Keywords
Environmental tobacco smoking; Female smokers; Smoking prevention initiative
Introduction
Environmental tobacco smoke (ETS) is breathing other people smoke and its inhalation is an unavoidable risk when being in a smoke-filled environment [1,2]. The volatilized gaseous elements of smoke particles are known to be precipitated on surfaces, including the human lungs [3]. The United States of America (USA) National Toxicology Program estimates that at least 250 chemicals in ETS are known to be toxic or carcinogenic [4]. In adults, studies showed that exposure to ETS has been associated with heart diseases and lung cancer in nonsmokers [1-3]. In children, it has been linked to sudden infant death syndrome, acute respiratory infections, ear infections, worsening of asthma symptoms and other health conditions [1-3].
According to the World Health Organization (WHO) 2013 reports, the tobacco epidemic is one of the biggest public health threats in Palestine [5]. Worldwide, tobacco smoking is estimated to be responsible for nearly six million deaths per year and more than 600 000 of these deaths are among nonsmokers who usually exposed to ETS [5]. The WHO supports most countries in the world in implementing the provisions of the WHO Framework Convention on Tobacco Control. The Convention represents a milestone for the promotion of public health and provides new legal dimensions for international health cooperation [5].
Different studies had shown significant adverse effects of ETS in adults and children [6]. A smoking-related behavior and attitudes survey in the United Kingdom (UK), reported high level of knowledge about the impact of ETS (92% of adults were aware that exposure to ETS increases a child’s risk of chest infections and 86% were aware of an increased risk of asthma) [7]. Prenatal exposure to tobacco smoke has significant adverse impacts on the health of the fetus including low birth weight, premature birth, spontaneous abortion and still birth [8,9]. Furthermore, prenatal exposure can have adverse impacts on the learning and behavioral development of a child. Maternal prenatal smoking is associated with both antisocial behavior and attention deficit hyperactivity disorder in children and adolescents [10]. In the UK, it has been reported that around 40% of people with asthma reported that triggers at workplace settings make their asthma worsened and 38% of those, considered ETS exposure as the trigger. Therefore, reducing exposure to ETS in the workplaces has been found as a key solution to reduce workplace asthma [11].
According to the Palestinian Central Bureau of statistics, the percentage of individuals aged 18 years and above that reported as smokers in the State of Palestine was about 22 % [12]. However, no data is available regarding ETS exposure. Females are vulnerable group to ETS compared to males [13-15]. Indeed, due to gender culture that is linked to social inequalities in the Middle East, females could be on higher exposure rates to ETS in the households [5]. We aimed to evaluate the ETS exposure among females working in academic institutions applied An-Najah National University (the largest Palestinian university located in the Northern West Bank) as the study setting and model.
Materials and Methods
Study design, setting and population
We conducted a quantitative cross-sectional study. The study population was the non-smokers Palestinian females who currently employed in an academic institution in the Northern part of the West Bank (An-Najah National University) since at least one year regarding the ETS exposure.
Sample size
Recruitment of participants has been chosen from the nonsmokers females working since at least one year at An-Najah National University (the old and new campus) using a convenient sampling technique. We were able to recruit twohundred and two non-smokers females. Given 95% confidence level and 5% allowable error with an expectation of exposure rate to ETS among participants not less than 40% [16,17], this sample size is usually considered sufficient.
Data collection
All data required for this study was collected using a previously standardized and validated questionnaire [18-21] using a face-to-face structured interview. The researchers were filling the questionnaire after asking the subjects to ensure validity and no missing data. All researchers were trained together on the questionnaire and how to deliver the questions in the same manner. In order to maximize the sample size and ensure the presence of the employees in their office and not to interrupt their work, interviews had been started from 12 P.M and forward. The usual academic daily working hours in Palestine are from 8 A.M to 3.5 P.M without an official pause in-between and the lunch is usually taken on the working desk. The questionnaire contains different parts of measurements including knowledge, attitudes and avoidance behavior toward the ETS exposure.
Ethical and administrative considerations
The study was approved by the Institutional Review Board (IRB) at An-Najah national University and permission to conduct the study was taken from the administrative authorities at the university. Participation was voluntary after explanation of the study objectives to the participants ensuring the anonymity and confidentiality of each participants information with optional withdrawal at any time from the study. A written informed consent was obtained from each participant.
Data analysis
In the analysis, the four and five points likert-type responses scales were merged so that at the end three mutually exclusive scales were created from the original scales (examples: strongly agree/agree were merged as agree and almost always true/usually true were merged as true). This was conducted due to low numbers of respondents (less than 5 and sometimes zero) in some of these categories. We believe that these new and simple classifications usually quantify the responses in a clear and direct way of thinking especially in such judgment of responses that don’t have standard cut-off points.
All data was entered and analyzed using the Statistical Package for Social Sciences (SPSS) software program version 16 [22]. P-value less than 0.05 was always considered statistically significant. Chi-Square test was used to highlight differences among categorical variables. Due to lack of normality, Mann- Whitney U test and Kruskal’s-Wallis test were used.
Results
General characteristics and self-reported exposure to ETS
As shown in Table 1, nearly 70% of the study participants were between the ages of 20 to 40 years old. About 106 participants (52.5% of the total) reported living in homes with either a smoker husband and/or member family. Of the 106, 52.8% reported exposure to ETS six to seven days per week (mean exposure days per week was 5 days with a standard deviation; SD of 2.6 days).
| Variable |
n (%) |
| Age (years) |
| 20-30 |
68(33.7) |
| 31-40 |
74(36.6) |
| 41-50 |
52(25.7) |
| > 50 |
8(4.0) |
| Educational level |
| College school |
102 (50.5) |
| Graduate School |
100 (49.5) |
| Time spent at work |
| Primarily indoors |
148 (73.3) |
| Primarily outdoors |
4(2.0) |
| Both indoors and outdoors |
50(24.8) |
| Do you have a smoking policy at workplace |
| Yes |
174 (86.1) |
| No |
18 (8.9) |
| Don’t know/not sure |
10 (5.0) |
| Living with a smoking husband and/or family member |
| Yes |
106 (52.5) |
| No |
96(47.5) |
| Kind of tobacco that participant family members smoke the most* |
| Cigarette with filter |
30(28.3) |
| Cigarette without filter |
34(32.1) |
| Hand-rolled tobacco |
6(5.7) |
| Tobacco pipe with or withoutwater |
12(11.3) |
| Other (many kinds) |
20(18.9) |
| Don’t know / Not sure |
4(3.8) |
| Participants’ days per week exposure to ETS * |
| One |
14(13.2) |
| Two-three |
16(15.1) |
| Four-five |
20(18.9) |
| = Six |
56(52.8) |
*Analysis out of 106 respondents who answered yes to “living with a smoking husband and/or family member”. ETS: Environmental tobacco smoke.
Table 1: General characteristics and self-reported exposure to ETS (N=202).
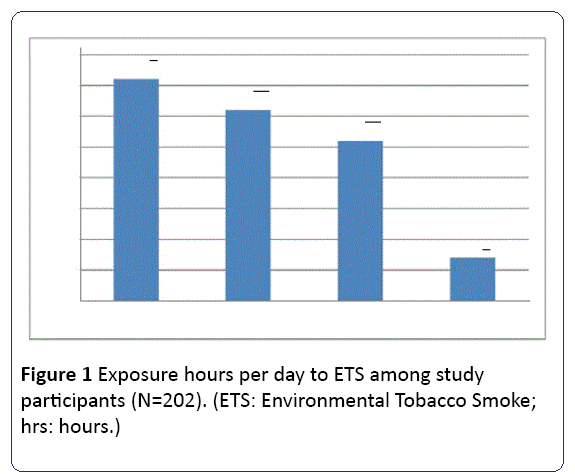
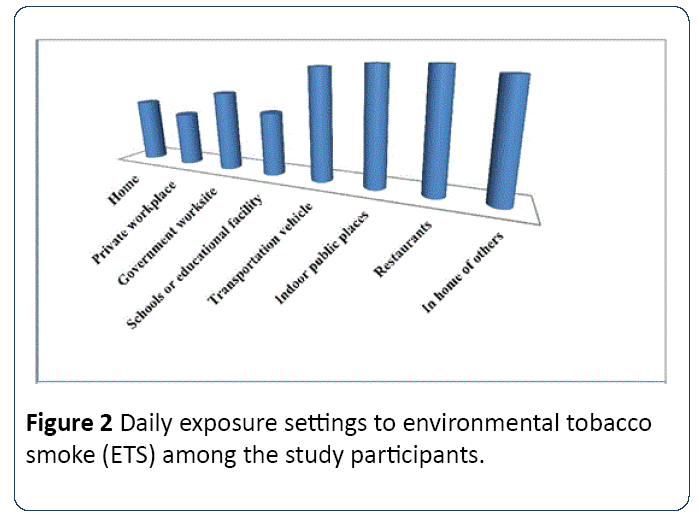
On the other hand, of the total study sample, nearly 26% self-reported exposure to ETS five to seven hours per day; the mean ± SD of exposure hours per day was 3.4 ± 2.6 (Figure 1). Regarding the settings of daily exposure to ETS, nearly 50% reported exposure on homes, 88.1% had self-reported (always/sometimes) daily exposure on restaurants, while private workplace has contributed to almost 42% of the selfreported daily exposure (Figure 2).
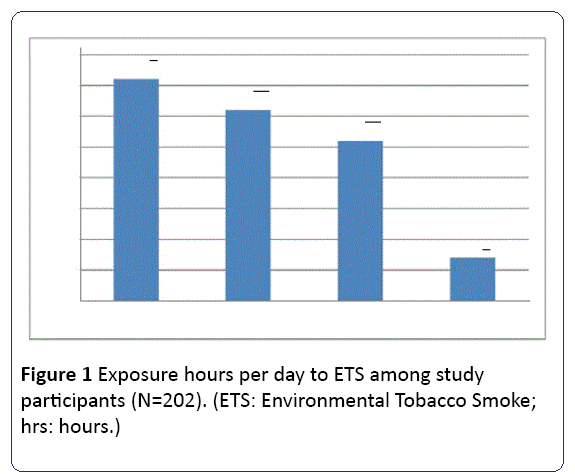
Figure 1: Exposure hours per day to ETS among study participants (N=202). (ETS: Environmental Tobacco Smoke; hrs: hours.)
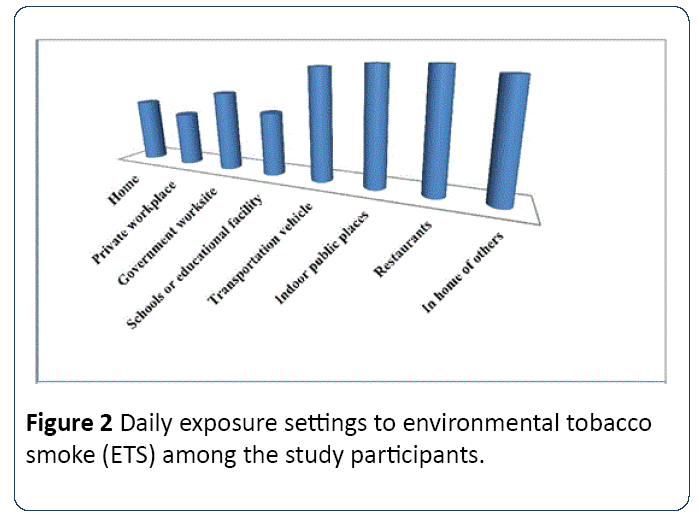
Figure 2: Daily exposure settings to environmental tobacco smoke (ETS) among the study participants.
Knowledge about ETS exposure
Table 2, shows the knowledge perspectives toward ETS. In overall, the participants’ females showed a good knowledge indication of the ETS on their health (health of non-smokers) with an average agreement response among all indicators of knowledge scale of about 77.2% (Table 2) which reflects a good knowledge about ETS. It should also be noted that the agreement category percentage for each indicator of knowledge perspectives was clearly higher compared to disagree and don’t know categories.
| Variable |
Agree n(%) |
Disagree n(%) |
I don't know n(%) |
| Knowledge perspectives |
| Tobacco smoke is dangerous for non-smoker's health. |
190 (94.1) |
4(2) |
8(4) |
| Children who are exposed to tobacco smoke have more illnesses, such as colds. |
180 (89.1) |
8(4) |
14 (6.9) |
| Exposure to tobacco smoke can cause lung cancer in non-smokers. |
162 (80.2) |
16 (7.9) |
24(11.9) |
| Public places should be smoke-free. |
156 (77.2) |
32(15.8) |
14 (6.9) |
| Parents or adults should not smoke near children. |
194 (96.0) |
4(2) |
4(2) |
| Smoke from other people's cigarettes will shorten my life. |
154 (76.2) |
24(11.9) |
24(11.9) |
| Smoke from other people's cigarettes is harmful for me. |
186 (92.1) |
12 (5.9) |
4(2) |
| Smoking should be banned in all public places |
172 (85.1) |
10 (5.0) |
20 (9.9) |
| SHS smoke makes my child's health worse. |
188 (93.1) |
4(2) |
10 (5.0) |
| I let visitors smoke in my home. |
92 (45.5) |
84(41.6) |
26(12.9) |
| Ask people around me to put out their cigarettes. |
126 (62.4) |
40(19.8) |
36(17.8) |
| ETS causes low birth weight. |
138 (68.3) |
12 (5.9) |
52(25.7) |
| ETS causes ear infections in children. |
104 (51.5) |
20 (9.9) |
78(38.6) |
| ETS causes heart attacks to children. |
152 (75.2) |
10 (5.0) |
40(19.8) |
| ETS is associated with crib death (SIDS). |
128 (63.4) |
16 (7.9) |
58(28.7) |
| ETS is associated with allergies in children. |
162 (80.2) |
12 (5.9) |
28(13.9) |
| ETS is associated with asthma in children. |
168 (83.2) |
8(4) |
26(12.9) |
| ETS: Environmental tobacco smoke. |
Table 2: Knowledge about environmental tobacco smoke (ETS) exposure (N=202).
Avoidance efforts and practice against ETS
Table 3, however, shows the avoidance efforts and practice against ETS. In overall, lower percentages of avoidance behaviors and practice against ETS had been seen (Table 3). For example, 41% of the participants answered positively on that they always remain with the group if someone started smoking, and nearly 50% reported that they routinely associate with people who smoke. On the other hand, 31% reported that they always allow people to smoke in their home. Further, 42% reported that they always remain with the friends or relatives while they are smoking.
| Variable |
Always true n (%) |
Always not true n (%) |
Don't know what to do n(%) |
| When I encounter someone who is smoking, I distance myself to ensure that I will not be exposed to smoke. |
160 (79.2) |
30 (14.9) |
12 (5.9) |
| When I am in public place such as restaurant or offices or clinic, I will leave if unable to sit in the nonsmoking section. |
106 (52.5) |
58 (28.7) |
38 (18.8) |
| When I trip by bus, or any other public transportation I would request a nonsmoking seat. |
138 (68.3) |
46 (22.8) |
18 (8.9) |
| If I am with people who are smoking and I cannot leave, I will ask them to refine from smoking. |
122 (60.4) |
44 (21.8) |
36 (17.8) |
| When an outdoor functions where smoking is present, I will move a way to avoid it. |
146 (72.3) |
32 (15.8) |
24 (11.9) |
| When an outdoor functions where water pipe smoking is present, I will move a way to avoid it. |
144 (71.3) |
38 (18.8) |
20 (9.9) |
| When exposed to secondhand smoke, I wash my clothes solely to remove the smell of smoke from them even if they are otherwise clean. |
132 (65.3) |
42 (20.8) |
28 (13.9) |
| I find it unpleasant to be around secondhand smoke. |
166 (82.2) |
20 (9.9) |
16 (7.9) |
| I allow people to smoke in my home. |
64 (31.7) |
94 (46.5) |
44 (21.8) |
| If I am with a group of people, and someone begins to smoke, I will remain with the group. |
84 (41.6) |
62 (30.7) |
56 (27.7) |
| If I encounter a friend or relative who is smoking, I will sit and talk with him/her while he/she is smoking. |
86 (42.6) |
76 (37.6) |
40 (19.8) |
| I allow people smoking in my car. |
46 (22.8) |
122 (60.4) |
34 (16.8) |
| If my husband, or friends or relatives are gathering in a designated smoking area to smoke, I will join them rather than be alone. |
66 (32.7) |
100 (49.5) |
36 (17.8) |
| I will sit in the smoking section of a public place or bus station if there are no seats available elsewhere. |
110 (54.5) |
48 (23.8) |
44 (21.8) |
| I routinely associate with people who smoke |
100 (49.5) |
76 (37.6) |
26 (12.9) |
Table 3: Practiceandavoidanceeffortsagainstenvironmentaltobaccosmoke(ETS) exposure(N=202).
Duration of exposure to ETS
In order to understand the impact of living with a smoking husband and/or family member, we have assessed the number of hours per day exposure to ETS and other variables among those who reported living with a smoking husband and/or family member. In Table 4 and due to lack of normality of duration of exposure variable, we used Kruskal-Wallis (KWT; for the three or more categories independent variables) and Mann-Whitney U tests (MWT; for the two categories independent variables) to compare the differences in the numbers of hours per day a participant exposed to ETS and some socio-economical variables such as age and scientific degree.
| Variable |
n |
Median (max – min) Hours/day |
Non-parametric KWT* or MWT* P-value |
| Age |
|
| 20-30 years |
38 |
2 (8-0.25) |
0.006 |
| 31-40 years |
32 |
3.5 (7-0.25) |
| 41-50 years |
30 |
4 (10-0.50) |
| more than 50 years |
6 |
1 (1-0.50) |
| How many years did you go to school? |
|
| 13 to 17 years (College/University) |
54 |
3 (10-0.50) |
0.384 |
| More than 17 years (Graduate School) |
52 |
3 (8-0.25) |
| Do you work outside of your home? |
|
| No |
4 |
3.25 (6-0.50) |
0.663 |
| Yes |
102 |
3 (10-0.25) |
| At work, where do you spend most of your time? |
|
| Primarily indoors |
78 |
3 (10-0.50) |
0.079 |
| Primarily outdoors |
2 |
8 (8-6) |
| Both indoors and outdoors |
26 |
3 (8-0.25) |
| Does your place of work have a policy that restricts smoking in any way? |
|
| No |
10 |
3 (8-2) |
0.016 |
| Yes |
92 |
2.50 (10-0.25) |
| Don’t know / Not sure |
4 |
6.50 (7-6) |
| Which of these best describes your place of work's smoking policy for indoor areas? |
|
| Not allowed in any indoor areas |
80 |
3 (10-0.25) |
0.029 |
| Allowed in some indoor areas |
14 |
2 (6-0.25) |
| Allowed in all indoor areas |
4 |
6.50 (8-5) |
| Don’t know/ Not sure |
8 |
3.50 (7-0.50) |
*KWT: Kruskal-Wallis Test; MWT: Mann-Whitney Test
Table 4: Association of number of hours/day exposure to environmental tobacco smoke (ETS) and some socio-economical variables (n=106).
No statistically significant differences were found between the median number of hours of exposure/day with the scientific degrees, the participants’ self -report work outside of home and the participants where spent most of their time at work variables (P-values>0.05; see Table 4).
However, those who were between 31 to 50 years old were found to be probably experience higher exposure hours/day compared to younger and older age’s groups ( P-value=0.006). in the meanwhile, those who reported that they don’t know or not sure if their workplace have a smoking restriction policy where found to have higher median hours/day exposure to ETS (6.5 hours) compared to those who reported negative response (3hours) or yes (2.5 hours) (P<0.016). Furthermore, those who reported that their workplace allow smoking in all indoor areas also found to be at a significantly higher median hours/day exposure to ETS (6.5 hours) compared to those who reported the answers (2-3.5 hours) (P=0.029; see Table 4).
Discussion
This study provides an overall view concerning the ETS exposure of specific target population (the educated women working in academic institutions). We have selected this population to evaluate the common beliefs that well-educated working women experience less ETS exposure compared to women with poor education or lower socioeconomic status [23]. To the date, no data of ETS exposure among the general population is available in our country. However, previous studies had shown that lower socioeconomic status could be directly associated with higher ETS exposure for females due to insufficient knowledge and higher rates of smoking among them [24-26]. In contrast, our results don’t support such conclusions as our participants were a group with a high level of socioeconomic status.
Table 4 Association of number of hours/day exposure to environmental tobacco smoke (ETS) and some socioeconomical variables (n=106).
Nearly 86.1% of our study participants reported that there is an anti-smoking policy at their workplace. Therefore, the educated working females have the acceptable background knowledge regarding their institutional ant-smoking policy. However, that seems to be insufficient to protect these females from the exposure to the ETS. At the meanwhile, our finding that nearly 33% of participants have been exposed to ETS ≥ five hours per day might not support such good knowledge.
One of the main findings of this study were that about 106 participants (52.5% of the total) reported living in homes with a smoker husband and/or member family and approximately 50% of the total participants reported that they routinely associated with people who smoke. These results could reflect the social and gender disparities in the Arab world where males are usually dominant and females don’t have too much impact on preventing males from smoking around them [27]. Concerning our Palestinian community, former studies showed that the Palestinian men typically have higher rates of smoking (52.7%) compared to females (16.5%) [28], which reflects higher levels of households’ ETS exposure among non-smoking households’ females.
This study also showed that our study participants (educated females) experience a major lack of the avoidance behaviour regarding ETS exposure in their private and public settings. It worthwhile to indicate that most of the study females (80%) thought that distancing themselves from smokers within the same area may be effective in reducing their exposure to ETS. However, this could not be appropriate as just only 100% of smoke free places could be considered sufficiently protective against the risks of ETS exposure [29].
The social and cultural aspects of Palestinian society are gender biased where male smokers in Palestine are culturally and physically resistant to smoking restrictions. This led us to an important finding that ETS exposure was common and high prevalent in home settings. The same might be frequently seen in other societies like the Korean Americans where exposure to ETS was found to be mostly common in work and home [30].
The Palestinian authorities have anti-smoking regulations and policies that prevent smoking in public and workplaces, but compliance with these regulations seems to be poor, perhaps due to the lack of the bylaws accompanied by the adapted anti-smoking policy from one side and that more than 50% of the Palestinian men are smoker from the other side [28]. Also, little is known in the general population regarding the actual risk of ETS exposure and the right practices of avoidance. Therefore, appropriate interventions programs to avoid exposure to ETS should be implemented in the Palestinian society as a whole where the impact would be very effective. This would further reverse the social inequalities and standards about smoking [31,32].
Like most epidemiological studies, this study has some limitations. Only one higher academic institution was selected. We have conducted a convenient sampling technique from females working in the selected academic institution. This could have limited our sample and the generalizability of our study results. However, An-Najah National University is the largest university in the West Bank. This study is a questionnaire based where under or over estimation could have been occurred. Despite these shortcomings, our study hit the head of one of the most challenging issue in developing countries with social and gender inequalities.
Conclusion
Despite the high level of knowledge regarding the risk of ETS exposure, the Palestinian females working in higher education institute in the Northern part of the West Bank have low level of practice and avoidance behavior to ETS exposure. Our findings highlight the necessary for implementation of smoking prevention measures and the encouragement of the promotions of smoke-free homes initiates. However, the targets should include not only females with low socioeconomic status but also the educated females with higher socioeconomic status. This would further help reverse the socioeconomic disparities and standards about environmental tobacco smoke.
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
HA designed and coordinated the study protocol and drafted the manuscript. AT, RG, AT, HK, TK collected the data and all authors conducted the statistical analysis. All authors read and approved the final manuscript
Acknowledgements
The authors would like to thank An-Najah National University administration for the permission to conduct this study among the female employees where major parts of this research would not have been conducted without their kind assistance and support. We are grateful to all the female participants in this study for the time they devoted and their understanding.
17832
References
- US Department of Health and Human Services (2006) The Health Consequences of Involuntary Exposure to Tobacco Smoke: a Report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention.
- World Health Organization (2008) WHO Report on the Global Tobacco Epidemic. The MPOWER Package, Geneva.
- Williams MA, Mittendorf R, Stubbleield PG, Lieber-man E, Schoenbaum SC, et al. (1992) Cigarettes, coffee, and preterm premature rupture of the membranes. Am J Epidemiol 135: 895-903.
- Office for National Statistics (2009) Opinions Survey Report No. 40. Smoking-related behaviour and attitudes. The information centre.
- World Health Organization: Regional office for the Eastern Mediterranean, Information resources, Countries, Occupied Palestinian Territories, WHO collaboration, countries cooperation strategy 2009-2013:
- Tobacco smoke and involuntary smoking: summary of data reported and evaluation(2004) Lyon, International Agency for Research on Cancer, IARC Monographs.
- Passive smoking and children. (2010) A report of the tobacco advisory group of the royal college of physicians. RCP London.
- Neal MS, Hughes EG, Holloway AC, Foster WG (2005)Sidestream smoking is equally as damaging as mainstream smoking on IVF outcomes. HumReprod 20: 2531-2535.
- Alwan N, Siddiqi K, Thomson H, Cameron I (2010) Children's exposure to second-hand smoke in the home: a household survey in the North of England. Health Soc Care Community 18: 257-263.
- Button T, Thapar A, McGuffin P (2005) Relationship between antisocial behaviour, attention deficit hyperactivity disorder and maternal prenatal smoking. Br J Psychiatry 187: 155-160.
- Palestinian Central Bureau of statistics (2013) Final report of the Palestinian family survey 2010. Ramallah, State of Palestine. 303: 43-46.
- Gu D, Wu X, Reynolds K, Duan X, Xin X, et al. (2004)InterASIA Collaborative Group: Cigarette smoking and exposure to environmental tobacco smoke in China: the international collaborative study of cardiovascular disease in Asia. Am J Public Health 94: 1972-1976.
- Hughes SC, Corcos IA, Hofstetter CR, Hovell MF, Seo DC, et al. (2008)Secondhand smoke exposure among non-smoking adults in Seoul, Korea. Asian Pac J Cancer Prev9: 247-252.
- Nebot M, López MJ, Tomás Z, Ariza C, Borrell C, et al. (2004) Exposure to environmental tobacco smoke at work and at home: A population based survey. Tobacco Control 13: 95.
- GharaibehH, Haddad L, AlzyoudS, El-ShahawyO, Abu Baker N, et al. (2011) Knowledge, attitudes, and behaviorin avoiding secondhandsmoke exposure among non-smoking employed women with higher education in Jordan. Int J Environ Res Publ Health 8: 4207-4219.
- Abdullah AS, Driezen P, Sansone G, Nargis N, Hussain GA, et al. (2014) Correlates of exposure to secondhand smoke (SHS) at home among non-smoking adults in Bangladesh: findings from the ITC Bangladesh survey. BMC Pulmonary Medicine 14: 117.
- Wipfli H, Avila-Tang E, Navas-Acien A, Kim S, Onicescu G, et al. (2008) Secondhand smoke exposure among women and children: Evidence from 31 countries. Am J Public Health 98: 672-679.
- GlascowRE, Foster LS, Lee ME, Hammond SK, Lichtenstein E, et al. (1998) Developing a brief measure of smoking in the home: Description and preliminary evaluation. Addict Behav 23: 567-571.
- Kurtz M, Kurtz J, Contreras D, Booth C (2003) Knowledge and attitudes of economically disadvantaged women regarding exposure to environmental tobacco smoke. Eur J Pub Health 13: 171-176.
- Wang WL, Herting JR, Tung YY (2008) Adolescents’ avoidance of second hand smoke exposure: Model testing. West J Nurs Res 30: 836-851.
- SPSS Inc (2007) SPSS 16 for windows- Statistical package for the social sciences. Chicago, USA.
- Best CM (2008) Parental smoking and increased risk of child malnutrition among families in rural Indonesia. Tob Control 17: 38-45.
- Nakkash R, Lee K (2009) The tobacco industry’s thwarting of marketing restrictions and health warnings in Lebanon. Tob Control 18: 310-316.
- Madanat H, Barnes MD, Cole EC (2008) Knowledge of the effects of indoor air quality on health among women in Jordan. Health EducBehav 35: 105-118.
- Baker AN, Haddad L, Savage C (2010) The influence of secondhand smoke exposure on birth outcomes in Jordan. Int J Environ Res Publ Health 77: 616-634.
- BonevskiB, Paul C, Jones A, BisqueraA, Regan T (2014) Smoky homes: gender, socioeconomic and housing disparities in second hand tobacco smoke (SHS) exposure in a large population-based Australian cohort. Prev Med 60: 95-101.
- Musmar SG (2012) Smoking habits and attitudes among university students in Palestine: A cross-sectional study. East Mediterr Health J 18: 454-460.
- Fact Sheet (2011) Second hand smoke and cancer; National cancer institute: Bethesda, USA.
- Hughes S, Corcos I, Hofstetter C, Hovell M, Irvin V (2008) Environmental tobacco smoke exposure among Korean American nonsmokers in California. Nicotine Tob Res 10: 663-670.
- Ding D, Wahlgren D, Liles S, Jones J, Hughes S, et al. (2010) Secondhand smoke avoidance by preteens living with smokers: To leave or stay?. Addict Behav 35: 689-694.
- Lin P, Huang K, Lu K, Chen T, Lin W, et al. (2010) Second-hand smoke exposure and the factors associated with avoidance behavior among the mothers of pre-school children: A school-based cross-sectional study. BMC Public Health 10: 606-609.