Keywords
Intuition; Nursing practice; Years of experience
Introduction
Intuition constitutes a phenomenon which appears in international bibliography and is extremely intricate and difficult in the examination and understanding of levels of the nursing staff [1-4]. There have been given various definitions of intuition in nursing. In a research study some researchers defined intuition as the kind of knowledge, for the access to which there was no conscious awareness of reasoning [1]. Another researcher suggests that it is a rational procedure based on “silent” learning. In more detail, the experiences of a person are stored deeply in the mind and reemerge in the form of intuition [2]. Furthermore, intuition in nursing has also been defined as the outcome of the incorporation of ways of knowledge into an unexpected awareness which, subsequently, will generate analytical procedures that will guide nursing care [3]. The theory of intuition on which the study in point was based defines intuition as a non-linear procedure of knowledge, which results from three basic factors: the emotional and physical awareness or the creation of connections on a physical or even mental level. The awareness (intuition) stems from the interaction of these three factors [4].
The emotional awareness is defined as knowledge derived from feelings that can be either positive or negative concerning the evaluation of the patient condition or patient care and empathy [5,6].
Physical awareness is the knowledge that transpires from the body and can be construed from the five sensory organs. But it can also be perceived beyond the sensory organs, for example, shivers along the spine, headaches, muscular stiffness, general frustration, increase of heartbeat, perspiring palms, stress, and clenched jaws [6].
The third part of intuition is the formation of connections with patients which can exist on a physical or spiritual level [5,7,8]. The relations that allow the understanding of body language and nonverbal communication are called physical. Relations can also exist on a spiritual level [8]. On this level there is deeper perception of knowledge and intuition may manifest itself as energy that the nurse feels towards a patient.
Importance
Due to the difficulty in defining intuition there has been a notion that the former constitutes an unreliable, anti-scientific and unworthy nursing method. However, on the basis of bibliography it actually plays a significant part in clinical decision making [9]. If solely scientifically documented nursing practices are taken into account, then not only subjective knowledge but also interaction between the nurse and the patient should be invalidated, albeit the former being, in essence, the basic source of subjective stimuli. The nurses denying their intuition and relying exclusively on reason is not adequate in nursing practice, [8] which consequently tends to be downgraded [10]. According to literature, intuitive experience is necessary for spiritual development; for this reason, it is imperative that we recognize and trust the intuitive incidents which occur [8]. Intuition must not be ignored because it is a part of nursing practice and nursing decision making [11,12]. With the acceptance of intuition, nursing knowledge is expanded and experience is reinforced [13]. This leads to the enhancement of nursing procedure, since the patient is to directly or indirectly benefit from the use of intuition [9].
The aim of the study was the evaluation of the intuition levels of the nursing staff who work in the nursing units of state hospitals in the prefecture of Iraklion.
Methodology
The aim of this study was to describe and compare the intuition levels of the nursing staff working in the Emergencies Department, the Intensive Care Unit and in the surgical clinics of the University General Hospital of Iraklion and the Venizeleion- Pananion General Hospital of Iraklion. The research questions were the following:
1. What are the intuition levels of the nursing staff working in the Emergencies Department of the two state hospitals in the prefecture of Iraklion?
2. What are the intuition levels of the nursing staff working in the Intensive Care Unit of these two state hospitals in the prefecture of Iraklion?
3. What are the intuition levels of the nursing staff working in the surgical clinics of the two state hospitals in the prefecture of Iraklion?
4. Is there a difference in the intuition levels of the nursing staff in terms of department of work?
The research was conducted in the two state hospitals of the Iraklion Prefecture, Crete, namely the University General Hospital of Iraklion and the Venizeleion-Pananeion General Hospital of Iraklion. The selection of data lasted for 2 months, that was from September to October 2013.
In order for the study to be conducted a protocol was submitted and a written approval was granted by the administrations of the nursing services of the two hospitals, the 7th Health Region of Crete and the directors of the departments whose staff was to participate in the study. Additionally, reassurance was given by the researchers that the anonymity of the participants will be retained and the findings of the study will exclusively be used for research purposes.
For the collection of the sample, the method of non-random sampling, specifically, convenience sampling was implemented during the study. The sample of this research work was comprised of 122 members of nursing staff and their verbal consent was requested for their participation in the study.
The research instrument used in the study was the Smith Intuition Instrument questionnaire for the measurement of intuition levels of the nurses. The questionnaire which was used for the selection of the data stems from the Greek translation of the American “Smith Intuition Instrument” which was created in 2007 by Anita Joel Smith, associate professor in the University of Alabama (Maternal Child of Nursing, University of South Alabama).
It contains 5 questions about the demographic characteristics of the nursing staff and a main body of 18 questions which are divided into 4 categories: physical sensations, bad feelings, spiritual connections, reassuring feelings. The level of intuition results from the calculation of the total score of the Likert answers to the questions. The grading is specifically as follows:
Low intuition levels score: 18 – 42
Mean intuition levels score: 43 – 66
High intuition levels score: 67 -90
The demographics included the following: gender, age, qualification, work department, and years of experience.
The nursing staff were required to reply to each question on a rating of possible responses from 1–5 on the Likert scale, whereby: (1) never, (2) rarely, (3) sometimes, (4) often, (5) always.
The Greek translation of the questionnaire followed the double Backward translation method and cultural adaptation was conducted via consensus panel methodology, prior its final form [14,15]. In order to assess the reliability of the questionnaire, the test-retest reliability [14,15] was conducted on a sample of 10 respondents refilling in the questionnaire at an interval of 3 weeks in between.
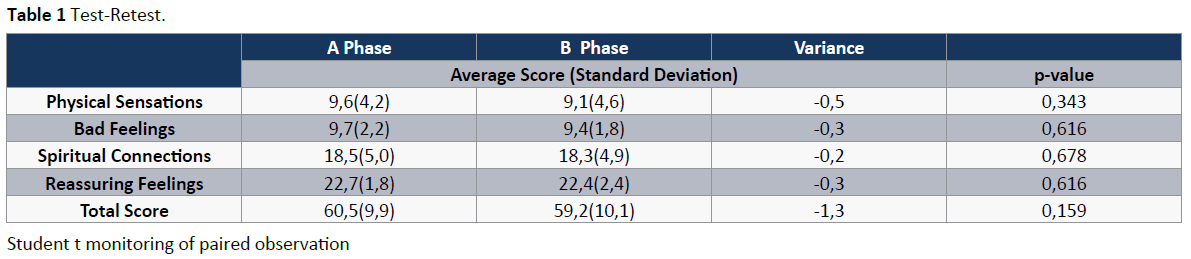
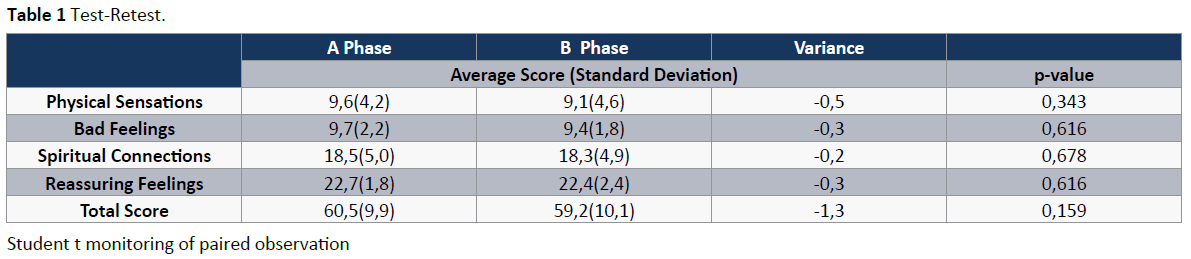
During the monitoring of test-retest, the 10 members of the nursing staff who filled in the questionnaire gave a total reliability score 0.871 as measured by Cronbach alpha in phase A and 0.899 in phase B. Additionally, the 4 units of the questionnaire as well as their total score were calculated and the 2 phases were compared. No statistically significant difference was found, which indicates the consistency of the questionnaire (Table 1).
As regards the reliability of the research instrument, the total reliability score was 0.895 as measured by Cronbach alpha, while in each unit separately a reliability score of 0.804 was produced, as measured by Cronbach alpha, in the category of physical sensations, 0.710 in the bad feelings, 0.830 in spiritual connections and 0.875 in the category of reassuring feelings.
Results
Sample description
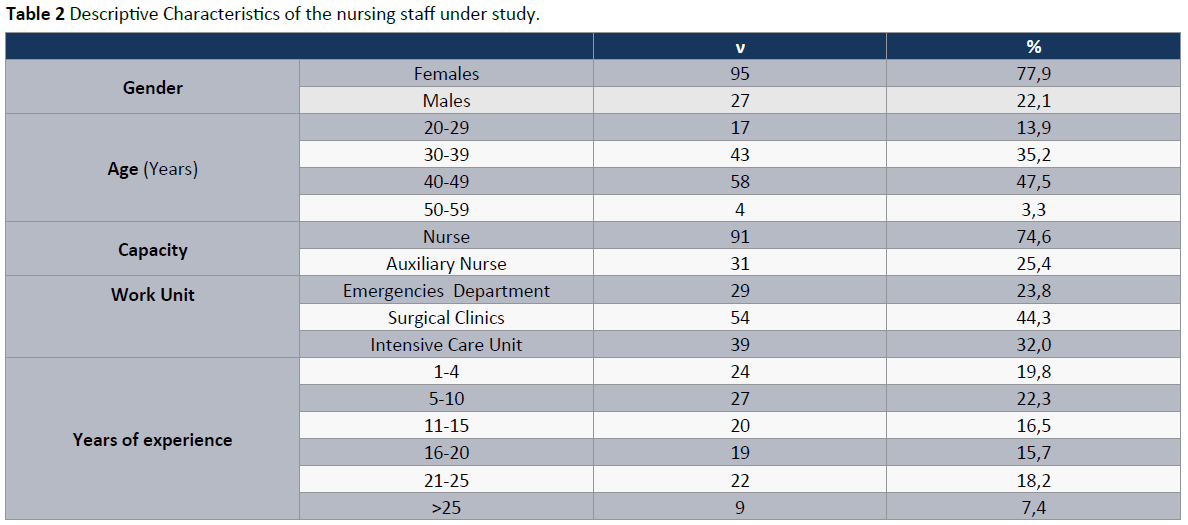
The sample in the study was comprised of 122 members of nursing staff, 77.9%of whom (n=95,) were females and 22.1% (n=27) males (Table 2). In terms of age, the majority of the sample featured an age range between 30 and 49 years (83%, n=101) (Table 2) with a range of work experience between 1 and 25 years (n=112).
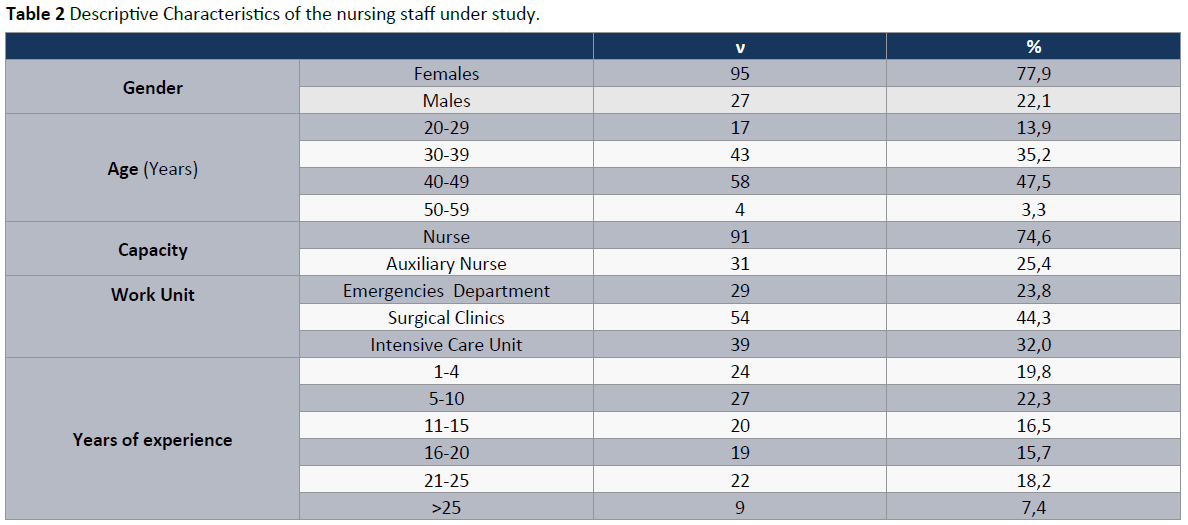
In terms of work capacity, 74.6% of the respondents (n=91) were registered nurses and 25.4% (n=31) were auxiliary nurses (Table 2).As regards the work units, 23.8% (n=29) worked at the Emergencies Department, 44.3% (n=54) in surgical clinics and 32% (n=39) in Intensive Care units (Table 2).
Intuition scale in the nursing staff under study.
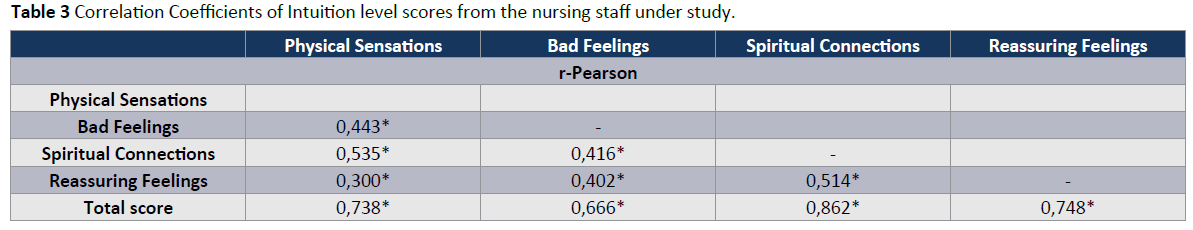
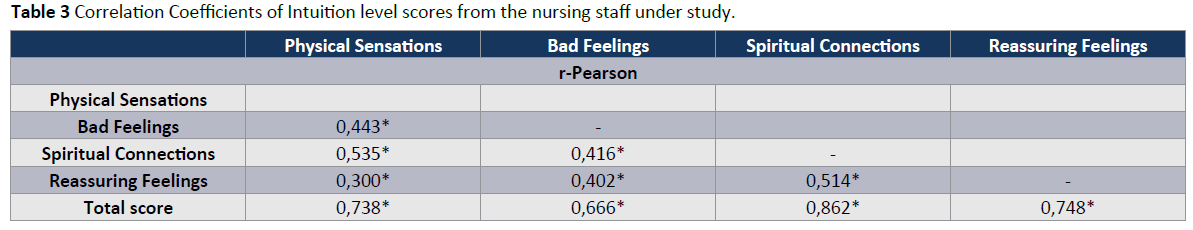
While comparing the categories above via the use of the Pearson correlation coefficient, it became obvious that all the combinations of categories showed positive correlation between them. The physical sensations and the spiritual connections mainly show higher correlation (p-value=0.535) and there may be a stronger relation between them (Table 3). Table is of dual utility since it is also a form of checking the construct validity of the questionnaire, with the correlation coefficients showing convergent validity.
On the basis of the distribution of responses to the questions of the intuition questionnaire given by the nursing staff, the findings showed that in the categories of physical sensations and spiritual connections the highest percentages of responses were “never” and “rarely” responses with the exception of the first question of the spiritual connections where the percentages of “never” and “rarely” (37%, n=45) are lower than the ones of the response “sometimes” alone (38.7%, n=47), while “sometimes” represents the highest percentage of responses (38.7%, n=47) and “rarely” the next highest one (30.3%, n=37).
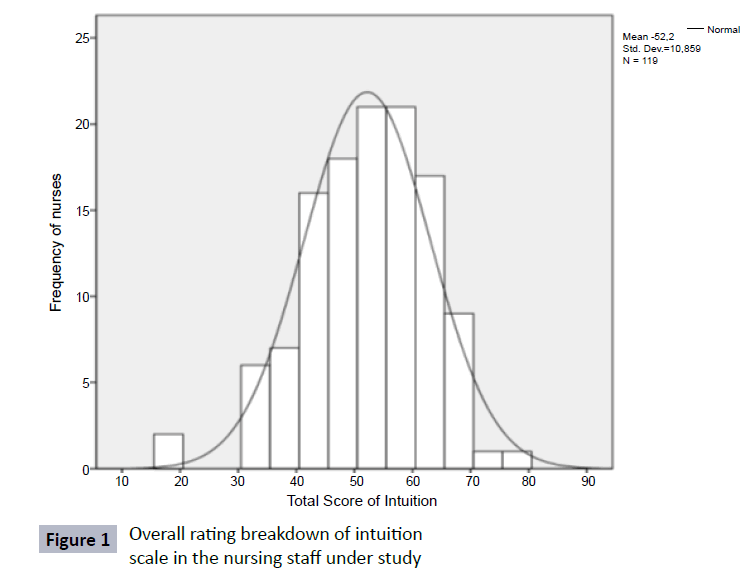
On the contrary, in the categories “bad feelings” and “reassuring feelings” the highest percentages shift towards the responses “sometimes” and “often” for “bad feelings” and towards “often” and “always” as regards the “reassuring feelings” (Table 4). On the whole, the intuition levels in the total of the nursing staff ranged at intermediate levels (mean=52.2) showing a normal distribution with a standard deviation 10.859 (Figure 1 and Table 5).
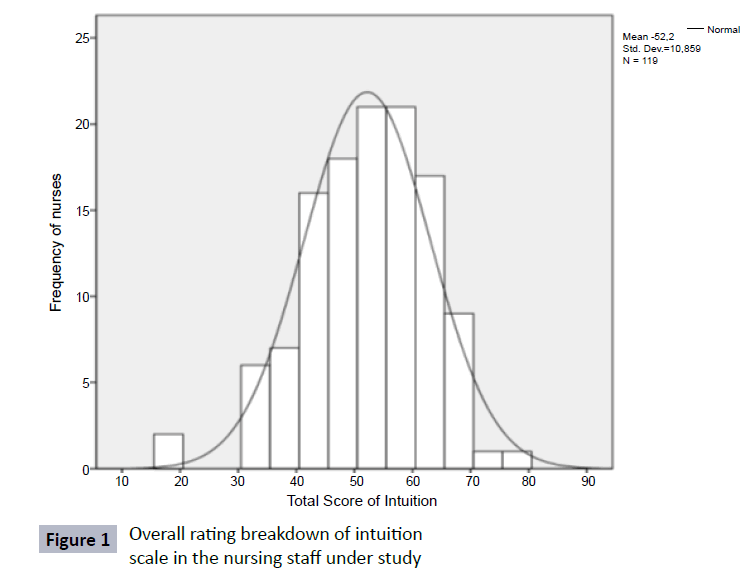
Figure 1: Overall rating breakdown of intuition scale in the nursing staff under study
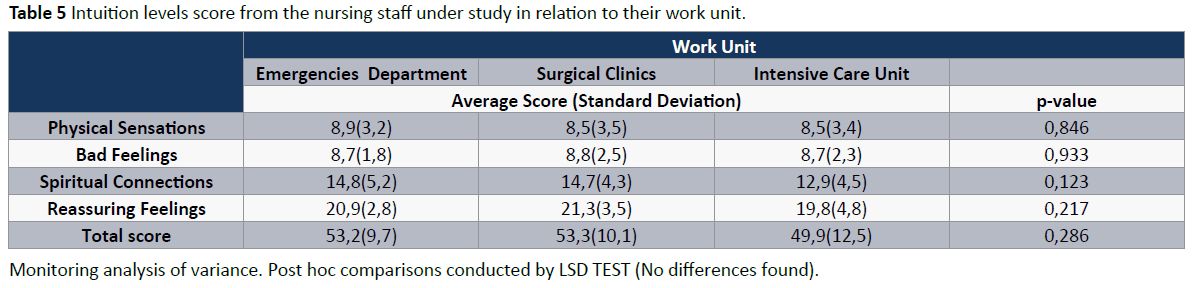
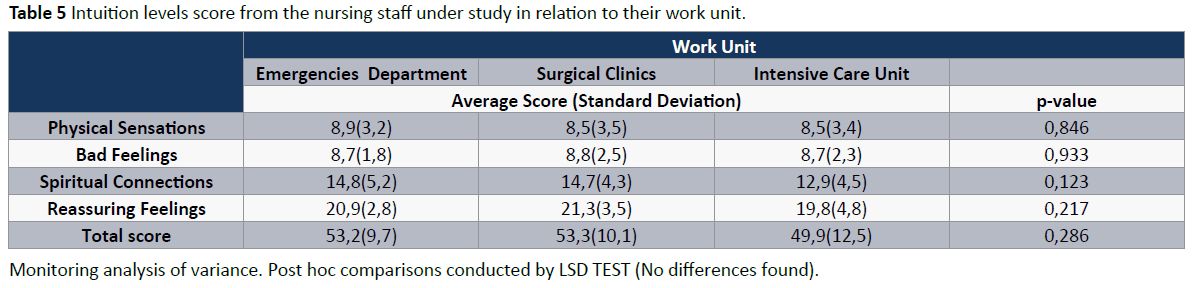
In terms of work unit of the nursing staff, the intuition scores ranged at 53.2, 53.3, and at 49.9 concerning the nursing staff in the Emergencies Department, the surgical clinics and the Intensive Care units respectively. But no statistically significant differences cropped up (Table 6).
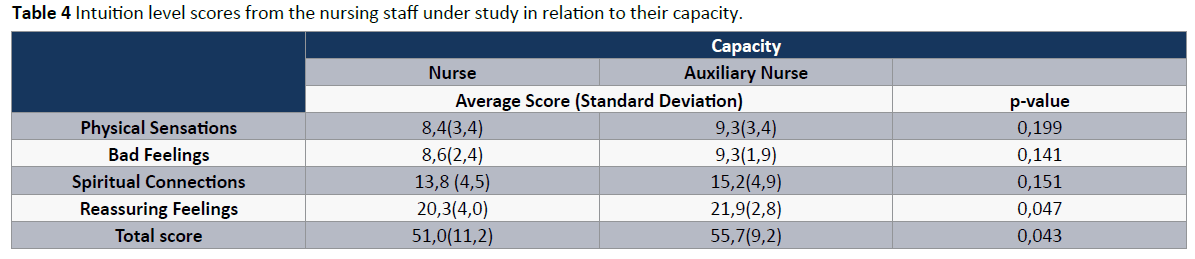
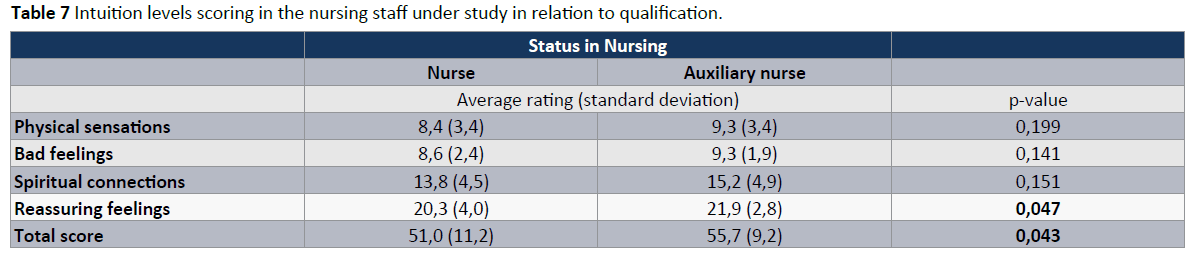
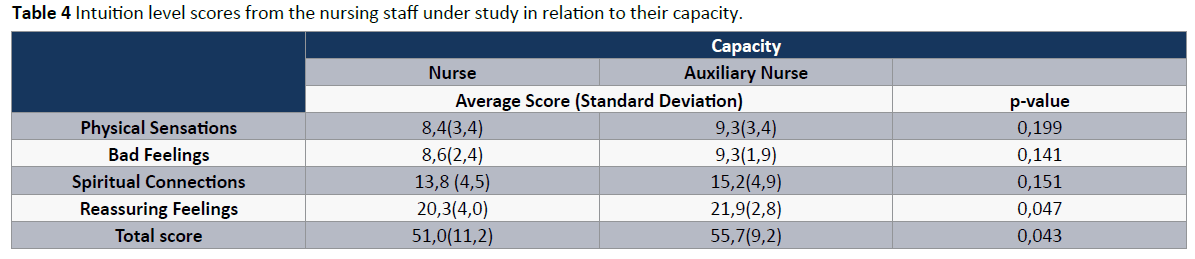
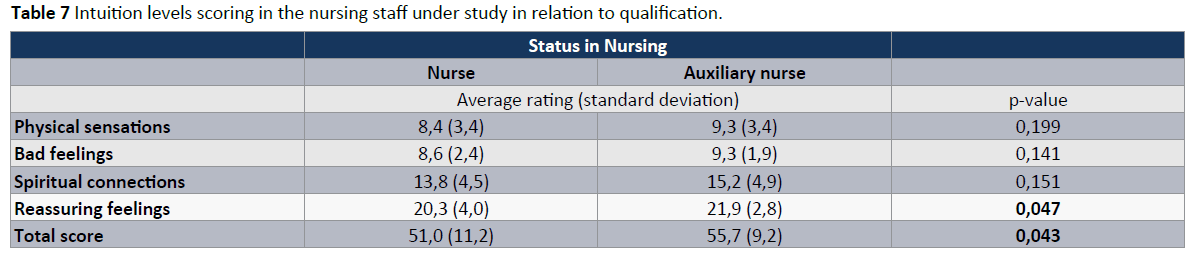
Upon correlating the categories of the questionnaire with qualification, the total intuition score was 51.0 in the nurses and 55.7 in the auxiliary nurses. Moreover, there was statistically significant difference between the overall intuition score of nurses and that of auxiliary nurses (p=0.043), the same occurring in the category of “reassuring feelings” (p=0.047) with the higher intuition scores in auxiliary nurses than in nurses (Table 7).
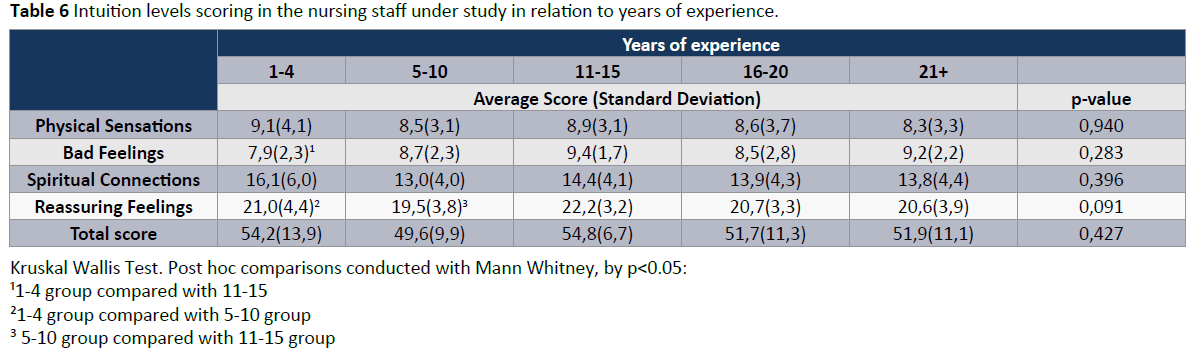
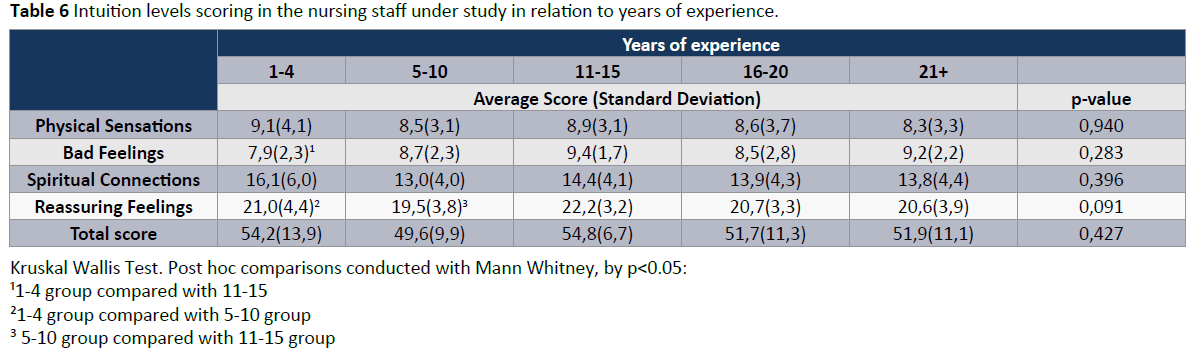
As regards work experience, the intuition scores which came up ranged between 49.6 for 5-10 years of experience and 54.8 for 11-15 years of experience. No statistically significant difference arose in the intuition scores in terms of work experience of the respondents.
Finally, as far as the correlations are concerned, the highest intuition scores were noticed in the categories of “spiritual connections” and “reassuring feelings”.
Discussion
The findings of this study showed that there is intuition at moderate levels in nursing practice of the nursing staff under study. It is worth noting that in the study in point intuition is manifested by majority in the form of feelings, positive or negative (reassuring or bad) rather than in the form of physical sensations or spiritual connections. Also, notable is the existence of positive correlation among the categories of questions in the questionnaire. Mainly it is the physical sensations and spiritual connections which produce higher correlation scores. On the contrary, there is not a significant difference between the intuition levels and years of experience. In terms of job qualification, the results showed that auxiliary nurses had higher levels of intuition than the nurses with an absolutely marginal statistical difference; however, this is a chance finding since the sampling was convenience and the auxiliary nurses made up the minority compared to the nurses.
From the study in point, it was concluded that there are considerable intuition levels in nursing practice of nurses. The current study was the first one conducted by the use of the Smith Intuition instrument for evaluation of intuition’s levels. Previous studies concerning Smith Intuition Instrument referred to the development and psychometric evaluation as well as the revision of the intuition instrument. In the international literature there is reference of a great number of studies on intuition in nursing practice which bear out the findings in point [3,11,12,16-20]
A grounded theory study was conducted in Australia with a sample of 262 registered nurses who volunteered to participate. Data were collected by focus group interviews and Delphi survey technique. The results confirmed the existence of intuition in nursing practice similarly to the current study’s results [9].
Another study, phenomenological, took place in Australia, in which 14 experienced emergency nurses accepted to provide their accounts regarding intuitive knowledge. The data analysis revealed the use of intuitive knowledge in emergency nursing which derived from feelings, syncretism and connection [21]. Adding to this study, Ian Parsonage reflects to the intuitive decision-making process by analyzing a case. Eventually, he came to the conclusion that both an analytical and an intuitive decisionmaking method should be used [22]. Furthermore, intuition as an essential part in nursing was also revealed in another study from interviewing fourteen nurses as regards to their intuitive experience [23].
Overall, in this study there was no statistically significant difference registered in the intuition levels as regards the work units and the years of experience of the nursing staff. Concerning the work units there are not any sources in literature which support this finding.
As regards the work experience and intuition levels, similar results were produced by a study conducted in the USA in a sample of 174 nurses from hospital and a domestic care unit in New York. That study is the only one with similar findings to the ones in the current study [24]. The majority of studies in international literature register statistically significant correlation of the staff’s work experience with intuition levels [3,9,11,16,21,23-25].
The current study indicates that feelings (bad and reassuring) are positively related to physical sensations. This is also supported by the theory according to which intuitive knowledge is related to both feelings and physical or behavioral reactions of a person resulted from a qualitative study by the observation and interview of 61 nurses in England [25,26].
In addition, the phenomenon of positive correlation of feelings (bad and reassuring) was in evidence this time with the creation of connections. The finding in point is partially supported by the theory mentioned above that refers to intuition as the result of interaction of feeling, comparison and connection [21]. Connection as a factor of intuition has been mentioned in a similar qualitative study which was conducted in 1987 [7].
In conclusion, mean intuition levels were observed with the work unit and the years of experience not constituting factors of differentiation of intuition levels in the nursing staff under the current study. Additionally, higher scores were observed in the categories of spiritual connections and reassuring feelings. A noteworthy fact which was also underscored by the results of this study is that nurses use intuition in daily clinical practice. On the basis of the results of the current study the following are recommended:
• The recognition and acceptance of intuition as a valid part of nursing practice from nurses so that their confidence in its implementation will increase. This will lead to the reinforcement of this phenomenon in the workplace, as well as to its appropriate use in combination with other cognitive functions leading to sound judgment during decision making.
• As regards the measurement of intuition, it is recommended that further weighing up and adjustment of the questionnaire to the Greek context be made. It is also recommended that new research instruments to measure intuition be created and weighed up.
• The research be repeated in more hospitals in Greece so that the results would be compared and intuition and its levels be further researched in nursing practice, as well as more questions raised could be answered concerning this phenomenon. Additionally, the cooperation of nurse researchers with researchers specialized in other fields could constitute a useful instrument so that broader research could be conducted which would provide a more profound understanding of the multiple dimensions of intuition in health care professionals.
• Finally, it is imperative that the teaching of intuition be integrated into nursing training so that prospective nurses would be positively sensitized to this issue when they start nursing practice.
Acknowledgement
The authors would like to thank Dr. Anita Joel Smith, associate professor in the University of Alabama for her consent to use the questionnaire “Smith Intuition Instrument” in the current research and for her valuable advices in the Greek translation and adaptation of the questionnaire in the Greek population.
6531
References
- Chaffey L, Unsworth C, Fossey E (2010) A grounded theory of intuition among occupational therapists in mental health practice. Br J OccupTher 73: 300-308.
- Hogarth R (2001) Educating Intuition; University of Chicago Press, USA.
- Rovithis M, Parissopoulos S (2005) Intuition in nursing practice. ICUs Nursing Web Journal 22.
- Smith AJ, Thurkettle MA, dela Cruz FA (2004) Use of intuition by nursing students: instrument development and testing. J AdvNurs 47: 614-622.
- Pyles SH, Stern PN (1983) Discovery of Nursing Gestalt in critical care nursing: the importance of the Gray Gorilla syndrome. Image J NursSch 15: 51-57.
- Rew L (1988) Intuition in decision-making. Image J NursSch 20: 150-154.
- Schraeder BD, Fischer DK (1987) Using intuitive knowledge in the neonatal intensive care nursery. Holist NursPract 1: 45-51.
- Rew L (1989) Intuition: nursing knowledge and the spiritual dimension of persons. Holist NursPract 3: 56-68.
- McCutcheon HH1, Pincombe J (2001) Intuition: an important tool in the practice of nursing. J AdvNurs 35: 342-348.
- Young CE (1987) Intuition and nursing process. Holist NursPract 1: 52-62.
- Smith A (2007) Measuring the use of intuition by registered nurses in clinical practice. Nurs Stand 21: 35-41.
- Correnti D (1992) Intuition and nursing practice implications for nurse educators: a review of the literature. J ContinEducNurs 23: 91-94.
- Merkouris A (2008) Methodology of Nursing Research. Ellhn Publications.
- Cioffi J (1998) Decision making by emergency nurses in triage assessments. AccidEmergNurs 6: 184-191.
- Alverzo J (2004) The use of aesthetic knowledge in the management of brain injury patients. RehabilNurs 29: 85-89.
- Benner P, Tanner C (1987) Clinical judgment: how expert nurses use intuition. Am J Nurs 87: 23-31.
- Smith AJ (2007) Embracing intuition in nursing practice. Ala Nurse 34: 16-17.
- Lyneham J, Parkinson C, Denholm C (2008) Intuition in emergency nursing: a phenomenological study. Int J NursPract 14: 101-108.
- Parsonage I (2010) Making clinical decisions in emergency situations. Emerg Nurse 18: 18-21.
- Lyneham J, Parkinson C, Denholm C (2008) Explicating Benner's concept of expert practice: intuition in emergency nursing. J AdvNurs 64: 380-387.
- Parsonage I (2010) Making clinical decisions in emergency situations. Emerg Nurse 18: 18-21.
- Handy CM (1999) Intuition, autonomy and level of clinical proficiency among registered nurses. New York University, NY.
- King L, Macleod CJ (2001) Intuition and the development of expertise in surgical ward and intensive care nurses. J AdvNur 37: 322-329.