Dimitrios Tziallas1*, Catherine Kastanioti2, Kostas Savvas3, Michael S. Kostapanos3, Vasillios Tziallas4, Petros Skapinakis5, Moses S.Elisaf6, Venetsanos Mavreas7
1MSc, NFESC, Head Nurse, Department of Internal Medicine, School of Medicine, University of Ioannina, Greece
2MSc, PhD, Assistant Professor, Department of Health care Management, Technological Institute of Kalamata, Kalamata, Greece
3MD, University Hospital of Ioannina, Department of Internal Medicine, Greece
4MSc, Associate Head Nurse, Department of Urology, General State Hospital of Athens, Greece
5MD, MPH, PhD, Assistant Professor, Department of Psychiatry, School of Medicine, University of Ioannina, Greece
6MD, PhD, Professor of Pathology, Department of Internal Medicine, School of Medicine, University of Ioannina, Greece
7MD, PhD, Professor of Psychiatry, Department of Internal Medicine, School of Medicine, University of Ioannina, Greece
- *Corresponding Author:
- Dimitrios Tziallas
University Hospital of Ioannina
45500 Ioannina, Greece
Tel: +30 265109929621
Fax: +30 265199620
E-mail: dtziallas@gmail.com
Key words
Health related quality of life, metabolic syndrome, cardiovascular disease, depression.
Introduction
Over the recent years, there is a growing interest of the impact of various psychosocial factors in cardiovascular morbidity and mortality1. Several prospective studies suggested that common mental disorders, such as depression and anxiety, may be associated with an increased risk of cardiovascular events in either healthy subjects or patients with coronary heart disease (CHD) [1]. Similarly psychosocial factors, such as enhanced job strain as well as the lack of social support, have been proposed as risk factors for CHD.
The Metabolic syndrome [MetSyn] comprises the clustering of traditional cardiovascular risk factors, including obesity, hypertension, dyslipidemia and hyperglycemia [1] and is highly associated with increased risk of cardiovascular disease [2,3]. In developed countries MetSyn is a common condition and is being increasingly found in older populations. The Third National Health and Nutrition Survey has estimated that 1 of 5 US citizens have this condition [4], a statement that is in agreement with the results from the ATTICA study, in a representative sample from the general population in Greece [5]. Moreover, according to the results of the MetS-Greece Study [6] a cross-sectional analysis of 4153 participants, MetSyn is highly prevalent in the Greek adult population.
Although, the aetiology of MetSyn is not entirely understood, is considered as a complex health problem that can trigger physical, emotional and psychosocial problems [7]. Previous studies have shown that this condition is associated with an increase risk for psychiatric co-morbidity, stress and impaired health-related quality of life [HRQoL] [7-12]. The Pilsen Longitudinal Study III [13] had proven that depressive disorders were nearly twice as frequent in patients with MetSyn compared to individuals without MetSyn. On the other hand, prospective data, though limited, suggest that depression, anger and negative health behaviours predict increased risk for the metabolic syndrome [14-15]. As a consequence, MetSyn is a risk factor for the development of psychological strain in terms of depression and anxiety and vice versa [16].
Although, obesity [8,17-21] and diabetes [22-24] have obvious consequences on HRQoL, the question whether MetSyn is associated with the change of well-being and HRQoL requires further evaluation. Therefore, the aim of this prospective cross-sectional study is to assess the hypothesis that MetSyn is an independent determinant of HRQoL.
Material and methods
Study population
This cross-sectional study was conducted in Ioannina, a major university city of the Northwestern part of Greece. New consecutive patients with a presumptive diagnosis of MetS referred to the Outpatient Lipid Clinic of the University Hospital of Ioannina (the referral centre for the broader region of Epirus with 300,000 inhabitants), from April 2007 to January 2009, were involved in the study. Participants were excluded if they had significant medical or psychiatric comorbidities. These included coronary heart disease, types 1 or 2 diabetes, thyroid disorders, severe hepatic or renal diseases. For the diagnosis of the MetS the New International Diabetes Federation (IDF) definition and its diagnostic criteria were used [25]: i) BMI >30kg/m² and waist circumference does not need to be measured, ii) triglyceride (TG) levels > 150 mg/dL, iii) reduced high-density-lipoprotein (HDL)-cholesterol levels < 40 mg/dL for men and < 50 mg/dL for women, iv) high fasting glucose ≥ 100 mg/dL and v) elevated blood pressure ≥ 130/85 mm Hg or relevant antihypertensive treatment. According to the new IDF definition, MetSyn is diagnosed when patients have central (abdominal) obesity which is a prerequisite factor plus any two of the above criteria.
Study design - study cohort
According to the above mentioned definition, our population was divided into those subjects who fulfilled the diagnostic criteria for the MetS (MetS group; cases) and those who did not fulfill the criteria for the diagnosis of the MetS (control group; controls). All subjects gave a written informed consent and the study protocol was approved by the Ethics Committee of the University Hospital of Ioannina.
Clinical evaluation
According to the study protocol, at the first visit of each subject in the Outpatient Lipid Clinic, the following parameters were evaluated: i) anthropometric indices [body mass index (BMI), waist circumference], ii) smoking habits, iii) blood pressure readings, iv) routine laboratory measurements including fasting blood glucose and serum lipid profile.
Waist circumference was measured by placing a tape in a horizontal plane around the abdomen between the lower rib and iliac crest. The tape should have been snug without compressing the skin and parallel to the floor. Measurements were taken at the end of a normal expiration by the same investigator. Blood pressure was measured in triplicate, following ten minutes rest, at each visit. (Measurements were carried out by trained physicians in the sitting position using a standard validated automated sphygmomanometer).
All laboratory measurements were performed at the Biochemistry Laboratory of the University Hospital of Ioannina by standardized methods using an Olympus AU600 clinical chemistry analyzer (Olympus Diagnostica, Hamburg, Germany).
Assessment of Health-related quality of life
All participants completed the Medical Outcomes Study, Short Form-36 (SF-36) [26] to assess HRQoL. The SF-36 health survey contains 36 questions covering functional health status and general health [27], and has been validated in a Geek general population [28]. The questions are summarized into eight subscales measuring; physical functioning [PF], role physical [RP], bodily pain [BP], general health [GH], vitality [VT], social functioning [SF], role emotional [RE] and mental health [MH], with higher scores [0-100 range] indicating better health.
Assessment of Anxiety and Depressive symptoms
Anxiety and depressive symptoms were assessed by a validated Greek version of the Hospital Anxiety and Depression Scale (HADS) [29]. The HADS is a brief self-assessment scale assessing the two most common aspects of psychological distress found in hospital settings: anxiety and depression [30]. The scale consists of 14 items, seven for each subscale, and each item is rated on a four-point (0-3) scale, giving maximum scores of 21. The scoring system ranges from the absence of a symptom or the presence of positive features (scoring 0) to the maximal presentation of symptoms or the absence of positive features (scoring 3). Although, there is no single generally accepted cut-off score for the HADS, in the present study scores of 11 or more on either subscale are considered to be a significant 'case' of psychological morbidity, while scores of 8–10 represents 'borderline' and 0–7 'normal'.
Statistical analysis
The SF-36 subscales were scored according to documented procedures [26]. Normality was tested with Kolmogorov-Smirnov test. Data were expressed as mean ± SD, except for non-Gaussian parameters, which were presented as median (range). Descriptive statistics were used to evaluate the distribution of socioeconomic, demographic and clinical variables and HRQoL and depression and anxiety measurements. Measurements were compared within groups, using independent Chi-square and Mann-Whitney nonparametric test. The strength of associations of socioeconomic parameters, anxiety and depressive symptoms as well as HRQOL dimensions with the MetSyn were assessed by means of regression analysis, comparing subjects who met the diagnostic criteria for the MetS and those who did not meet the criteria for the diagnosis of the MetS. These associations were first tested in univariate analysis (Pearsons and Spearman correlations coefficients) and multivariate analysis was then performed by binary logistic regression analysis. Significance levels were set at p<0.05 in all cases. SPSS 16.0 (SPSS Inc., Chicago, IL, USA) and Stata 9.0 (StataCorp, College Station, Texas) were used to perform the statistical analyses.
Results
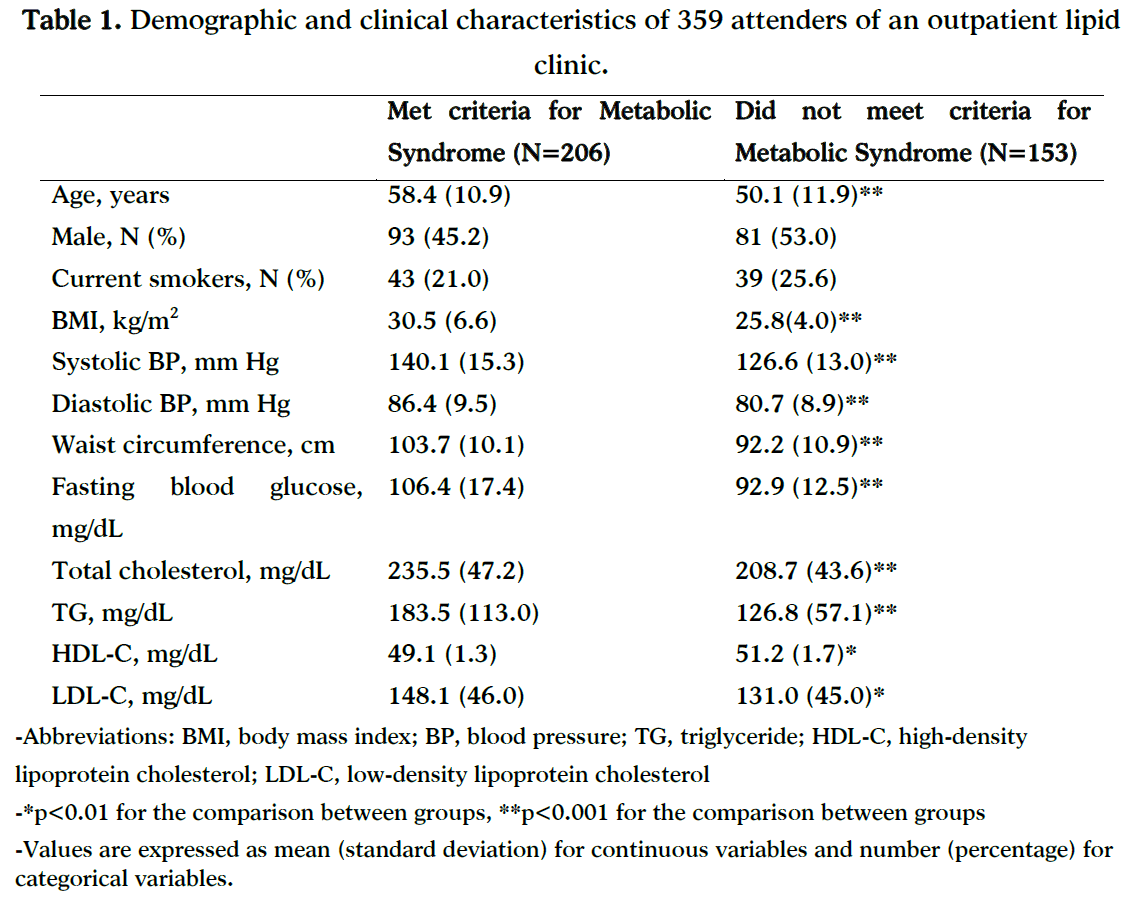
A total of 359 subjects [206 (57.4%) subjects who fulfilled the diagnostic criteria for the MetS (cases) and 153 (42.6%) subjects who did not meet the criteria for the diagnosis of the MetS (controls)] were included in the present study. Baseline demographic and clinical characteristics of the study population are shown in Table 1. Patients with the MetS were older as compared to controls (Table 1). As expected, patients with the MetS exhibited higher BMI, waist circumference as well as BP measurements than controls (Table 1). Furthermore, fasting blood glucose, TG, total cholesterol as well as LDL-cholesterol and HDL-cholesterol levels were significantly higher in the MetSyn group than in the control group (Table 1). No difference between groups was noted with regard to the proportion of the current smokers.
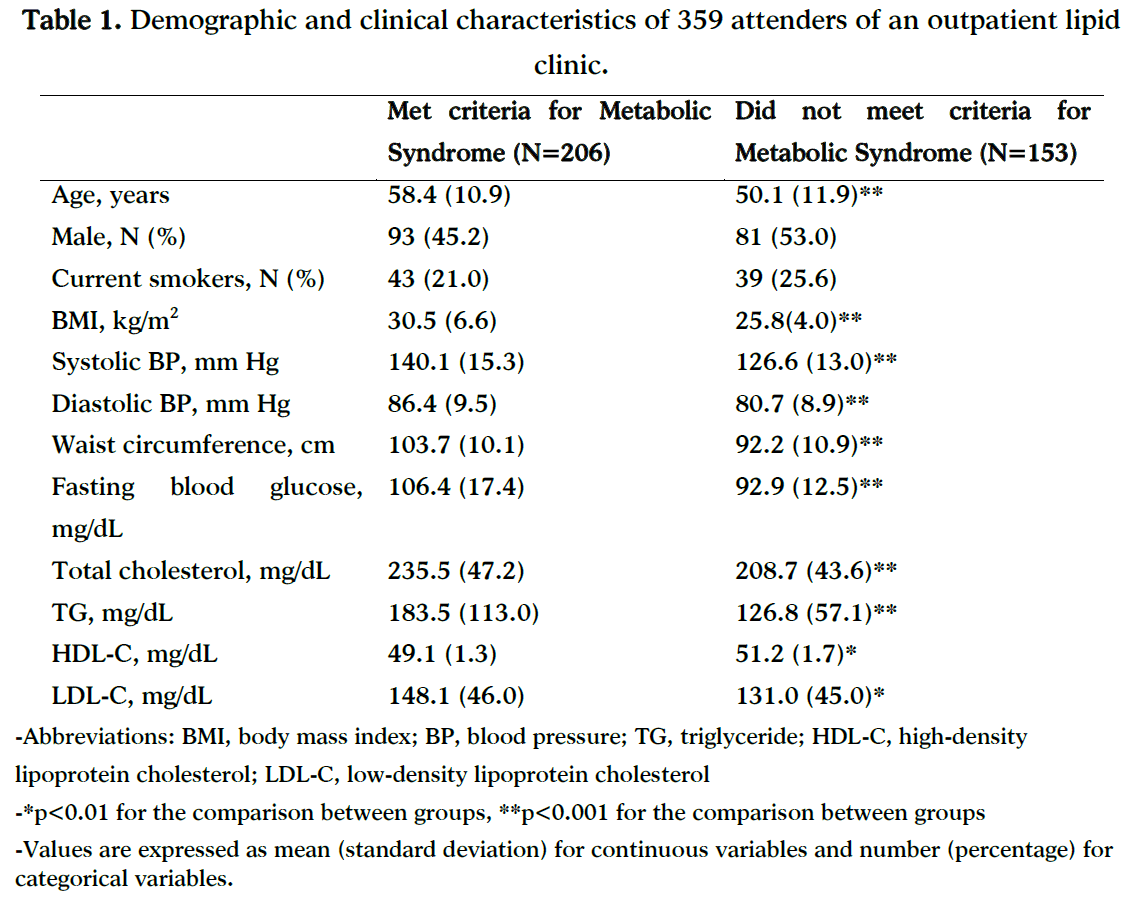
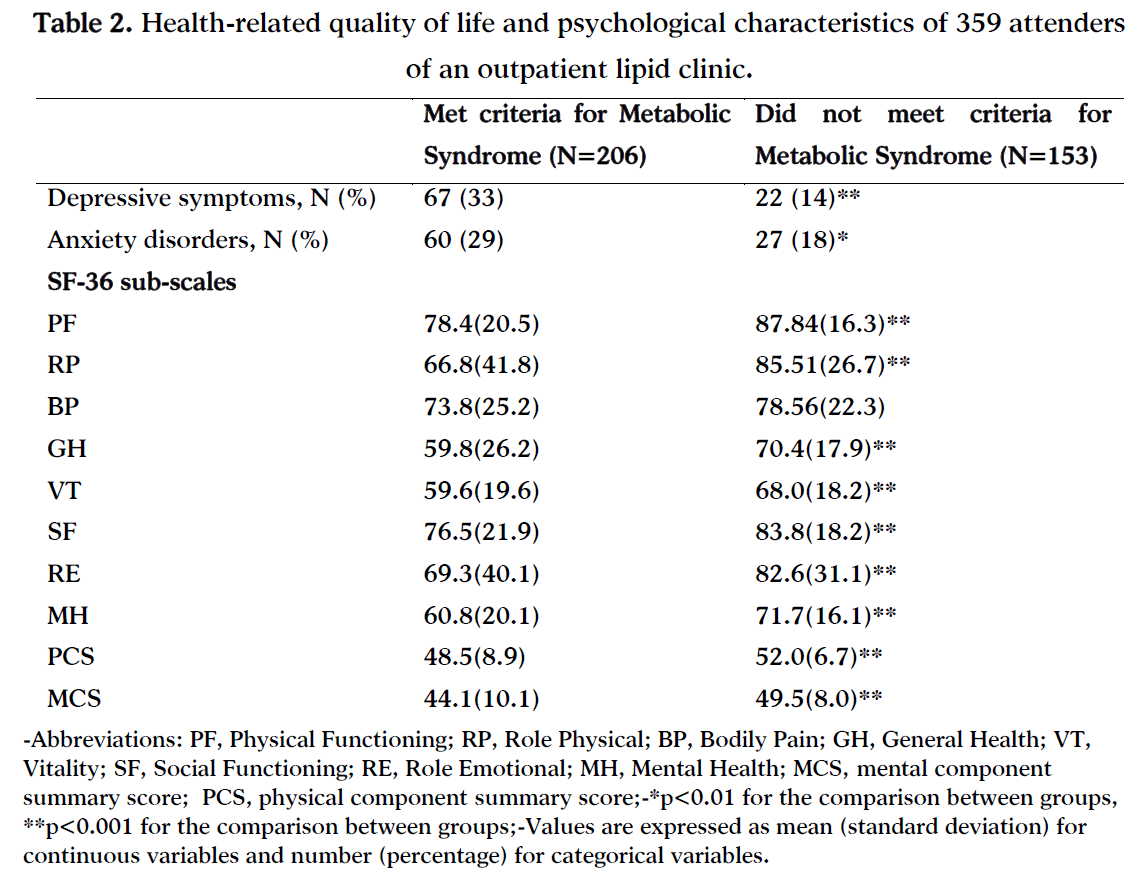
Table 2 presents comparisons of HRQoL between subjects with and without MetSyn. The subjects in the MetSyn group reported significantly lower scores on all subscales except of bodily pain. Subjects with MetSyn also scored significantly lower on the physical component summary (PCS) score as well as on the mental component summary (MCS) score. A predominance of anxiety and depressive symptoms was observed among subjects with MetSyn as compared to controls (Table 2).
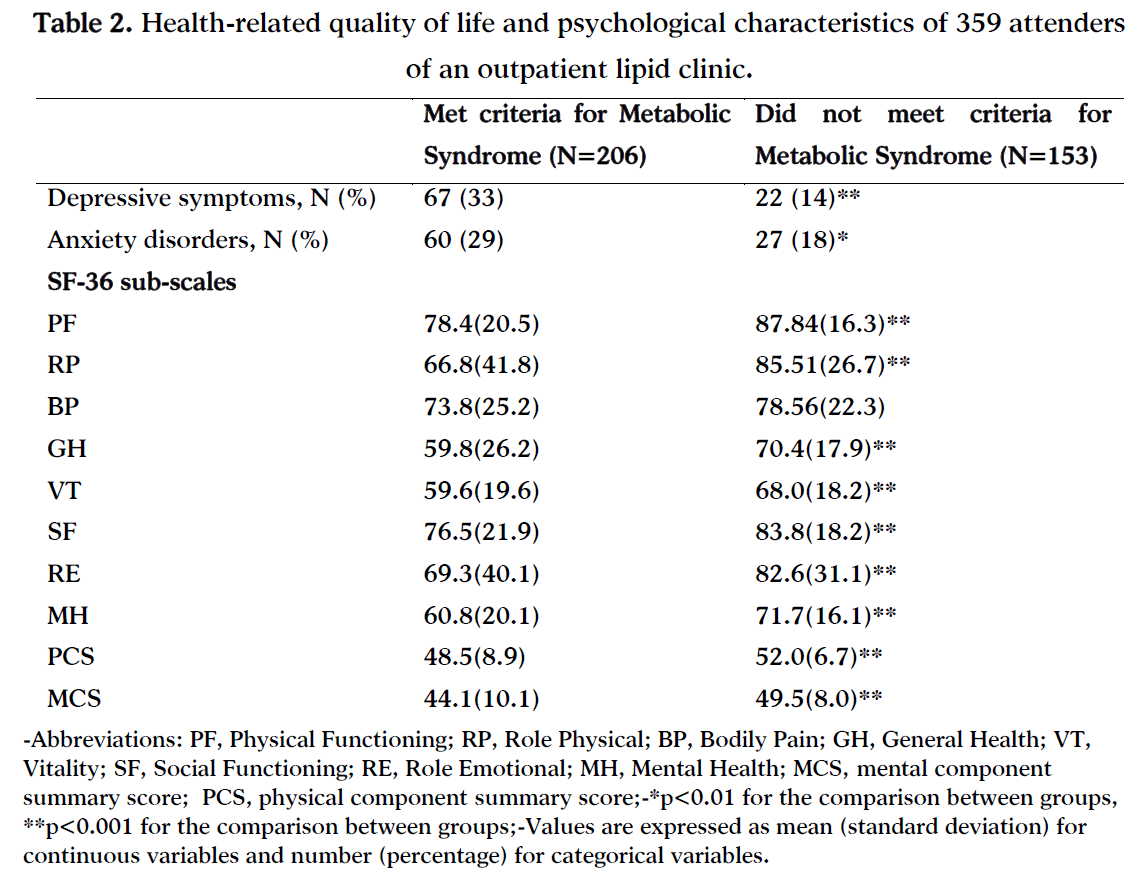
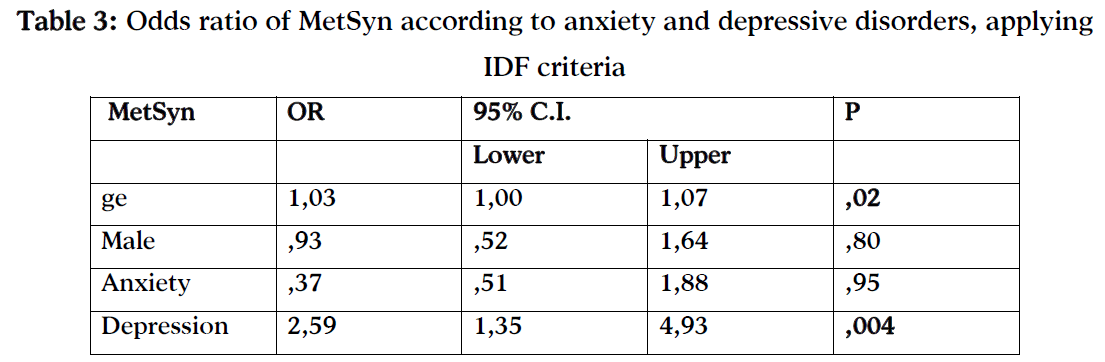
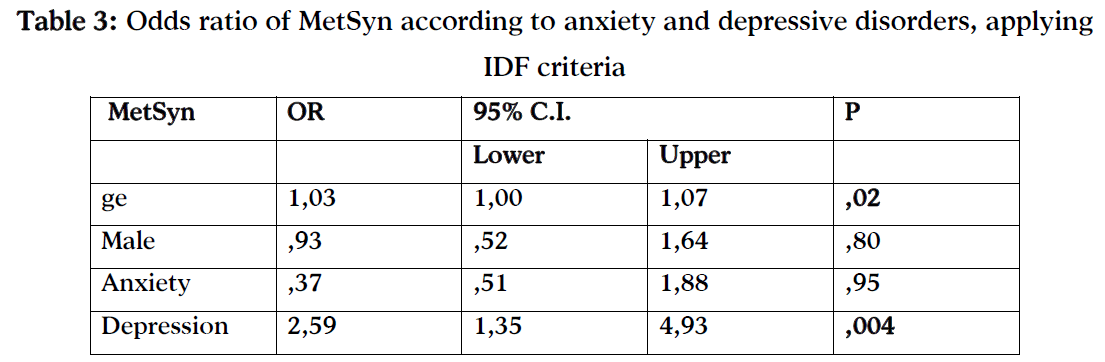
Table 3 presents the results of the multiple logistic regression models, giving the likelihood of having MetSyn for anxiety and depressive symptoms. Age was independently associated with risk of having MetSyn.
Discussion
MetS is a combination of metabolic risk factors and is associated with depressive symptoms. The impact of MetS on HRQoL is yet to be clearly established, although according to various studies obesity [9], diabetes [17] and hypertension [12] had obvious consequences on HRQoL [8].
The major finding in the present study is that MetSyn is significantly correlated with impaired HRQoL. Subjects with MetSyn reported lower SF-36 scores on seven of the eight subscales except of bodily pain. In addition, subjects with MetSyn scored significantly lower on the physical component summary (PCS) score as well as on the mental component summary (MCS) score than did participants without the syndrome. Comparing our data with descriptive Greek population “norms” it is revealed a decrease in all SF-36 subscales scores [31].
Obesity is associated with a profound decrease in HRQoL and the most significant impairment tends to be associated with physical domains of functioning [8]. The mean BMI of subjects in this study was overweight (28.45 Kg/m2) according to the IDF definition for MetSyn, which includes abdominal obesity as an essential component. In this regard, it is not surprising that being obese (BMI with MetSyn 30.5 Kg/m2 vs 28.8 Kg/m2, p<0.001) was a significant predictor of MetSyn prevalence and had a negative impact on the PCS score of SF-36 instrument, particularly in MetSyn subjects. Recent studies [7-9,32,33] suggest that MetSyn is a complex condition involving both physical and psychological aspects.
The high prevalence of anxiety and depressive symptoms in subjects with MetSyn, also observed in our study, may be of help to explain the association between MetSyn and lower MCS score.
Our results are consistent with the previous findings indicating that psychiatric disorders are associated with MetSyn [11,32,33]. Furthermore, we should recognize that being labelled with a disease (i.e. the MetS) may have accounted for the impact of the MetS on mental functioning observed in our study. This impact may have passed through an increase of pre-existing anxiety or depressive symptoms after being labelled with a disease.
Our results must be interpreted in the light of certain limitations. Namely, the data are cross-sectional and therefore we were unable to draw conclusion on the causal relationship between HRQoL and MetSyn. Longitudinal studies should explore further this issue. Second, we used a generic instrument, the SF-36 questionnaire, as a MetSyn-specific HRQoL instrument has not been developed yet. In contrast to generic measures, disease-specific instruments are designed to identify HRQoL associated with specific health problems.
There is also the possibility of measurement errors, especially in the assessment of psychiatric symptoms. The latter were crudely assessed with a simple self-reported instrument and there is the possibility of misclassification. However, this will be most likely of a random nature and a systematic error is unlikely. Third, the prevalence of MetSyn in study subjects based on IDF criteria was 57.4%. The use of the IDF criteria of MetSyn has provided a higher prevalence estimate of MetSyn than the estimate based on the NCEP ATP III criteria in the European population [34].
In this cross-sectional study we identified that an increased emotional distress is strong and independent predictors of the MetSyn. Since the MetSyn serves as a prodromal stage in the development of atherosclerotic vascular disease, it is crucial to adopt an approach in order to optimize the identification of subjects at risk for the development of this syndrome. High cardiovascular risk derived from clustering of risk factors in the MetS should be presented to those subjects as an opportunity for action to reduce risk through addressing lifestyle and adhering to treatment. Then, behavioral along with psychological prevention strategies could stand as helpful tools in the primary prevention of atherosclerotic vascular disease and its related outcomes. Unfortunately, in Greek healthcare system, there are few healthcare units that can provide a holistic approach to the management of cardiovascular risk, mostly within tertiary healthcare units, including university hospitals. A well-designed study conducted in units of primary health care could provide more representative, population-based data with regard to potential associations of psychosocial and sociodemographic characteristics with morbidities, such as the MetS.
Conclusion
Health professionals should be prompted to recognize subjects at high risk for cardiovascular disease attending the primary prevention healthcare system, by taking into consideration not only classical cardiovascular risk factors, but also socio-economic, educational characteristics and personality traits of each individual.
5300
References
- Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr, Lenfant C. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. National Heart, Lung, and Blood Institute; American Heart Association. Arterioscler Thromb Vasc Biol. 2004; 24(2):e13-8.
- Malik S, Wong ND. Metabolic syndrome, cardiovascular risk and screening for subclinicalatherosclerosis. Expert Rev Cardiovasc Ther 2009; 7:273-280.
- Milionis HJ, Rizos E, Goudevenos J, Seferiadis K, Mikhailidis DP, Elisaf MS. Components of the metabolic syndrome and risk for first-ever acute ischemic nonembolic stroke in elderly subjects. Stroke. 2005 Jul; 36(7):1372-6.
- Horton ES. Effects of lifestyle changes to reduce risks of diabetes and associated cardiovascular risks: results from large scale efficacy trials. Obesity (Silver Spring). 2009; 17 Suppl 3:S43-8.
- Panagiotakos DB, Pitsavos C, Skoumas Y, Stefanadis C. The association between food patterns and the metabolic syndrome using principal components analysis: The ATTICA Study. J Am Diet Assoc. 2007;107(6):979-87.
- Athyros VG, Bouloukos VI, Pehlivanidis AN, Papageorgiou AA, Dionysopoulou SG, Symeonidis AN et al: For the MetS-GREECE Collaborative Group: The prevalence of the METabolic Syndrome in GREECE-The MetS – GREECE. Multicenter Study. Diabetes Obes Metab 2005; 7: 397-405.
- G.H. Frisman, M. Kristenson. Psychosocial status and health related quality of life in relation to the metabolic syndrome in a Swedish middle-aged population European Journal of Cardiovascular Nursing 2009; 8: 207–215
- Han J. H, Park H S, Shin C. I, Chang H. M, Yun KE, Cho SH, et al: Metabolic syndrome and quality of life (QOL) using generalised and obesity-specific QOL scales. Int J Clin Pract, May 2009, 63, 5, 735–741
- Tsai AG, Wadden TA, Sarwer DB, Berkowitz R, Womble LG, Hesson LA, et al: Metabolic Syndrome and Health-related Quality of Life in Obese Individuals Seeking Weight Reduction. Obesity(2008; 16: 59–63.
- Neumann NU, Frasch K. Coherences between the metabolic syndrome, depression, stress and physical activity. Psychiatr Prax. 2009; 36(3):110-4.
- Goldbacher EM, Matthews KA. Are psychological characteristics related to risk of the metabolic syndrome? A review of the literature Ann Behav Med 2007; 34:240-252.
- Sullivan PW, Ghushchyan V, Wyatt HR, Wu EQ, Hill JO. Impact of cardiometabolic risk factor clusters on health-related quality of life in the U.S. Obesity 2007;15:511–521.
- Frasure-Smith N, Lesperance F. Reflections on depression as a cardiac risk factor. Psychosom Med 2005;67(suppl 1):S19-25
- Chang P, Ford D, Meoni L, Wang N, Klag M. Anger in young men and subsequent premature cardiovascular disease; the precursors study. Arch Intern Med 2002; 162:901-16
- Maciejewski ML, Patrick DL, Williamson DF. A structured review of randomized controlled trials of weight loss showed little improvement in health-related quality of life. J Clin Epidemiol 2005; 5:568–578.
- Huang IC, Frangakis C, Wu AW. The relationship of excess body weight and health-related quality of life: evidence from a population study in Taiwan. Int J Obes 2006; 30: 1250–9.
- Banegas JR, López-García E, Graciani A, Guallar-Castillón P, Gutierrez-Fisac JL, Alonso J,et al. Relationship between obesity, hypertension and diabetes, and health-related quality of life among the elderly. Eur J Cardiovasc Prev Rehabil 2007; 14:456–62.
- Vanhala M, Jokelainen J, Keinänen-Kiukaanniemi S, Kumpusalo E, Koponen H. Depressive symptoms predispose females to metabolic syndrome: a 7-year follow-up study. Acta Psychiatr Scand. 2009 Feb; 119(2):137-42.
- Wadden TA, Phelan S. Assessment of quality of life in obese individuals. Obes Res 2002; 10:50S–57S.
- Hassan MK, Joshi AV, Madhavan SS, Amonkar MM. Obesity and health-related quality of life: a cross-sectional analysis of the US population. Int J Obes 2003; 27:1227–1232.
- Kolotkin RL, Meter K, Williams GR. Quality of life and obesity. Obes Rev 2001; 2:219–229.
- Fontaine KR, Barofsky I. Obesity and health-related quality of life. Obes Rev 2001; 2:173–182.
- Corica F, Corsonello A, Apolone G, Mannucci E, Lucchetti M, Bonfiglio C, et al. Metabolic syndrome, psychological status and quality of life in obesity: the QUOVADIS Study. Int J Obes 2008; 32: 185–91.
- Poljicanin T, Ajdukovic D, Sekerija M, Pibernik-Okanovic M, Metelko Z, Vuletic-Mavrinac G. Diabetes mellitus and hypertension have comparable adverse effects on health-related quality of life. BMC Public Health. 2010 Jan 13; 10(1):12. [in press]
- Website: The IDF https://www.idf.org/webdata/docs/IDF Metasyndrome definition. pdf /Accessed: 29 Aug 2005.
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36) I. Conceptual framework and item selection. Med Care 1992; 30:473-483.
- Ware JE, Kosinski M, Keller SD. SF-36 physical and mental health summary scales: A user's manual. New England Medical Center, Health Institute, Boston, MA, 1994.
- Pappa E, Kontodimopoulos N, Niakas D. Validating and norming of the Greek SF-36 health survey. Qual Life Res 2005; 14:1433-38.
- Mystakidou K, Tsilika E, Parpa E, Katsouda E, Galanos A, Vlahos L. The Hospital Anxiety and Depression Scale in Greek cancer patients: psychometric analyses and applicability. Support Care Cancer 2004; 12:821-825.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67:361-370.
- Galanis C, Kontodimopoulos N, Dalekos GN, Niakas D. A comparative study of health-related quality of life in patients with hepatitis B and C. Archives of Hellenic Medicine 2007; 24(Suppl. 1):51-57
- McIntyre RS, Rasgon NL, Kemp DE, Nguyen HT, Law CW, Taylor VH, et al. Metabolic syndrome and major depressive disorder: co-occurrence and pathophysiologic overlap. Curr Diab Rep 2009;9:51-59.
- Laudisio A, Marzetti E, Pagano F, Pozzi G, Bernabei R, Zuccala G. Depressive Symptoms and Metabolic Syndrome: Selective Association in Older Women. J GeriatrPsyciatr Neurol 2009; in press.
- Athyros VG, Ganotakis ES, Elisaf M, Mikhailidis DP. The prevalence of the metabolic syndrome using the National Cholesterol Educational Program and International Diabetes Federation definitions. Curr Med Res Opin 2005; 21:1157-1159