Keywords
Family caregiver, advanced cancer, caregiver burden, time consuming/difficult tasks, radiotherapy
Introduction
Research on informal caregivers tends to focus on the extent of tasks they undertake, describing the burden experienced by caregivers. A richer conceptualization includes comprising environmental factors, including patient level of dependency, which are subjectively experienced by caregivers [1]. Carers are likely to become more distressed and develop psychiatric morbidity as the illness advances and treatment becomes palliative [2]. Grunfeld’s et al., [3] findings indicated that, although patient’s physical and emotional factors predicted caregiver distress, perceived burden is the strongest predisposing factor of caregiver anxiety and depression. Advanced cancer often requires intensive and short- or long-term palliative care, [4] which induces physical, psychological and social consequences not only for the patient, [5] but also for family members [6]. Given et al., [7] in 2001 considered caregiver burden in advanced cancer as “resulting from an imbalance of care demands relative to caregivers’ personal time, social roles, physical and emotional status, financial resources, and formal care resources given the other multiple roles they fulfil”. Most researchers agree that there are two central dimensions, objective and subjective burdens, that comprise the family burden concept [8,9]. Objective burden can be defined as ‘the time and effort required of one person to attend to the needs of another’ [10]. Burden also includes time spent in caregiving, the kind of health and caregiving services, as well the financial expenses which can have implications on the “dependent” person’s life [9,11]. Alternatively, subjective burden comprises an individual’s beliefs, assumptions, and feelings with regard to the caregiver role and is defined as the distress experienced by the caregiver in dealing the objective stressors [8]. Caregivers have the responsibility not only for their patient but at the same time they have to face the demands of their job, of household and generally all family commitments. All of them may lead to the neglect of caregivers’ needs and to a poor health condition and vulnerability for illness [12]. Often caregiving burden may be associated with managing illness-related finances, assisting with household tasks, and providing patient transportation. Moreover caregivers reported that considerable time and effort is required to provide emotional support [13].
Potential predictors of caregiver burden might be patients’ demographic, clinical and psychosocial characteristics. These may include disease severity, number and extent of caregiving tasks, as well as the level of involvement in caregiving tasks [14]. Being female, older, unemployed, with low socioeconomic status are some of the characteristics which in conjunction with disease severity can contribute to caregiver’s burden [15].
In Greece, the caregivers’ characteristics are somewhat similar with those in other western countries, but due to traditional norms, there are still strong family bonds [16]. Unfortunately, in Greece the literature about informal caregiving is very poor [16,17,18]. Therefore, the necessity for an improvement in comprehending the factors which affect the experience of caregiving burden in Greek family caregivers of patients with advanced cancer forces into an attempt to define the best ways of dealing with individual needs and consequently encourage family members in their duty as care providers.
Purpose
The present study aimed to indentify the effects of patient and caregiver demographic, clinical and psychological variables on the perceptions of family caregivers experiencing burden (time consuming tasks and difficulty of provided tasks) when caring for a patient suffering from advanced cancer in Greece.
Patients and Methods
A prospective, purposive sampling approach was followed in this study. One hundred patients who diagnosed with advanced cancer (stage IV according to the medical record) and were receiving out-patient palliative radiotherapy conducted in the study. They nominated their primary family caregiver who provided the most, unpaid care for the patient. Eligible caregivers were required to be adults (>18 years of age), with no diagnosed psychiatric disorders, and with adequate knowledge of the Greek language.
Ethical approval for the study was obtained from the Ethics Committee at the School of Nursing, University of Athens, as well as the scientific boards for each hospital. The investigator provided patients with study information material to read and consider participation. Their family caregivers followed similar consent procedures. Data collection was conducted through interviews with all dyads during the patient’s appointment at the clinic.
Data was collected by the completion of a specially design questionnaire which included sociodemographic variables for the patients and caregivers, as well as clinical variables for the patients. Patients completed two questionnaires (The Hospital Anxiety and Depression Scale-Greek version and the MD Anderson Symptom Inventory-Greek version), and caregivers completed two questionnaires too (The Oberst Caregiving Burden Scale-Time and Difficulty, and the Hospital Anxiety and Depression Scale-Greek version).
The Oberst Caregiving Burden Scale (OCBS) is a 15-item questionnaire that was used to assess caregiver perceptions of the difficulty of caregiving tasks (OCBS-D) and time required in caring for their ill family member (OCBS-T) [13]. Such caring tasks including providing personal care and medical care, assisting with activities of daily living, monitoring symptoms, managing patient’s emotion and behaviours, dealing with finances, and coordinating and seeking health services. The difficulty of caregiving task measure was rated on a 5-point Likert scale from 1 (not difficult) to 5 (extremely difficult). Time spent on caregiving tasks was rated on a 5-point Likert scale from 1 (none) to 5 (a great amount of time). A total score is used and is the sum of 15 items. Higher scores indicate great task difficulty and more time spent on each task [19]. In this study, the Cronbach's alpha coefficient was 0.87 for OCBS-D and 0.83 for OCBS-T. According to current guidelines, two independent translators translated the OCBS into the Greek language and then another two independent translators translated it back into English. Then, these translations were matched.
Caregivers and patients were asked to complete The Hospital Anxiety and Depression Scale- Greek version (G-HADS). It is a self-assessment mood scale specifically designed for use in the hospital setting [20]. The HADS has been standardised, adapted and validated for use with Greek patients with cancer [21]. It is a brief self-report 14-item scale designed to measure the two most common aspects of mood disorder (i.e. anxiety and depression) on a 0-3 verbal numerical scale. Two subscale scores can be yielded, one for depression (G-HADS-D) and one for anxiety (G-HADS-A). Cronbach’s alphas in the present study were 0.77 for G-HADS-D and 0.86 for G-HADS-A.
Patients were asked to complete M. D. Anderson Symptom Inventory – Greek version (G-MDASI). The MDASI is a 15-item questionnaire that facilitates a brief assessment of the severity and impact of cancer-related symptoms [22]. Each symptom is rated on an 11-point scale (0-10) to indicate the presence and severity of the symptom with 0 meaning ‘not present’ and 10 meaning ‘as bad as you can imagine’ in the last 24 hours. It also includes 6 symptoms interference items that are rated based on the level of symptom interference with the function of a patient’s life in the last 24 hours, and also measured on an 11-point scale (0=‘did not interfere’ to 10=‘interfered completely’). The MDASI has been standardized and validated in a sample of Greek patients with advanced cancer (G-MDASI) as a useful measure of symptom distress and severity [23]. In this study, the Cronbach's alpha coefficient was 0.83 (severity and impact of cancer-related symptoms) and 0.85 (symptom interference with the function).
Statistical analysis
Basic descriptive statistics were computed for the sociodemographic variables, as well as means, standard deviations and ranges for continuous variables and percentages for categorical data. The Kolmogorov-Smirnov test was utilised to examine normality of continuous and interval-scale variables. Univariate analyses were conducted through use of independent samples t-tests, one-way analysis of variance (ANOVA) and Pearson’s r correlation coefficients to explore the relationships between the outcome variable (OCBS total score) and predictor variables. All predictors that were significantly associated with the outcome variable in univariate analysis were included in a multiple linear regression model, using the stepwise method to arrive at the final model and determine a multivariate summary model of determinants of outcome variable. All assumptions of linear regression analysis (homoscedasticity, linearity, normality and independence of error terms, as well as multicollinearity of independent variables using the variance inflation factor (VIF) of Tolerance were examined. A p-value of <0.05 (two-sided) was used to denote statistical significance. All analyses were carried out using the statistical package SPSS v. 16 (Statistical Package for the Social Sciences, SPSS Inc., Chicago, Ill., USA).
Results
Descriptive statistics
One hundred and sixty patients included firstly in the study and their nominated primary family caregivers. Twenty-five patients were unable to identify a caregiver or were unable to participate in the study due to low performance status, while 35 caregivers refused to participate due to lack of interest, perceived psychological distress, or fear for patient strain. In final analyses were included only consenting patient-caregiver dyads. Thus, the final sample consisted of 100 dyads (62.5% of eligible patients and caregivers).
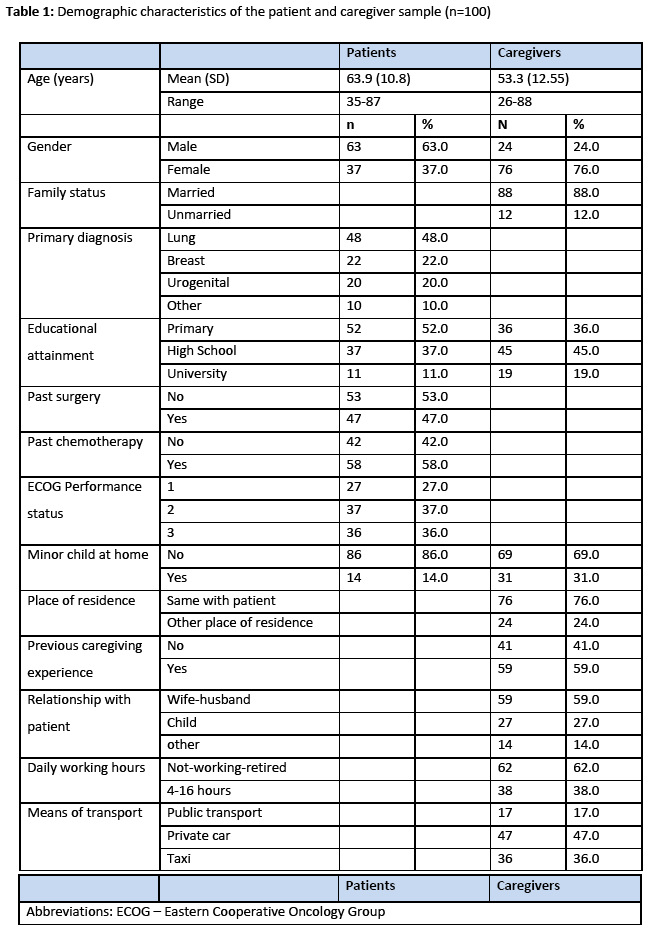
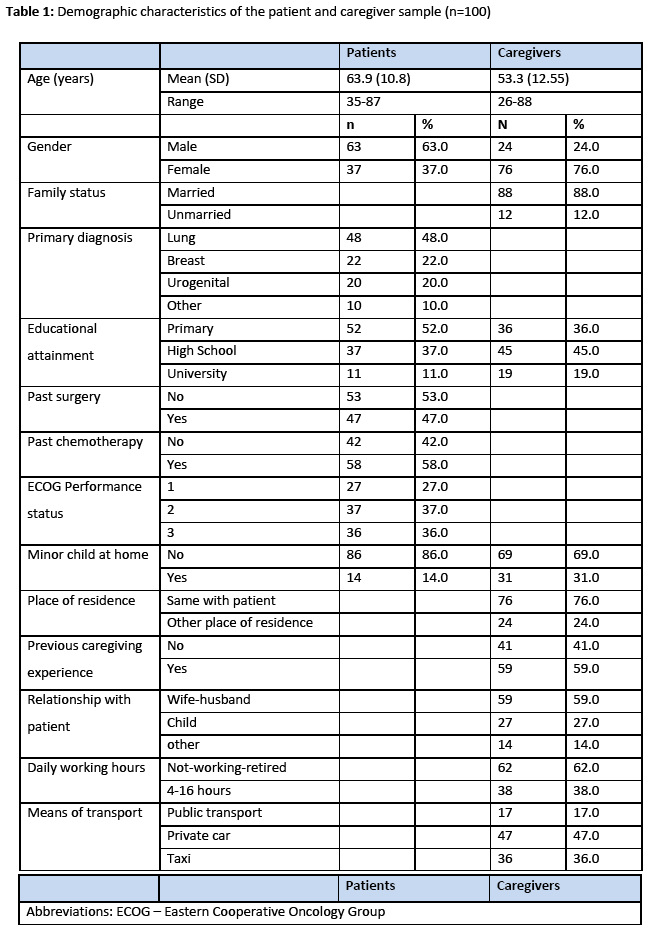
Patient and caregiver demographic characteristics and patient clinical characteristics are outlined in Table 1. The mean age of the patients was 63.9 years (SD=10.81, range 35-87) and the mean age of the caregivers was 53.3 years (SD=12.55, range 26-88). Of the 100 patients, the majority was male (63%) and of the 100 caregivers, the majority was female (76%). The typical caregiver was married, had high school education, lived in the same household as the patient, had care experience, was spouse, did not work or was retired and moved to and from the hospital by private car. Regarding patients’ disease stage, all of the patients were diagnosed with stage ΙV cancer.
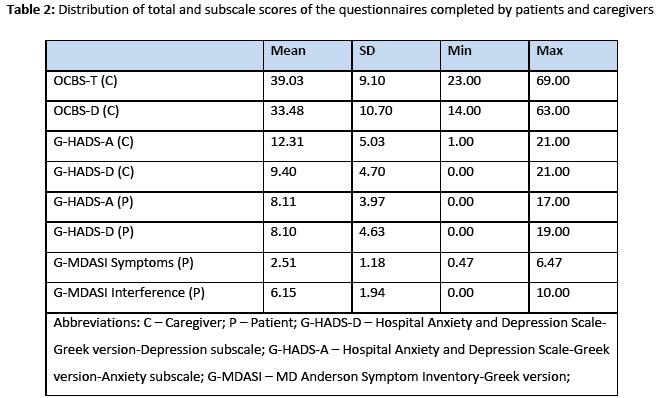
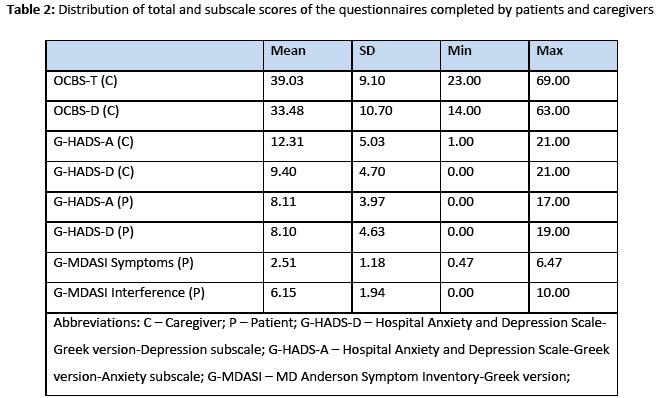
Means, standard deviations and range for OBCS, HAD and MDASI Symptoms and Interference are shown in Table 2.
Univariate analyses
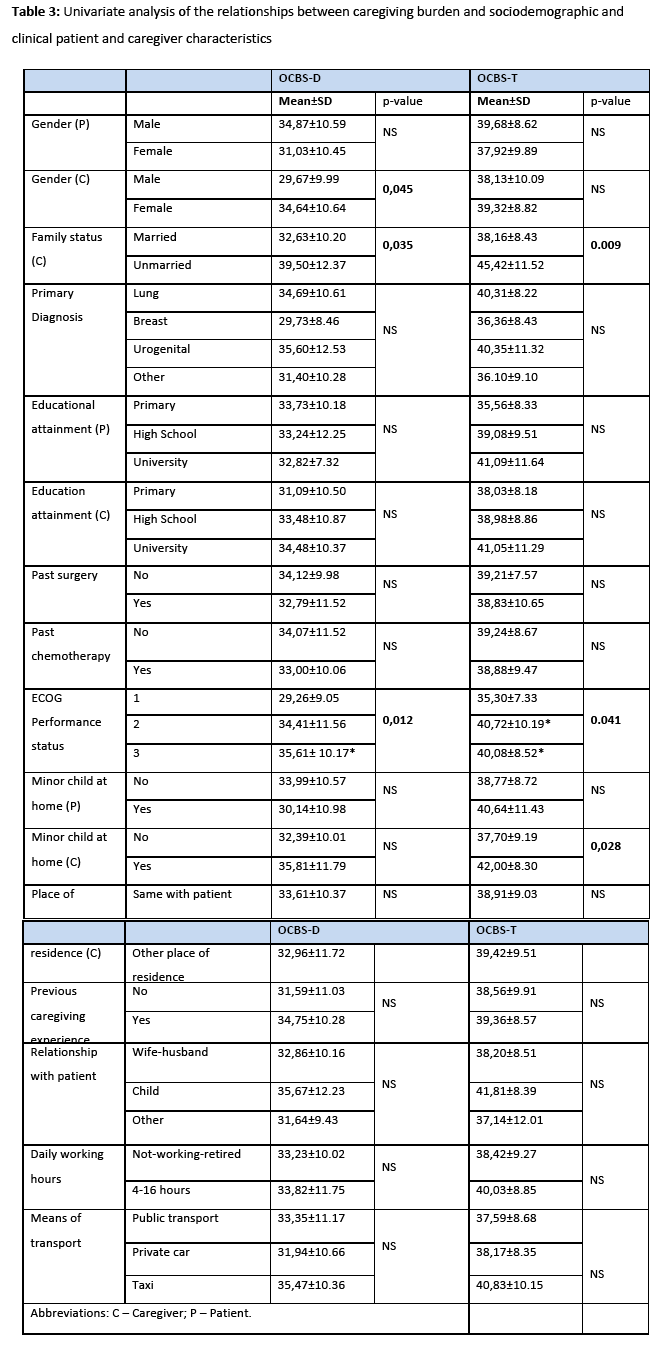
Results indicated some statistically significant associations between OCBS-T and the categorical predictors. Unmarried caregivers (p<0.009), and those with minor child (p=0.028), mentioned more perceived time spent or difficulty with caregiving tasks, compared to their respective counterparts. Moreover, caregivers of patients with ECOG score 2 and 3 reported greater burden than those who cared for a patient with ECOG score 1 (p=0.041) (Τable 3). Concerning the relationship between caregiver burden (OBCS-T) and caregivers’ continuous/interval-scale predictors, statistically significant moderate correlations were found between time required for caregiving tasks and age (r=-0.300; p=0.003), time required for caregiving tasks and anxiety (G-HADS-A, r=-0.386; p<0.001), as well as time required for caregiving tasks and depression (G-HADS-D, r=-0.303; p=0.002). Moreover, statistically significant moderate correlation was found between caregiver burden (OBCS-T) and patients’ symptoms (MDASI-Symptoms, r=0.302; p=0.002), and statistically significant weak correlation was found between caregiver burden (OBCS-T) and perceptions of greater symptom interference (MDASI-Interference, r=0.238; p=0.017).
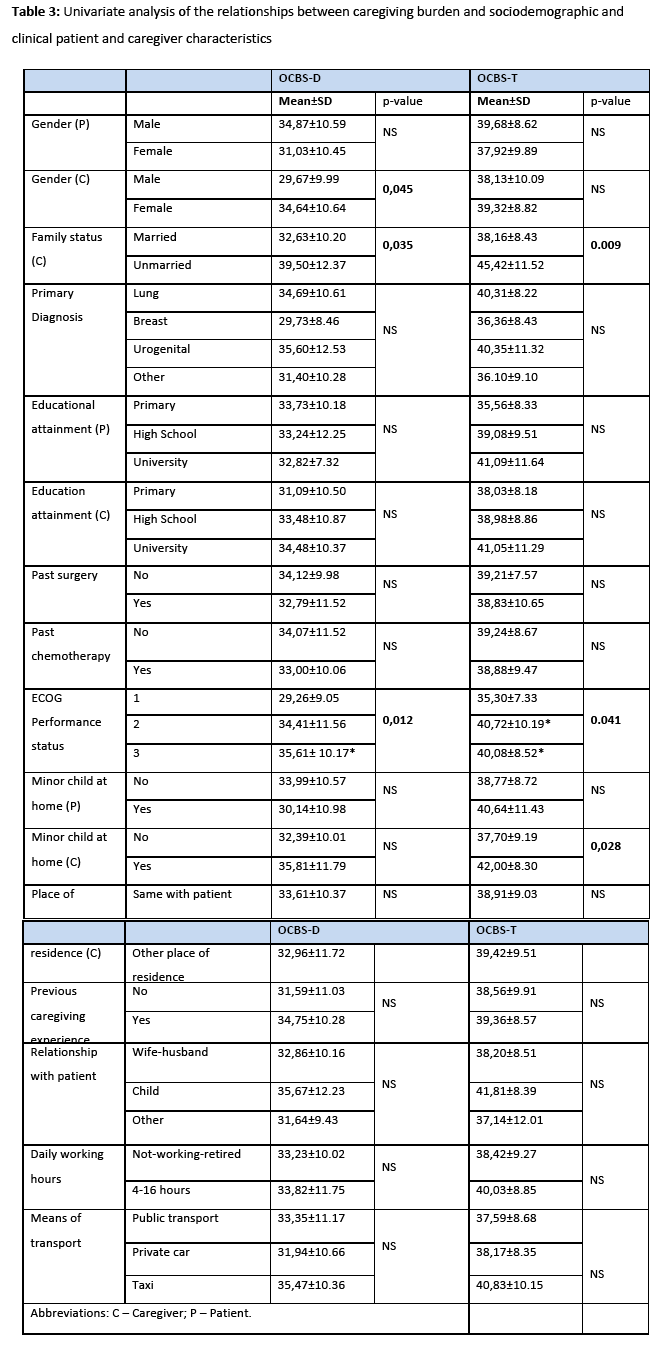
Similarly, results indicated some statistically significant associations between OCBS-D and the categorical predictors. Female caregivers (p=0.045), and married (p=0.035), mentioned statistically significant more care difficulties compared to their respective counterparts. Caregivers of patients with ECOG score 3 reported greater burden than those who cared for a patient with ECOG score 1 or 2 (p=0.012) (Τable 3). Concerning the relationship between burden (OBCS-D) and continuous/interval-scale caregiver’s predictors, statistically significant moderate correlations were found between perceived difficulty during the patient’ care and anxiety (G-HADS-A, r=-0.470; p<0.001), as well as perceived difficulty during the patient’ care and depression (G-HADS-D, r=0.476; p<0.001). When correlations between caregiver burden (OBCS-D) and patient psychosocial variables were examined, three weak-to-moderate correlations were found: patients’ anxiety (G-HADS-A, r=0.242; p=0.016), patients’ symptoms (MDASI-Symptoms, r=0.288; p=0.004), and patients’ perceptions of greater symptom interference (MDASI-Interference, r=0.331; p=0.001), all associated with greater caregiver burden.
Multivariate analyses
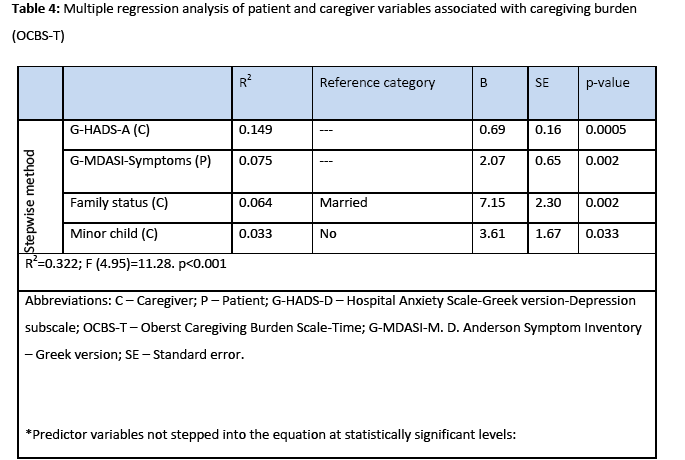
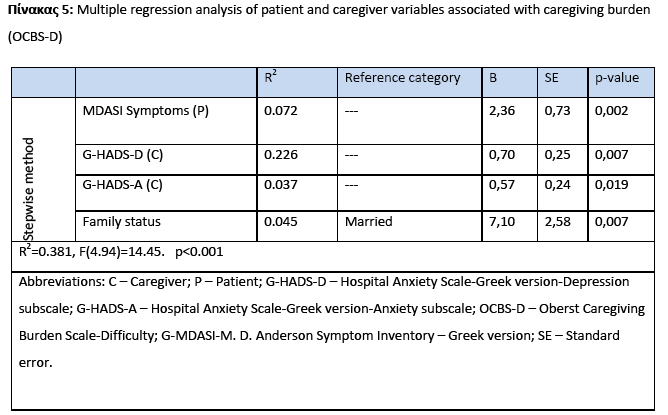
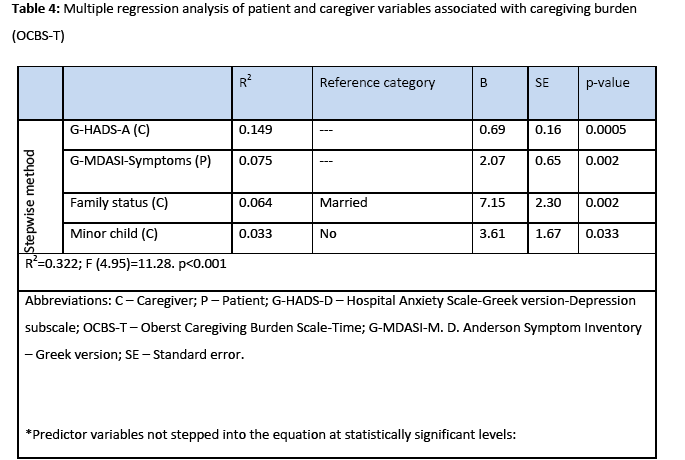
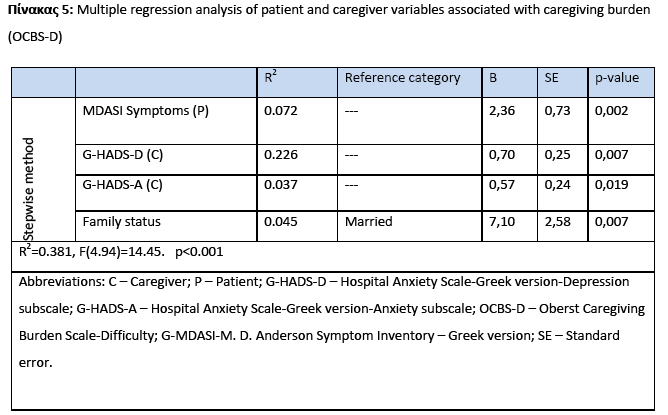
In multiple regression analyses, the stepwise method was used in order to examine which of the variables from the univariate analyses could act as the strongest predictors of caregivers’ burden. Results demonstrated that 32.2% of the variance (R2) in predicting caregiving burden-Time (OCBS-T) was accounted for by ‘caregiver anxiety’ (B=0.69, p<0.001), ‘MDASI-Symptoms’ (B=2.07, p=0.002), ‘caregiver family status’ (B=7.15, p=0.002), and ‘caregiver minor child’ (B=3.61. p=0.033). These predictors were retained in the final model (Table 4). Similarly, 38.1 of the variance (R2) in predicting caregiving burden-Difficulty (OCBS-D) was accounted for by ‘caregiver depression’ (B=0.70, p=0.007), ‘caregiver anxiety’ (B=0.57, p=0.019) ‘MDASI-Symptoms’ (B=2.36, p=0.002), and ‘caregiver family status’ (B=7.10, p=0.007) (Table 5).
Discussion
Caregivers often face difficult and time consuming tasks required for the care of cancer patients in a home setting. Cancer patients’ care is described as a tiresome process that requires a lot of time and energy, sometimes for months or for years [24]. Caregiving is a difficult situation and in combination with the difficult process of cancer management can have a major impact on a caregiver’s life [25] The current study investigated the effects of both caregiver (sociodemographic characteristics and mood disorders) and patient factors (sociodemographic and clinical characteristics, anxiety and depression, severity and interference of symptoms of advanced cancer) on perceived caregiving burden regarding difficult and time-consuming tasks in a convenience sample of Greek family members caring for patients with advanced cancer in a home setting.
In the present study, caregivers’ depression was the most important predictor of burden. This finding is consistent with other studies describing high levels of psychological morbidity in this group of informal caregivers [1,26]. Similarly Papastavrou et al., [16] found strong correlations of depression with perceived burden among caregivers of patients with cancer. There are also findings which emphasize on the fact that anxiety levels are increased in daughters of patients with cancer, as well as caregivers of patients with dementia [27,28]. Some researchers argued that burden is equal to depression [24,29]. Grunfeld’s et al.,3 claimed that, although patient’s physical and emotional factors predicted caregiver distress, perceived burden is the strongest predictor of caregiver anxiety and depression.
Univariate and multivariate analyses showed that patient symptom, functional status and depressive mood can influence the perception of burden. Burden and depressed mood probably are based in predictors of burden reported consistently in the literature, including the caregiver gender, the patient symptom status, and the patient functional status. The patients declining health status definitely influences the caregiver’s reactions, especially at the patients’ transition to the more severe illness’ stages [3,30,34]. In a Greek study, examining the psychological status of Greek cancer patient’ caregivers, it was found that depression and anxiety as well as low quality of life was prominent [18].
Severity of patient’s symptoms can be the cause of reactions such as irritability, frustration and depression [31]. Evidence of patient dependency should be a definite warning sigh for healthcare professionals to caregivers involved [13]. There are studies, in which the patients’ prognosis, metastatic disease and the presence of severe cancer related symptoms were found to be linked to a greater degree of burden to caregivers [15,32]. Depression of the patient is related to caregiver’s distress and behavioural changes [33]. In a Greek study, patient’s symptoms were not found to be associated with the caregiver’s burden [18].
Univariate analyses showed statistically significant associations between caregiver burden and caregiver gender, family status, and age.
Female caregivers perceived their caregiving role as more burdensome, confirming existing findings [16,34]. This preponderance may be related to the cultural “norm” requiring females to be the most devoted to family member’s care. Moreover, the negative impact of care is shown to be higher in married than non-married caregivers, which is in agreement with existing evidence supporting that spouses are the busiest group of caregivers [35]. Also, the present study showed a negative correlation between burden and caregiver’s age. Older people experienced less burden than younger, although adult caregivers experience physical vulnerability caused by ageing. However, results are inconsistent. Between several previous studies, younger caregivers mentioned more burden than the older and vice versa [36,37].
The multiple regression analysis revealed that caregivers with minor child were more burdened (perceived the caregiving tasks as time consuming) compared to their respective counterparts. Similarly, in relevant literature, caregivers with caring responsibilities to minor child are most likely to feel distressed [38].
There are several important limitations in this study. The sample was restricted to outpatients receiving palliative radiotherapy and consisted of patients with diverse primary diagnoses. In relevant literature, most studies use input of family carergivers of hospitalised patients with advanced cancer or patients receiving different types of care. Moreover, the heterogeneity of the primary diagnosis of the study sample inhibits the ability for generalization.
It is generally considered that additional variables, as the duration of illness, the intensive care, and the quality of relationship among the involved persons can also cause burden and emotional distress. Finally it is acknowledgeable the fact that the study population may not be entirely representative of the total population of family caregivers of patients with advanced cancer in Greece.
Conclusions
In the present study, Greek family caregivers who reported higher difficulty with the caregiving tasks were women, those unmarried, those with greater psychological morbidity and those who cared for patients with poor performance status, severe symptoms and higher score of anxiety. Moreover, Greek family caregivers who reported higher time consuming with the caregiving tasks were unmarried caregivers, younger, those with minor child, those with greater psychological morbidity and those who cared for patients with severe symptoms and poor performance status.
Factors that may predict caregivers’ burden need further to be examined in order to clarify the notion of caregiver’s response to severe illnesses states of beloved persons. Expectations from patients’ families are generally greater in the context of a National Health System such as the Greek one, in which only a few dedicated plans exist, such as in-home health care services and only in a very limited form.
2631
References
- Zapart S, Kenny P, Hall J, Servis B, Wiley S. Home-based palliative care in Sydney, Australia: the care’s perspective on the provision of informal care. Health and Social Care in the Community 2007;15(2):97-107.
- Pitceathly C, Maguire P. The psychological impact of cancer on patients' partners and other key relatives. European Journal of Cancer 2003;39(11):1517-24.
- Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle, C.C, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ 2004;170(12):1795-1801.
- Nijboer C, Tempelaar R, Sanderman R, Triemstra M, Spruijt RJ, van den Bos GA. Cancer and caregiving: The impact on the caregiver’s health. Psycho oncology 1998;7:3-13.
- McLean L.M, Jones J.M. A review of distress and its management in couples facing end-of-life cancer. Psychooncology 2007;16(7):603-616.
- Thomas C, Morris S.M. Informal carers in cancer contexts. Eur J Cancer Care 2002;11(3):178-182.
- Given B.A, Given C.W, Kozachik S. Family support in advanced cancer. CA Cancer J Clin 2001;51(4):213-231.
- Montgomery RJV, Goneya JG, Hooyman NR. Caregiving and the experience of subjective and objective burden. Family Relations 1985;34:19-26.
- Sales E. Family burden and quality of life. Quality of life research 2003;12:33-41.
- Kahana E, Biegel D, Wykle M. Family Caregiving Across Lifespan. Eds., Sage Publications, California, 1994.
- Van Houtven C.H, Ramsey S.D, Hornbrook M.C, Atienza A.A, van Ryn M. Economic burden for informal caregivers of lung and colorectal cancer patients. Oncologist 2010;15(8):883-893.
- Mazanec S.R, Daly B.J, Douglas S.L, Lipson A.R. Work productivity and health of informal caregivers of persons with advanced cancer. Res Nurs Health 2011;34(6): 483-495.
- Carey P.J, Oberst M.T, McCubbin M.A, Hughes, S.H. Appraisal and caregiving burden in family members caring for patients receiving chemotherapy. Oncol Nurs Forum 1991;18(8):1341-1348.
- Kotronoulas G, Wengström Y, Kearney N. Informal carers: A focus on the real caregivers of people with cancer. Forum Clin Oncol 2012;3:58-65.
- Chou K.R. Caregiver burden: A concept analysis. J Pediatr Nurs 2000;15(6):398-407.
- Papastavrou E, Charalambous A, Tsangari H. Exploring the other side of cancer care: the informal caregiver. Eur J Oncol Nurs 2009;13(2):128-136.
- Iconomou G, Vagenakis A.G, Kalofonos H.P. The informational needs, satisfaction with communication, and psychological status of primary caregivers of cancer patients receiving chemotherapy. Support Care Cancer 2001a;9(8):591-596.
- Iconomou G, Viha A, Kalofonos H.P, Kardamakis D. Impact of cancer on primary caregivers of patients receiving radiation therapy. Acta Oncol 2001b;40(6):766-771.
- Bakas T, Champion V, Perkins S, Farran C, Williams L. Psychometric Testing of the Revised 15-item Caregiving Outcomes Scale. Nursing Research 2006;55(5):346-355.
- Zigmond A.S, Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-370.
- Mystakidou K, Tsilika E, Parpa E, Katsouda E, Galanos A, Vlahos L. The Hospital Anxiety and Depression Scale in Greek cancer patients: psychometric analyses and applicability. Support Care Cancer 2004b;12(12):821-825.
- Cleeland C.S, Mendoza T.R, Wang X.S, Chou C, Harle M.T, Morrissey M, et al, Assessing symptom distress in cancer patients. Cancer 2000;9(8):1634-1646.
- Mystakidou K, Cleeland C, Tsilika E, Katsouda E, Primikiri A, Parpa E, et al. Greek MD Anderson Symptom Inventory: Validation and utility in cancer patients. Oncology 2004a;67(3-4):203-210.
- Tang S.T, Liu T.W, Tsai C.M, Wang C.H, Chang G.C, Liu L.N. Patient awareness of prognosis, patient–family caregiver congruence on the preferred place of death, and caregiving burden of families contribute to the quality of life for terminally ill cancer patients in Taiwan. Psycho-Oncology 2008;17(12):1202-1209.
- Deeken J.F, Taylor K.L, Mangan P, Yabroff K.R, Ingham J.M. Care for the caregivers: a review of self-report instruments developed to measure the burden, needs, and quality of life of informal caregivers. J Pain Symptom Manage 2003; 26 (4):922-953.
- Harding R, Higginson I, Donaldson. The relationship between patient characteristics and carer psychological status in home palliative cancer care. Support Care Cancer 2003;11(10):638-43.
- Raveis V.H, Karus D, Pretter S. Correlates of anxiety among adult daughter caregivers to a parent with cancer. Journal of Psychosomatic Oncology 1999;17:1-26.
- Chapell N.L, Penning M. Behavioural problems and distress among caregivers of people with dementia. Ageing Society 1996;16:57-73.
- Sherwood P.R, Given B.A, Given C.W, Schiffman R.F, Murman D.L. Lovely M, et al. Predictors of distress in caregivers of persons with a primary malignant brain tumor. Research in nursing & health 2006;29(2):105-120.
- Kim H, Chang M, Rose K, Kim S. Predictors of caregiver burden in caregivers of individuals with dementia. Journal of Advanced Nursing 2011;68(4):846-855.
- Given B, Given C.W. Family caregiver burden from cancer care. In McCorkle, R., Grant, M, Frank, M, Stromborg, M., Baird, S. (Eds.). Cancer Nursing: A comprehensive textbook. Saunders, Philadelphia, 1995.
- Palos G.R, Mendoza T.R, Liao K.P, Anderson K.O, Garcia‐Gonzalez A, Hahn K, et al. Caregiver symptom burden: the risk of caring for an underserved patient with advanced cancer. Cancer 2011;117(5):1070-1079.
- Mourik J, Rosso S, Niermeijer M, Duivenvoorden H, Van Swieten J, Tibben A. Frontotemporal dementia: behavioral symptoms and caregiver distress. Dementia and geriatric cognitive disorders 2004;18(3-4):299-306.
- Rinaldi P, Spazzafumo R, Mastriforti R. Mattioli P. Marvardi M. Polidori M. C. et al. Predictors of high level of burden and distress in caregivers of demented patients: results of an Italian multicenter study.International Journal of Geriatric Psychiatry 2005;20(2):168-174.
- Vellone E, Sansoni J, Cohen M.Z. The experience of Italians caring for family members with Alzheimer's disease. Journal of Nursing Scholarship 2002;34(4):323-329.
- Goldstein N, Concato J, Fried T, Cherlin E, Kasl S, Bradley E. Factors associated with caregiver burden among caregivers of patients with cancer in a hospice setting. Journal of Clinical Epidemiology 2002;55: 628.
- Serrano-Aguilar P.G., Lopez-Bastida J., Yanes-Lopez V. Impact on health-related quality of life and perceived burden of informal caregivers of individuals with Alzheimer’s disease. Neuroepidemiology 2006;27(3):136–142.
- Whitlatch C.J., Noelker L.S. Caregiving and Caring. The Margaret Blenkner Research Institute, Cleveland OH, USA, 2007.