
Male |
Married |
Under
graduate |
Accountant |
Yes |
42 |
8 |
| 8 |
52 |
Female |
N/A |
Primary |
Cleaner |
Yes |
30 |
20 |
| 9 |
56 |
Female |
Married |
Diploma |
Housewife |
Yes |
38 |
18 |
| 10 |
51 |
Male |
Married |
Secondary |
Director of Engineering |
Yes |
21 |
30 |
| 11 |
21 |
Female |
Single |
Under
graduate |
Student |
Yes |
14 |
7 |
| 12 |
39 |
Female |
Single |
Under
graduate |
Accountant |
Yes |
26 |
13 |
Meta-themes
Qualitative analysis yielded many common themes in the lives of study informants. An overview of the themes and subthemes (Table 3). Three meta-themes emerged as most representative of their phenomenological experiences: 1) Surviving the chronicity of the disease, 2) Accepting the disease and illness experience as part of their life, and 3) Thriving with the new assumptive world.
Table 3 The meta-themes generated from the interviews.
| Meta-themes |
Sub-themes emerged |
| 1.Surviving the chronicity of the disease |
•Emotionally experiencing the physical symptoms of the disease |
| •Understanding and compromising with the chronic nature of the disease and its impact on daily functioning |
| •Struggling with the alteration of body image |
| •Alternating between negativity and positivity during the course of treatment |
| 2.Accepting the disease and illness experience as part of their life |
•Disengaging from negative social support |
| •Cultivating empathy for both self and others through normalizing problems |
| •Re-allocating resources to other aspects of life |
| 3.Thriving with the new assumptive world |
•Finding benefits from the illness experience |
| •Exploring and establishing healthy lifestyles |
| •Constructing a prospective life plan |
| •Exploring and engaging with meaningful social activities |
Surviving the chronicity of the disease
Emotionally experiencing the physical symptoms of the disease: All informants reported that bodily discomforts were the most salient signal of their physical condition. The recurrence of physical symptoms was considered as one of the major sources of distress that include itching, pain, flaking, patching, festering and redness. Some informants felt that it was sometimes difficult for them to tolerate those physical discomforts that affected their psychological and social wellbeing. Relapse was considered as a frightening threat leading to anxiety regarding the weakening of the immune system. Some informants also worried about the possible onset of arthritis and other unpredictable complications, which would further adversely impact their quality of life. Regarding their treatment, some informants were concerned about a decreased capability to endure the side effects of steroids.
“My understanding is that it is a genetic problem and I cannot get away from it… to minimize the side effects of medicine… At least I am still functional, though not flexible. I hope it won’t get worse, and then generate more diseases like vascular disease, heart disease, arthritis, and so on … ” (Informant 11).
“Sleeping is the most difficult part of my life. I have not slept well for many years due to itching. I know I keep scratching while I am asleep. When I wake up in the morning, I found my bed full of flaked skin and dandruff. I found blood on the fitted sheet as well. You know, people become moody when they do not have good quality of sleep. I feel very tired and am easily irritated during the daytime. My mood is not very good at all”. (Informant 3).
Understanding and compromising with the chronic nature of the disease and its impact on daily functioning: Most informants reported that after struggling and experiencing recurring episodes of symptoms, such as painful scaly skin, redness and thickened skin as well as the unpredictable effects of the treatments and therapies they began to understand, and compromise with the chronicity of their illness and learn how to deal with it.
“I know this is a genetic problem and I cannot get away from it. So I need to find a way to coexist with it… and my goal is not to achieve total cure, but to minimize the side effect of medicine. At the end, psoriasis is not life threatening and is not the worst scenario like cancer. Then I try to accept it as part of my life... for instance, I will not let the disease occupy my whole life. I will still work and live as usual” (Informant 1).
“I began to get used to the cycle of success and failure. Whenever somebody told me about the successful stories of other patients who have tried alternative treatments, I would also try, as long as they were affordable. After attempting in vain to get cured from a series of treatments, I gave in and accepted the reality about the chronicity of my condition… Of course, if I had never gone through the treatments with no promising outcomes, I would not come to this realization” (Informant 2).
Struggling with the alteration of body image: People with psoriasis also experienced the huge adverse impact on their self-esteem, and poor self-esteem leads to reduction of desire and behavior to be socially active. With lowered confidence levels, some informants indicated that they were sensitive to exposure of their skin condition in public and intentionally skipped classmate reunions or dating activities to avoid the scrutiny of others. Reduced social engagement confined patients’ life circles and further impaired their psychological well-being.
Alteration on body image impacted on males and females differently. For female patients, their physical appearance with “imperfect” skin condition implied a loss of social capital. Change in body image was perceived to reduce sexual attractiveness and communication with people of the opposite gender. In our interviews, male patients were also concerned about altered body image as well as the effects of psoriasis on genetic issues, career development and family harmony.
Alternating between negativity and positivity during the course of treatment: It was not uncommon to find that patients went “doctor-shopping” after diagnosis of psoriasis. Regardless of the incurable and life-long nature of psoriasis, all informants indicated that they had undergoing various types of medication and healthcare in order to achieve a complete recovery. Some patients pursued the latest developments in treating their disease, including oral treatments and biologics, even if the treatment protocol was still subject to a clinical trial.
Whenever they heard of any new treatment or alternative therapy from family, friends, or support group members, they would try and maintain a positive expectation regarding the outcome. Since there was no guarantee of success of treatment, some informants experienced alternate cycles of hope and disappointment during the course of medication.
“I have been trying different types of treatment, biologics, oral medications, Chinese Traditional Medicine, natural therapy. I am almost an expert patient…… I am still hopeful about the advancement of medicine. I shall maintain my fighting spirit, although there will be disappointments when things are not going smoothly. But after all, I will not give up as ruminations on failures will not be helpful. I had experienced down times and I know about the effects of that kind of emotional turmoil. Therefore I would not allow the negative mood to overwhelm me for a long period of time” (Informant 10).
Accepting the disease and illness experience as part of their life: Due to limited public awareness, psoriasis has been widely misunderstood as a contagious skin disease, which caused scrutiny, teasing, and reproach from the public. Limited knowledge about psoriasis may create anxiety and fear that this skin disease could be highly and easily infectious through social interactions, which would ultimately lead to unfriendly behaviors, stigmatization and discrimination. Most informants reported that they would isolate themselves from their social circles in order to avoid encountering negative responses, although the magnitude and duration of social withdrawal were different for different informants.
Stigmatization experiences in interpersonal interactions impeded informants’ passion and participation in social activities. With visible symptoms, people with psoriasis were disliked, excluded and isolated by others. Informants felt exhausted after providing numerous explanations about the incurability and non-contagious nature of psoriasis.
Disengaging from negative social support: Given uncomfortable stigmatization, some informants attempted to avoid judgments by hiding their symptoms, disengaging from social activities and keeping psoriasis as an unspoken secret, resulting in social withdrawal or isolation. They reported that they became more selective in making new friends or establishing meaningful interpersonal relationship. Informants frequently mentioned that they were socially disrupted by psoriasis by stating that “Now, social activities were largely reduced” (Informant 5) and “I became more solitary, lonely and eccentric” (Informant 8).
“Although physical appearance was not important for me, I would feel embarrassed when other people focused on my bodily condition, especially when I went swimming and had to expose my body in public. Some people know that it is not infectious, but in the public area (like swimming) when you take off your clothes…, I still feel embarrassed. It doesn’t look good to others, so I’ve tried to avoid it…I learned not to be influenced by others. I must thank my wife as she has to do my skin care for me every day… The most important thing is that she (wife) understands and supports me”.
Cultivating empathy for both self and others through normalizing problems: Some informants indicated that they began to live with the disease so it was crucial for them to develop and maintain a positive attitude. When compared with other life-threatening illness, psoriasis was not the ‘worst scenario’ at all. For some informants, although they suffered from this unexpected illness and its corresponding bio-psychosocial discomfort, they had identified various coping methods and they believed that they could still learn from the whole process by recognizing both losses and gains in the psoriasis experience. Some informants expressed that one of the most important ways they overcame unfriendly scrutiny and behaviors was by being normal and behaving normally in their daily life.
“It (social barrier) happened in the beginning years. My old friends were shocked when they saw my psoriasis symptoms. They were all concerned about whether it was contagious. However, I was open-minded and would never let misunderstandings from others affect me. I knew that I was just as normal as you. I had no difficulty in social interactions and was active as a volunteer for a decade” (Informant 3).
“I have survived through psoriasis for 13 years. My parents imposed high expectations on my academic performance when I was taking the high school examination. I was later diagnosed with something like platelet disorder, which might result in psoriasis through virus infection. My psoriasis symptoms would get worse if I was in a bad mood. In recent years, I fully accepted myself. I might be ill with psoriasis, but I am not problematic” (Informant 12).
“Recently, I changed my job. My scaling was so obvious on the black floor of the new office, which was embarrassing… What’s more, my boss is extremely hyper neat. So, I tried to be smart and laborious. When I found flaky skin, I cleaned it up with private brush. After all, I knew that I was hired for professional capacity…Sometimes, I was challenged by a job agency for my poor image, but I did nothing wrong. I am a person with psoriasis, that’s all” (Informant 10).
Re-allocating resources to other aspects of life: Most informants revealed that they felt depressed when they acquired more information about the disease, especially about its incurable nature. Patients with psoriasis are tortured by an unanswered question “Why me?” at the early stage of their illness. After years of medication and treatments, they also acknowledged the unpredictability and uncontrollability of their physical condition. They focused more on how to maintain an accommodating attitude and find ways to coexist with the disease.
“I didn’t know what to do when I was diagnosed with psoriasis around 10 years ago. I checked from the Internet and found out that it was incurable. I was so depressed about it…… I have consulted many doctors and sought different kinds of treatments, with the ultimate goal of total recovery. Unfortunately, I spent an enormous amount of money and nothing was effective…… My life has been stuck during the days when I kept pursuing treatments. In reality, I found that when I went traveling or was on holiday leave, my disease would improve for no reason. I cannot predict the timing of the outbreak of the disease or the timing of improvement. Therefore, I prefer to spend money on traveling than on medication” (Informant 1).
Thriving with the new assumptive world
Finding benefits from the illness experience: All informants mentioned not only the negative experiences during their illness, but also revealed how they had benefited and gained throughout the years, which was considered as a new schema of the reality in illness experience. While there were times when they felt depressed or emotionally unstable, there were occasions when they felt joyful, grateful, and appreciative. These bi-directional emotive experiences coexisted interchangeably in their life denoting a significant guideline to their life direction. Throughout years of illness experience, they would approach a balancing point imminently where personalized coping strategies were developed. Specifically, they learned from being reactive towards the experience to responsive in generating new behaviors in dealing with the illness.
“There must be ups and downs over the course of an illness. My mood will certainly be affected, sometimes being very irritated and frustrated due to the itchiness, but afterwards I would be okay as I know it will pass. Or, sometimes I felt upset about my face and appearance, yet I felt grateful and proud of myself that I have gone through all difficulties. However, I would not deny that I have my own weaknesses, but I have also learned something good about myself” (Informant 11).
“After years I know that is quite normal for people to encounter adversities. Illness is inevitable. I surrendered and I know this is fate. I appreciated that I have a good family who offered support and acceptance to me all along. They tolerated my bad temper when I felt irritated. They would gently remind me “don't scratch, okay?” and I would try to stop scratching, though I could not control… Just like the family relationships, there must be something good or bad, it’s just a matter how you perceive” (Informant 7).
Exploring and establishing healthy lifestyles
Throughout years of combating the disease, most informants mentioned that they have established healthy lifestyles, compared with their previous days. The illness has motivated them to develop positive energy, and new lifestyles through trial-and-error, in order to deal with their bodily and psychological discomfort.
“I have to be careful about my diet, don’t eat toxic food like goose, duck, red meat… and eat less seafood such as crab and shrimp. Regarding positive changes, I have met more people who were more accepting… I will eat and relax with others and joined the patient group so that I know more about the disease discuss with people and find out any possible treatment method… Instead of being passive and discriminated against because of misconception, I will talk to them (friends) about the disease – psoriasis is not infectious… I will let them understand more…” (Informant 1).
“I will do more exercise and be health conscious. You don't know what the illness will turn into, maybe even worse, such as arthritis. Therefore I will try my best to keep my body in better condition… And I know that stress is not helpful to recovery from illness. I will try to relax, such as not being not too demanding on myself, not be too perfectionist”.
Constructing a prospective life plan
Some informants expressed anxiety about the financial burden arising from treatment that they might undergo in the future; on the other hand they also gained insight in managing their expenditure such as planning for retirement.
“My body might be getting worse. If you think about it, why do you have to work that hard? So I may want to do something that I like… perhaps I will retire earlier..., or after my retirement, I may need to spend more money to take care of my body (disease)…” (Informant 2).
“Sometimes I would feel uncomfortable with my bodily discomfort and the discriminatory looks of other people. However, looking backward was impractical… just like a half glass of water… good I have half a glass of water… but not… I only have half a glass of water left… Sometimes we should not look back… It is better for us to look forward. You can’t control the disease… you want to do more on your body… minimize its impact… stay positive, this is an important attitude…” (Informant 12).
Exploring and engaging with meaningful social activities
Anticipatory problems in family formation, such as, genetic issues and poor self-image with apparent symptoms, hindered informants’ ability to initiate and maintain long-term romantic relationships. Some informants experienced sadness in grieving the impossibility of building an intimate relationship. Some tended to be more sociable and energetic in interpersonal interactions, which might lead them to explore and engage with meaningful social activities, such as working as volunteers in different social service sectors.
“To be honest, I encountered no difficulties in normal social communication. However, when it comes to dating, I became a timid person. I never had the courage to do handholding. With psoriasis, I experienced emotional blockage in romantic relationships. In the beginning, you will bring up future plans, including forming a family, giving birth to a child. But I’ve decided not to have children, because I would likely pass on my psoriasis to the next generation. I got enough of psoriasis; I would not let my offspring continue suffering… In most cases, they (the dating partners) will stop the relationships” (Informant 4).
“I started to volunteer to work with new immigrants and later maintained a friendship with them. At first, they did not talk to me. As time passed by, they would reveal their earlier fear and accepted me. I used to explain what psoriasis was to them. Now, I would say that I am positive, especially after I joined in organizing the psoriasis association. I took the TV interviews and did the promotion to let more people know about psoriasis…It (Volunteerism) makes me happy” (Informant 3).
Discussion
Consistent with previous studies [24-26], patients living with psoriasis experienced the disease in a multidimensional perspective in terms of physical, emotional and social ill-being and well-being. Prominent physical symptoms are itching, pain, flaking/scaling and red patches of skin, any of which can significantly impact patients’ emotional states and social functioning. Previous research has revealed that psoriasis has altered patients’ body image negatively that resulted in psychosocial impairment of patients with visible symptoms [27], while the present study also found that visible physical symptoms might affect various aspects of patients’ daily life. Patients might experience difficulties in maintaining former social interactions or establish new interpersonal relationships. However, the most significant psychosocial stress expressed by our informants was social stigma resulting from their physical appearance. In line with previous studies, patients recalled social stigma as perceived scrutiny, judgment, aversion and rejection from others who might conceive their skin problems as contagious or a result of poor personal hygiene. The experience of constant social stigmatization could contribute to emotional distress and social limitations.
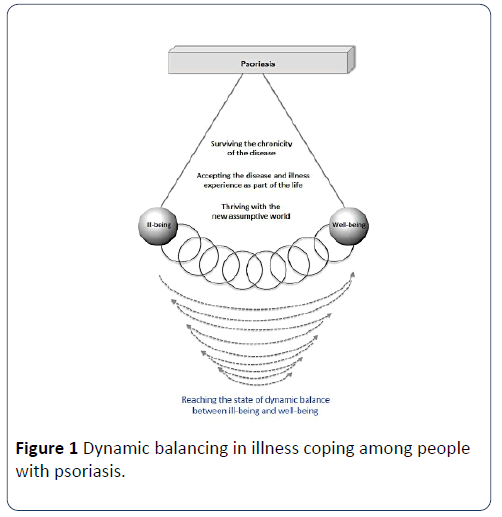
Although different informants adopted various strategies to cope with the illness experience, common characteristics have been identified in their emotional regulation and adjustment process. It was also noticed that positivity and negativity were bound together as a whole in the illness experience. These two entities denoted two opposite yet complementary interactive forces. Balance, or equilibrium, could be achieved as a result of continuing adjustment between these two forces. The balance was neither static nor absolute. The magnitude of the psychological adjustment between ill-being and well-being gradually decreases with the duration of illness experience. Based on the experiences from our informants, the decrease in magnitude also implied a general tendency to maintain a balance dynamically.
The dynamic balancing process is illustrated in Figure 1. On the side of ill-being, people with psoriasis demonstrated intolerance of bodily discomfort, exacerbation of uncertainty, avoidance of social stigmatization, alteration of self-image. On the side of well-being, they demonstrated the capacity to accept the disease and illness experience as part of their lives, engagement in social activities, and development of healthy lifestyles. Eventually, there was no absolute good-or-bad dichotomy between ill-being and well-being. Rather, the two forces were relative to each other with an individual’s functioning. For instance, the level of tolerance and intolerance of bodily discomfort was interdependent with one’s level of acceptance.
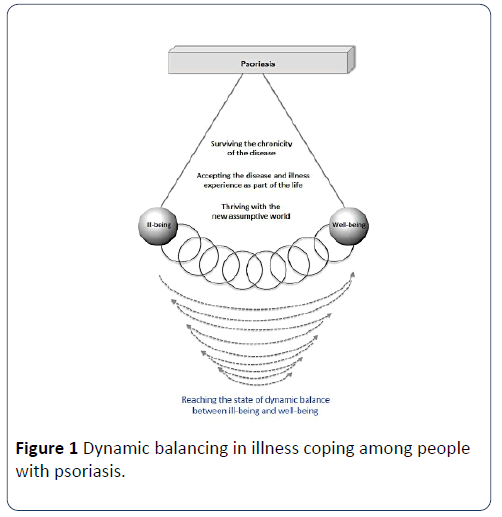
Figure 1: Dynamic balancing in illness coping among people with psoriasis.
To maintain a balance between ill-being and well-being in the illness experience, informants made the effort to normalize and try out new living experiences. Normal human life was the result of the interaction between ill-being and well-being, which helped maintain the constant state of dynamic balance. One of the important motives was social role performance within families and job settings. The obligation to perform duties and maintain expectations acted as an incentive to bounce back from ill-being. It was found that individuals who performed social roles displayed greater capacity than those who failed to maintain those roles due to the disease.
Illness did not necessarily lead to a miserable life, the inner strengths and capacity in coping among patients showed the greatest potential to facilitate the dynamic balancing in illness experience. Unfortunately, existing models do not adequately capture the active process of illness coping by including the negative experience of disease. The model proposed in this study has demonstrated the co-existence of positivity and negativity during the life course illness experience. Instead of symptom-focused analysis, the inner strengths embedded in the coping experience with psoriasis and life transitions were also highlighted. The enunciation of the ongoing oscillation between illness and wellness functioning may be beneficial for future development of psychosocial interventions for the psoriasis population.
Mainstream medical and psychosocial intervention approaches aim to help patients to ‘recover’ from illness or adverse situations. However, for patients with chronic illness whose original physical functioning is altered, it is unrealistic to emphasize the goal of recovery. Instead of ascertaining the resumption of functioning, the direction of integrating illness into life experience could better generate a balanced state of functioning.
Limitations
One of the major limitations of this study was the small sample size. The findings, based on 12 informants, reflected the experiences of a specific group of patients with psoriasis, might have limited generalizability. Another limitation relates to self-selected bias as most informants were recruited from the same community-based psoriasis patient group in Hong Kong. All informants were chosen based on available access and voluntary participation, which implies the limitation in generalization and the subjectivity of sampling to some extent. Patients hidden from the community due to avoidance of social interaction may represent other characteristics of illness experience, which may need further attention in any future study.
From a methodological perspective, the current study did not aim to categorize informants into specific illness stages because the proposed model suggested the coexistence of both positive and negative experiences. In fact, this study was conceded with what informants had come across in the management of their illness based on their personal understanding and interpretation at a certain time point. These perceptions, however, could eventually be changed by time so longitudinal study with interviews of the same informants at different time points should be considered in future research, in order to improve the accuracy of the dynamic balancing model.
Conclusion
With incurability and unknown etiology, psoriasis imposes multidimensional impacts on patients’ illness experience as do many other chronic illnesses. An increasing body of literature has shown interest in how patients can adaptively coexist with chronic illnesses. With respect to psoriasis, the findings in the current study contribute to a comprehensive understanding of the ongoing process in coping with psoriasis, in which dynamic balancing between psoriasis-specific strains, and individual strength has been reflected. There has long been a trend to regard psoriasis as a disease that generates emotional and social impairment. However, acceptance of psoriasis can also be considered as one of the surmountable challenges for patients. Active coping and positive thinking can be nurtured in surviving long-term medication and bio-psycho-social disruption of psoriasis. These can serve as an understanding for medical and counseling professions in engaging patients with psoriasis.
The dynamic balancing depicts an all-round life picture of patients with psoriasis. Instead of solely focusing on challenges that informants faced, their inner strengths as well as external resources are also revealed as survivor characteristics. On the basis of this finding, an integrative assessment of patients' conditions is required to achieve a full understanding of patients' life experience.
20035
References
- O'Neill P, Kelly P (1996) Postal questionnaire study of disability in the community associated with psoriasis. BMJ 313: 919-921.
- Rapp SR, Feldman SR, Exum ML, Fleischer AB, Reboussin DM (1999) Psoriasis causes as much disability as other major medical diseases. J Am AcadDermatol 41: 401-407.
- Koo J (1996) Population-based epidemiologic study of psoriasis with emphasis on quality of life assessment. DermatolClin 14: 485-496.
- Hrehorów E, Salomon J, Matusiak U, Reich A, Szepietowski JC (2012) Patients with psoriasis feel stigmatized. ActaDermVenereol 92: 67-72.
- Ginsburg IH, Link BG (1993) Psychosocial consequences of rejection and stigma feelings in psoriasis patients. Int J Dermatol 32: 587-591.
- Fried RG, Friedman S, Paradis C, Hatch M, Lynfield Y, et al. (1995) Trivial or terrible? The psychosocial impact of psoriasis. Int J Dermatol 34: 101-105.
- Choi J, Koo JY (2003) Quality of life issues in psoriasis. J Am AcadDermatol 49: 57-61.
- Kimball AB, Jacobson C, Weiss S, Vreeland MG, Wu Y (2005) The psychosocial burden of psoriasis. Am J ClinDermatol 6: 383-392.
- Finlay A, Coles E (1995) The effect of severe psoriasis on the quality of life of 369 patients. Br J Dermatol 132: 236-244.
- Krueger G, Koo J, Lebwohl M, Menter A, Stern RS, et al. (2001) The impact of psoriasis on quality of life: results of a 1998 National Psoriasis Foundation patient-membership survey. Arch Dermatol 137: 280-284.
- Weiss SC, Kimball AB, Liewehr DJ, Blauvelt A, Turner ML, et al. (2002) Quantifying the harmful effect of psoriasis on health-related quality of life. J Am AcadDermatol 47: 512-518.
- Gupta M, Gupta A (1998) Depression and suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis and psoriasis. Br J Dermatol 139: 846-850.
- Leventhal H, Leventhal E, Contrada R (1998) Self-regulation, health, and behavior: A perceptual-cognitive approach. Psychol Health 13: 717-733.
- Elwy AR, Yeh J, Worcester J, Eisen SV (2011) An illness perception model of primary care patients’ help seeking for depression. Qual Health Res 21: 1495-1507.
- Pettie, D, Triolo AM (1999) Illness as evolution: The search for identity and meaning in the recovery process. PsychiatrRehabil J 22: 255-262.
- Greenley JR, Mechanic D (1976) Social selection in seeking help for psychological problems. J Health SocBehav 17: 249-262.
- Bandura A (1986) Social foundations of thought and action: A social cognitive theory. Prentice-Hall, Englewood Cliffs.
- Clark NM, Gong M, Kaciroti N (2014) A model of self-regulation for control of chronic disease. Health EducBehav 41: 499-508.
- Grønning K, Lomundal B, Koksvik H Steinsbekk A (2011) Coping with arthritis is experienced as a dynamic balancing process: A qualitative study. ClinRheumatol 30: 1425-1432.
- Smith JA, Jarman M, Osborn M (1999) Doing interpretative phenomenological analysis. Qualitative Health Psychology: Theories and Methods. Sage Publications, London. pp: 218-240.
- Smith JA, Flowers P, Osborn M (1997) Interpretative phenomenological analysis and the psychology of health and illness. Material Discourses in Health and Illness. Routledge, London. pp: 68-91.
- De Korte J, Mombers FM, Bos JD, Sprangers MA (2004) Quality of life in patients with psoriasis: a systematic literature review. J InvestigDermatolSympProc 9: 140-147.
- Nelson PA, Chew-Graham CA, Griffiths CEM, Cordingley L (2013) Recognition of need in health care consultations: A qualitative study of people with psoriasis. Br J Dermatol 168: 354-361.
- Rasmussen GS, Maindal HT, Lomborg K (2012) Self-management in daily life with psoriasis: An integrative review of patient needs for structured education. Nurs Res Pract2012: 890860.
- Khoury LR, Danielsen PL, Skiveren J (2014) Body image altered by psoriasis. A study based on individual interviews and a model for body image. J Dermatolog Treat 25: 2-7.