Keywords
HIV/AIDS; HIV Linkage; HIV Enrolment
Introduction
HIV/AIDs is a global epidemic that affects the immune system of all those who get into contact with the disease. Globally, there was approximately 36.7 million people worldwide living with HIV/ AIDS at the end of 2016. Of these, 2.1 million were children (<15 years old). An estimated 1.8 million individuals worldwide became newly infected with HIV in 2016 – about 5,000 new infections per day. This includes 160,000 children (<15 years). Most of these children live in sub-Saharan Africa and were infected by their HIVpositive mothers during pregnancy, childbirth or breastfeeding. Currently only 60% of people with HIV know their status. The remaining 40% (over 14 million people) still need to access HIV testing services. As of July 2017, 20.9 million people living with HIV were accessing antiretroviral therapy (ART) globally, up from 15.8 million in June 2015, 7.5 million in 2010, and less than one million in 2000 [1].
This study evaluated the effectiveness of HIV linkage of newly diagnosed HIV positive clients following the initial HIV/AIDs testing focusing on Mukono and Mengo hospitals’ HIV departments. The independent variable ‘HIV testing and linkages’ is divided into testing and linkage time, recorded linkages, and linkage obstacles whereas the dependent variable ‘enrolment for care’ is categorized into information, prescription, treatment, and routine check-ups. The study focused on the analysis of the current prevalence rate, opportunistic infections, deaths, and attitude of those tested positive towards enrolling for treatment. The study also focused on issues of stigma, denial, distance, negligence, and ignorance. This chapter presents the background, the research problem, purpose, objectives, research questions, hypotheses, significance, justification, scope, conceptual framework, as well as, definitions of terms and concepts used in the study [2].
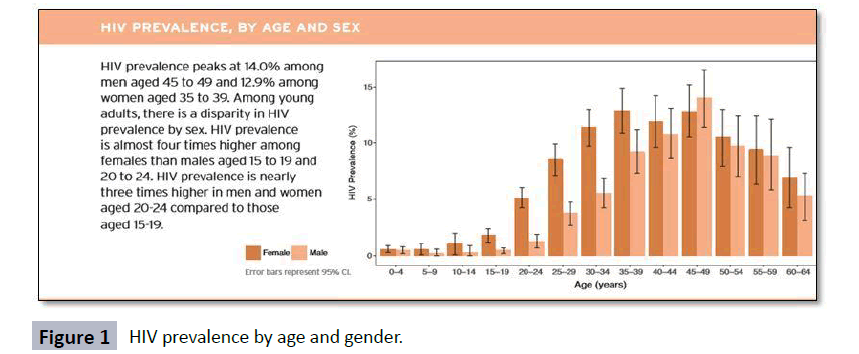
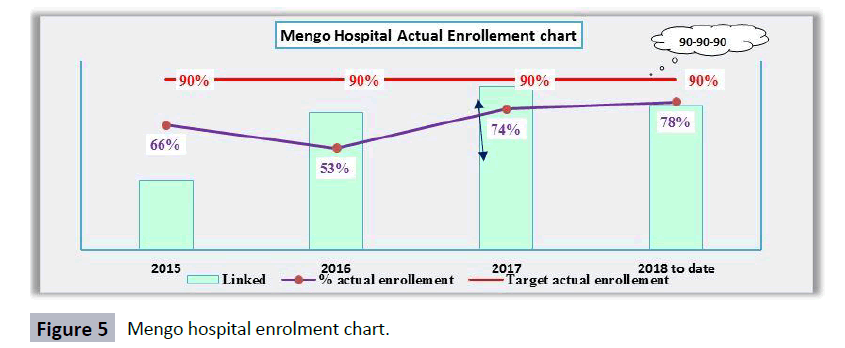
The selection of the above variable as focus for the study was based on the fact that the HIV situation in Uganda remains a big challenge. The reports indicate that many young people, especially girls aged between 15 and 24, are disproportionately affected by HIV infection. The report further indicates that Uganda registers 230 HIV new infections a day with an average of 1,300,000 to 1,600,000 people living with HIV/AIDS in 2015 as indicated in the. Among the reasons for the increasing numbers is due to the linkage gap of HIV positive clients from the identification level to care entry point following testing. Many HIV positives are tested and diagnosed from the HCT point then linked to but less enroll into care hence causing a big gap between those linked and actually enrollments. This gap and the factors contributing to it were the overall focus of this study (Figure 1).
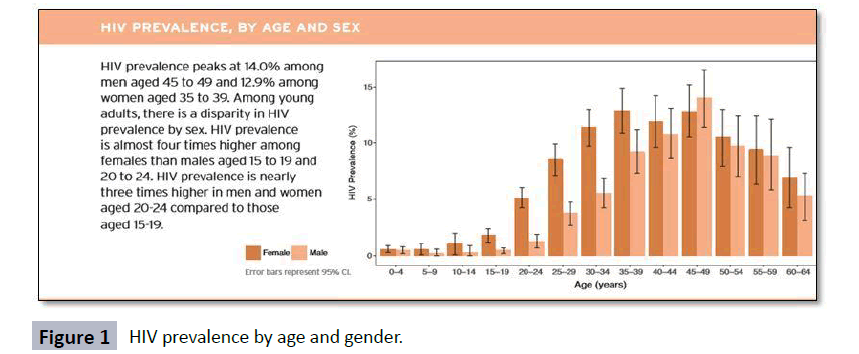
Figure 1: HIV prevalence by age and gender.
Research Background
AIDS-related deaths have declined from a peak of about 1.9 million in 2005 to around 1.0 million in 2016, largely due to treatment scale-up—for the first time more than half of people with HIV are estimated to be on treatment. Since 2010, the annual number of new infections in all age groups has decreased by 16% to around 1.8 million in 2016. However, progress is variable, and despite a global downward trend in the epidemic, several regions are experiencing sharp increases in new infections and struggling to expand treatment. More than two-thirds of people living with HIV knew their status in 2016. Around 77% of them were on treatment, and 82% of those on treatment had suppressed viral loads. In 2016, around 19.5 million people with HIV (53%) were on treatment, up from 17.1 million in 2015 [3-5].
In the Middle East and North Africa, trends vary, and although numbers of new infections seem stable since 2010, AIDS-related mortality has increased in the past decade. In the same period in Eastern Europe and central Asia, the number of new infections has risen to 190 000 in 2016, a 60% increase. The region's HIV epidemic is mainly within two countries: Russia and Ukraine. People who inject drugs accounted for 42% of new HIV infections in the region in 2015. In both countries, there are large gaps across the 90-90-90 continuum. HIV testing and treatment coverage are low. Key populations in these regions are unable to access services and linkage to care is weak. These regions are unlikely to meet the 90-90-90 target [6,7].
East and Southern Africa is the region hardest hit by HIV. It is home to 6.2% of the world’s population but over half of the total number of people living with HIV in the world (19.4 million people). In 2016, there were 790,000 new HIV infections, 43% of the global total. South Africa accounted for one third (270,000) of the region’s new infections in 2016. Another 50% occurred in eight countries: Mozambique, Kenya, Zambia, Tanzania, Uganda, Zimbabwe, Malawi, and Ethiopia. Just fewer than half a million people (420,000) died of AIDS-related illnesses in the region in 2016, although the number of deaths has fallen significantly from 760,000 in 2010 (AVERT report 2017 East and south African region) [8,9].
The HIV situation in Uganda calls for renewed and urgent action. This was highlighted at the end of a UNAIDS Global Review Mission to Uganda, which held multi stakeholder consultations in Uganda 21st to 23rd of February 2017. Young people, especially girls aged between 15 and 24, are disproportionately affected by HIV infection. Among adolescent girls; every single hour, 2 young women are getting infected with HIV in Uganda. The prevalence of HIV among adolescent girls stands at 9.1 percent, compared to the national prevalence rate of 7.3 percent. Uganda registers 230 HIV new infections a day. Despite widely available antiretroviral therapy, 76 people die of AIDS-related causes every single day! This illustrates the urgent unfinished business of ending AIDS, made more worrisome by recent calls to reduce the health and education budgets, that are important sectors for the fight against HIV, which at this critical time, do not augur well for ending the epidemic.
The effects of reluctance to enroll for treatment after testing positive has exposed more citizens to new infections due to the increased viral loads for the initiated on ART. Due to increased viral load copies in those who are not no ART, there more infections to all those who get exposed with those not on ART eventually led to increased HIV prevalence and increased HIV related deaths (Uganda AIDs Commission Review Report, 2017). From the UPHIA data 2017, show that the viral load suppression among HIV positive patients is still low indicating that many people still have a high content of the virus risking more citizens to get HIV in case of any sexual intercourse [10].
Statement of the problem
HIV remains an epidemic still claiming many lives in Uganda, this is due to challenge of many people testing positive but do not actually enroll into care even when they have been linked. This has led to more people getting infected by those who don’t seek treatment, which increasing HIV spread. This is a reality at Mukono and Mengo hospital where, according to a 2016 Health Services Audit Report, 39% and 44% respectively were linked and enrolled after initial testing of HIV immediately. This created a gap of 61% and 56% of Mukono and mengo hospital respectively, most those who test positive feel stigmatized, stay in denial and some due to distance prefer to get enrolled to other health facilities near where they live [10].
According to a report from the Uganda AIDS Commission, HIV positive clients in hospitals in Uganda, some of which included Mukono and Mengo hospitals, are not immediately enrolled after testing eventually don’t enroll. Additionally, the same report indicates that people who test HIV positive by do not enroll think of enrollment when they get sick and weak. The effects of reluctance to enroll for treatment after testing positive has led to reduced viral load suppression levels that eventually led to increased HIV prevalence and increased HIV related deaths (Uganda AIDs Commission Review Report, 2017). From the UPHIA data 2017, show that the viral load suppression among HIV positive patients is still low indicating that many people still have a high content of the virus risking more citizens to get HIV in case of any sexual intercourse.
The study therefore evaluated the effectiveness of HIV testing and linkage of newly diagnosed HIV positive clients to care services so as to produce relevant findings based which hospitals and others offering HIV care services could base to make informed decisions about enrolment of HIV clients into care [11].
Research Objectives
To evaluate the completeness and effectiveness of HIV testing and linkage on enrollment of HIV positive clients into care with specific objectives as below;
• To assess the linkage time lag between the time of testing and the time of actual enrollment of people that test HIV positive.
• To examine variance between the reported linkages and actual enrollments.
• To assess the obstacles to enrollment for care.
Research Questions
• Why is there linkage time lag between the time of testing and the time of actual enrolment?
• What causes variance between reported linkages and actual enrolment?
• What are the different challenges faced that hinder them from linking immediately?
Justification of the Study
The various challenges of most positive clients that are not immediately enrolled from the same facility that they tested from eventually don’t enroll. Furthermore, patients tested think of enrollment when they get sick and weak hence reducing viral load suppression which risks more people getting infected with HIV to increase infections. The effects of reluctance to enroll for treatment after testing positive has led to increased HIV prevalence and increased HIV related deaths. These problems may not be fully solved if Mukono and Mengo hospitals don’t know the effectiveness HIV linkage of newly diagnosed HIV positive clients following the initial testing. This study, thus, is necessary to evaluate the effectiveness HIV linkage of newly diagnosed HIV positive clients following the initial HIV/AIDs testing. Ministry of health (MOH) under the government of Uganda passed the national 90-90-90 policy that advocate for test and treat, All those HIV positive clients are tested and know their HIV status, and all are started on ART and they are virally suppressing. When you identify an HIV positive client, immediately ensure that you give them ARVs faster before anything and then link to care. This would help them suppress the viral load [12-16].
Methodology
The nature of the study is Qualitative and minimal quantitative methods. Qualitative data helped the researcher to get first hand insight to the study and understanding fully the respondent’s ideas from an insider’s perspective. The study used a qualitative research design and it mainly used personal interviews which entailed face to face interviews, semi structured questionnaires for health workers and patients, key informant interviews (from the health service providers especially those dealing with HIV/AIDs) and informal discussions (for example the use of case stories).
Qualitative data was collected using an open ended questionnaire which was administered to counselors and HIV positive clients in Mukono and Mengo hospitals. Interviews were used to collect data from doctors who attend to HIV positive clients in Mukono and Mengo hospitals. A total of 72 respondents actually participated in answering the questionnaire and responding to interview questions. The questions asked on the questionnaire and in the interviews were based on each of the study objectives. Under the first objective about linkage time lag between the time of testing and the time of actual enrolment clients whose test results show they are HIV positive the questions asked focused on: whether clients that tested HIV positive were willing to enroll for care, a description of the procedure for linkage, the attitude of clients while undergoing linkage HIV care, and the how the hospitals (Mukono and Mengo hospitals) dealt with clients less interested in completing the procedures for linkage.
The target population for this study was 94 respondents comprising doctors, counselors, and HIV positive patients (Table 1). It was mainly focusing on clients of mainly adults who tested HIV positive and those already in care, assessing how long it took them to accept and enroll in care. The doctors and Nurses are believed to have a lot of information on these clients the fact that they work on them. This depends on the how long they stayed that particular hospital. Using the Krejcie and Morgan tables for sample size determination, a sample/accessible population for this study was determined to be 83 respondents as detailed in the sections below.
Table 1 Sample size by population categories.
| Population category |
Target Population (N) |
Sample (n) |
Data Type |
Research Instrument |
Sampling technique |
| Doctors |
8 |
8 |
Primary/Secondary |
In-depth Interviews |
Purposive Sampling |
| Counsellors |
36 |
21 |
Primary/Secondary |
In-depth Interviews |
Purposive Sampling |
| HIV Positive Patients |
50 |
44 |
Primary/Secondary |
Questionnaire and In depth Interviews |
Systematic Sampling |
| Total |
94 |
83 |
|
|
|
Sample Size and Selection
From the study population mentioned above, an appropriate sample size for each of the respondent categories were purposively selected, as illustrated in the table below, tables for sample size selection (Table 2). The samples include medical doctors currently working in the HIV departments in the different hospitals of Mengo and Mukono hospital that are directly involved in HIV testing and care. The counsellors included in the sample are also involved in fulltime counselling of HIV clients at the hospitals, whereas the clients selected for sampling were tested for HIV at HIV departments and referred for care. For secondary data, the study population sampled was only those newly diagnosed HIV positive, those that enrolled and those who preferred to be referred to other centres that didn’t actually reach but instead stayed in community [17].
Table 2 Number of respondents sampled by facility.
| Population category |
Mengo Hospital |
Mukono Health Centre IV |
| Doctors |
4 |
4 |
| Counsellors |
16 |
15 |
| HIV Positive Patients |
24 |
20 |
| Total |
44 |
39 |
The Table 2 below, guided by Krejcie et al. for sample determination, presents the respective respondent categories, the population of the study and the respective samples, as well as the sampling techniques that was used for each respondent category. The selected population sample was from Mengo and Mukono hospitals. The respondents included in the sample from each of the two hospitals include doctors, counselors, and HIV positive clients. The sampling approaches that will be used in this study include stratified, simple random and purposive sampling as described. The study also sampled secondary data for all those that were tested positive, enrolled and preferred to be transferred to other nearby facilities due to different reasons of stigma, distance, accessibility, costs and comfort.
The distribution of respondents per facility was equal basing on representation to obtain balanced findings from both hospitals. Both hospitals have the same average number of clients seen per day and active in care. Since one is private (Mengo Hospital) and another government sharing the sample equally presented views from the different environments.
Data Collection Methods
The primary data collection methods used was questionnaire survey, secondary reviews and interviews. This research employed Questionnaire and interview data collection methods since it involved some questions completed and returned by the respondents and others completed through interviews. Secondary reviews were used to collect secondary data from the hospital systems and reports for more analysis.
Data collection took place over a period of two months. Before information gathering process, the researcher looked for authorization from the Hospital research offices and administrations to complete the study in the area. This helped to get the hospital authorization but also to operate in line with the research ethics committee considering the ethical considerations. The researcher additionally sought for authorization from health workers to take an interest in the study. The information was gathered through narrative investigation or record audit (document review), direct perception and casual talks; researcher administered questionnaires and interviews. Unstructured surveys were used as information gathering instruments during the meetings.
Data collectors primarily included Health workers and facility linkage facilitators. Personal interviewing as another data collection strategy included up close and personal collaboration with the respondents and the interview guides were used to gather information from form the hospitals. Report audit/ document review was used to gather secondary information from hospital reports and data bases [18].
Procedure of Data Collection
In order to recruit primary respondents for interviewing, appointments were made with the relevant respondents by the FLFs. For Health workers appointments were made and interviews were carried out immediately because of their tight schedule. The researcher divided the respondents into different days ten per week for the patients and for doctors and counselors, interviews were conducted as the get free time due to their tight schedules. For the interviewers, each one was required to sign as oath of confidentiality ensuring that information collected from The questionnaires were administered to all and data collected, it was entered into a data base called EPI-Info for qualitative analysis through assigning thematic to the different responses.
Additionally for secondary data, the researcher asked for access to the soft copy HIV testing and counseling data bases for the respective hospitals with authority from the administrators. This data was capturing indicators of number tested positive for the given period of time, number linked to care then total number who actually linked/enrolled immediately. This secondary data helped the researcher to understand the trends of linkage for the respective hospitals (Mukono and Mengo hospitals) in order to get more reliable representative data for analysis [19].
Data Quality Control
Pre-testing of the sample was done using 5 respondents from the study population to validate the questionnaire and interview guide for targeted respondents. The purpose of conducting a pre-test was to test the rigor of the appropriateness of the research questionnaire tool. The pre-testing ensured clarity and consistency throughout the study. The system used for analysis also had data quality controls in it where some questions had options where the respondents would choose from to avoid enormous wrong data. For the secondary data, quality checks were put in place in the analysis software to ensure that quality checks are put in place.
Validity
Validity is the extent to which research instruments measure what they are intended to measure. The researcher used expert judgment of the supervisors and other reviewers to confirm the validity of the instruments. The relevance of each item in the research instruments to the research objectives was evaluated. The reviewers rated each item as either relevant or not relevant. Validity was determined using Content Validity Index (C.V.I).
C.V.I=Items rated relevant by both judges divided by the total number of items in the questionnaire as shown below:
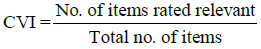
According to Amin, after calculation based on the contents of the questionnaire, the instrument that scores above 0.7 is considered valid.
Reliability
Reliability is commonly used as a measure of the internal consistency or reliability of a psychometric test score for a sample of examinees. According to Sekaran a reliability of 0.70 or higher (obtained on a substantial sample) is required before an instrument is used. Upon performing the test, the results should be 0.7 and above to be considered reliable.
Data Management
Data collection was done over a period of two month. A team of research assistants was led by the researcher to collect data. In the first week data collection instruments were pre-tested on five respondents then the scoring of patient’s case management files. In the second week, making appointments with respondents was done. In the third and fourth week, questionnaires was administered and collected from all the selected respondents. In the fifth and sixth week, interviews with key respondents were conducted. In the seventh and eighth week, all collected data was sorted, coded and analysed.
Data generated from open ended interview questions were used in the qualitative analysis. The information was studied and categorized according to context; the responses were grouped according to the dominantly relevant themes. The Likert scale is chosen because it is easier to use compared to other methods.
Data Analysis
This data was collected and entered in Epi-info for aggregation from which we finally extracted and analysed. For secondary data, it was already entered in an excel data base at the respective facilities where we extracted and cleaned for analysis [20].
Qualitative data analysis
Qualitative data responses was transcribed, sorted and classified according to identified relevant themes. Data analysis was done in Epi-Info/excel and responses capturing people’s perceptions, attitudes, views, sentiments, etc. were summarized according to the research questions: why don’t HIV positive clients enroll for care after being linked; how long does it take for an HIV positive diagnosed clients to actually enroll in care; what are the different challenges faced that hinder them from linking immediately. Analysis was finally represented in tables and graphs as shown below.
After collecting qualitative data analysis was done using excel where categorization of the responses was done and then summarized the findings according to the categorization. Then after converting all the data I excel number formats then all was migrated into excel where more analysis happened [21].
Quantitative Data Analysis
Qualitative data analysis was used to analyze the secondary data for the different facilities across the year per quarter. It included variables such as number of those tested HIV positive, those linked to care, how many enrolled immediately at linkage, how many were referred to other health facilities and how many didn’t enroll following initial testing. Data entry was done in Epi- Info and analysis done in excels using pivots and chats to make graphs. SPSS analysis package was also used to in analysis to carry out comparatives between different variables and understand if the data is statistically significant. It was used to assess the relationship between enrolment verses gender, enrolment verses age, enrolment verses education and enrolment relationship to the challenges.
Results
Background characteristics of the respondents
The background characteristics of primary respondents who were interviewed in the study are discussed in this Table 3 below. Primary respondents were clients who are HIV positive in both hospitals. The level of education, gender and age was also considered in the study. Key informants were the doctors and counselors who have worked in the respective HIV departments for the hospitals for some time. Data presentenced was significantly representing 93% of females that were linked enrolled into care while only 46% of males that were linked enrolled into care.
Table 3 Background characteristics of primary respondents.
| Characteristics |
Female |
Male |
P Value |
| Population |
27 (68%) |
13 (33%) |
<0.001 |
| Age in years |
| Median (IQR) |
34.0 (27-47) |
33.0 (26-41) |
0.736 |
| 21-30 |
11 (41%) |
6 (46%) |
| 31-40 |
8 (30%) |
3 (23%) |
0.904 |
| 41-55 |
8 (30%) |
4 (31%) |
| Education Level |
| Secondary |
10 (37%) |
6 (46%) |
0.581 |
| Degree/Diploma |
17 (63%) |
7 (54%) |
| Hospital/Facility |
| Mengo Hospital |
16 (21%) |
7 (14%) |
0.324 |
| Mukono Health Centre IV |
59 (79%) |
42 (86%) |
| Time lapse to accept linkage to care |
| Time (Hours) |
7.0 (3-12) |
24.0 (15-34) |
0.001 |
| Enrolment into Care |
| No |
2 (7%) |
7 (54%) |
<0.001 |
| Yes |
25 (93%) |
6 (46%) |
Demographic characteristics of respondents
This section presents the demographic characteristics of the respondents. The gender, age, relationship, period of stay with hospital by the HIV Positive respondents and education level is highlighted in this section. Figure 2 above shows that the majority of the respondents, 68.06% were Females, as compared to 31.94% Male. Majority of the respondents were female because the study population comprised more females than male active participating in the study. Females access health care interventions more compared to the male counterparts. These findings are in agreement with the UPHIA 2017 report that highlights that HIV health care is high in females.

Figure 2: Distribution of respondents by gender.
Females have the antenatal clinic where they access maternal care; this has given them more opportunities to test for HIV. During the interviews a 28 years married woman from kojja village enrolled in Mukono health centre IV agreed to the notion by saying the following in her own words:
“I was requested by a doctor to come with my husband when tested HIV positive. When I asked him, he just quarreled and told me for him he doesn’t sleep around and he is too busy for that. When I insisted he threatened to chase me away from his home. I tested to know my HIV status so that if positive I protect my child but my husband doesn’t care”.
Table 4 above shows that the majority of the respondents, 41.8% were between the ages of 18-30 years, while 28.1% were between 31-40 years, while 20.0% were between the ages of 41-50 years. The study registered high numbers of HIV positive respondents between ages 18-30 because HIV prevalence is most in this age bracket (UPHIA report 2017). Only 10.1% were 51 years and above since they are passed the sexually active stage. The majority of the respondents were between the ages of 18-30 years because this age category comprised most of the key respondents of the project, patients/clients.
Table 4 Distribution of respondents by age.
| Age (Years) |
Frequency |
Percentage |
| 18-30 |
30 |
41.80% |
| 31-40 |
20 |
28.10% |
| 41-50 |
14 |
20.00% |
| 51 and above |
8 |
10.10% |
| Total |
72 |
100.00% |
Table 5 above shows that the majority of respondents 65.4% had interacted with the hospital for between 4 – 6 years, while 10.9% for 7 years and above, and 24% between 1-3 years. Relationships means the number of time the staff/client has spent in the hospital. Since those respondents who have interacted with the hospital for a longer period were represented in the study, may mean a reliable representation of the population from the most informed category.
Table 5 Distribution of respondents by years of relationship.
| Years in relationship |
Frequency |
Percentage |
| 01-Mar |
17 |
24% |
| 4-6 |
47 |
65.40% |
| 7 and above |
8 |
10.90% |
| Total |
72 |
100.00% |
Findings on linkage time lag between the time of testing and the time of actual enrollment of people that test HIV positive
Impact of time lag to enrolment outcomes: The findings on this research objective was analysed through SPSS, the research used it to understand the time lag factor from the time of testing to time of enrolment. In this analysis the outcome is enrollment into care. We used generalized linear models with a Poisson distribution that looks at discrete frequency distribution which gives the probability of a number of independent events occurring in a fixed time. It was used to generate relative risk ratios and 95% confidence intervals involved the use of relative ratios (uRRRs) and adjusted relative ratios (aRRs) of the different variables across models (Table 6).
Table 6 Factors associated with enrolment to linkage.
| Characteristics |
%Enrolled (n/N) |
Univariate model |
Bivariate model A |
Bivariate model A |
| uRRRs (95% CI) |
p-value |
aRRRs 95% CI) |
p-value |
aRRRs 95% CI) |
p-value |
| Time lag to enrolment |
| Overall |
22.50(9/40) |
1.11 (1.0-1.2) |
<0.001 |
1.11 (1.0-1.2) |
<0.001 |
|
|
| Gender |
| Female |
7.41(2/27) |
Ref 7.27 (1.5-35.0) |
0.013 |
|
|
Ref 7.47 (1.5-36.1) |
0.012 |
| Male |
53.85(7/13) |
| Hospital facility |
| Mengo Hospital |
26.32(5/19) |
Ref 0.72 (0.2-2.7) |
0.63 |
|
|
|
|
| Mukono HC-IV |
19.05(4/21) |
uRRRs=Relative Risk Ratios, aRRs=Adjusted Relative Risk Ratios
Overall, there is significant relationship between time lag and enrollment as evidenced by the p-value 0.001 less than 0.05. Non-enrolment into care was 22.5% (9/40), but significantly lower in female 7.4% (2/27) compared to males 53.8% (7/13). In the univariate analysis, time lag to enrolment facility and male gender were independently. One hour increase in time lag to arrive at enrolment facility was associated with 11% increased risk of non-enrolment (uRRs=1.11, 95% CI=1.0-1.2). This showed that there is a gap in enrollment, where people don’t immediately enroll. Overall a patient at Mukono health center IV take less time (19.05) hours to enroll compared to Mengo Hospital (26.35) hours at a significance level of p-value <0.001.
Clients’ willingness to enroll for care after testing HIV positive: Most of the counselors (55%) interviewed on whether clients who tested positive were willing to enroll for HIV care indicated that the majority of clients go through a denial phase right after receiving the results that they are HIV positive. They added that the denial phase varies from client to client, further indicating that some stay in denial for a little as a few hours, while others take weeks, months, and even years to come back to the hospital to enroll for care. During interviews, counselor form Mukono health center IV who at the same time an expert client narrated one of the stories that a patient told him, in his own words;
“Most of the clients we test that turn positive first stay in denial and shock even after intensive counseling. One of my patients who tested HIV positive and when I asked her to start drugs in her statements in her own words …….. “musawo” meaning counselor ……I can’t be HIV positive because I have never slept around and I trust my husband, I want to first go to another facility and test so that I confirm if am really positive. Those results are wrong. … She kept on weeping tears in shock. Finally she went out of the clinical room and didn’t enroll. She promised to come back after confirmation”.
These kinds of response from counselors for the unwillingness to enroll immediately after testing positive was similar in both Mukono and Mengo hospital, according to the counselors that responded to the questionnaires, this kind of response continues to be observed among male clients, especially those between 18- 31 years. Other health workers interviewed also acknowledged that clients that test HIV positive but somewhat had an idea that they might be HIV positive find it easy to enroll for HIV care than clients that are shocked at the news of their HIV positive status “.........Counselor my friend told me that you will die faster when I start drugs early at least leave me to first become sick”.
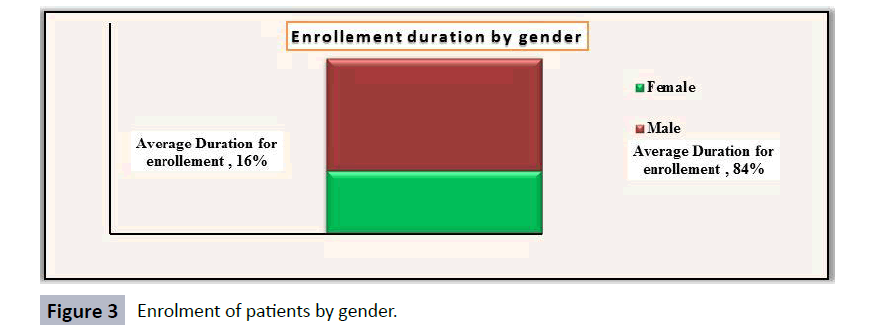
Figure 3 above from both primary and secondary (qualitative and quantitative) data showed that men take longer durations than women. The chart analysis shows enrollment duration by gender, describing the time it takes for a patient to enroll by gender. From the results, it was evident that men (84%) take long to enroll in care compared to female (16%) after initial test. This also showed that there is a correlation between the HIV prevalence by gender and the enrollment. More females are enrolled in care than males since it’s said that men have a low health seeking behavior than women.
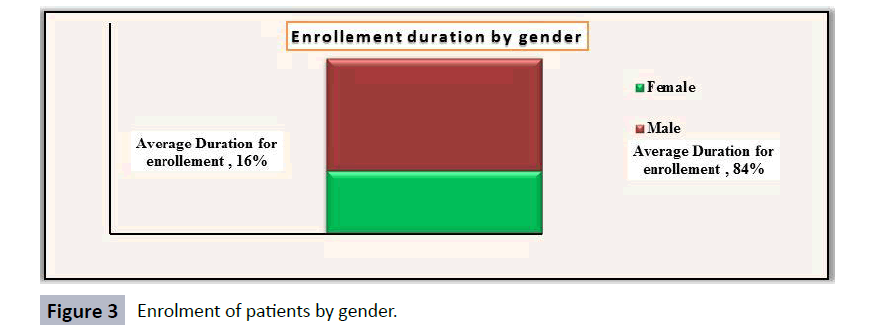
Figure 3: Enrolment of patients by gender.
Interviews conducted with medical doctors on whether clients willingly enroll for HIV care after testing positive. Two of them indicated that, clients after knowing they are HIV positive they do not immediately think about enrolment for care. Doctors indicated, withdraw into a reflective, often regretful mood from which many of them take long to recover. Doctors’ responses also indicated that how soon clients enroll for care after testing HIV positive largely depends on the level of pretest and posttest counseling given to the clients. “…some clients become bitter, remorseful, and even violent sometimes as soon as they know that they are HIV positive” reported one health worker. In their observations, some of the doctors revealed that clients who have just learnt that they are HIV positive are thinking about who might have infected them, also think about how they will accomplish their lives onwards, and some are still in denial about the results.
It should be noted however that a few doctors advised that it is not appropriate for the doctors or counselors to insist on talking to the clients about enrollment for care when they are in state of confusion. Instead, they advise the clients to go home but return as soon as to schedule visits when emotionally stable. This is the time when doctors and nurses constructively engage clients in conversations about enrollment. That withstanding, some of the doctors indicated that there are clients who, after testing HIV positive are willing to discuss and even enroll for care immediately. During the interview, a doctor of Mengo Hospital shared some experience about a scenario that happened in one of the patient’s life that refused to enroll a year before. In his own words he narrated:
“I worked on a couple who was preparing for their wedding and had come to know their HIV status before the wedding. The man turned HIV positive and the woman Negative, the situation first became so intense in the counseling room. The man first accused me for using expired kits since he had tested before and was HIV negative. I asked the man to repeat the test and results came out positive still and wife negative. The man cried, became bitter and remorseful then I advised him to relax outside come back after calming down. He first asked me to lie about his results when they come back for couple group counseling where both are given results as a couple though I refused. When they came back for couple counseling the man insisted they wrong results”.
“They left and went home after a six months period the wife brought back the husband when he was in the later stage with kaposi’s sarcoma. On probing more why they came at a late stage the wife said that she had always encouraged the husband to get linked to but he deliberately refused. He lived in denial. This is evident that men think about enrolling when they are so sick”.
The clients involved in the study were at different stages of access to care. Some of them had just been tested and they had just been informed that they were HIV positive, while others were already enrolled and were accessing care from Mukono and Mengo hospitals. Most of the clients that had just been tested and found out they were HIV positive were reluctant to provide information, indeed, some refused totally. Many of those who responded indicated that they were still not sure of what to do about the news they had just received. Some of them indicated they were willing and already learning more about the available care services. Of the 9 respondents who had just tested positive and engaged, 7 of them were women. All the seven women indicated they were willing to enroll for care but five of them expressed worry about how they were going to break the news of the HIV positive status to their partners, even after some of them acknowledged that their partners must have infected them with HIV.
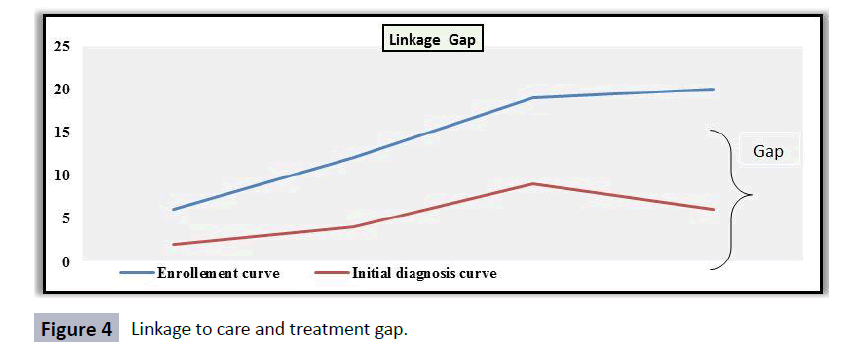
Responses from clients that were already enrolled for care were slightly different from those of clients who had just found out they were HIV positive. Most of the 29 clients who responded to questionnaire and interview questions indicated that their decision to enroll for care was mainly influenced by the post-test counseling they received. Some of them, however, revealed that their decision to enroll was not an instant decision. Indeed, as was indicated by several clients, denial, anger and regret were some of the immediate reactions after knowing that they were HIV positive. In relation, some of the (female) clients revealed that they underwent misunderstandings with their partners after breaking the news to them that they were HIV positive (Figure 4).
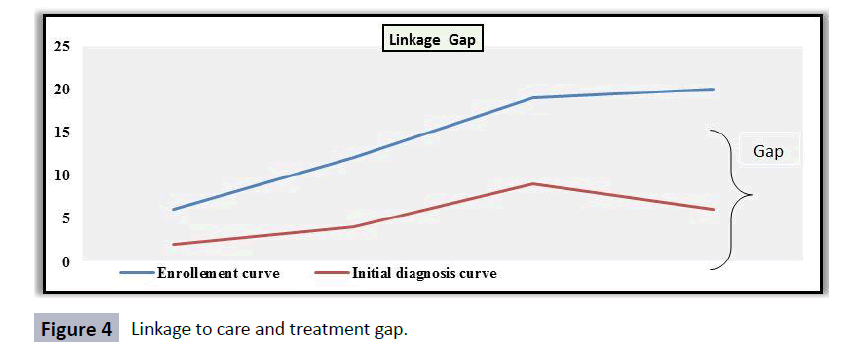
Figure 4: Linkage to care and treatment gap.
The graphs shows the average time lag between the initial diagnosis and enrollment, where we have many newly diagnosed and linked but take averagely (10 months) long time to accept their health status and link for access to health services.
Attitudes of patients while undergoing procedures for enrolment to HIV care: The study sought to examine the attitudes of patients in the process of enrollment to HIV care. In their responses, doctors and counselors acknowledged that at initial testing patients that test HIV positive are usually nervous and when they get the news that they are HIV positive. They usually give them a number of reasons such as spousal rejection, or neglect from their families. There however who request support and consent from their spouses. Some say these drugs are big so they usually never want them.
Majority of the doctors interviewed indicated that there is not a general attitude among HIV patients, adding that patient attitude varies from patient to patient and even within the same patient, the attitude changes depending on prevailing circumstances. Specifically, the doctors revealed that, according to their observation, patients tend to have a negative attitude when they have just enrolled for care but as they start to get used to living positively with HIV, they start to develop a more positive attitude especially a change of lifestyle in the way they take care of their lives.
However, the same doctors also noted that some patients; after progressing well on care suddenly lose interest, and stop showing up for checkups and medication. “Some of the reasons why clients become unresponsive are their frustration that they have to be on care for life. Further, doctors indicated that some clients do not have enough family support to keep them stay committed to access care” reported one of the Doctors interviewed in Mengo Hospital. Indeed, as indicated by some doctors, domestic misunderstandings, financial struggles, violence, among others have been observed as contributory factors towards patients’ withdrawal from HIV care.
Responses from counselors differed from those by doctors. Counselors indicated for the newly diagnosed positives, they usually first cry since they go in shock. “Others don’t react because they are already in care in some other facilities. Most of those ask to be referred to other facilities near to them like for Mengo they prefer Rubaga, Nsambya among others and for Mukono they prefer kojja, mukono church of Uganda facility because its private among others” reported by one of the counselors. When the research assistants probed more about whether they reach, counselors said that the patients never go, instead stay in community re-infecting as they wait to get sick and weak then enroll. The clients who have stayed in touch with their counselors, they have developed strong positive attitude towards access to care. The counselors indicated this is due to the continuous sharing of experiences between counselors and clients. While counselors, as they revealed, endeavor to follow up on some clients, some of the clients deliberately avoid staying in touch. On the overall, however, the counselors indicated that most clients that enrolled for care are still accessing care services.
Responses from HIV Patients on their attitude during the process of enrolling for care were scanty. Most of the HIV Patients interviewed and those who answered questionnaires were caution while talking about their own attitude towards care services. However, some Patients mostly indicated that the toughest period is when they had been told that they have HIV. Their attitude, as they revealed, was negative towards care. Some of them said they enrolled for care but reluctantly. However, after months and years, on care, some of the Patients confessed that they have such positive attitude towards life, and do not see themselves as dying soon as had been the case earlier.
How hospitals deal with Patients that do not complete the procedure for linkage and enrolment, and those that stop coming for care?
Following up from the previous question on the attitudes of clients towards accessing care service, the researcher engaged doctors and nurses about the strategies hospitals have to address unresponsive clients to linkage, enrolment, and care. While each of the hospitals has different approaches to Patients services, they indicated that they follow the national HIV/AIDS care guidelines designed by the ministry of health. Doctors in hospitals indicated that they are still implementing the community outreach program which, among others, follows up on clients at the household level, mechanism called index testing and community linkages.
This methodology uses facility linkage facilitators and expert clients to following up on those lost to follow-up at HCT level, they usually know the community and the people very well. It also involves use of direct home visits using locator forms and phones calls. As was indicated by the doctors, through the community outreach program, the hospitals have been able to bring back some of the clients that had abandoned the care services at the hospitals though others have still refused hence risking more citizens in the community. Further, responses indicated that the outreach program also caters for clients that are interested in the care services but do not feel comfortable to show up at the hospital to access care services. The community outreach has also been used to offer customized care for some clients in terms of hours of services and counseling services based on the realities in the client being attended to.
While the outreach program has been useful for reaching out to clients that have abandoned care services, this has been only possible for such clients that do not leave far away from the localities of the Mukono and Mengo hospitals. Indeed, as was revealed by the doctors and counselors, the community outreach program has become logistically costly for the hospitals to sustain. This leaves many clients unattended by the program. Relatedly, Mukono and Mengo hospitals are addressing the issue of clients that are reluctant to get linked and enrolled for care by shortening the process of linkage and enrollment. From experience, according to doctors, when clients are let to go home and come back another day for linkage and enrollment they seldom come back. Thus, doctors indicated that when someone walks for the testing, the hospitals are ready to immediately link such a person to enroll for care in case they test HIV positive.
Findings on the variance between reported linkages and actual enrollments
Data presented under this objective was both primary and secondary, it was collected mainly from the hospital data bases for HCT (EPI-Info and Excel) and doctors and counselors with interest of finding out whether all clients who test HIV positive and get linked for care are actually enrolled. The findings are presented on three thematic areas including: level of linkages completed over the past three years, and level of enrollment completed over the same period. Data from each of the three hospitals varied. The secondary data was for a period of four years aggregated with the primary data from doctors and counselors; this was availed after authorization from the administrative units of Mukono and Mengo hospital.
Level of linkage in the past three years
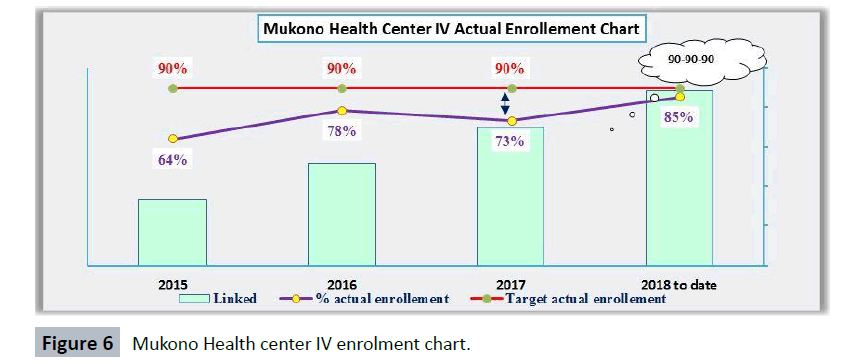
Doctors and counselors in Mengo hospital indicated that, according to hospital records, in the past four years an approximated total of 98,100 people were counseled and tested for HIV. This number includes those tested at the hospital and those tested through the community outreach program. Thus, on average, a total of 97,133 people have been tested annually in the past four years. Of those tested annually approximately 3% were found with HIV, (about 2914 Patients). Those entire tested HIV positive were linked to care immediately. However, of the 2914 clients liked to care, approximately 719 are annually enrolled for care and only 68% averagely for four years. Patients are not recorded to have enrolled for care because they choose to have private care services arranged on a personal level by their preferred care service providers. The secondary data indicated that the number of women testing for HIV, and enrolling for care was overwhelmingly higher than that of men (Figure 5).
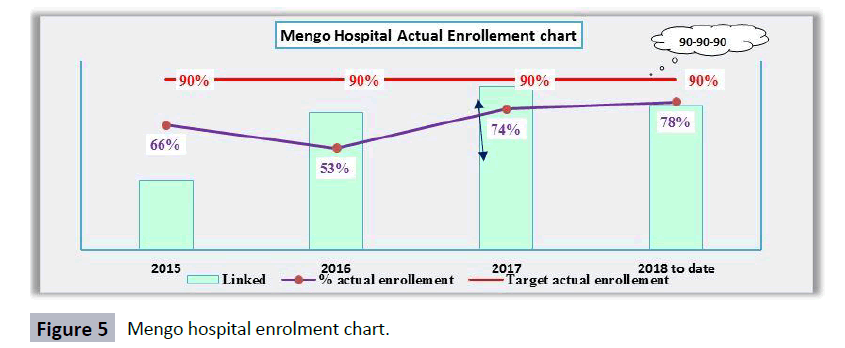
Figure 5: Mengo hospital enrolment chart.
The graph from the secondary data collected from the facility revealed that there is still a big gap in meeting the 90-90-90 Ministry of Health; (MOH) guidelines that aim at enrolling all that are linked in care. At least 90% of those who are positive must know their HIV status and of those 90% must be started on treatment finally 90% of those started should suppress. At least 90% of those tested should be enrolled in care but different in the graph above. In 2018 up to date there is gap of 12% difference between the target 90% and 78%, though progressively the actual enrollment narrowed since 2015 to 2018. This all was evident enough to prove that at not all linked actually enroll.
Doctors and counselors in Mukono hospital indicated that, according to hospital records that were accessible, in the past three years an approximated total of 142,456 people were counseled and tested for HIV at the hospitals and through the community outreach program. Thus, on average, a total of 33,574 people have been tested annually. Data indicated that of the approximated 20,000 tested annually for HIV, about 2% were HIV positive (730 clients). Those entire tested HIV positive were linked to care immediately. However, of the 673 clients liked to care annually, approximately 570 are annually enrolled for care. Clients are not recorded to have enrolled for care because they choose to have private care services arranged on a personal level by their preferred care service providers. The secondary data indicated that the number of women testing for HIV, and enrolling for care was overwhelmingly higher than that of men (Figure 6).
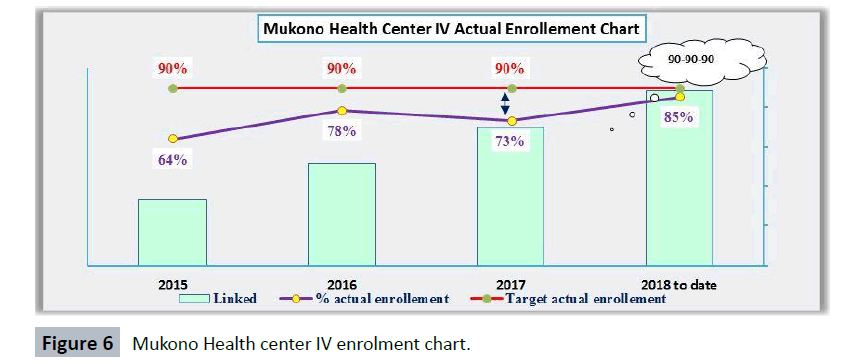
Figure 6: Mukono Health center IV enrolment chart.
Figure 6 from the secondary data collected from the facility it was evident that there is still a small gap in meeting the 90-90-90 MOH guidelines that aim at enrolling all that are linked in care, at least 90% of them must be enrolled in care but from the diagram like in 2018 up to date there is gap of 5% difference between the target 90% and 85%. Though progressively the actual enrollment narrowed since 2015 to 2018. This all was evident enough to prove that at not all linked actually enroll.
Findings on challenges faced during enrolment for care
Data collected in line with this objective was collected from doctors, counselors, and Patients. The doctors and counselors expressed their observations based on their day to day interaction with Patients. Some of the Patients interviewed shared some of the personal experiences that hinder them from enrolling for care services, after they tested HIV positive. Data on this objective was categorized into the following themes: obstacles clients face while accessing care services, obstacles hospitals face while providing care services and strategies hospitals have put in place to deal with the obstacles.
Challenges faced by clients during enrolment for care
Reponses on this theme were mainly collected from Patients who have been tested and linked but are not accessing care services, and those that are already accessing care services. Most of the clients indicated that the lack of family and moral support was one of the challenges they experienced. The commitment to stay on care services, as was indicated by some of the Patients, largely depends on the emotional support they receive from family and friends. Misunderstandings in home, especially between spouses were mentioned as a factor that leads to abandonment of accessing care services by Patients. The inability to afford transport and others small costs involved especially traveling to the hospital, and meeting the small fees charged was another obstacle mentioned. This obstacle was common among respondents (clients) in Mukono hospital. Stigma and the fear to be found out by friends and family was another obstacle mentioned especially by male respondents in both Mukono and Mengo hospitals. Some men revealed that some of the people they used to visit the hospital with to access care stopped because they struggled with stigma and did not want anyone close to them to know they had HIV (Figure 7).

Figure 7: Challenges faced by clients during enrolment for care.
The data revealed that Men have more stigma related issues than females and females have more family related issues and transport issue than Men. Average level of obstacles is with females than males as evidenced by the trend line for females higher than that for males.
Challenges faced by hospitals while enrolling clients for care
Doctors in both hospitals revealed that the biggest challenge they faced was the in-consistence of clients and supplies. The 90-90-90 MOH guidelines advocate for test and start, meaning as you the patient tests positive then you immediately link and start on ARVs but most times they are inadequate to serve the purpose according to doctors. This makes many health workers to go for outreaches and they don’t start the patients immediately this causing gap in linkage. Many clients, according to doctors’ indication, are on and off care services which makes it difficult for proper monitoring. Indeed, some clients disappear completely and when followed up they avoid health workers. This affects timely distribution to clients on care. However, they added that this happens once in a long while. The cost of HIV care services has increased making almost unaffordable for the hospitals, especially in case where financial, material, and technical support from central government is received late, not enough for all the budgeted costs. Research also indicated a gap in the facility linkage where FLFs are support to escort patients to the ART/HIV clinics for enrollment and linkage and it doesn’t happen due to the distance between the testing points and the HIV clinics. This makes clients to run away before enrolling even after being linked. Doctors also indicated issues of waiting time when a patient is newly diagnosed; he doesn’t have to wait for so long. It happens due to the work load especially in government hospitals such as mukono health center IV. Eventually the patients get tired and run away.
Strategies to overcome the challenges
According to the doctors, diversifying sources of funds to support the care services program was the biggest strategy doctors from both hospitals mentioned. They added that the current sources of HIV/AIDS funds (government and PEPFAR) do not meet all cost needs of the counterprograms. Further, responses revealed that the hospitals are now focused more on seeking support in form of materials, equipment, supplies, drugs, and medicines since these are the things that need a lot of money to procure. This is in response to the increasing costs of administering care services by Mukono and Mengo hospitals.
For waiting time, the hospitals are coming up with visible strategies to ensure that the newly tested HIV positives are given priority; this would reduce on the numbers that run away. In addition the linkage gap at the facility, the hospitals also came up with strategies and approaches of facility – facility linkages and community- facility linkages. This involves having a designated FLF to just ensure immediate linkages, attaching targets and monitory benefits to all new positives linked immediately and followed up for those lost.
The doctors indicated that continuous sensitization on the prevention and transmission of HIV/AIDS is prioritized by both hospitals to which is aimed at tackling the obstacle of negative attitude towards care by clients. In addition, the doctors added that intensified and customized counselling services continue to be promoted by both Mukono and Mengo hospitals. It is believed this will improve enrolment numbers.
Discussion of Study Findings
The discussion of study findings is based on findings on each of the three objectives of the study; to assess the linkage time lag between the time of testing and the time of actual enrolment of people that test HIV positive; to assess the reported linkages and actual enrolment; to assess the reasons as to why those linked to don’t enroll. The discussion of findings bases on both secondary and primary data as presented in chapters one, two, and four respectively. The discussion relates primary data to already existing secondary data to identify similarities, differences, contradictions, and gaps based on which conclusions and recommendations are made in chapter five.
Discussion of findings on linkage time lag between the time of testing and the time of actual enrolment of people that test HIV positive [22-26].
Clients’ willingness to enroll for care after testing HIV positive: the finding that most clients who test HIV positive go through a denial phase right after receiving the results that they are HIV positive gives HIV care providers, especially Mukono and Mengo hospitals an aspect they can focus intensive counseling to be able to build trust, confidence, and commitment to care by clients. Whether or not clients embrace enrolment for care largely depends on how effectively their fears/denial is addressed by counselors. Thus, care services should not be seen to start when someone enrolls for treatment but as soon as they enter a health facility to test for HIV.
Previous studies agree with the finding that women are more willing to test and enroll for HIV care than their male counterparts. Just as this study observed that most of the clients enrolled on care on Mukono and Mengo hospitals are women, a report on HIV community outreach by the ministry of health in central Uganda established that women were more willing to test for HIV especially after risky exposure. While high responsiveness by women is a positive sign, without their male counterparts involved the fight against HIV may remain difficult to win. Sadly, as according a WHO Report (2016), despite the global increase in accessibility to ART, people living with HIV, especially men, continue to start treatment late, which increases mortality. This is especially true in developing countries, where the median CD4 count at the point of enrollment is well under 200 cells/micro liter and the 12-month mortality rate for those on ART ranges from 8 percent to 26 percent. Adherence to ART can be challenging because treatment is lifelong [27-29].
Attitudes of clients while undergoing procedures for enrolment for HIV care: The observation by doctors that clients have a negative attitude when they have just enrolled for care but start to develop a more positive attitude especially a change of lifestyle as time passes indicates that care service providers, in this case Mukono and Mengo hospitals’ reactions to clients have to patient and tolerant to avoid compelling clients to lose interest since loss of interest in enrolling and accessing care services were already listed as common occurrences among clients.
The finding by this study that some clients become unresponsive to care services due to frustration that they have to be on care for life is in line with a report by USAID (2017) on uptake of HIV care services in Uganda which showed that, clients’ frustration is real but often is caused by factors outside of the hospital mandate, for instance, low mobility, depression, drug and alcohol use, mental health problems, symptoms and side effects, stigma, and transport costs to the clinic. These external and internal factors are, partly, responsible for the negative towards care, as detailed in chapter four [30].
The inconsistent and late use of care services is a big obstacle to the fight against HIV/AIDS. Indeed, as indicated in a CDC Report (2016), timely treatment of HIV infection has been shown to improve clinical outcomes and reduce medical care costs. Persons who initiate treatment at higher CD4+ levels experience lower morbidity and mortality than those who delay care until substantial immune system damage has occurred. Reducing viral load among persons living with HIV has been proposed as a public health strategy to reduce HIV transmission at the population level, underscoring the importance of timely HIV treatment to reduce the risk of transmission to non-infected partners. For these reasons, reducing delays between HIV diagnosis and initiation of HIV care is viewed as a public health priority [31,32].
How hospitals deal with clients that do not complete the procedure for linkage and enrolment, and those that stop coming for care: it was reported in the findings that each of the hospitals (Mukono and Mengo hospitals) have different approaches to client services but both follow standard HIV/AIDS care guidelines issued by the ministry of health in Uganda. As was indicated by the doctors, through the community outreach program, the hospitals have been able to bring back some of the clients that had abandoned the care services at the hospitals.
The community outreach has also been used to offer customized care for some clients in terms of hours of services and counseling services based on the realities in the client being attended to. The finding that clients are reluctant to enroll for care, or abandon care after enrolling is similar to findings in previous studies. For instance, in line with the indication in chapter two on time between linkage and enrollment, despite the importance of initiating timely HIV treatment and care, as many as 20–40% of HIV positive people in the United States do not initiate care within the first 6 months after their diagnosis. The study adds that 89% of HIV positive people in Massachusetts and Rhode Island delayed care for more than 1 year. Further, 34% of HIV positive people delayed care for more than 1 year following diagnosis and a study using a nationally representative sample found that 17–29% of HIV positive people delayed care for more than 3 months, with a median delay of 1 year [33-35].
Discussion of findings on reported linkages and actual enrolments
Level of linkage in the past three years: The high reported variance those who test HIV positive and those who actually enroll for care services, according to previous reports as detailed in the literature review inn chapter two, is due to personal, internal and external factors. It is complex to improve responsiveness since various stakeholders have to combine effort. For instance, at the individual level, the client (with the help of the caretaker of the client) has to deliberately choose to enroll for care. At the hospital level, strategies have to be enforced that will promote increased responsiveness towards seeking care services among clients that have tested HIV positive.
In line with findings of this study previous studies have also pointed at the complexity of improving access to care services. For instance, a WHO Report on HIVAIDS service provision in Sub Saharan Africa showed that most parts of the world HIV treatment initiatives have focused on increasing access to antiretroviral therapy (ART). The report further indicated that treatment availability alone is insufficient to stop the epidemic. In South Africa, according to the report, only one third of individuals living with HIV are actually on treatment. Treatment refusal has been identified as a phenomenon among people who are asymptomatic, however, factors driving refusal remain poorly understood. Findings suggest that improving engagement in care for people living with HIV in South Africa will require optimizing social integration and connectivity for those who test positive [36,37].
Discussion of findings on obstacles preventing linked clients from enrolling for treatment
Obstacles faced by clients during enrolment for care: the finding that the lack of family and moral support was one of the challenges they clients experienced as an obstacle at the personal level towards access to care services. This, coupled with misunderstandings in homes, especially between spouses was mentioned as a factor that leads to abandonment of accessing care services by clients. These findings are in agreement with findings in earlier studies. For instance, a ministry of health study in Uganda shows that the point of HIV testing is significantly associated with early entry in care and treatment.
Patients diagnosed from points other than a health facility and VCT center have a lower chance of early entry in care, compared to those diagnosed at a VCT center. Relatedly, Reddy (2016) points out that in Tanzania, clients who tested in a community setting were less likely to enter care early than were those who tested at a healthcare facility, adding that clients who were diagnosed at in-patient departments were more likely to enroll in a CTC early than were those diagnosed at out-patient departments or testing facilities. Further, according to Aaron (2015), counseling should stress the importance of early CTC, whether or not the client has a good CD4 count or feels healthy, to allow close monitoring of the client and prophylaxis for opportunistic infections, to avoid a drop in CD4 count and allow timely initiation of medication.
Obstacles faced by hospitals while enrolling clients for care: the finding that most clients are on and off care services which makes it difficult for proper monitoring is more evidence of the need for strengthened community outreach programs. It is through community outreach programs that clients who disappear completely and when followed up they avoid health workers will be reconnected to care services. however, it must be observed that while community outreach programs are essential, this might be difficult to increase to desired levels since it was already reported that both Mukono and Mengo hospitals are experiencing increased costs of HIV care services making almost unaffordable, especially in case where financial, material, and technical support.
Conclusions and Recommendations
The study results show that many Patients, especially men, are not enrolling for care after testing HIV positive. Patients are in denial in the initial stages of knowing they are HIV positive but are already enrolled for care much later. Denial, anger and regret are the immediate reactions after knowing one was HIV positive. In addition, negative attitude towards care among clients is high but varies from individual to individual. The negative there is highest when clients have just tested or enrolled for care but as they start to get used to living positively with HIV. Some clients, after progressing well on care lose interest, even stop medication. Counseling is still a useful component if enrolment for care is to improve. Patients who have stayed in touch with their counselors developed strong positive attitude towards access to care. Most clients that enrolled for care are still accessing care services.
Mukono and Mengo hospitals follow the national HIV/AIDS care guidelines designed by the ministry of health. The customized community outreach care programs that offer care for some Patients in terms of hours of services and counseling services based on the realities in the client have improved responsiveness and adherence to care services among Patients in Mukono and Mengo hospitals. Furthermore, the study results indicate that most of the people that HIV positive go on to enroll for care service. The enrolment, however, does not happen immediately. Most of the clients take weeks, months, even years to enroll for care services. Most of the people who enroll for care services actually stay committed to accessing the services.
The lack of family and moral support has hindered enrolment for care services. Misunderstandings in home, especially between spouses have led to abandonment of accessing care services by clients. The inability to afford transport and others small costs involved especially traveling to the hospital, and meeting the small fees charged are obstacle to access to care services. Stigma is a big obstacle to access to care services. The cost of HIV care services has made it difficult for some to access are services.
Recommendations
As far as reported linkages and actual enrollment of people that test HIV positive is concerned, it is recommended that hospitals in Uganda especially those offering HIV services increase the contact time they have with clients that have tested HIV positive to ensure they enroll for care as sooner than later. They should be given priority and closely followed to ensure complete linkage. More prevention programs like Obulamu must be intensified to reduce stigma. Also ministry of health should roll out index testing to help out in identifying more HIV positives in the community to the index patients. In the process this would complete linkage. The ministry must intensify the male involvement in the HIV testing and treatment. As indicated in the findings that men are the ones who don’t enroll at initial test, intensifying partner notifications and male involvement will help then be involved.
As far as time lag between linkages and actual enrollments is concerned, it is recommended that hospitals and others offering HIV care services increase their manpower to improve client – health worker ration. Also the facility-facility and community facility model should be employed for efficient follow up of all tested positive and doesn’t enroll. In this model, an expert client is used to follow up all those linked but don’t immediately enroll to ensure they enroll. He directly follows a client from the testing point to HIV care and treatment center to be enrolled in care. An expert client follows up directly from one village to another all those tested HIV positive and didn’t enroll. This would effectively complete linkage.
As far as challenges preventing linked clients from enrolling for treatment are concerned, the study recommends that hospital seek more financial and technical support from the government and the international community address the obstacles. Also more adverts to cub the stigma issues and denial.
Acknowledgement
This research was supported by staff in the HIV departments of Mukono Health Centre IV and Mengo hospital. Special appreciation goes to Doctor Edith Namulema Program Manager Mengo Hospital HIV department and Racheal Ankunda Monitoring and Evaluation Officer who provided insight and expertise that greatly assisted the research; Masters Lecturer Nazziwa Florence Uganda Martyr’s University.
We thank the counselors and other health workers for assistance with in obtaining primary data and for their comments that greatly improved the manuscript. We would also like to show our gratitude to the clients for sharing their cases with us during the course of this research.
Declarations
Ethics approval and consent to participate
Consent of respondents was sought from each respondent prior to engagement so that they don’t feel coerced; the researcher had to request for consent from the respective facilities through the research institutions and others through the hospital administrators. An ethical form was signed and presented to every respondent and administrator at the time of interview. Confidentiality is important to facilitate interaction with respondents (Russell, 2011). Thus, all information given by respondents was handled with confidentiality. Respondent anonymity – all addresses and contacts as well as names of respondents remained anonymous during and after the study. We used unique numbers to identify respondents not names. Also, the researcher ensured that all materials used in this research were properly cited and referenced to avoid plagiarism with guidance from the respective hospital research units.
Availability of data and material
The study used secondary data from hospitals and primary data from the field research.
Authors' contributions
IMK contributed to the design and implementation of the research, to the analysis of the results. DSN contributed to the interpretation of results. Both authors contributed to the writing of the manuscript.
24738
References
- Allen S, Tice J, Van de Perre P, Serufilira A, Hudes E (1992) Effect of serotesting with counselling on condom use and seroconversion among HIV discordant couples in Africa, Accra, Ghana. BMJ 304: 1605-1609.
- Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG (2009) Universal voluntary HIV testing and immediate antiretroviral therapy: as a strategy for elimination of HIV transmission: a mathematical model. Lancet 373: 48-57.
- Attia S, Egger M, Muller M, Zwahlen M, Low N (2009) Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS 23: 1397-1404.
- https://nareswari.web.ugm.ac.id/wp-content/uploads/sites/8668/2017/10/Earl_R.Earl_R._Babbie_Babbie_The_Basics_of_SocBookZZ.org_.pdf
- Bennett DE, Myatt M, Bertagnolio S, Sutherland D, Gilks CF (2008) Recommendations for surveillance of transmitted HIV drug resistance in countries scaling up antiretroviral treatment. Antivir Ther 13: 25-36.
- Auvert B, Males S, Puren A, Taljaard D, Carael M (2004) Can highly active antiretroviral therapy reduce the spread of HIV. Pretoria, South Africa. 36: 613-621.
- https://pdfs.semanticscholar.org/73b7/18e508fa943dfb22a9cb5fb17f888239ad0e.pdf
- https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0030124
- Gorard S (2003) Quantitative methods in social science. New York: Continuum.
- Grbich K (2007) Qualitative data analysis: An Introduction. Thousand Oaks, CA: SAGE Publications Limited.
- Sandhya K, Kumar DP (2000) Employee retention by motivation. Ind J Sci Technol 4: 1778-1782.
- Lugada E (2009) Comparison of home and clinic based HIV counseling and testing among household members of persons taking ART: Uganda. Sixteenth Conference on Retroviruses and Opportunistic Infections, Montreal.
- Maxwell JA (2005) Qualitative research design: An interactive approach. (2nd edn.). Thousand Oaks, CA: SAGE Publications Limited.
- Ministry of Health (MOH) (2011) Monitoring and evaluation plan for heath sector strategic and investment plan 2010/11-2014/1.
- Ministry of Health (MOH) (2011) The Integrated National Guidelines on ART, PMTCT and Infant and Young Child Feeding, (1st edn.).
- Ministry of Health (MOH) (2014) Minsterial Directive on Access to Health Services without Discrimination.
- Ministry of Health (MOH) (2016) Rapid Assessment Report of the 2010 HIV Counseling and Testing Policy and Implementation Guideline.
- Mugenda and Mugenda (2002) Research methods quantitative and qualitative approaches. Nairobi. ACTS Press
- Mwinga K, Allen S (2009) Rapid voluntary testing and counseling for HIV. Acceptability and feasibility in Zambian antenatal care clinics. Ann N.Y.
- Neuendorf KA (2002) Content analysis guidebook. London, UK: Sage Publications.
- Neuman WL (2006) Social research methods: Qualitative and quantitative approaches. (6th edn.).
- Nuwaha F (2009) Population-level changes in knowledge of HIV status, stigma, and HIV risk behavior after district-wide door-to-door voluntary counseling and testing: Bushenyi District, Uganda. Sixteenth Conference on Retroviruses and Opportunistic Infections, Montreal.
- https://www.amazon.com/Questionnaire-Research-Practical-Mildred-Patten/dp/1884585329
- Sekaran U (2003) Research Methods for Business;A Skill-Building Approach, 4th ed. Boston: John Willey & Sons. Inc.
- Uganda AIDS Commission (2015) The National HIV and AIDS monitoring and evaluation plan 2015/2016- 2019/2020.
- https://ug.one.un.org/press-releases/press-release-hiv-situation-uganda-february-23-2017
- WHO (2013) Consolidated guidelines on the use of antiretroviral drugs for preventing and treating HIV infection.
- https://www.amazon.co.uk/Science-Research-Published-association-University/dp/0761967982
- Yin RK (2008) Case study research: Design and methods. Applied social research methods. (4th edn.). City ST: Sage Publications.