Keywords
Community acquired pneumonia; Distribution; Determinants; Burden; Prevention; Control; Strategy
Introduction
Pneumonia has been known as a common and potentially death causing condition for nearly two hundred years. The disease affects the respiratory system, mainly the lungs. It is recognized by a collection of symptoms and signs together with at least one opacity on chest radiograph. Pneumonia can be widely classified as community-acquired pneumonia(CAP) and hospital acquired pneumonia. CAP can be defined as an acute infection that harms the lower respiratory tract, which occurs in patients outside health facility or develops within the first two days after admission to health facility. It is a widely prevalent medical condition globally and shares a significant consumption of healthcare resources in both developed and developing countries [1-3].
More than 100 microbial causes of CAP are identified of which bacteria, fungi, viruses, and parasites are the main. The five commonest microbes are Streptococcus pneumoniae, Mycoplasma pneumoniae, Chlamydia pneumoniae, Haemophilus influenzae, and influenza viruses. Streptococcus pneumonia, Haemophilus influenza and Pseudomonas aurugnosa are the most frequent causes worldwide as well as in Ethiopia [4,5].
The infection remains a major reason for hospital admission and a common death cause in the world. Admitted patients remained the main source of the most epidemiological data. Results of population based studies indicated that the annual incidence rate of CAP in adults in developed countries ranges from 2.6 to 13.4 per 1,000 inhabitants, with a bit higher figures among males and the elders. Admission rates ranging from 22% to 51% have been reported with annual mortality rates between 0.1 and 0.7 per 1,000 inhabitants [6].
The 2010 World Health Organization survey revealed that lower respiratory tract infections, mainly CAP, caused 429.2 million episodes of illness globally and were the top causes of disease burden measured in terms of disability-adjusted life years (DALYs) among all age groups, accounting for 94.5 million DALYs. In sub- Saharan Africa this infection ranks consistently high as a cause of admission in hospital based series [7].
Youngsters and elders are at the highest risk of both Hospital acquired and CAP. An estimated 2 million children below five years of age die from pneumonia every year, accounting for approximately 1 in 5 child deaths globally. Even though mortality from childhood CAP has decreased in the last few decades in developed countries, the disease continued to be a common cause of morbidity and hospitalization [7,8]. Low birth weight, malnutrition, indoor air pollution, non-exclusive breastfeeding, parental smoking, crowding, zinc deficiency, mother’s experience as a caregiver, mother’s age, lack of education in the mother, poor socio-economic status, humid conditions, vitamin A deficiency, birth order, high altitude and outdoor air pollution were found as possible risk factors of pneumonia among children in developing countries [1,7]. In Ethiopia, CAP is among the main causes of hospital visit and death, especially in children younger than five and the implication of this infection on health and economy of the country is concerning [4,9,10]. Therefore, it was found relevant to conduct a review on CAP with due emphasis to the epidemiologic aspects (distribution, determinants, burden and available prevention and control strategies) so as to contribute much in control and prevention of this infection. The result of this review may also serve as a reference for future studies on this disease.
Methods
A systematic review of available literatures on epidemiology of CAP was carried out. Three search engines: Google, Google scholar and Pub Med were used to access relevant materials online. The search terms used were “Community acquired pneumonia”, “Epidemiology of community acquired pneumonia in Ethiopia“, “Community acquired pneumonia and its prevalence in Ethiopia”, “determinants of community acquired pneumonia”, “outcome of community acquired pneumonia” and “prevention and control strategies of community acquired pneumonia”. A total of 47 research articles, reports and other documents published since 2000 were identified. Of these 34 articles and 5 reports were used in the review and the rest were excluded because of irrelevance to the review.
Results
Thirty nine papers in total were identified for inclusion in the review of which 34 were journal literatures and 5 were national and international report documents on CAP. The articles and reports revealed the following information.
Distribution (frequency and pattern) of community acquired pneumonia
In Ethiopia, pneumonia is one of the leading causes of hospital admissions and mortality. In a study done in Addis Ababa, CAP was identified to be the leading cause of respiratory diseases and the 2nd most common cause of adult medical admissions [4]. It was reported to be one of the common causes of under-five mortality and hospital admissions. Children below 3 years experience 7.9 incidents of respiratory illness per year; children from 3–5 years experience 6.6 episodes in Ethiopia [11,12]. Some 51.1% of the 963 pediatric admissions to Chiro Hospital had respiratory infections; of these 19.2% had CAP [13] and approximately 14.2% of acute respiratory infection cases collected from the Butajira Rural Health Project were acute lower respiratory infections (CAP as a major), most common in children from 1–6 months of age [14]. Two studies from different areas of North west Ethiopia indicated the prevalence of CAP in below fives to be 16.1% and 20.6% while it was 21% in a studies conducted in Southern Ethiopia [15-17]. Data from different regions in Ethiopia also showed different results (Table 1).
| Investigator |
Type of study |
Sample size |
Prevalence of CAP among the sick children by region |
| SNNP |
Amhara |
Tigray |
| JSI Research & Training Institute(2013) |
iCCM survey of health posts and house holds |
780 children with acute respiratory infection 260 (80.8%), 390(68.2%) and 130 (56.9%) from SNNP, Amhara and Tigray respectively |
280
(80.3%) |
264
(63.3%) |
73
(17.8%) |
Table 1 Prevalence of CAP among under five children in three regions of Ethiopia, December, 2012.
Among 77 HIV-positive children admitted to Ethio-Swedish Children’s Hospital between January 1990 and April 2000, CAP was found in 27 (35.1%). Eight percent of patients diagnosed with CAP in a hospital in Addis Ababa were HIV-positive, compared with 2.4% for HIV free patients. The prevalence of this infection is set to rise with increasing incidence of HIV [18,19].
Determinants of community acquired pneumonia
In Ethiopia and other developing countries, malnutrition, low socio-economic status, indoor air pollution, low birth weight, viral infections, low immunization coverage, overcrowding and poor ventilation, humid conditions, zinc and calcium deficiency, smoking, vitamin A and D deficiency, high altitude, and outdoor air pollution were the identified risk factors for CAP and other respiratory infections in populations of different age group [10,20,21].
HIV/AIDS, Charcoal use for cooking, cooking within the main house, type of roof of the main house, keeping cattle in the main house and household crowding status were found as important determinants for the development of CAP in a study conducted in north west Ethiopia. Another study stated that the risk of developing CAP among children below 5 who are stunted and who lived in thatch roofed house was 2.5 times higher compared to children who lived in corrugated iron roofed house and Children from severely crowded houses were 4 times more likely to develop CAP compared to children from under-crowded houses [15,17]. Rural dwellers are more susceptible to CAP due to poorer sanitation, lack of electricity, and low literacy rate [14].
In Ethiopia and other developing countries bacteria are the major causes of respiratory infections including CAP even though the infections are sometimes caused by viruses and fungi. The leading causes of bacterial pneumonia are: Streptococcus pneumonia, Haemophilus influenza, Streptococcus pyogenes and Staphylococcus aureus. A study from Black Lion Hospital and Arbaminch Hospital on adult patients with CAP indicated that Streptococcus pneumoniae and Staphylococcus aureus were the most common pathogens followed by Pseudomonas aeruginosa, and Klebsiella pneumonie [22,23]. Mixed bacterial isolates were also identified in some patients in the study done in Arbaminch Hospital [22]. Streptococcus pneumoniae and Haemophilus influenza (type b) were identified as the commonest causative agent in children diagnosed with CAP in another studies conducted in Addis Ababa and Gondar [10,24].
Burden of community acquired pneumonia
Studies done in different places in Ethiopia indicated that pneumonia is a major cause of mortality and morbidity among children below five and the geriatrics. Of 15 countries that have the biggest death rate from clinical pneumonia in children below 5, Ethiopia ranks 4th globally (84.6 deaths per 10,000 under five population) and one major cause of this mortality is CAP [9,25,26]. A study conducted in a health center in Southern Ethiopia indicated that from the total cases admitted with CAP, 18.79% deaths occurred. Similar study from a specialized hospital in Southwest Ethiopia showed that from the total patients admitted with CAP, there was a 20.2% death case. A high proportion of cases admitted with this infection came up with complicated (Para pneumonic effusion and septic shock) and severe types of infection [4,27].
Rapid development of drug resistance by common bacterial causative pathogens of CAP toward commonly used drugs has complicated the selection of empirical therapy for CAP and has increased the health care cost associated with managing the disease. Streptococcus pneumonia and Haemophilus influenzae (the well-known causes of CAP) reportedly showed resistance to macrolides, penicillin, cotrimoxazole and chloramphenicol which can lead to rapid spread of these bacterial strains within the community [2,28]. This is supported by the study conducted in a specialized hospital in Southwest Ethiopia that stated among twenty Streptococcus pneumoniae isolates, overall resistance rate was high to oxacillin and low resistance were observed for erythromycin, chloramphenicol, and tetracycline; Of 16 Staphylococcus aureus isolates subjected to antimicrobial susceptibility testing, overall resistance rate were high to, oxacillin, ampicillin, cotrimoxazole, penicillin, tetracycline, erythromycin, and doxycycline. Pseudomonas aeruginosa isolates showed relatively high resistance to gentamycin. The antimicrobial testing of Pseudomonas mirabilis, Klebsiella pneumonia, Haemophilus influenza, and Escherichi coli isolates showed that all isolates had high resistance to ampicillin, tetracycline, and cotrimoxazole [23].
Prevention and control strategies of community acquired pneumonia
Both, preventive and curative measures should be implemented to address the consequences of CAP. Early diagnosis and treatment (if positive) is essential in preventing the complications associated with the infection. Breast feeding, child immunization, Vitamin A supplementation and adequate child exposure to sun light and proper ventilation and separate living rooms from kitchen are the major preventive strategies of CAP. Health education should be delivered to the community in general and to the mothers in particular regarding danger signs of severe pneumonia and early recognition of symptoms and visit to health institutions or a community health worker, nutrition, living room ventilation and administration of drugs and care as prescribed by health professionals [10]. The country has deployed a number of community health workers to the Kebeles in the country to deliver “promotive, preventive and selected curative health care services. The community health workers are playing a major role in enhancing community health awareness through delivering community health education and in treating selected (simple) health problems. They are also involved in assessing, classifying, and referring major health problems including pneumonia to health facilities [29].
Discussion
Distribution (frequency and pattern) of community acquired pneumonia
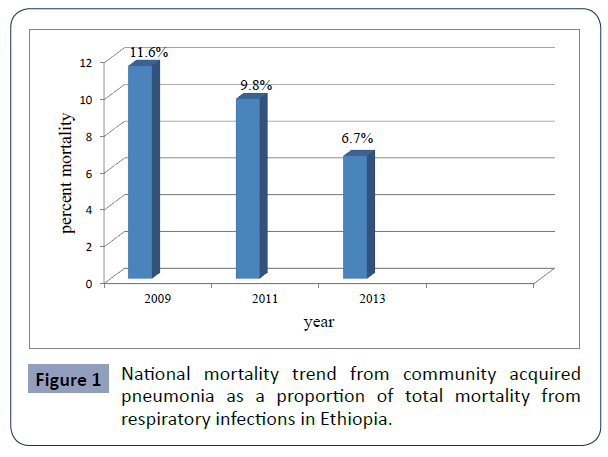
Studies conducted in different parts of Ethiopia indicated differences in prevalence, incidence, and hospital admissions due to CAP [4,11-14]. Study done in 2009 in Esete town, North West Ethiopia revealed that the prevalence of CAP among under-fives in the town was 16.1% while it was 20.6% in the rural areas of the same town in the same year [15,17] indicating that rural prevalence was higher than urban prevalence. This might be because urban residents are much closer to health related information relative to rural residents and due to the wider prevalence of CAP risk factors among rural than urban residents. The prevalence of the infection in under five children in Southern Ethiopia in 2013 was 21% [16] which was higher compared to the national Figure 1 (12.9%) of 2011 but lower than South East Asia where the estimated prevalence of the infection was 36% [30].
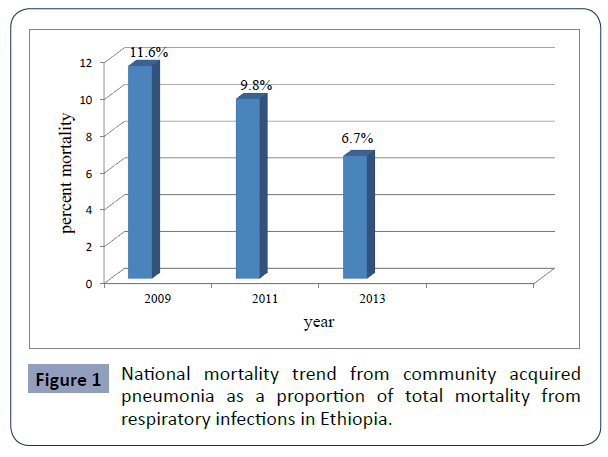
Figure 1 National mortality trend from community acquired pneumonia as a proportion of total mortality from respiratory infections in Ethiopia.
There is an increased prevalence and incidence of lower respiratory tract infections including CAP among HIV/AIDS patients compared to HIV negative individuals [7]. A study from Addis Ababa where 8% of patients diagnosed with CAP were HIV-positive, compared to 2.4% in HIV/AIDS free population and Indian study that showed incidence of CAP to be higher in patients with chronic respiratory disease and HIV positive groups compared to healthy population supports this association [18,19,31]. The association implies these groups of patients (HIV/ AIDS patients) need special attention to protect them against pneumonia and other opportunistic infections. In light of this HIV/AIDS patients are receiving different medication to prevent these infections currently. The relationship that seasonality and gender have with the risk of developing CAP was not revealed in studies done in Ethiopia but researches from another countries like Spain and Philippines have shown that the risk of the infection is higher in males than in females and that it mostly occurs during the summer season [6,32]. The prevalence and risk of CAP was also shown to be higher in individuals who have comorbid conditions like chronic respiratory and cardiovascular diseases, cerebrovascular disease, diabetes, Parkinson's disease, epilepsy, dementia, dysphagia, chronic renal or liver disease in studies done in Ireland, Egypt and India [31,33] but such a relation has never been studied thoroughly in Ethiopia.
Determinants of community acquired pneumonia
Different studies indicated various risk factors for CAP in Ethiopia. Studies from Addis Ababa and from a district in North West Ethiopia identified malnutrition, low socio-economic status, low birth weight, crowding, indoor air pollution, low immunization coverage, viral infections , Overcrowding and poor ventilation, smoking, zinc and calcium deficiency, high altitude, humid conditions, vitamin A and D deficiency, and outdoor air pollution as risk factors for CAP and other respiratory infections in populations of different age group. These risk factors were shown to be more common among the rural population than urban population [10,20,21]. This is consistent with studies from Egypt, South East Asia and India that showed poverty, indoor air pollution, poor immunization status, overcrowding, smoking and poor nutritional practices as the major risk factors for the occurrence of this infection mainly in rural areas [31,33,34]. The commonness of risk factors among the rural residents than urban may be related to the life style followed (poorer sanitation, poor hygiene, overcrowding, etc.) and low literacy rate.
The risk of developing CAP among under-five children who are malnourished and who live in severely crowded houses is more than two times higher than the risk in children who are well nourished and who live in under crowded houses [15,17]. This can be dangerous to the Ethiopian population (both urban and rural) where lower economic status have hindered proper housing and nutrition. The rural populations with relatively good economic status were also unable to provide their families with proper nutrition and sufficient and hygienic room due to lower literacy rate [13].
Bacteria are the commonest causative agent for CAP even if the infection can sometimes be caused by viruses and fungi. Studies from Addis Ababa, Arbaminch and Jimma University Specialized Hospital have shown that Streptococcus pneumonia, Haemophilus influenza and Staphylococcus aureus accounted for the highest percent of bacterial community acquired infection [10,22-24] and this agrees with the study from South Africa and United States of America where these pathogens were found to be the major causes of CAP [35,36].
Burden of community acquired pneumonia
CAP is a common and potentially-serious illness worldwide. It is the main cause of morbidity and mortality, which particularly targets under five and elderly patients and those with comorbid conditions. In adults aged over 59 years, it causes 1.6 million deaths annually [7,30]. In Ethiopia, CAP is one of the leading causes of hospital admissions and mortality especially in under five children [37,38]. The country is one of the fifteen nations that have the highest death rate from pneumonia in children younger than five years old (84.6 deaths per 10,000 under five population,) and one of the major causes of this mortality is CAP [9,11,25,26].
A study conducted in Hawassa and Jimma indicated that from the adult patients admitted with CAP, 18.79% and 20.2% death cases occurred in these facilities respectively. A significant number patients admitted to these facilities with CAP had complicated (Para pneumonic effusion and septic shock) and severe infection. The arrival of the patients to the facilities after complication made the disease management difficult and hence resulted in the death of a number of patients. The health care cost including the cost of drugs and intensive care was also significant [4,27]. This has implications on the need of strengthening early community level case management and referral of CAP and other infections and the necessity of strengthening public awareness about the infections through community health education.
An Increasing resistance of bacterial causes of CAP toward commonly used antibiotics has complicated the choice of proper therapy and has increased the health care costs of treating the infection [28]. There is an increasing report from different areas in Ethiopia that the common pathogens causing CAP like Streptococcus pneumoniae, Staphylococcus aurus, Pseudomonas aurugnosa, Haemophilus influenza and Klebsiella pneumonia are developing resistance toward commonly used medications [4,23]. This might have resulted from over?the-counter sale of these antimicrobials, mainly for self-treatment of suspected infection in humans and poor prescription practice and poor adherence of the patients to prescribed medications. The increase in resistance implies that there is a need to strengthen the control of these antibiotics use and to promote proper diagnosis and prescription at health facilities and to enhance patient adherence to the prescribed medication.
Prevention and control strategies of community acquired pneumonia
Reducing risk factors, improving case management at the community and facility levels, ensuring regular supervision and reliable logistics, and sound monitoring and evaluation are the most effective ways of reducing morbidity and mortality from pneumonia [34]. Individuals who are suspected of contracting the infection should be diagnosed and take proper treatment (if positive) to prevent complications and risk of death. Breast feeding, child immunization, vitamin A supplementation and adequate child exposure to sun light, proper ventilation and separate living rooms from kitchen should be implemented to prevent CAP [10]. Ethiopia has deployed a number of community health workers to the kebele level to deliver “promotive, preventive and selected curative health care services to the community. The community health workers are being involved in providing health education to the community in general and to the mothers in particular regarding danger signs of severe pneumonia and early recognition of symptoms and visit to health institutions, nutrition, living room ventilation and administration of drugs and care as prescribed by health professionals. They are also being involved in treating simple health problems and in assessing and referring severe and complicated health problems to health facilities. The role of community health workers coupled with improved health facility services has made the prevalence, incidence and burden of CAP to be decreased these days nationally [10,29,30,39].
The country has introduced pneumococcal vaccine to further accelerate its efforts of reducing child death due to pneumonia. Immunization against Haemophilus influenza b, measles, and pertussis are showing a good result [40].
Conclusion and Recommendation
The literature review has shown that CAP is still one of the major health problems in Ethiopia especially in under five children, even though its prevalence, incidence and disease burden is decreasing overall. Various factors contribute to the risk of developing CAP in the population. In order to address the consequences of CAP, the country is undertaking various preventive and control measures at the community and health facility level. The promotive, preventive and selected curative health care services being delivered by community health workers are showing encouraging results and hence need to be sustained.
Consent for publication
Not applicable
Competing Interests
The authors declare that they have no competing interests with respect to publication of this article
Authors’ Contributions
TA contributed to the conception and design of the review. He also undertook the review work and drafted the manuscript with TR. Both authors read and approved the final manuscript.
Funding
The authors received no financial support for the authorship and/or publication of this article.
35058
References
- Working Group of the South African Thoracic Society(2007) Management of Community-Acquired Pneumonia in Adults. S Afr Med J 97:1295-1306.
- Gutierrez F, Masia M, Rodriguez JC, Mirete C, Soldán B, et al. (2005) Epidemiology of community-acquired pneumonia in adult patients at the dawn of the 21st century: a prospective study on the Mediterranean coast of Spain. Clin Microbiol Infect 11:788-800.
- Mocelin CA, dos Santos RP (2013) Community-acquired pneumonia at the Hospital de Clínicas de Porto Alegre: evaluation of a care protocol. Braz J infect dis 17:511-515.
- Ahmedtaha OM, Yami A, Mohammed MA (2014) Treatment and Outcomes of Community-Acquired Pneumonia in Hospitalized Patients: The Case of Jimma University Specialized Hospital. Ther Innov Regul Sci 48:220-225.
- Gross AE, Van Schooneveld TC, Olsen KM, Rupp ME, Bui TH, et al. (2014) Epidemiology and Predictors of Multidrug-Resistant Community-Acquired and Health Care-Associated Pneumonia. J American society of microbiology 58:5262-5268.
- Almirall J, Bolobar I, Vidal J, Sauca G, Coll P, et al. (2010) Epidemiology of community-acquired pneumonia in adults: a population-based study. Eur Respir J 15: 757-763.
- World Health Organization (2012) The global burden of the disease. 2012 update. Geneva, Switzerland.
- Gabbad A, Alrahman G, Elawad M (2014) Childhood Pneumonia at Omdurman Paediatric Hospital, Khartoum, Sudan. Int J Multidiscip Curr Res 2:1139-1147.
- Dadi A, Kebede Y, Birhanu Z (2014) Determinants of Pneumonia in Children Aged Two Months to Five Years in Urban Areas of Oromia Zone, Amhara Region. Ethiop J Health Dev 3: 35-42.
- Mitike G, Addissie M, Admassu M (2011) Pneumonia in Under-Five Children. Ethiopian Public health training initiative 2:18-23.
- Central Statistics Agency (2011) Ethiopian demographic and health survey. Addis Ababa, Ethiopia.
- Freij L (2007) Exploring child health and its ecology. The Kirkos study in Addis Ababa an evaluation of procedures in the measurement of acute morbidity and a search for causal structure. Acta Paediatr Scand Suppl 2:171-180.
- Mariam A (2013) A two year retrospective review of reasons for pediatric admission to Chiro Hospital, Eastern Ethiopia. Ethiop Med J 43:241-249.
- Muhe L, Byass P, Freij L, Sandstrom A, Wall S (2005) A one-year community study of under-fives in rural Ethiopia: Patterns of morbidity and public health risk factors. Public Health J 109: 99-109.
- Abeje G, Wubshet M, Asres G (2014) Prevalence of pneumonia among under- five children in Este town and the surrounding rural kebeles, Northwest Ethiopia; A community based cross sectional study. Sci J Public Health 2:150-155.
- Dessalegn B (2013)Household fuel use and acute respiratory infection among younger children: An Exposure Assessment in Shebedino Woreda, Southern Ethiopia. J Health Dev 3:124-129.
- Fekadu G, Terefe M, Alemie G (2013) Prevalence of pneumonia among under- five children in rural kebeles of Northwest Ethiopia : A community based cross sectional study. Sci J Public Health 2:157-162.
- Aderaye G (2004) Community acquired pneumonia in adults in Addis Ababa: etiologic agents and the impact of HIV infection. Tuber Lung Dis 75: 308-0312.
- Bedri A, Lulseged S (2001) Clinical Description of children with HIV/ AIDS admitted at a referral hospital in Addis Ababa. Ethiop Med J 39:203–211.
- Gedefaw M, Berhe R (2015) Determinates of Childhood Pneumonia and Diarrhea with Special Emphasis to Exclusive Breastfeeding in North Achefer District, Northwest Ethiopia: A Case Control Study. Open J Epidemiology 5:107-112.
- Kebede D (2007) Risk factors for acute lower respiratory infections in under-five children in Addis Ababa: ArticleReview. Ethiop J Health Dev 11:150-155.
- Regasa B (2014) Aetiology of Bacterial Pathogens from Adult Patients with Community Acquired Pneumonia in Arba Minch Hospital, South Ethiopia. Sci J Clin Med 3:33-36.
- Regasa B,Yilma D, Sewunet TS (2015) Antimicrobial susceptibility pattern of bacterial isolates from community-acquired pneumonia patients in Jimma University Specialized Hospital, Jimma, Ethiopia. Saudi J Health Sciences 4:59-61.
- Mohammed E, Muhe L, Geyid A, Dejene A, Mekonnen Y, et al. (2000) Prevalence of bacterial pathogens in children with acute respiratory infection in Addis Ababa. Ethiop Med J 38:165-174.
- Ali M(2007) The epidemiology of infectious and noninfectious respiratory disease in Ethiopia: A review article. African J Respiratory Med 3:71-76.
- Deribew A, Tessema F, Girma B (2007) Determinants of under-five mortality in Gilgel Gibe Field Research Center, Southwest Ethiopia. Ethiopian J Health Develop 21:117-124.
- Teka Z, Taye A, Gizaw Z (2014) Analysis of risk factors for mortality of in-hospital pneumonia patients in Bushulo Major Health Center, Hawassa, Southern Ethiopia. Sci J Public Health 2:373-377.
- Daka D, Loha E, Giday A (2011) Streptococcus pneumonia and antimicrobial resistance, Hawassa Referral Hospital, South Ethiopia. J Medical Laboratory and Diagnosis 2:27-30.
- Degefie T, Marsh D, Gebremariam A (2009) Community case management improves use of treatment for childhood diarrhea, malaria and pneumonia in a remote district of Ethiopia. Ethiop J Health Dev 23:120-126.
- Center for Disease Control and Prevention (2013) Global community acquired pneumonia epidemiology. A comprehensive report.
- MishraA, BeheraG (2016) Community Acquired Pneumonia, Detection and Prevention: A Hospital Based Descriptive Study. Int J Contemporary Med Res 3:1127-1129.
- Torres A, Peetermans W, Viegi G, Blasi F (2016) Risk factors for community-acquired pneumonia in adults in Europe: a literature review. Thorax 68:1057-1065.
- Butt Z, Aamar A, Nagi D (2012) Factors Associated With In – Hospital Mortality in Community Acquired Pneumonia in an Irish District Hospital: A Short Report. Annals KEMU 18:292-295.
- Ghimire M, Bhattacharya S, Narain J (2012) Pneumonia in South-East Asia Region: Public health perspective. Indian J Med Res 135:459-468.
- Zar H, Jeena P, Argent A, Gie R, Madhi SA, et al. (2009) Diagnosis and management of community-acquired pneumonia in childhood. S Afr J Epidemiol Infect 24:25-36.
- Stupka J, Mortensen E, Anzueto A, Restrepo MI (2009) Community-acquired pneumonia in elderly patients. Aging Health 5:763–774.
- Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, et al. (2010) Global, regional, and national causes of child mortality: a systematic analysis. Lancet 375: 1969-1987.
- Central Statistics Agency and ICF Macro (2011) Ethiopia Demographic and Health Survey. Preliminary Report. Addis Ababa, Ethiopia.
- Federal Ministry of Health (2014) Health and health related indicators 2012/2013. A comprehensive report. Addis Ababa, Ethiopia, 2014.
- Global Alliance for Vaccines and Immunization (2011) Measures to tackle childhood killer in Ethiopia: GAVI press release. Addis Ababa. Ethiopia.