Research Article - (2022) Volume 16, Issue 5
Factors Influencing Hepatitis B Virus Co-Infection among HIV Patients Attending Health Care Services in Mungula Health Centre IV Adjumani District, West Nile Region Uganda. Hospital-based cross-sectional study
Judith Drazidio*,
Christine Atuhairwe and
John Bosco Alege
Clarke International University, Kampala, Uganda
Schools of Public Health & Applied Human Sciences, Kenyatta University, Nairobi, Kenya
St Francis Hospital Nsambya, Homecare Department, P.O.BOX 7146 Kampala, Uganda
*Correspondence:
Judith Drazidio, Clarke International University, Kampala,
Uganda,
Tel: +256784229187,
Email:
Received: 25-Apr-2022, Manuscript No. Iphsj-22-12755;
Editor assigned: 27-Apr-2022, Pre QC No. PreQC No. Iphsj-22-12554 (PQ);
Reviewed: 11-May-2022, QC No. QC No. Iphsj-22-12755;
Revised: 16-May-2022, Manuscript No. Iphsj-22-12755 (R);
Published:
23-May-2022, DOI: 10.36648/1791-809X.16.5.943
Abstract
Background: Hepatitis B virus is the primary leading cause of morbidity and mortality
among HIV patients and remains a remarkable public health burden. The global
prevalence of co-infection is 7.4%, 23% in Uganda, and 1.68% in the Adjumani district.
In 2016, The World Health Assembly endorsed the global health sector strategy on
viral hepatitis, which calls for the elimination of viral hepatitis as a public health threat
by 2030. As a measure, Uganda adopted WHO guidelines that recommend hepatitis
B testing in all HIV-infected patients, but only 46% of them have screened. Therefore,
this study assessed factors influencing HBV co-infection among HIV patients attending
ART clinics in Mungula health Center IV, Adjumani district.
Methods: The study employed a hospital-based cross-sectional study design where
226 respondents were interviewed using researcher administered technique.
Purposive and simple random sampling techniques were used to select the study
unit and respondents. In the analysis, the Chi-square test established the level of
association between each independent variable and HBV-co-infection while binary
logistic regression analysis determined factors accountable for co-infection in HIV
patients using an odds ratio at 95% confidence interval.
Results: 14.16% out of 226 respondents were found co-infected. The factors found
associated included HBV screening [OR=3.29, 95%CI: 1.071-10.137, p-0.02], Vaccination
against HBV [OR=12.018, 95%CI: 1.93-74.825, p-0.004)]. Expenses in accessing
vaccination services [OR=6.137, 95%CI: 2.025-18.601, p-0.018] were contributing
factors to the co-infection;
Conclusion: Extension of HBV screening and treatment services to all HIV clients
through community outreaches.
Keywords
HIV; HBV; HIV/HBV co-infection
What is already known on this topic: Approximately, 35 million
(32.2–38.8 million) individuals worldwide are HIV carriers,
of which 3 to 6 million had chronic hepatitis B (CHB) with an
estimated HBV co-infection incidence of 5–20%. Although coinfection
with HIV and HBV is recognized as being common, there
are limited data to provide an international perspective on this
HBV co-infection among HIV patients in Adjumani, therefore
this research study contributed to the identification of major
determinants of HBV co-infection and established the exact
frequency of the co-infection.
What this study adds; our study finding revealed that the
prevalence of HBV co-infection among HIV patients in the
Adjumani district is very high as compared to the national
prevalence.
How this study might affect research, practice or policy; when
appropriate interventions such as mandatory screening of HIV
patients for HBV and vaccinations are not done, there is will high
HBV related mortality, constraints health resources allocation
because the HIV patients are treated with two different chronic
diseases.
Introduction
Hepatitis B virus is among the primary causes of morbidity and
mortality among HIV patients. World health organization [2]
report revealed that about 2.6 million out of 36 million people
living with HIV are co-infected with chronic hepatitis B virus.
Hepatitis B virus co-infection has a significant association with
reduced survival, increase risk of progression to liver cancer,
and increased risk of hepatoxicity associated with antiretroviral
therapy. In addition [3] revealed that HBV endemic countries
accounted for 25% of co-infection from 350-400 million HIVinfected
individuals. This co-infection occurs during childbirth due
to a lack of resources for diagnosis and management of bloodborne
viruses in pregnancy and per partum period. However,
the prevalence of co-infection in Sub-Saharan Africa is attributed
to shared risk factors and co-transmission events like sexual
co-acquisition, unsafe injection, and traditional scarification
practices [4].
In Brazil, a study conducted by [5] revealed that a number of
sexual partners, practice of oral sex and anal sex influenced
HBV co-infection among HIV patients. Furthermore, a consistent
study conducted in central Nigeria revealed that heterosexuals
among HIV patients were the risk factor influencing co-infection
with 50% [6]. The result of risk factor analysis showed that
infection through male homosexual
contact had the highest
rate, 64 (74.4%), and 16 (18. 6%) were IDUs. Similarly, a study
conducted in Uganda indicated that having greater number of
sexual partners was over represented in male population that had
significant association with HBV co-infection [7]. Furthermore,
a cohort study conducted among pregnant women in Nigeria
showed a statistically significant association between multiple
sex partners and rate of co-infection. In the sixty sub-Saharan
African countries, the prevalence of HBV co-infection among
HIV patients was 14.9% [8]. Higher than 7.4% in South Africa
and Zambia and 7.0% among HIV patients in Botswana [9]. The
difference in variation was due to perinatal transmission, close
households contacts, medical, and cultural procedures, such as
scarification and tattoos.
In Ghana, a hospitalized cohort study conducted among HIV
positive patients at a tertiary care institution in Kumasi by [10].
Revealed that the prevalence of co-infection was 16.7%. This was due to health worker’s knowledge on management of HBV.
Furthermore, several studies were conducted to scrutinize the
epidemiology of HIV and HBV independently in sub-Saharan
African countries, where both diseases have hit so hard. The
study findings revealed that the prevalence of HBV co-infection
in HIV patients was 9.9% in Zambia [11] as compared to the
17.5% in Malawi [12]. The variations of the estimates obtained
from different areas of sub-Saharan Africa clearly demonstrated
lack of on-going surveillance activities and screening services to
determine presence of co-infection.
A study done in Nigeria revealed that pregnant women aged
36-40 years were more co-infected as compared to those 16-20
years [13]. On the contrary, a study done in Ghana revealed that
HIV patients aged 31-40 years reported very high co infection
rate 4.4% without cases observed in those 21 - 30 years age [14].
In the same study children below 18 years were more infected
30.7% compared to adults 7.8%.
In Uganda, the national prevalence of HBV co-infection was
3.9% attributed to low vaccination coverage against HBV and
lack of awareness of the HIV patients on modes of transmission
of HBV that put them at increased risk of the co-infection [15].
Meanwhile, a cohort study done in southwest region of Uganda
found the prevalence rate of 3.9% among HIV patient [16] In
addition, a similar study conducted in north western Uganda
revealed that out of 438 respondents, 7% of the HIV infected
patients were HBsAg positive. This was due to law screening and
vaccination services against HBV particularly among susceptible
HIV adults. On the other hand, a study conducted in north
western Uganda revealed that men had a significant relationship
with co-infection unlike their female counterparts 6.2% vs 2.95
(54/886) and (55/1934) [17].
In Adjumani district, the prevalence of HBV co-infection among
HIV patients was 1.68% irrespective of availability of its free
screening services and vaccination installed by the government in
all health centers, IIIs and IV (HMIS 080 2017). At present, there
is limited information on prevalence of HBV co-infection and
its associated factors among HIV patients in Uganda especially
Adjumani district due to limited research study conducted. To
the best of my knowledge, this is the first study conducted to
determine the prevalence and factors associated with hepatitis B virus co-infection among HIV infected persons in Adjumani
district. Therefore, the purpose of this study was to identify
possible areas of intervention and strategic policy directions to
the screening of all HIV patients for HBV. However, it was crucial
to determine the proportion of HIV patients co-infected with HBV
at Mungula health Centre IV for better allocation of resources
to enhance preventive and treatment measures. Additionally,
the findings obtained will provide important information for
stakeholders within and out Adjumani district involved in the
fight against HBV and HIV care and treatment.
Methodology
Study design and setting
This was health facility based analytical cross-sectional study
conducted at Mungula health Centre IV at ART clinic between July
and August 2017. In this study, both qualitative and quantitative
data were collected using structured and open-ended questions.
A quantitative questionnaire was design to capture information
on socio-demographics, economic factors, and life style and
knowledge factors influencing HBV co-infection among HIV
patients. Mungula health Center IV is government health facility
that serves both nationals and refugees in Mungula refugee’s
settlement.
Study population
The study population was HIV positive clients diagnosed in
the past three months attending ART clinic in Mungula health
Centre IV, Adjumani district. The sample size was determined
using Taro Yamane formula of 1973 at 95% level of confidence
and the proportion of attribute available in the study population
was taken at a 5% with 10% non-response rate of the study
participants. This formula was used based on known population
of N vs n where N is the number of HIV patients attending ART
clinic at Mungula health Centre IV.
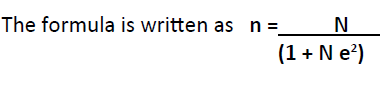
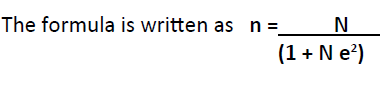
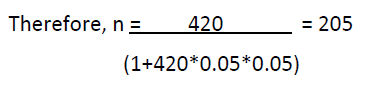
Where N is the total population of HIV patients attending ART
clinic, n= is the required was the required sample size. e2 is the
margin of error allowed at 95% level of confidence.1 is a constant
in the formula. But N= 420 HIV patients (hospital record 2017).
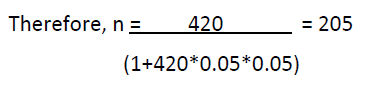
None response rate of 10%= 205*0.1 gives 21; Therefore, n=
205+21 gives 226 participants.
The respondents were recruited using the inclusion of criteria
of age 18 years above but below 70 years. This was done using
ART register to conform that the patient had been registered/
enrolled on ART at the clinic. However, simple random sampling
technique was used to select the study respondents and
purposive non probability sampling technique was used to select
five key informers.
Interviews
The interviews were conducted using structured questionnaire and key informant interview guide to obtain information ranging
from demographic characteristics (Age, sex, marital status,
religion, education level and occupation), Knowledge factors
(Knowledge of co-infection causes, knowledge of co-infection
services, knowledge of co-infection treatment, and knowledge of
co-infection prevention).
Socio-demographic variables
The socio-demographic variables included in the analysis were
age, sex, marital status, religion, level of education and HBV
screening status and its test result.
Knowledge variables
The knowledge factors examined in this analysis were Knowledge
of causes of HBV co-infection, knowledge of services for coinfection,
knowledge of treatment of co-infection and knowledge
of co-infection prevention.
Data handling and statistical analysis
The data was entered using EPIdata version 3.1 and analyzed using
statistical package for social sciences version 24.0. The proportion
of HBV co-infection among HIV patients was expressed using
percentages with corresponding frequencies. Pearson chi-square
was used to determine the level of association between each
independent variables and HBV co-infection at 95% confidence
level. However, fisher exact test was used to establish the level
of association for variables whose cell counts were less than 5 at
95% confidence level. Multiple logistic regressions was used to
determine independent predictors that significantly contributed
to HBV co-infection among HIV patients using probability value
(p-value) ≤0.05. At multivariate analysis, only variables that were
statistically significant at bivariate analysis were fitted in the
model.
Ethical Considerations
During our study time (year 2017 below), undergraduate
students were not submitting protocols for ethical review but
we were required to submit to the faculty of public health and
management to approve for data collection.
Results
Two hundred and twenty-six HIV infected patients were recruited
during the study period, of which 58% were female, 38.1% were
aged 20 to 30 years, 49.6% were married, and 43.6% Catholics
and 53.5% had non-formal education.
The study found that 53.1% of the respondents had screened
for HBV, and of those 14.16% were HBV co-infected with HIV.
However, results obtained from key informant interview revealed
very few cases of HBV co-infection among HIV patients. One
respondent was quoted” We have registered few cases of HBV
co-infection among HIV patients because we started screening
for HIV concurrently with HBV of recent that made us to obtain
very few numbers.
The majority of those who have been diagnosed with HIV one
year below (below 2017) missed HBV screening and found
it hard to go back for HBV screening due to the fear that they may be diagnosed with it which may cause discrimination and
stigmatization since very few people have understood about HBV
in their communities. Another challenge they faced is that when
someone tests HIV positive, they hardly belief the test result, thus
do not enrol in to ART and lost to follow up that makes screening
for HBV difficult. (KI, IN-CHARGE ART CLINIC) (Tables 1 and 2).
| Variables |
Responses |
Frequency(n=226) |
Percentage (%) |
| Age |
< 20 years |
21 |
9.3 |
| 20-30 years |
86 |
38.1 |
| 31-40 years |
65 |
28.8 |
| 41-50 years |
27 |
11.9 |
| 51 years and above |
27 |
11.9 |
| Sex |
Male |
95 |
42 |
| Female |
131 |
58 |
| Marital status |
Single |
66 |
29.2 |
| Married/cohabiting |
112 |
49.6 |
| Divorced |
28 |
12.4 |
| Widow/widower |
20 |
8.8 |
| Religion |
Catholic |
99 |
43.8 |
| Protestants |
51 |
22.6 |
| Muslim |
20 |
8.8 |
| Born again |
23 |
10.2 |
| Others |
33 |
14.6 |
| Education level |
Pre-primary |
14 |
6.2 |
| Primary |
62 |
27.4 |
| Secondary |
21 |
9.3 |
| Tertiary |
8 |
3.5 |
| Non-formal education |
121 |
53.5 |
| Screened for HBV |
Yes |
120 |
53.1 |
| No |
64 |
28.3 |
| Don't know |
42 |
18.6 |
| Test result for HBV |
Positive |
33 |
14.6 |
| Negative |
87 |
38.5 |
| Don't know |
106 |
46.9 |
| Total |
226 |
100 |
Table 1. Socio-demographic characteristics of study population (n=226).
| Variables |
Category |
HBV co-infected |
Total |
χ2 |
P-value |
| Yes |
No |
| Age |
< 20 years |
2(6.3%) |
19(9.8%) |
21(9.3%) |
0.999 |
0.908 |
| 20-30 |
12(37.5%) |
74(38.1%) |
86(38.1%) |
|
|
| 31-40 |
11(34.4%) |
54(27.8%) |
65(28.8%) |
|
|
| 41-50 |
4(12.5%) |
23(11.9%) |
27(11.9%) |
|
|
| 51 years and above |
3(9.4%) |
24(12.4%) |
27(11.9%) |
|
|
| Sex |
Male |
14(43.8%) |
81(41.8%) |
95(42.0%) |
0.045 |
0.849 |
| Female |
18(56.3%) |
113(58.2%) |
131(58.0%) |
|
|
| Marital status |
Single |
13(40.6%) |
53(27.3%) |
66(29.2%) |
9.546 |
0.018* |
| Married /cohabiting |
14(43.8%) |
98(50.5%) |
112(49.6%) |
|
|
| Divorced |
0(0.0%) |
28(14.4%) |
28(12.4%) |
|
|
| Widow /widower |
5(15.6%) |
15(7.7%) |
20(8.8%) |
|
|
| Religion |
Catholic |
17(53.1%) |
82(42.3%) |
99(43.8%) |
2.13 |
0.729 |
| Protestants |
5(15.6%) |
46(23.7%) |
51(22.6%) |
|
|
| Muslim |
2(6.3%) |
18(9.3%) |
20(8.8%) |
|
|
| Born again |
4(12.5%) |
19(9.8%) |
23(10.2%) |
|
|
| Never |
4(12.5%) |
29(14.9%) |
33(14.6%) |
|
|
| Education level |
Pre -primary |
5(15.6%) |
9(4.6%) |
14(6.2%) |
5.015 |
0.249 |
| Primary |
8(25.0%) |
54(27.8%) |
62(27.4%) |
|
|
| Secondary |
2(6.3%) |
19(9.8%) |
21(9.3%) |
|
|
| Tertiary |
1(3.1%) |
7(3.6%) |
8(3.5%) |
|
|
| Never |
16(50.0%) |
105(54.1%) |
121(53.5%) |
|
|
| Screened for HBV |
Yes |
17(53.1%) |
103(53.1%) |
120(53.1%) |
8 |
0.016* |
| No |
4(12.5%) |
60(30.9%) |
64(28.3%) |
|
|
| Don't know |
11(34.4%) |
31(16.0%) |
42(18.6%) |
|
|
| Total |
32(100.0%) |
194(100%) |
226(100%) |
|
|
Table 2. Socio-demographic characteristics associated with HBV coinfection
among HIV patients.
There was statistically significant relationship observed between
marital status and HBV co-infection among HIV patients in this
study (p=0.018). Similarly, results obtained from key informant
interview revealed that single respondent had higher chances
of HBV co-infection with HIV. Quotation during key informant
interview states “Majority of the respondents who are not
married and young are more likely to be co-infected due to lack
of resources to take care of themselves and children, they tend to
involve into transactional sex to earn a living which predisposes
them to HBV after HIV infection and single people do not have
control from anyone thus engage in to sexual activity at any time
according to their will.
He further emphasized that majority of single people are
adolescents who are sexually active compared to their
counterpart therefore they fill having sex is a priority and their
principle is to first have sex before getting involve in to courtship
and this occurs mostly at functions (KI, ART NURSE).
Therefore, more public health intervention should be directed
to the youths like forming association and creation of vocational
schools that can make them earn a living instead of engaging in
to cross generational and transactional sex.
In addition, the study finding revealed that having screened for
HBV was found associated with its co-infection (p=0.016). this
corresponds with qualitative result which revealed that most of
the HIV patients after testing and being diagnosed negative with
HBV influences them to engage in to more sexual act compared
to those diagnosed with the disease and those who have not yet
screened thus ignore the uptake of vaccination as a result HBV
comes as an opportunistic infection, (KI, ART COUNSELOR).
This implies that vaccination should be initiated immediately
after HBV screening for those who are negative and those who
tested positive should be initiated on treatment as soon as
possible. Furthermore, HBV vaccination should be given during
community outreach program on criteria that the community
members present with their previous vaccination card or books
to curb the prevalence rate.
As much as level of education was found not associated with HBV co-infection using quantitative data, results obtained from
key informant interview revealed statistical relationship as
evidence below. Level of education significantly influenced HBV
co-infection among HIV patients because most highly educated
people secondary and above feel they know more than any other
person in the community as a result they ignore community
outreach programs conducted on HBV prevention by health
workers (KI, NURSING OFFICER).
This implies that there is need for conducting outreach programs
in secondary schools and tertiary institutions to inform them
about HBV infection.
Factors associated with HBV co-infection among
HIV patients
In a multivariate analysis, having been screened for HBV was found
associated with co-infection. Vaccinating against HBV, number of
doses, reasons for not vaccinating and ways of preventing HBV
infection was found associated with HBV co-infection. However,
respondents who had screened against HBV were three more
protected from co-infection as compared to those who did not
screen (OR=2.294;95%CI:1.071-10.137, p=0.02). Similarly, high
chances of protection from HBV co-infection were seen among
respondents who had vaccinated against HBV as compared to
those who did not (OR=12.018;95%CI:1.93-74.825, p=0.004).
However, respondents who had received three shots (doses)
had reduced odds of HBV co-infection unlike those who had one
shot (OR=0.196; 95%CI: 0.049-0.784, p=0.003). Furthermore, the
study found that respondents who reported expense involved
as a reason for not vaccinating against HBV were six times more
likely to be co-infected (OR=6.137;95%CI:2.025-18.601,p=0.018)
(Table 3).
| Variables |
P-Value |
OR |
95% C.I. for OR |
|
Lower |
Upper |
| Marital status |
- |
- |
- |
- |
| Single |
0.49 |
1.725 |
0.379 |
7.85 |
| Widows/widowers |
- |
1 |
Reference |
- |
| Level of education |
- |
- |
- |
- |
| pre-primary |
0.391 |
1 |
Reference |
- |
| Secondary |
0.535 |
1.478 |
0.044 |
49.867 |
| Tertiary |
0.535 |
0.257 |
0.022 |
2.99 |
| Knowledge factors |
- |
- |
- |
- |
| Done HBV screening |
- |
- |
- |
- |
| Yes |
0.02 |
3.294 |
1.071 |
10.137 |
| No |
- |
1 |
Reference |
- |
| Causes of HBV co-infection |
- |
- |
- |
- |
| Having unsafe sex |
|
- |
- |
- |
| Yes |
0.563 |
1.385 |
0.394 |
4.868 |
| No |
- |
1 |
Reference |
- |
| Have you vaccinated against HBV |
- |
- |
- |
- |
| Yes |
0.004 |
12.018 |
1.93 |
74.825 |
| No |
- |
1 |
Reference |
- |
| How many does have you received |
- |
- |
- |
- |
| One |
- |
1 |
Reference |
- |
| Two |
0.005 |
1.705 |
0.153 |
18.965 |
| Three |
0.003 |
0.196 |
0.049 |
0.784 |
| Reasons for not vaccinating |
|
- |
- |
- |
| Expense involve |
0.018 |
6.137 |
2.025 |
18.601 |
| Ways of preventing HBV infection |
- |
- |
- |
- |
| Vaccination |
0.24 |
0.541 |
0.186 |
1.576 |
Table 3. Socio-demographic and knowledge variables associated with
HBV co-infection among HIV patients.
Discussion
The study finding revealed high (14.16%) prevalence of HBV coinfection
among HIV infected patients attending ART clinic at
Mungula health IV Adjumani district. This prevalence is higher
than 3.9% obtained in a cohort study done in south western
Uganda by [16]. Similarly, [6] revealed lower prevalence in
Garuku central Nigeria (13% vs 14.6%. On the contrary, the
prevalence HBV co-infection in HIV was found higher 16.7% in
Ghana [10]. Our study finding is attributed to late initiation of
HBV screening among HIV patients, inadequate uptake of HBV
vaccinations which increased prevalence of HBV co-infection.
More so, being single and having limited knowledge about HBV
infection increased chances of co-infection.
The study also established what causes the spread of HBV coinfection,
and the results indicated that having unsafe sex,
sharing tooth brush, unsafe delivery and sharing of food and
drinks were found associated with HBV co-infection with HIV.
Our study finding was consistent with results obtained from
Malaysia among international students which showed that being
aware about HBV infection, routes of transmission had strong
correlation with its co-infection among HIV patients, r 0.73,
p-value<0.001 (50.3%) [17].
Furthermore, our study established that respondents that had
screened for HBV had three times increased chances of being protected from co-infection unlike those who were not screened.
This finding was in correspondence with result obtained in
Malaysia which revealed that screening for HBV had significant
influence to its co-infection among HIV patients [18]. Similarly,
findings in central Nigeria indicated that inadequate screening
services influenced HBV co-infection by 13% and reduce
prognosis significantly [19].
Our study result showed that uptake HBV vaccination was
found associated with HBV-co-infection. Thus, those who got
vaccinated were 12 times most likely to be protected co-infection
unlike their counterparts. This is because the vaccine inhibits the
development of the virus in to an infectious organism in the body.
Our study finding revealed that being knowledgeable methods
of HBV prevention were found associated with co-infection
among HIV patients. For example, using sterilized medical
instrument was found determinant factor of preventing HBV coinfection
and having had community health talks on hepatitis B
virus raises people’s awareness on prevention of Co-infection.
This is consistent with findings in Kenya which indicated that
public health intervention strategies like health education on
having safe sex, dangers of having multiple sexual partners and avoidance of close contact with body fluid determines HBV coinfection
because health education conducted raises awareness
about risk factors that increases co-infection [20]. Therefore,
conducting public health education about dangers of HBV coinfection
can significantly influence on its co-infection among HIV
patients in Mungula health Centre IV.
Conclusion
The prevalence of HBV co-infection among HIV patients was very
high, emphasing the importance of screening all HIV patients for
HBV in the whole district to establish the exact prevalence of coinfection
for proper medical and public intervention strategies.
Additionally, this study found that knowledge variables such
as HBV screening, vaccination against HBV, number of doses
received and expense involved significantly determined HBV coinfection
among HIV patients.
REFERENCES
- Bautista-Amorocho H, Castellanos-Domínguez YZ, Rodríguez-Villamizar LA, Velandia-Cruz SA, Becerra-Pena JA et al. (2014) risk factors and genotypes of HBV in HIV-infected patients in the northeast region of Colombia: high prevalence of occult hepatitis B and F3 sub genotype dominance. PLoS One 9:e114272.
Indexed at, Google Scholar, Crossref
- World Health Organization (2016) Draft global health sector strategy on HIV, 2016–2021 (Draft 01.12.2015).
Indexed at, Google Scholar
- KOURTIS N ENG J (2012) HIV-Co-infection in Sub-Saharan Africa. Division Of Hepatology, Department of medicine Groote Schur hospital and university of cape town. 3366:1749.
Google Scholar
- Thumbiran NV, Moodley D, Parboosing R, Moodley (2014) Hepatitis B and HIV co-infection in pregnant women: indication for routine antenatal hepatitis B virus screening in a high HIV prevalence setting. 104:307-309.
Indexed at, Google Scholar, Crossref
- Oliveira MP, Lemes PS, Matos MAD, Del-Rios NHA, Santos Carneiro MA et al. Overt and occult hepatitis B virus infection among treatment-naïve HIV-infected patients in Brazil. J Med Virol 88:1222-1229.
Indexed at, Google Scholar, Crossref
- Gyar S, Agbo P, Reuben C (2014) Assessment of Hepatitis B Co-infection among HIV/AIDS Patients Attending Antiretroviral Therapy (ART) Clinic in Garaku, Central Nigeria. Res J Microbiol 9:232.
Indexed at, Google Scholar, Crossref
- Calisti G, Muhindo R, Boum Yn, Wilson LA, Foster GM et al. (2015) Epidemiology of HBV infection in a cohort of Ugandan HIV-infected patients and rate and pattern of lamivudine-resistant HBV infection in patients receiving antiretroviral therapy. Trans. R Soc Trop Med Hyg 109:723-729.
Indexed at, Google Scholar, Crossref
- Barth REa, Quirine Huijgen, Jantjie Taljaard b, Andy I.M (2010) Hepatitis B/C and HIV in sub-Saharan Africa: an association between highly prevalent infectious diseases. A systematic review and meta-analysis. Int J Infect Dis 14:e1024-e1031.
Indexed at, Google Scholar, Crossref
- Matthews PC, Beloukas A, Malik A, Carlson JM, Jooste P et al. (2015) Prevalence and characteristics of hepatitis B virus (HBV) confection among HIV-positive women in South Africa and Botswana. PLoS One 10.
Indexed at, Crossref
- Geretti A, Patel M, Sarfo Fs, Chadwick D, Verheyen J et al. (2010) Detection of highly prevalent hepatitis B virus confection among HIV-seropositive persons: Ghana. J Clin Microbiol 48:3223-3230.
Indexed at, Google Scholar, Crossref
- KAPEMBWA GJ, LAKHI S, BANDA Y, BOWA K, VERMUND SH (2011) HIV Hepatitis B and Hepatitis C: Zambia. J Glob infect Dis 3:269-274.
Indexed at, Google Scholar, Crossref
- Nyirenda BM, Stephany P, Hart Ca, Hart Ij, Munthali C et al. (2008) Prevalence of infection with hepatitis B and C virus and coinfection with HIV in medical inpatients: Malawi. J Infection 57:72-73.
Indexed at, Google Scholar, Crossref
- Lar P, Pam K, Christopher, gwamzhi L, Mawak D (2013) African journal of clinical and experimental microbiology department of Microbiology, Faculty of Natural Sciences, University of Jos: Nigeria. PMB 2084, Jos Department of Medicine, Jos University Teaching Hospital, JUTH.
Google Scholar
- Kye-Duodu G, Nortey P, Malm K, Nyarko KM, Sackey SO et al. (2016) Prevalence of hepatitis B virus co-infection among HIV-seropositive persons attending antiretroviral clinics in the Eastern Region of Ghana. Pan Afr med 25.
Indexed at, Google Scholar, Crossref
- Bwogi J, Braka F, Makumbi I, Mishra V, Bakamutumaho B (2009) Hepatitis B infection is highly endemic in Uganda: findings from a national serosurvey. Afr Health Sci 9:98-108.
Indexed at, Google Scholar
- Stabinski L, Reynolds SJ, Ocama P, Laeyendecker O, Serwadda D et al. (2011) Hepatitis B virus and sexual behavior in Rakai, Uganda. J Med Virol 83:796-800.
Indexed at, Google Scholar, Crossref
- Bwogi J, Braka F, Makumbi I, Mishra V, Bakamutumaho B et al. (2009) Hepatitis B infection is highly endemic in Uganda: findings from a national serosurvey. Afr Health Sci 9.
Indexed at, Google Scholar
- Daw MA, El-Bouzedi AA, Ahmed MO, Dau AA, Agnan MM (2016) Geographic integration of hepatitis C virus. global threat 5:170.
Indexed at, Google Scholar, Crossref
- Gyar SD, Dauda E, Reuben CJIJCMAS (2014) Prevalence of tuberculosis in HIV/AIDS patients in Lafia, Central Nigeria. 3:831-835.
Indexed at, Google Scholar
- Budambula N, Kerosi DO, Odari E, Lihana R, Osman S et al. (2015) Human Immunodeficiency Virus-1 and Hepatitis B Virus Co-Infections among Injecting Drug Users in Malindi, Kenya.
Indexed at, Google Scholar
Citation: Drazidio J, Kirabira SP, Atuhairwe
C, Alege JB (2022) Factors Influencing
Hepatitis B Virus Co-Infection among HIV
Patients Attending Health Care Services in
Mungula Health Centre IV Adjumani District,
West Nile Region Uganda. Hospital-based
cross-sectional study. Health Sci J. Vol. 16 No.
5: 943.