Keywords
Traumatic brachial plexus; Sensory re-education; Manual dexterity; Functional ADL; Hand sensibility
Introduction
Background
Brachial plexus injury (BPI) is a severe peripheral nerve injury affecting upper extremities, causing functional damage and physical disability (The most common cause of adult BPI is a traffic accident, such as motorcycle accidents. Most patients are young men between 15 and 25 years of age. Other traumatic causes include sports injuries, incised wounds, gunshot wounds, carrying a heavy backpack, and inappropriate operative positioning. Non-traumatic causes consist of tumors, irradiation and congenital abnormalities such as cervical ribs. It has been established that traumatic brachial plexus injuries among adult‘s populations are critical which often produce severe disability and the prognosis is often guarded [1].
An injury affecting the plexus brings about several ranges of injuries. The well-established Sunderland's outstanding arrangement is valuable to comprehend the idea of the damage. The classification emphasises on 3 essential types of nerve damage caused by various external impact factors. Neuropraxia (repairable with onset of recovery within weeks following trauma and surgical correction with a great prognosis), Axonotomesis (compose of few damage and nerve transfer is required in case of poor prognosis), Neuroma in congruity accounting for Sunderland type 3 and 4 and further requires operation, Rupture (Injury affecting the post ganglionic area of the nerve and its classified as sunderland), Avulsion (Injury affecting the pre ganglionic area of the nerve and its classified as sunderland 5). It is well proven that neurapraxia and axonotmesis injuries improves spontaneously with good outcome, whereas neurotmesis injuries require additional surgical intervention and intensive graded rehabilitation program to improve nerve regeneration process [2].
Globally, the exact number of patients with brachial plexus injuries per year is difficult to specify but due to the increase in the participation in extreme sports and the increased number of motor vehicle accidents survivors, there is global increase in the incidence of brachial plexus injuries. There is a significant predilection in male gender and ages between 15 and 25 years old. Traumatic brachial plexus lesions due to traffic accidents account to 70% and mostly due to motor cycles [3].
Mechanisms of injury
Extend/stretch is the most well-known system of damage of the brachial plexus. Most much of the time, these injuries occur due to rapid accelerated motor vehicle mischances that create a sudden shoulder re-directed downwards and in reverse, and neck re-directed the other way as the patient strikes the ground. The caudal traction of the shoulder and arm more often than not harms the upper underlying foundations of the plexus (C5 and C6), lateral traction harms the C7 root and cranial traction harms the lower roots (C8 and T1).
Sensory re-education
Sensory disturbances in the affected limb vary according to the extent of the root involved in Brachial Plexus injury. The outcomes of injury affecting the peripheral nerves are usually bad even with advent of nerve repair. Following nerve injury and recovery, sensorimotor re-education and inclusion of normal movement patterns for cortical remapping is essential. Use of the injured extremity and bimanual tasks will facilitate normal movement patterns in selfcare, recreation, and work [4]. The Sensory Re-education Program is based upon the assumption that, in the patient undergoing regeneration of a peripheral nerve, there will be a time when he will begin to demonstrate less recovery of functional sensation than he is capable of demonstrating. The basis of this under achievement would be the failure of the patient to interpret correctly in his central nervous system the altered profile of impulses discharged when the sensor distribution of his regenerating nerve is stimulated which ideally takes a long time to grow the nerve, approximately 1 mm per day.
Cortical induction
After regeneration the individual fibers do not make contact with their original target area within the somatosensory cortex [5]. As a consequence, the original topographic mapping of the hand is changed and consequently also the meaning of the projections to subsequent areas. This technique is based on the ability of the sensory cortex to expand the representation of a stimulus when presented repeatedly [5,6]. The technique uses the intact topographic mapping as a seed to grow a new topographic mapping for the damaged area. By gradually expanding and differentiating the cortical map, the correctly mapped region will grow while the incorrectly mapped region will shrink until it eventually vanishes. According to Dellon et al. [7] the appropriate time to begin a sensory re-training programme is when the patient can appreciate 30cps of vibration stimulus at some distant level, but moving touch is perceived only at a more proximal level. Alternatively training should commence immediately after the perception of sensation at the level of the fingers [8]. The incidence of injury to the peripheral nerve that supplies the hand is usually associated with disorder affecting mobility, sensation as well as hand functions [9,10]. The sensory re-education programmes that we use today were designed in the 1960s and 70s. They are aimed at an optimal functional capability and capacity of the cortex to function along the continuum of cortical functional reorganizations result [11]. The design and protocols of sensory re-education programmes have not changed in recent decades even with the advancement in Neuroscience and cognitive science. However, only one study has been done on new sensory re-education which was based on Central nervous system (MS) and till date none has been done on peripheral/LMN neuron lesion. This study will determine the effectiveness of a new modified sensory Re-education Protocol on clients with TBP injury.
Materials and Methods
This study employed quantitative quasi experimental design which explains the effect of the modified sensory re-education program through convenience sampling method of patients with Traumatic Brachial plexus injury within 10 to 45 years of age. The sample size is (N=10), Experimental group (n=5), Control group (n=5).
Sample procedure
The study was based on 10 subjects with upper extremity sensory dysfunction, duly assessed with; Tuning fork (Vibration), Semmes-weinstein monofilaments (light-touch and pressure sensation), Nine hole peg (finger discrimination) and all the samples are collected from three hospital set-ups following screening criteria of inclusion and exclusion, Intervention process was explained to the patient and writing consent was signed by the participants before the commencement of the protocol. The inclusion Criteria was aimed at Patients diagnosed with TBPI, Duration more than 1 month, Age 10 through 45 years while exclusion criteria focus on patients with psychiatric disorders, Head injury patients (including problems with cognition), patients with upper motor neuron lesion and patients with other or co-morbid neurological Problems.
Data source
Data for this study were obtained from RIGHT Hospital, SRM Hospital and research institute and Coastal Huts Hospital (Chennai). According to the intervention protocol analysis allows for a detail study of the patients with direct observation of performance in clinical settings.
The current study allowed a small quantity of data to be changed to a form that could be easily analyzed after collation. Experts’ observer bias was as well made possible by reviewing the Michigan Hand Outcome questionnaire.
All Sensory Re-education sessions takes place at RIGHT Hospital, SRM Hospital and research institute and Coastal Huts Hospital (Chennai) in the Department of Occupational Therapy. All ten participants that from both experimental and control group were randomly distributed with four subjects presenting mild sensory impairment affecting C5&C6 dermatome while other six participants with two presenting C5,C6,C7,C8 lesion affecting larger portion of the limb dermatome and the remaining four subject having presented with flail hand without motor or sensory function preservation.
Instrumentation
Semmes-Weinstein monofilaments
Most clinics adopt the use of Semmes-Weinstein monofilaments as a choice for testing sensitivity, mostly because of its characteristic repeatable prompt with a little standard deviation in opposition to others. The filaments are supplied in varying sizes and are each mounted on a handle. The filament is applied to the skin until it bends. The patient is asked to report, with eyes closed, whether the filament is touching the body part. Each monofilament supplies a specific amount of force when it is placed on the test area and gently bent. The monofilaments are available in a large set but most testing can be accomplished using a few filaments. An individual has normal sensation when the 4.17 monofilament (1 g of force) can be felt. An individual has protective sensation intact when the 5.07 filament (10 g of force) can be felt [12].
Nine hole peg
In various neurological disorders, finger dexterity is measured using the 9 hole peg board, the patient is asked to pick out pegs from a box, one after the other then put each of them inside the holes in the pegboard, this should be done with speed. Only the hand assessed is required to perform the test, the other hand is allowed to grip the board at its tip for stability. The numbers of points are rated based on the time used to finish the activity, this is indicated in seconds. Note that the stopwatch or the timer should start at the moment the patient touches the first pegboard until the final peg gets into the box. The items include: flat Board (wooden or plastic) that has nine openings each with 10 mm diameter, 15 mm depth which is placed apart by 32 mm or 50 mm [13] or 50 mm. A container for the pegs: square box (100 100 10 mm) apart from the board or a shallow round dish at the end of the board 9 pegs (7 mm diameter, 32 mm length) [14], (Acute and Chronic Stroke), Excellent test-retest reliability for entire group (ICC=0.85). Adequate test-reliability for individuals with hand spasticity (ICC=0.64). Excellent test-retest reliability for individuals without hand spasticity (ICC=0.86).
Nottingham extended daily life participation
The Nottingham Extended Daily Life activities Scale has used countless times in the clinical profession and also in the researches and rehabilitation of patients who have difficulties in achieving independence in Activities of daily living [14]. Summative subscales and total scores can be calculated from the EADL. For this scale and its four subscales, it has been tested to have a high internal consistency (alpha 0.72-0.94). The test reliability is satisfactory (r(s) 0.81-0.90) with a mean difference in scores on the two occasions of 0.29. The factor analysis has generally supported the subscale structure.
Michigan hand outcomes questionnaire (MHQ)
Michigan Hand Outcomes Questionnaire (MHQ) is a 5-point Likert scale questionnaire comprises of 37 units that measures body function, activity and participation. The total score of MHQ ranges from 0 interpreted as (most sever disability) to 100 explain as (no disability). The MHQ is specially design for the hand under six performance domains: 1) overall hand function, 2) activity of daily living, 3) pain, 4) work performance, 5) aesthetics, and 6) patient satisfaction of hand functioning. It contains a set of questions on bilateral task performance [15]. Factor analysis supported the 6 hypothesized scales. Test-retest reliability utilizing Spearman's correlation exhibited generous understanding, going from 0.81 for the aesthetics scale to 0.97 for the ADL scale.
Demographic characteristics of tools used
Head set, Room freshener, Mirror box, Tactile brush (grade 3), Hand held vibrator (100-300Hz), Texture materials-wool/foam/ Velcro/sand/stone, Shaped objects (circle/square, rectangle), Rubik‘s cube, ADL tools (brush/fork/coins/plastic knife/cotton buds/key and buttons), Ice cube tray and Stop watch.
Data Analysis
Patients with traumatic brachial plexus injury (age 10 to 45 years) were recruited for the study based upon the inclusion and exclusion criteria. The purpose of the study was explained to the subjects. Written consent form obtained from each subject as required. Initially all subjects both control and experimental groups were screened with Semmes Weinstein monofilaments (Hand sensibility), tuning fork (protective sense) and nine hole peg board test (finger dexterity). Overall, the data collection lasted for a period of 12 weeks. Outcome measurements were assessed on two occasions: at the beginning of the study i.e., 1st week (baseline) and at the end of the 12th week using Semmes Weinstein monofilaments, tuning fork, Nine hole peg board, Nottingham Extended activities of daily living (ADL) Scale and Michigan Hand outcome questionnaires (Functional use of hand). The intervention protocol was carried out for 10 weeks beginning from 2nd week to 11th week.
Experimental group
The intervention has two phases (Sensory Desensitization and Tactile localization). Each phase comprise of twelve sessions in which participants are trained based on either desensitization or Tactile localization techniques depending on the duration of sensory impairment and baseline data. Each session lasted for 45 min. In the first phase (Sensory Desensitization), all activities were performed by the therapist over the patient‘s affected area. In the second phase (Tactile localization), different textures, shapes, Rubik cubes, ADL gadgets, thermo exposure, tactile meal and animal assisted therapy as a stimuli were trained over ten treatment sessions followed by post-test evaluation.
Intervention Protocol
Protocol
Week I: Demographical data collected and subjects were screened using.
• Semmes-Weinstein monofilament.
• Tuning fork.
• Nine hole peg test.
Base line measures/Pre-test data were collected using
• Semmes-Weinstein monofilament.
• Tuning fork.
• Nine hole peg test.
• Nottingham Extended ADL Scale
• Application of Michigan Hand Outcome questionnaires (Primary outcome).
Week II to XI (10 interventional sessions): Desensitization and Localization
• Multi-sensory stimulation: Patient was on head set with soft musical beats, mirror for visual feedback mechanism and room/air freshener (olfactory stimulus) to enhance- Multi sensory stimulation.
• Contra-lateral tactile input: Patient applied tactile brush, followed by vibrator of (100-300Hz) for (1-2 min) on the affected hand from proximal to distal using normal hand.
• Bilateral input: Both affected (passively) and unaffected hand (actively) engaged in flexion, extension, circumductory movements of the wrist, supination and pronation of the fore arm and MCP and IP movements of the fingers. The participants simultaneously replicated same actions with both the hands.
• Mirror Illusion: Using the mirror, Participants were encouraged to exhibit various directional hand movements with the unaffected hand there by giving illusion effect to the affected hand.
• C-icing: Slow and gentle swipes on the affected hand with ice pack or ice cube from distal to proximal was applied for 3 times.
• Touch localization: Identifying the familiar objects by touch initially with vision and later with visual occlusion was done.
• Texture manipulation: Various textile materials e.g. (wool, foam, soft and hard Velcro), sand, stone and weight were manipulated for 3 minutes.
• Shapes: Sorting of various shaped objects i.e., circle, triangle, rectangle, and square.
• Manipulation: Manipulation of Rubik cube for 2 minutes
• Manipulation of ADL tools: The participants manipulated and were encouraged to use the ADL tools functionally. The tools include; spoon, fork (blunt end), knife (plastic), cotton buds, keys, coin, button and brush.
• Tactile meals: Peel and open refrigerated orange, pomegranate, onion or garlic.
• Thermo-exposure: Participants immersed the affected hand fully to the wrist level in the beaker filled with warm water followed by cold water.
• Animal assisted therapy: Participants were asked to cuddle, play and pet either cat or dog at home frequently.
Week XII: Collection of post test data (Table 1).
Table 1: Interventional protocol
| S. No |
Desensitization (0-3 months) |
Tactile localization (6-8 months) |
| 1 |
Multi-sensory stimulation (30 minutes) |
Textures |
| |
-Addresses several senses |
Soft, hard, foam, sand, stone, wool, weight |
| |
-Larger parts of brain activated |
| |
Treatment |
Shapes |
| |
-Auditory head set |
Circle, Square, Rectangle, Triangle (2 minutes) |
| |
-Mirror/room |
| |
-Room air freshener |
| 2 |
Bilateral input (motor activities) |
Rubiks cube (Dexterity) (5 minutes) |
| |
-Weight bearing |
| 3 |
Illusions with mirror imagery of the unaffected hand (15 minutes) to enhance cortical mapping |
Objects/ADL Tools |
| |
-Mirror visual feedback (MVF) |
-Spoon, fork, brush, button, toothpick, cotton buds, key, coins (NEW) |
| 4 |
Contralateral input |
Thermo exposure (hand immersed in cold water) |
| |
-Texture, tactile brush |
| |
-Diwel texture |
C-icing (quick dermatome swipe of the cube 3 times) |
| |
-Immersion texture |
| |
-Vibration level, 1-2 min |
| 5 |
|
Tactile meal |
| |
|
-Orange peeling, permanganate in refrigerator (5 min) |
| |
|
Animal assisted therapy |
| |
|
Dogs or cats |
Data Analysis
The data were analyzed by using the Statistical Package for the Social Science (SPSS 22 version). In order to answer research questions, mean, standard deviation and paired t-test and independent t-test were used.
Statistical methods
Inferential statistical analysis was conducted in this present study. Results on continuous measurements are presented on Mean, SD (Min-Max) and results on categorical measurements are presented in Number (%), Dependent variables are normally distributed, Comparative statistical analyses (Mean, range and SD) conducted to find out the baseline characteristics (like age and duration of illness) of the samples, and Graphical representations have been constructed for describing visually the participant‘s demographic characteristics.
Significance is assessed at P value <0.05 level. Significant figures: +Suggestive significance (P-value: 0.05
Ethical clearance: Ethical clearance was obtained from Institutional ethics committee of SRM Medical college Hospital and Research Centre.
Ethical clearance number: 1200/IEC/2017.
Results
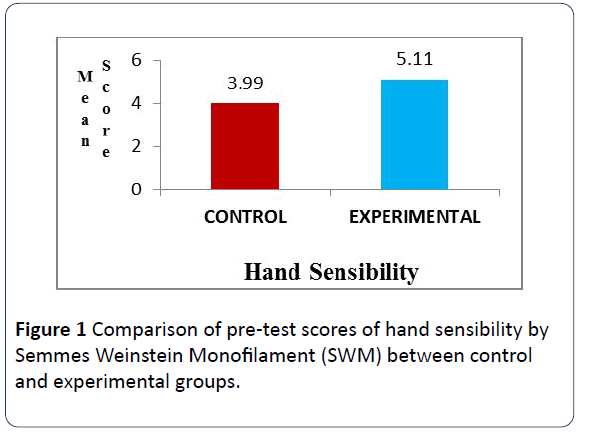
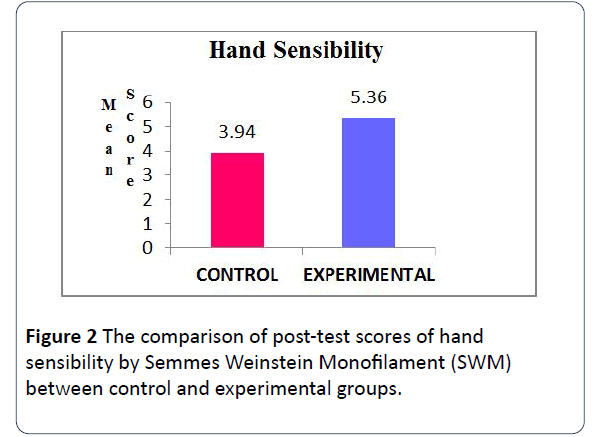
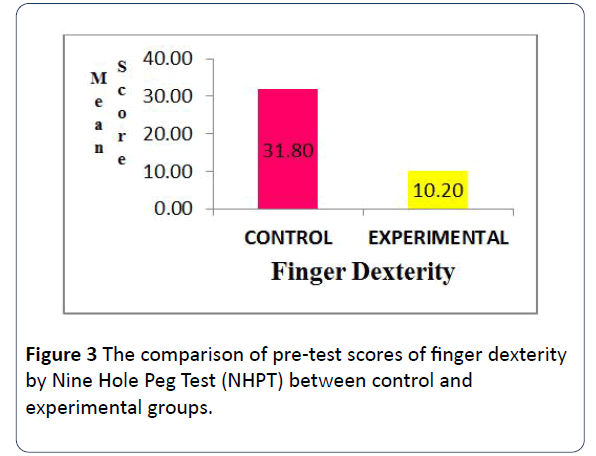
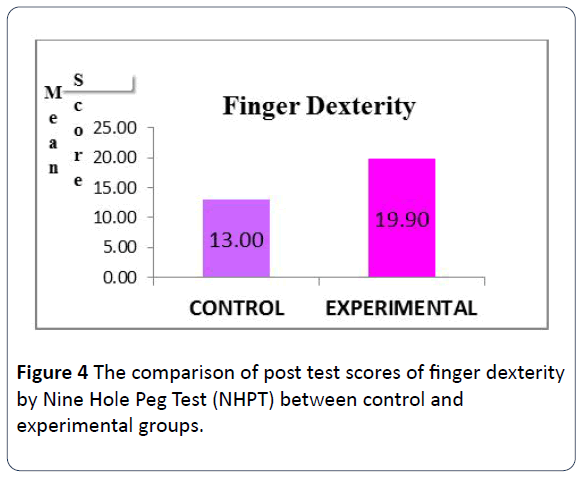
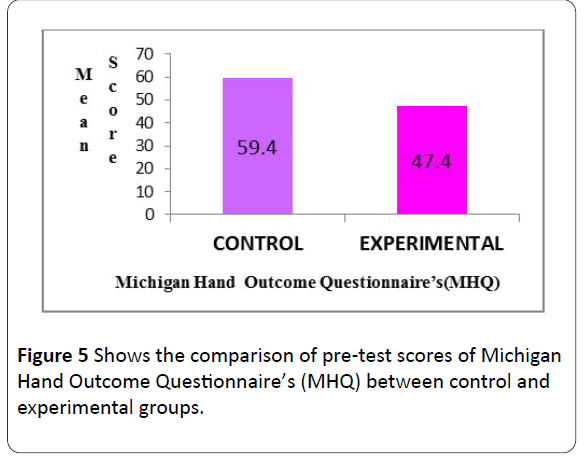
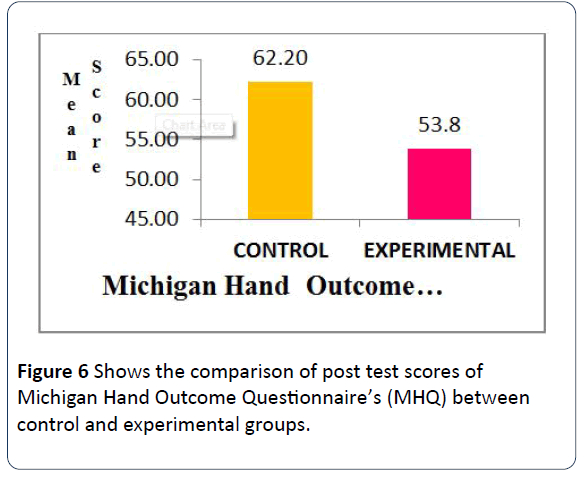
The findings of this study show the comparison of pre-test scores of Michigan Hand Outcome Questionnaire’s (MHQ) between control and experimental groups using independent ttest. The p-value of 0.000 is significant at one per cent level indicating that there is significant difference in mean scores of Michigan Hand Outcome Questionnaire’s (MHQ) between control and experimental groups in pre-test. Also, comparison of post test scores of Michigan Hand Outcome Questionnaire‘s (MHQ) between control and experimental groups using independent t-test. p-value of 0.000 is significant at one per cent level indicating that there is significant difference in mean scores of Michigan Hand Outcome Questionnaire‘s (MHQ) between control and experimental groups in post-test. Hence, the Michigan Hand Outcome Questionnaire‘s (MHQ) is different between control and experimental groups in post-test (Figures 1-6).
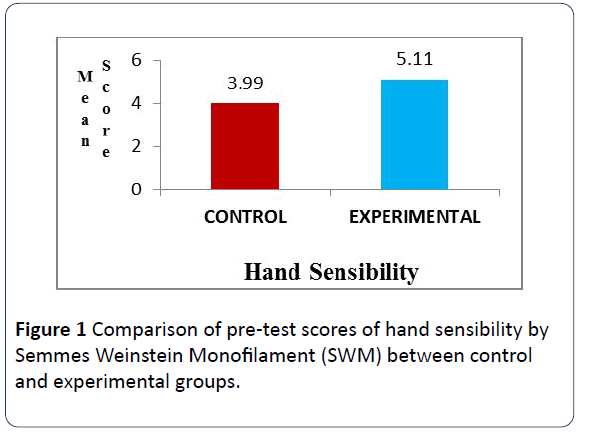
Figure 1: Comparison of pre-test scores of hand sensibility by Semmes Weinstein Monofilament (SWM) between control and experimental groups.
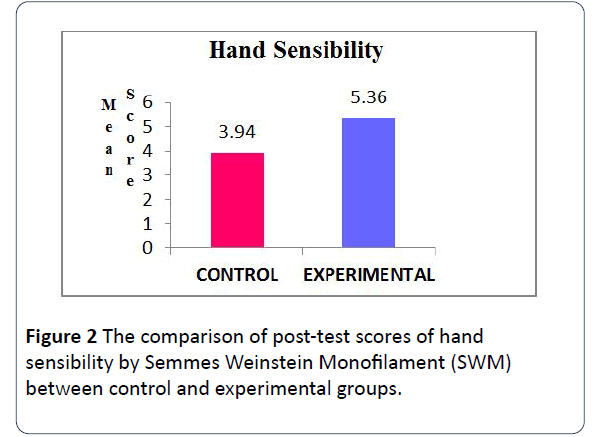
Figure 2: The comparison of post-test scores of hand sensibility by Semmes Weinstein Monofilament (SWM) between control and experimental groups.
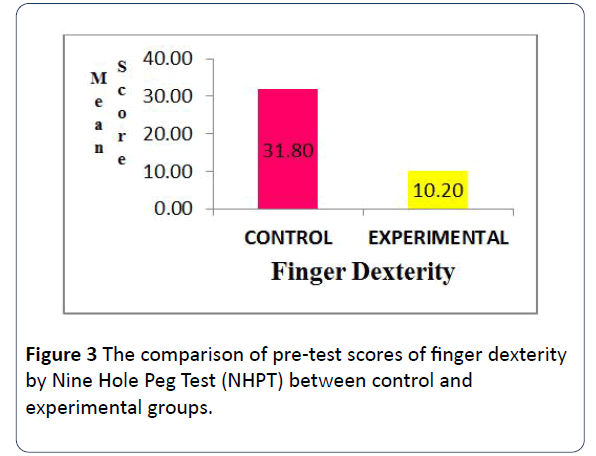
Figure 3: The comparison of pre-test scores of finger dexterity by Nine Hole Peg Test (NHPT) between control and experimental groups.
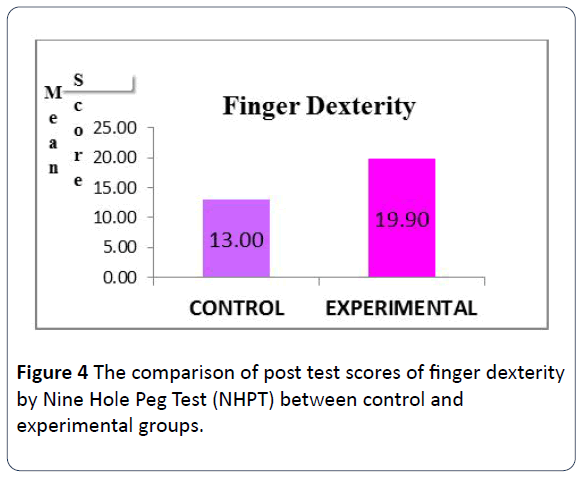
Figure 4: The comparison of post test scores of finger dexterity by Nine Hole Peg Test (NHPT) between control and experimental groups.
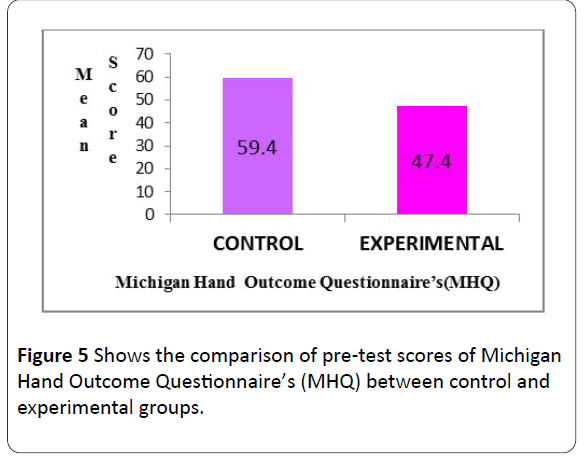
Figure 5: Shows the comparison of pre-test scores of Michigan Hand Outcome Questionnaire’s (MHQ) between control and experimental groups.
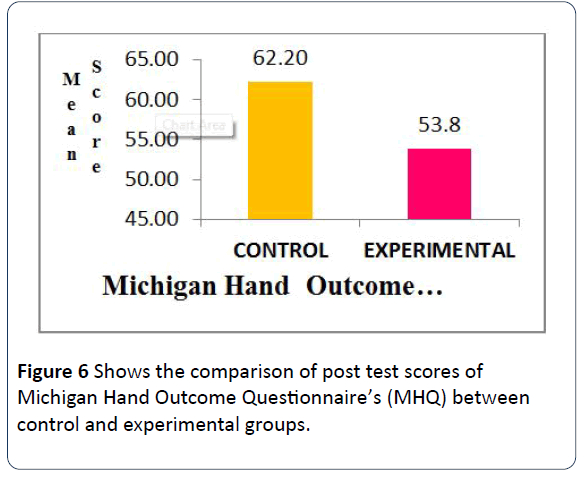
Figure 6: Shows the comparison of post test scores of Michigan Hand Outcome Questionnaire’s (MHQ) between control and experimental groups.
Discussion
This study detailed a pilot, intensive sensory re-education training program and associated outcome measures, emphasizing hand sensibility, manual dexterity, and functional use of hand. This study was based on previous literature emphasizing the need for modification in sensory re-education protocol due to insufficient evidence as to “active” approaches to sensory rehabilitation for retraining the upper limb. The sensory re-education intervention protocol used in this study applied “active-cognitive” approaches which enhance sensory neural pathways recruitment and completion of re-education activities that largely rely on cognitive and perceptual abilities of the participants.
During intervention, the participants in experimental group actively engaged and were able to participate at relatively similar levels, as indicated by duration on task, despite differences in hand functions. Activities were easily adapted to meet the functional level of each individual and progressed to challenge emerging skills through neural reorganization of the sensory cortex. This is further illustrated by the activity level of the participants during desensitization and or tactile localization period.
The results of the study supported our main hypothesis that Adults with TBPI would improve on functional use of hand using MHQ through modified sensory re-education protocol compared to the control group. The activities were function-based and monitored with adequate clinical guidance by the Occupational therapist (researcher) at different levels through repeated practice and encouragement. The modified sensory Reeducation program has led one of the participants to return to his work (TVS Service center, Chennai Central) and active bike riding with near normal engagement in task and functional participation. In addition, two other participants regained functional hand use with minimal assistance to maintain a firm grip and better control on ADL incorporated activities such as (eating with spoon, bilateral hand use with plastic knife, attempt to buttoning shirt etc.).
The intervention protocol stressed on Nottingham Extended ADL Scale to evaluate functional activities of daily living participation among the participants. Review of the results and observation regarding their application yielded several key ideas. The NEADL scale is easy to complete and allows sufficient and varied practice in terms of daily engaging task. The result has shown no statistical significant difference in NEADL scores between the groups. Although, the findings seem disappointing but a notable appreciating fact was established between the pre and post-test analysis of NEADL in experimental group with p<0.05. Motivation i.e., Intrinsic motivation coupled with external cue (tools) influenced participants performance during intervention which enabled immediate feedback and mediated to success in ADL. This present study out-come can be delineated to previous study conducted by Carey et al. [16] on Effectiveness of Neuro-rehabilitation on Sensation. The authors conducted a randomized parallel-group controlled trial, with blinding of subjects, clinical assessors, and data analysts. Fifty subjects with impaired texture discrimination, limb position sense, and/or tactile object recognition (>6 weeks, median 48 weeks post-stroke) were randomized to receive somato-sensory discrimination training (n=25) or repeated exposure to sensory stimuli (n=25) in 60-minute sessions for a total of 10 hours.
The primary outcome was change in a composite standardized somato-sensory deficit (SSD) index following intervention. The intervention, follow-up was at 6 weeks and 6 months posttraining respectively. Between-group comparisons revealed a significantly greater improvement in sensory capacity following sensory discrimination training; Improvements were maintained at 6 weeks and 6 months. Sensory discrimination training can achieve significant improvements in functional sensory discrimination capacity after stroke. The conclusion of their clinically oriented training achieved transfer of training effects to novel stimuli.
The overall outcome of the NEADL between the groups could be traced to the inconsistence in participant participation during the study period. This may be due to the psychological influence of the injury and post-operative motor and sensory return which has no significant improvement over a period of eight months with classical sensory-motor training. Thereby, the subjects were already losing interest in the use of their hand and only craving for magic effect within a short moment. These findings are supporting the previous literature by Terri et al. [17] in rehabilitation of the hand and upper extremity, 2-volume with analysis based on environmental influence on sensory reeducation. It was emphasized that several factors may influence the results from the sensory re-educational programs in a positive or negative way. For instance, active and conscious use of the hand in daily activities as well as attention during training combined with high motivation by the patient is extremely important. An enriched environment is fundamental to facilitate learning. It has been demonstrated that passive unattended and repetitive tasks lead to negative changes of the associated territories in the sensory cortex. These observations have been discussed especially as a genesis model for dystonia and repetitive strain injury problems.
It was revealing that with regard to both hand sensibility using SWM and Hand dexterity using NHPT, no significant difference was noted. But with hand dexterity there was a minimal noticeable improvement in two out of five participants in experimental group. The duration of task completion has improved with adequate grip on NHPT during the post-test study as compared to pre-test performance level. Furthermore, the two subjects are presented with mild sensory impairment affecting C5 and C6 dermatome with preservation of protective sensation, which can arguably be the reason behind the clinical difference noted. this can be distinguished from result obtain from other remaining three participants with one presented with C5,C6,C7,C8 lesion affecting larger portion of the limb dermatome and the remaining two subject having presented with a flail hand without motor or sensory function preservation. This denotes that sensory re-education is super imposed on motor function. This is in accordance with a research conducted by Bo-He et al. [18] to investigate the factors associated with sensory and motor recovery after the repair of upper limb peripheral nerve injuries. This includes: age, gender, repair time, repair materials, nerve injured, defect length, and duration of follow-up and return of motor components.
Lastly, in experimental group participants without remarkable sensory recovery after training as justified by Semmes Weinstein monofilament were able to appreciate protective sense of vibration on larger joints as well as the MCP without no effect on the IP joints. Also, participants were able to discriminate temperature differences with hot and cold water. This can be supported with the use of vibrio-tactile signals as reflected in a study conducted by Birgitta et al. [19,20] on recovery of functional sensibility after nerve transection and repair. They emphasized on timing specifics to activities through vibratory effect as a substitute to an alternate feed-back which hypothetically helps to maintain or re-establish the cortical hand mapping in the brain following deficit. The presence of nonadhesive scar formation in the anterior media aspect of the arm in one of the participant was cause for concern initially and this is the only raised issue regarding aesthetic appearance as other participants limb were well preserved during surgical procedure.
Furthermore, irrespective of the nerve involvement, the enthusiasm for functional return was observed in all the participants. This made them to actively engage in tasks beyond just object rudimentary touching as its practiced traditional wise. It has been established in the previous literature by Alon et al. [21] on effects of a new home-based sensory re-education training tool on hand sensibility and manual dexterity in people with Multiple Sclerosis concluded that sensory abilities would be achieved when cognition challenge and perception are integrated during intervention and the sensory re-education training activities can be frustrating and worrisome in participants with cognitive declining [22].
The need for cognitive perceptual integration in traumatic brachial plexus injured patients is to bridge the barrier and link the upper motor neuron with lower motor neuron which in-turn is speculated to aid cortical mapping through neuro and cortical plasticity. However, the outcome of this dissertation can be supported with a study conducted by Heremans et al. [23] on thirty Multiple sclerosis patients. The result shows significant correlations between imagery abilities, cognitive functioning and motor performance of the hand. Further, neuronal plasticity and interconnection of brain networks on people with MS and the result shows adequate evidence based relationship between cognitive function, motor function, and cortical activation.
Implications
Clinical
• This study is in accordance with other literature findings was able to determine the effect of modified sensory reeducation protocol based on advancement in cognitive neuroscience.
• One of the most clinical relevant findings of this study was that middle age group with TBPI were able to achieve significant gains with intensive period of sensory reeducation program over a short duration of time. Furthermore, activities that incorporate into daily function are more beneficial, hence should be encouraged early.
• The use of functional attainment scale (MHQ) as an outcome measure should also be of interest to rehabilitation experts and the scope of this can be easily incorporated into regular clinical practice of sensory re-education.
Conclusion
Sensory re-education protocol not necessarily impacts the level of sensation damage in the hand but might also result to a positive result in functional ADL activities. Present findings were supported by Debora et al. [22] that extreme functional improvement in the management and rehabilitation of traumatic brachial plexus injury. This is due to the development of ingenious reconstructive techniques and electro-diagnostic testing methods etc. that guide the surgical procedure following TBPI repair. Also, the dramatic improvement shown by few of the patients in recent days after rehabilitation through sensory re-education process can be traced to the advancement in the knowledge of neuro-cognitive development. Early surgical corrective measure along with rehabilitation service is highly essential to preserve functional integrity of the hand and upper extremity with specific focus on activities of varied daily routine tasks.
Limitation
There were a number of study limitations which have been described in summary below:
The study was biased as the samples were selected through convenience sampling.
• The lasting effects of the functional gains could not be assessed due to shorter duration of study.
• Homogeneity in the age of respondents between control and experimental groups was not maintained but with regard to duration of illness homogeneity was maintained.
• Language and communication barrier. This is due to the fact that the researcher relied lengthily on Tamil voice transliterated scale for local participants that do not understand English and intervention was co-guided by Tamil and English fluent attendant/therapist/Nurse present at the study centres for proper guidance.
Suggestions for Future Researcher
In future study, the following are recommended. This study can be done in larger population for more accurate result, Gender wise distribution of patient selection, Duration of intervention can be increased in future research to elicit progress, Home or community program can be provided to reinforce learning that occurs in the clinical setting, Future researchers may focus on only ADL based activities for functional motor return, The MHQ seems to differentiate function as effective as possible. It is necessary to observe patients on a long term study importantly following the return of tactile sensation at the finger tips and The effects of previously modified sensory re-education protocols based on neurocognitive advancement can be compared with this study which can, in turn, contribute to clinical research and enhance evidence-based practice.
Acknowledgement
To the Glory of Almighty God, for he has never failed me. I would like to express my deepest gratitude to the co-author, contributors, adviser and guidance of this dissertation. A special thanks to Mrs Silpa Immanuel Voola for her immeasurable effort, Dr. U.Ganapathy Sankar and Ibraheem Arada of The ARADA Logistics Services Limited, for their assistance in making this paper a success.
24353
References
- Nagano A (1998) Treatment of brachial plexus injury. J Orthop Sci 3: 71-80.
- Grinsell D, Keating CP (2014) Peripheral nerve reconstruction after injury: A review of clinical and experimental therapies. BioMed Research Int 2014: 1-13.
- Narakas AO (2013) The treatment of brachial plexus injuries. Int Orthop 9: 29-36.
- Novak CB, von der Heyde RL (2015) Rehabilitation of the upper extremity following nerve and tendon reconstruction: when and how. Semin Plast Surg 29: 73-80.
- Merzenich MM, Kaas JH, Wall J, Nelson RJ, Sur M, et al. (1983) Topographic reorganization of somatosensory cortical areas 3b and 1 in adult monkeys following restricted de-afferentation. Neuroscience 8: 33-55.
- Jenkins WM, Merzenich M, Ochs MT, Allard T, Guic-Robles E (1990) Functional reorganization of primary somatosensory cortex in adult owl monkeys after behaviorally controlled tactile stimulation. J Neurophysiol 63: 82-104.
- Dellon AL, Curtis RM, Edgerton M (1974) Re-education of sensation in the hand after nerve injury and repair. Plast Reconstr Surg 53: 297-300.
- Parry CB, Salter M (1976) Sensory re-education after median nerve lesions. J Hand 3: 250-257.
- Jaquet JB, Luijsterburg AJ, Kalmijn S, Kuypers PD, Hofman A, et al. (2001) Median, ulnar, and combined median-ulnar nerve injuries: functional outcome and return to productivity. J Trauma 4: 687-692.
- Jaquet JB, Luijsterburg AJ, Kalmijn S, Kuypers PD, Hofman A, et al. (2001) Median, ulnar, and combined median-ulnar nerve injuries: functional outcome and return to productivity. J Trauma 51: 687-692.
- Bell-Krotoski JA, Fess E, Figarola JH, Hiltz D (1995) Threshold detection and Semmes-Weinstein monofilaments. J Hand Ther 8: 155-162.
- Mathiowetz V, Volland G, Kashman N, Weber K (1985) Adult norms for the Box and Block Test of manual dexterity. Am J Occupational Ther 39: 386-391.
- Mathiowetz V, Volland G, Kashman N, Weber K (1985) Adult norms for the Box and Block Test of manual dexterity. Am J Occupational Ther 39: 386-391.
- Das NR, Moreton BJ, Lincoln NB (2011) Rasch analysis of the Nottingham extended activities of daily living scale. J Rehabilitation Med 43: 944-950.
- Melissa JS, Kevin CC (2013) The Michigan Hand Outcomes Questionnaire (MHQ) after 15 years of field trial. Plast Reconstr Surg 131: 779-787.
- Carey L, Macdonell R, Matyas TA (2011) SENSe: Study of the Effectiveness of neuro-rehabilitation on sensation: a randomized controlled trial. Neurorehabilitation Neural Repair 25: 304-313.
- Terri MS, Lee OA, Jane F, Peter CA (2011) Rehabilitation of the Hand and Upper Extremity: Best practices in the rehabilitation of hand, wrist, elbow, arm and shoulder problems. Elsevier pp: 235-36.
- Bo Hi, Zhaowei Z, Qingtang Z, Xiang Z, Canbin Z, et al. (2014) Factors predicting sensory and motor recovery after the repair of upper limb peripheral nerve injuries. Neural Regen Res 9: 661-672.
- Birgitta R, Lundborg G (2004) Sensory re-education after nerve repair: aspects of timing. Handchir Mikrochir Plast Chir 36: 8-12.
- Kesselring J (2013) Neuro rehabilitation in multiple sclerosis-resilience in practice. Neuro Rehabilitation pp: 31-36.
- Heremans E, Nieuwboer A, Spildooren J, De Bondt S, D'hooge AM, et al. (2012) Cued motor imagery in patients with multiple sclerosis. Neuroscience 206: 115-121.
- Debora G, Elisabetta B, Roberto G, Stefano F (2013) Brachial plexus injuries in adults: management and repair strategies in our experience. Results from the Analysis of 428 Supraclavicular Palsies. J Neurol Neurophysiol 5: 1-8.
- Heremans E, Nieuwboer A, Spildooren J, De Bondt S, D'hooge AM, et al. (2012) Cued motor imagery in patients with multiple sclerosis. Neuroscience 206: 115-121.