Keywords
Secondary prevention; Coronary artery disease; Coronary artery bypass surgery; Cardiac rehabilitation
Introduction
Atherosclerosis-related coronary heart disease (CHD) has remained the leading cause of death globally for the past 40 years, accounting for one-third of all-cause mortality deaths, and its incidence is increasing by the each year in Taiwan [1,2]. Effective interventions that facilitate slowing CHD progression are essential and must be applied where appropriate. According to the American College of Cardiology/American Heart Association guidelines for the secondary prevention of CHD in patients with coronary and other atherosclerotic vascular diseases, a cardiac rehabilitation (CR) program should comprise appropriate exercise training; smoking cessation; blood pressure, sugar, and lipid management; and weight control [3-5]. Secondary prevention can control risk factors and reduce the degree of restenosis and mortality [6-9]. Lack of appropriate secondary prevention may lead to cardiac problems, requiring another invasive intervention.
Exercise-based CR is a crucial part of secondary prevention. CR can reduce risk factors and improve exercise capacity and survival after percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG). Furthermore, CR can enhance peak VO2; alleviate dyspnea or fatigue symptoms; improve oxygen utilization and quality of life; and reduce sympathetic tone [8,9].
Recently, most studies have reported that exercise-based CR reduces all-cause mortality by 15%–28% [6-9]. Adherence to CR may influence the survival benefits associated with CR. Studies have investigated the relationship between CR attendance and mortality, but the findings are mixed. In Sweden, CR attendance was associated with reduced mortality after 10 years but not after 5 years [10,11]. In a study on 846 CABG patients who received CR after surgery, a strong relationship was observed between CR attendance and longterm mortality reduction [8]. In a study on 544 coronary artery disease (CAD) patients, patients with < 25% CR attendance had a 2-fold higher mortality risk than did those with > 75% CR attendance. The study sample predominantly comprised younger men (73%; mean age, 62.5 ± 11.3 years) [10]. Several studies have reported that conditions such as traffic and work were the main reasons for poor attendance to an exercisebased CR program. Thus, programs that require minimum attendance and an enhanced exercise intensity progression proportion (EIPP) are essential for patients to undertake home-based exercise at an early stage, thus facilitating exercise regularity and promoting secondary prevention.
In this 6-year follow-up study, we examined the relationship between CR attendance and the cardiovascular event-free rate after CABG. Furthermore, we investigated whether a dose– response relationship existed among CR attendance, exercise intensity, and the short-term event-free rate.
Methods
Study population
In this retrospective cohort study, we evaluated the shortterm event-free rate of patients after CABG. We used data from the Cheng Hsin General Hospital (CHGH) database to identify patients who had undergone CABG January and December 2008 and excluded those who underwent combined surgery, those contraindicated for exercise, and those aged < 18 years. We included 266 patients (205 men, 78.5%) who had undergone CABG. To evaluate disease severity and avoid survival bias, we excluded 5 patients who died during hospitalization. All patients were encouraged to attend the CR program and retrospectively followed up for 6 years to determine their CR attendance and acute event incidence. All participants signed informed consent form before inclusion.
Exercise training intervention
The CHGH database was used for identifying patients who attended CR and those who did not (CR group [CRG] and NCR group [NCRG], respectively). Attendance was determined using the CR data in the CHGH database. In the CRG, CR attendance was defined as attendance of at least 1 outpatient session within 3 months of the index CABG. All patients who attended CR received aerobic exercise training and lifestyle counseling according to the guidelines of the American College of Sports Medicine (ACSM) and American Association of Cardiovascular and Pulmonary Rehabilitation. Most patients underwent a graded exercise test at the baseline as part of an exercise prescription. They were prescribed exercise for 20–40 minutes 3 times per week. The training program comprised warm-up, training, and cool-down phases. The training intensity depended on the anaerobic threshold (AT) obtained through the submaximal symptom-limited exercise test. If the patients did not achieve the AT, the peak VO2 was considered the training target.
In the NCRG, patients did not attend CR and received only accepted routine medical care. Furthermore, they did not receive any personal exercise consultations.
Study variables
The CHGH database was used for identifying patients who attended CR. The CR attendance rate was calculated as the number of sessions attended in 3 months divided by the number of CR sessions available in 3 months. The exercise intensity progression proportion was determined according to the proportion of the difference between the peak intensities achieved in the first and last sessions divided by the peak intensity achieved in the first session.
We searched inpatient files and reviewed medical charts to obtain basic data (sex, date of birth, height, weight, date of surgery, and discharge) as well as data on clinical characteristics (CAD risk factors, the New York Heart Association [NYHA] classification for heart failure, preoperative left ventricular function [preserved, mild, moderate, or severe dysfunction], coronary stenosis severity [number of artery stenoses], the use of left internal mammary artery grafts, and the ischemic time and pumping time), critical events (morbidity during hospitalization caused by acute renal failure and myocardial infarction [MI] during or after surgery), and functional performance (training intensity at first and last sessions, peak VO2, and %VO2 pred). The peak VO2 was derived from an exercise pulmonary function test (EPFT) using a modified Bruce protocol or a stationary bike ramp protocol.
Endpoints (outcomes)
The primary outcome in the 6-year follow-up was the incidence of cardiovascular events, such as death, which was ascertained using a 2-stage approach. All data on cardiovascular events, cardiac-related emergency room visits, repeat PCI, or repeat CABG were from charts. First, the vital status of the patients was extracted from the CHGH registration database. Second, patients with no record of death on the charts (indicated as alive) were ultimately censored on December 31, 2014. Patients who were not followed up in the outpatient department of CHGH were considered alive, and the last date of follow-up was obtained. The number of patients who developed cardiac events, including death and nonfatal MI, and underwent repeat CABG or percutaneous transluminal coronary angioplasty was identified, and the time to the first cardiac event was calculated.
Statistical Analysis
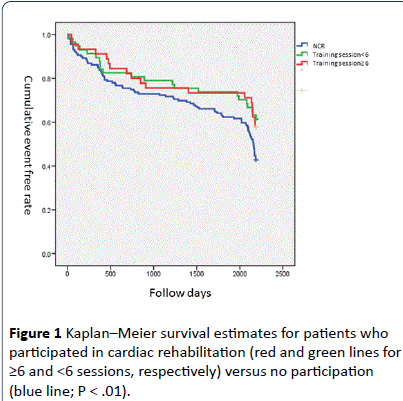
Baseline basic and clinical data are reported as means or proportions. To identify covariates that must be controlled in predictive analyses, we assessed the significance of any difference in baseline variables between the CRG and NCRG by using χ2 (for binary variables) and t tests (for continuous variables). Survival was described using the event-free rate. To describe the event-free rate of the study population, we plotted cumulative incidence estimates by using a single Kaplan–Meier curve for all patients and separate Kaplan– Meier curves for patients in the CRG and NCRG. We evaluated the differences between the separate curves by using the logrank test. For these analyses, the time at risk began on an event date and ended on the date of death or December 31, 2014.
To assess the relationship between the attendance and event-free rates, we constructed survival models. For the CRG, the CR attendance did not follow a normal distribution and was therefore classified into 2 categories of ≥ 6 and < 6 sessions. A 2-sided P value of .05 was considered statistically significant.
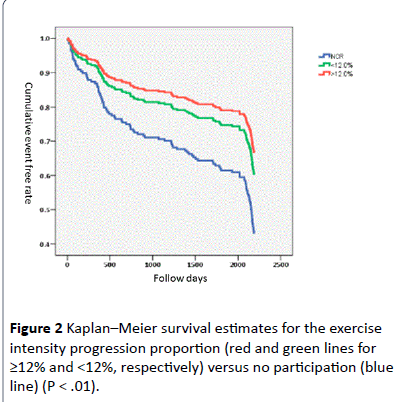
To assess the relationship between the exercise intensity progression proportion (EIPP) and the event-free rate, we constructed additional survival models. For the CR group, EIPP was derived from the maximal intensity difference between the first and last session divided by the %VO2 at the first session. This variable did not follow a normal distribution and was therefore classified into 2 categories, ≥ median and < median, on the basis of attendance.
Results
In this study, 266 post-CABG patients admitted to CHGH between January 2008 and December 2008 were selected. Five of the 266 patients who died during hospitalization were excluded, and the remaining 261 patients were enrolled. The number of patients was 102 and 159 in the CRG and NCRG, respectively. Basic demographic and clinical characteristics are listed in Table 1. The demographic data did not differ significantly between the 2 groups, except for age, ischemic time, and pumping time (Table 1). The mean follow-up period was 64.9 ± 23.7 months, and the event-free rate was 78.5%.
Data are presented as mean (SD) or No. of patients (%).
BMI: Body Mass Index, HTN: Hypertension, DM: Diabetes Mellitus, Hos duration, duration of hospital stay.
CR sessions and event-free rate
According to the ACSM risk stratification guidelines, patients in classes A and B were recommended to attend at least 6 CR sessions. The mean number of CR sessions was 13.3 ± 12.9 in the CRG. Patients who participated in CR had a significantly higher 6-year event-free rate than that of patients who did not participate (P < .01). The event-free survival curves for 6 years revealed that the event-free rate was 59.8% for the CRG and 42.8% for the NCRG. The event-free survival rate was 57.8% in 45 patients who attended ≥ 6 sessions and 61.4% in 57 patients who attended < 6 sessions. KM event-free survival curves of CR attendance based sessions ≥ 6 sessions versus < 6 sessions was shown in Figure 1. The event-free survival rates were not significantly different between the 2 groups of the CRG, but they were significantly higher than those of the NCRG (event-free rate: 42.8%).
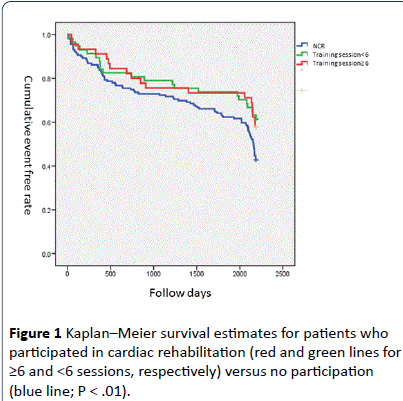
Figure 1:Kaplan–Meier survival estimates for patients who participated in cardiac rehabilitation (red and green lines for ≥6 and <6 sessions, respectively) versus no participation (blue line; P < .01).
EIPP and event-free rate
In the CRG, the intensity difference ratio between the first and last training sessions represented EIPP. ROC curve analysis revealed a significant intensity difference (12%) in the 6-year follow up. But 32 patients in CRG joined only 1 CR session. These patients were exclude for EIPP calculation. We divided the CRG into 2 subgroups as follows: EIPP ≥ 12% (n = 27), and EIPP < 12% (n = 43). No significant difference was observed in the event-free rate between the 2 groups (66.7% versus 60.5%); however, event-free rate in both subgroups was significantly higher than that in the NCRG (42.8%). KM eventfree survival curves of EIPP based EIPP ≥ 12% versus < 12% was shown in Figure 2.The hazard ratios [HRs] of the training intensity difference in both subgroups ( ≥ 12% and < 12%) were significantly higher in the NCRG than in the CRG (HR: 0.601 vs. 0.482, 95% CI: 0.243–0.956 vs. 0.358–1.008).
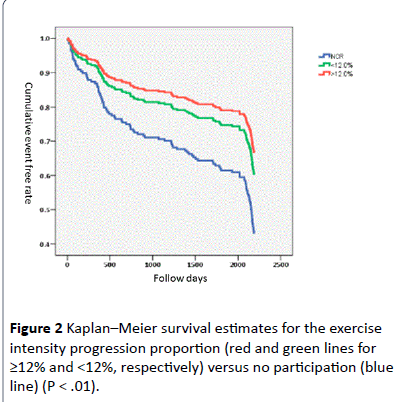
Figure 2:Kaplan–Meier survival estimates for the exercise intensity progression proportion (red and green lines for ≥12% and <12%, respectively) versus no participation (blue line) (P < .01).
Discussion
Previous studies have suggested that CR is associated with more favorable outcomes in CAD patients, and clinical trials have suggested that CR is beneficial to health [6,9,10,12-15]. In our study, we extended the findings of previous studies by examining a cohort of CABG patients, using the suggested proportion of exercise intensity progression between the first and last CR sessions, assessing both the event-free rate and EIPP, and exploring the relationship between CR patterns and the event-free rate.
In our study, the CRG was associated with a higher eventfree rate than that of the NCRG, which is consistent with the findings of previous studies [6,8,9]. The CRG patients were strongly encouraged to lead an active lifestyle and received intensive supervised exercise training. On average, the CRG patients joined 13.3 ± 12.9 sessions in 3 months. Physical training may reduce mortality and morbidity in CAD patients [6] (Table 2). A comprehensive CR program improved the longterm prognosis and reduced the need for hospital care in CABG- and MI-based studies [7,8]. These findings support the U.S. guidelines and coverage policies that recommend CR participation after CABG [8].
A few studies have investigated the exercise dose–response relationship. All of these studies assessed the relationship between the number of exercise sessions attended and the mortality or event-free rate [6,9,23]. However, regarding clinical implications, functional performance was associated with exercise intensity. Exercise training can significantly improve peak oxygen consumption, the exercise duration, the resting heart rate, and quality of life. Our study was the first to investigate the relationship between EIPP and the event-free rate. If EIPP is ≥ 12% compared with the baseline value, the 6- year event-free rate decreases significantly.
In this study on post-CABG patients who did and did not participate in CR, we observed no significant dose–response relationship. No significant difference in the event-free rate was observed for the 2 CR attendance groups, but the eventfree rate in the CRG was significantly higher than that in the NCRG during the 6-year follow-up. We speculate that the number of CR sessions might not affect the results. Evidence on the dose–response relationship between CR and event-free survival rate among patients with CHD is mixed. Most authors have reported benefits associated with an increasing number of CR sessions and a dose response to exercise [9,10,12,15-23]. The mortality rate significantly decreased in patients who attended ≥ 25 CR sessions [15-23]. The mortality risk was 2- fold higher in patients with acute MI, CABG, or PCI and ≤ 25% CR attendance than in those with ≥ 75% attendance [10]. The 1- and 5-year mortality rates decreased by 58% and 19%, respectively, in patients who attended more CR sessions. A community-based study reported that CR participation was significantly associated with an approximately 45% reduction in all-cause mortality. Although the number of sessions attended was not associated with long-term mortality, after adjustment for age, sex, and the Charlson index, [8] a 1% decrease in mortality was observed with each additional session attended (unadjusted HR, 0.99; 95% CI, 0.98–0.99) [6]. Each additional CR session was associated with a 6% (HR, 0.94; P < .001) lower risk of MI [9].
Our study strongly supports the notion that CR participation reduces the event-free rate. However, this study was limited by several factors. First, our data were obtained from a single medical center, and the patient population might be limited. The medical center is the first comprehensive heart center in Taiwan and was visited by patients from throughout Taiwan; thus, the findings of this study are highly generalizable. Second, a potential for bias exists because of the unmeasured underlying health statuses of patients. Patients who attended < 6 CR sessions may be generally healthier than those who did not attend CR sessions. In addition, there may be residual confounding by the health status even among these patients, although the direction in which the health status may bias the results is unclear. Healthier patients may not feel motivated to attend CR and may be likely to attend fewer sessions than other patients do. Furthermore, less healthy patients cannot tolerate CR and thus may attend fewer sessions than their healthy counterparts do. Third, patients might be lost to follow-up at the original hospital, and hence the primary endpoint may be lost. However, our research assistant made specific phone calls to follow up with the patients.
Conclusions
CR is associated with more favorable outcomes in CAD patients.CR attendance and EIPP ≥ 12% are associated with higher event free survival rate. Our results strongly support national policy that CR is recommended for CABG.
Acknowledgments
The authors thank Yu-Jen Wang for data collection, and all the studied subjects for their consents to join the study.
Funding
This research received no grant from any funding agency in the public, commercial or not-for-profit sectors.
Disclosures
The authors declare that there is no conflict of interest.
9503
References
- Lee CW, Wu YT, Tsai MW(2010) Age Stratification in Traditional Coronary Risk Factors in Eastern Taiwan Male with Acute Myocardial Infarction. FJM 14:485-495.
- https://www.mohw.gov.tw/CHT/Ministry/DM2_P.aspx?f_list_no=7&fod_list_no=5313&doc_no=49778/.
- Smith SC, Allen J, Blair SN, Bonow RO, Brass LM, et al. (2006) AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 113: 2363-2372.
- Thomas RJ, King M, Lui K, Oldridge N, Piña IL, et al. (2007) AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services. Circulation 116: 1611-1642.
- Thomas RJ, King M, Lui K, Oldridge N, Piña IL, et al. (2010) AACVPR/ACCF/AHA 2010 update: performance measures on cardiac rehabilitation for referral to cardiac rehabilitation/secondary prevention services: a report of the American Association of Cardiovascular and Pulmonary Rehabilitation and the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Clinical Performance Measures for Cardiac Rehabilitation). Circulation. 122: 1342-1350.
- Martin BJ, Hauer T, Arena R, Austford LD, Galbraith PD, et al. (2012) Cardiac rehabilitation attendance and outcomes in coronary artery disease patients. Circulation 126: 677-687.
- Hedbäck B, Perk J, Hörnblad M, Ohlsson U (2001) Cardiac rehabilitation after coronary artery bypass surgery: 10-year results on mortality, morbidity and readmissions to hospital. J Cardiovasc Risk 8: 153-158.
- Pack QR, Goel K, Lahr BD, Greason KL, Squires RW, et al. (2013) Participation in cardiac rehabilitation and survival after coronary artery bypass graft surgery: a community-based study. Circulation 128: 590-597.
- Hammill BG, Curtis LH, Schulman KA, Whellan DJ (2010) Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation 121: 63-70.
- Beauchamp A, Worcester M, Ng A, Murphy B, Tatoulis J, et al. (2013) Attendance at cardiac rehabilitation is associated with lower all-cause mortality after 14 years of follow-up. Heart 99: 620-625.
- Hedbäck B, Perk J, Wodlin P (1993) Long-term reduction of cardiac mortality after myocardial infarction: 10-year results of a comprehensive rehabilitation programme. Eur Heart J 14: 831-835.
- Whellan DJ, Shaw LK, Bart BA, Kraus WE, Califf RM, et al. (2001) Cardiac rehabilitation and survival in patients with left ventricular systolic dysfunction. Am Heart J 142: 160-166.
- Alter DA, Oh PI, Chong A (2009) Relationship between cardiac rehabilitation and survival after acute cardiac hospitalization within a universal health care system. Eur J CardiovascPrevRehabil. 16: 102- 113.
- Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, et al. (2004) Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med 116: 682-692.
- Lavie CJ, Milani RV (2011) Cardiac rehabilitation and exercise training in secondary coronary heart disease prevention. ProgCardiovasc Dis 53: 397-403.
- Chow CK, Jolly S, Rao-Melacini P, Fox KA, Anand SS, et al. (2010) Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation 121: 750-758.
- Grace SL, Russell KL, Reid RD, Paul O, Anand S, et al. (2011) Cardiac Rehabilitation Care Continuity Through Automatic Referral Evaluation (CRCARE) Investigators. Effect of cardiac rehabilitation referral strategies on utilization rates: a prospective, controlled study. Arch Intern Med. 171: 235- 241.
- Dunlay SM, Witt BJ, Allison TG, Hayes SN, Weston SA, et al. (2009) Barriers to participation in cardiac rehabilitation. Am Heart J 158: 852-859.
- Heran BS, Chen JM, Ebrahim S, Moxham T, Oldridge N, et al. (2011) Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev : CD001800.
- Goel K, Lennon RJ, Tilbury RT, Squires RW, Thomas RJ (2011) Impact of cardiac rehabilitation on mortality and cardiovascular events after percutaneous coronary intervention in the community. Circulation. 123: 2344- 2352.
- Lawler PR, Filion KB, Eisenberg MJ (2011) Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Am Heart J. 162: 571-584.
- O'Connor CM, Whellan DJ, Lee KL, Keteyian SJ, Cooper LS, et al. (2009) Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 301: 1439-1450.
- Suaya JA, Stason WB, Ades PA, Normand SL, Shepard DS (2009) Cardiac rehabilitation and survival in older coronary patients. J Am CollCardiol 54: 25-33.