Keywords
complementary and alternative medicine, people living with HIV/AIDS, HIV/AIDS
Introduction
It is common to see people living with Human Immunodeficiency Virus trying to relieve stress or pain by using complementary and alternative medicine (CAM). The fact that HIV cannot be cured [1] causes many of them try both conventional medicine and complementary and alternative therapies to improve their quality of life and longevity [2].
The prevalence of CAM use among people living with HIV/AIDS (PLWH) around the world is consequently high, although it varies widely, ranging from 50% to 95%. This rate is around three times higher than the rate of utilization of CAM among uninfected people [3-8]. In 2008, 51.3% of HIV-infected Africans used traditional CAM to treat the signs and symptoms of their infection [4]. In 2009, 79% of HIV-infected women in United States used CAM [9], which is similar to the 78.2% of HIV patients in Malaysia who utilized CAM [3]. Moreover, in Thailand 10 years ago, the rates of CAM use among HIV-infected patients in Chulalongkorn Memorial Hospital and Ramathibodi Hospital were 95% and 86.1% respectively [5,10].
Because the use of CAM among HIV patients has expanded constantly around the world, studies of the factors related to CAM use have been conducted in many areas. The demographic factors for the use of CAM in HIV/AIDS have been characterized as high educational level, high income and young age; [3,6,11] the biomedical characteristics for the use of CAM are correlated to higher frequency of symptoms, longer duration of the disease and higher degree of disability; [4,6,11] moreover, the main psychosocial characteristics have been identified as more severe symptoms of depressive [6,11] and family experience of CAM use [3]. In addition, HIV-infected people’s beliefs and perceptions have a significant influence on CAM use [4]. There is no single factor for predicting the health-seeking behavior of people who have HIV. In addition, many internal and external factors stimulate the desire for CAM use. The mass media, product information, friends, health service providers and family recommendations are potentially powerful factors influencing CAM use in HIV-infected people. All affect impressions about CAM and trust in CAM among people living with HIV/AIDS and lead to increased use of CAM [10].
Significant interest in CAM use among HIV infected people should be aware because the increase in brand loyalty of CAM products may affect patient’s perception. The disadvantage is that they consume CAM without taking precautions in using the products or services [3,12]. Until now, one problem has been the lack of sufficient evidence to support the usefulness and benefits of CAM among HIV-infected people [11]. Moreover, there is some information about the potential health risks for CAM use among HIV/AIDs patients who use antiviral medicines, such as drug interaction [13]. That CAM users are less likely to adhere to antiviral regimens has also been confirmed [14].
Little is known about CAM use among PLWH in Thailand. One study into the use of complementary and alternative medicine among Thais (2010) found that CAM plays a critical role conjunction with therapeutic in the maintenance of health in terms of mind and body care, integrated health care, holistic health care, decisions regarding self-care choices and naturalistic care at every level of Thai society [15]. It is clear that the use of CAM in the Thai community is intensive, while the Thai governmental health care system has provided anti-retroviral medicine free-of-charge to every HIV/AIDS patient since 2007 [16]. This study was therefore designed to find the current extent of CAM use and the factors related to CAM use among PLWH in Bangkok, Thailand. The associations between independent variables (socio-demographic, biomedical, knowledge, perceptions and cues to action) and CAM use were examined.
Methodology
A cross-sectional descriptive study was conducted among PLWH who were members of four HIV associations which cooperate with the Thai Red Cross AIDS Research Centre: the Pozz Home Center, Ya Fak, Namjai Poen Sai Sam and Mittrapap Hang Faa. The required sample size was estimated using a confidence interval of 95%, an acceptance of error of 3% and the proportion of CAM use in 2003 of 0.95.5 Thus, the sample size needed was at least 203. However, the sample size was increased by 10% to protect against information loss. Therefore, 225 questionnaires were distributed to PLWH in those four associations. Participants were selected in proportion to the overall membership of these organizations. The data collection was conducted in March 2012, after obtaining formal approval from the ethics committee at Mahidol University.
The structured questionnaire consisted of eight parts, namely demographic characteristics, biomedical characteristics, knowledge of CAM, perceptions towards CAM, cues to action and the use of CAM. Demographic characteristics comprised six questions dealing with age, sex, education level, employment status, monthly income, and health insurance status. Biomedical characteristics were obtained from three questions about length of time since being infected with HIV, CD4 count and number of HIV-related symptoms.
Knowledge about CAM was evaluated by nine statements focused on general information about CAM, and the benefits and side effects of CAM. Each question scored on the basis of one point for a correct answer and no points for an incorrect answer. The total score for the knowledge part was classified into three categories: good (80-100), moderate (60-79) and poor (less than 60) based on Bloom’s criteria [17].
The perceptions towards CAM addressed PLWHs’ feelings or opinions on HIV-related treatment, the potential consequences of the treatments, the benefits of CAM and the barriers to CAM use. Perceptions were measured by 24 statements using a five-point Likert scale. The scoring for each statement was 5, 4, 3, 2, 1 corresponding to “strongly agree”, “agree”, “unsure”, “disagree” and “strongly disagree”. The score was reversed for negative statements. The total scores for each part of the perception section were classified into two levels: positive perceptions and negative perceptions using the mean for the group as the cut-off point.
The cues to action section consisted of 12 questions about sources of information, one question on the accessibility of CAM products and one question on the availability of CAM products. Accessibility to CAM products was classified into easy to access and difficult to access. Availability of CAM products was categorized as sometimes unavailable and always available.
CAM use was measured by asking about kinds of HIV therapy that the PLWH had used over the previous three months. CAM users included both those who used only CAM and those who used both ARV and CAM. Non-users of CAM were those who used only ARV.
The questionnaire was pre-tested for validity and reliability before data collection. The results of the pilot study at the Samutsongkram HIV/AIDS association showed that the KR20 for knowledge was 0.6368 and Cronbach’s alpha for perception was 0.7317.
Frequency, percentage, mean and standard deviation were used to describe both the prevalence of CAM use and the variables. The chi-square test was used to determine a possible association between each independent variable and CAM use, and multiple logistic regression was used to determine the association between each independent variable and CAM use.
Results
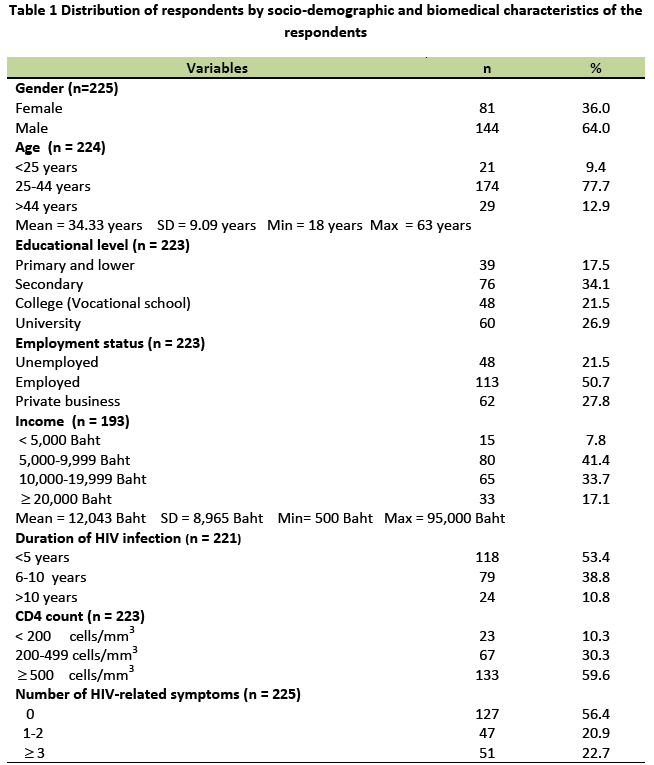
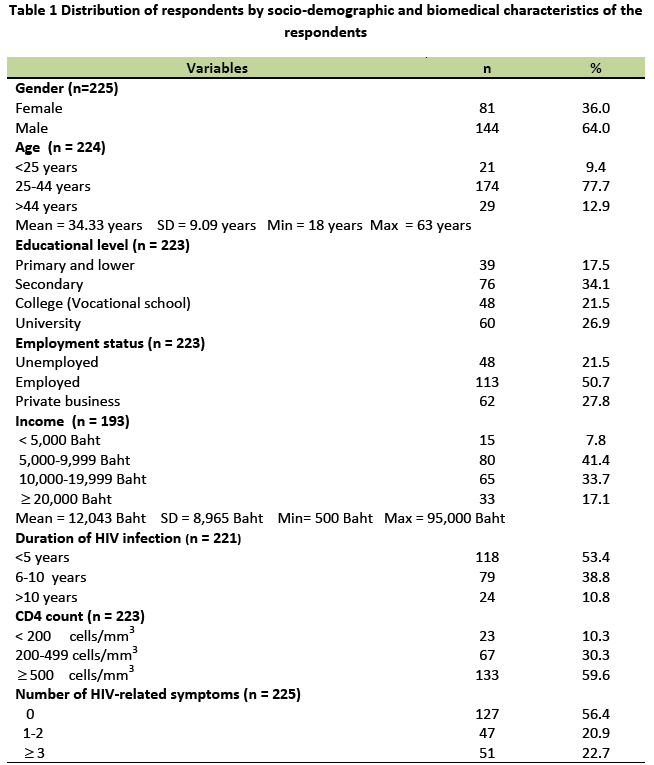
Table 1 shows that the majority of respondents were male (64.0%), aged between 25 and 44 years of age (77.7%), with the largest group educated at the secondary level (34.1%). Most CAM users were employed (50.7%), with the most frequent income range being 5,000-9,000 baht per month. Most CAM users had been infected with HIV for less than five years (53.4%), with a CD4 count more than or equal to 500 cells per mm3 (59.6%). More than half the respondents had no signs or symptoms.
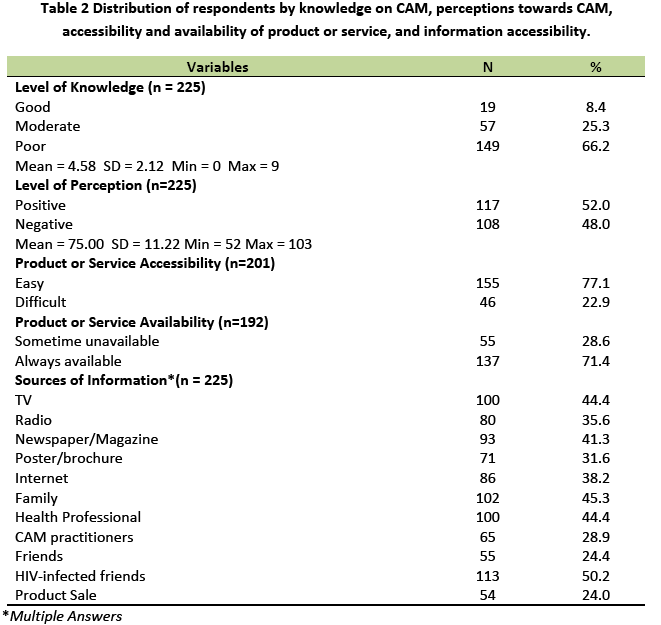
With regard to knowledge, perceptions and cues to action for the use of CAM, most respondents had poor knowledge (66.2%) and positive perceptions (52.0%) towards the use of CAM. Television, newspapers and magazines, and the Internet were the three most popular media for obtaining information about CAM. The people most responsible for giving information about CAM to respondents were HIV-infected friends (51.8%), family (46.8%) and health professionals (45.9%). A large majority (77.1%) of respondents also reported that it was easy to access CAM and about 70% of them had never encountered a lack of CAM products or services (Table 2).
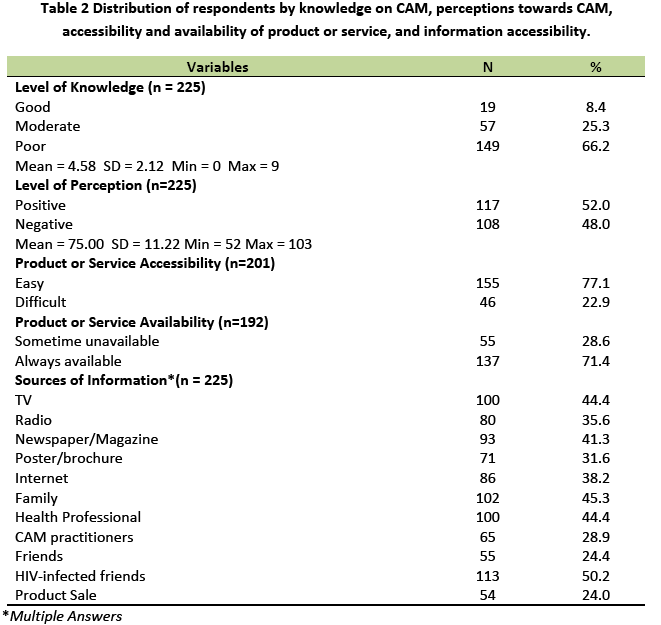
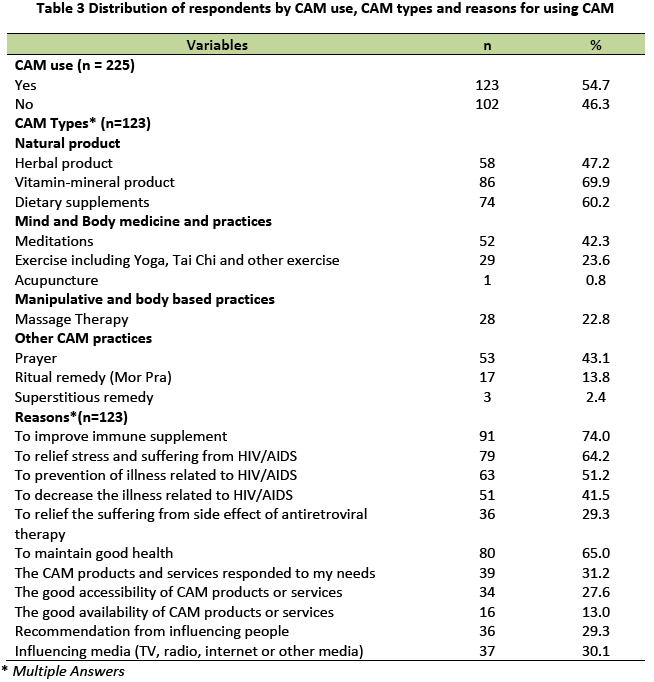
Table 3 shows that the prevalence of CAM use for the three months prior to the study was 54.7%. CAM users reported that vitamin-mineral products (69.9%), dietary supplements (60.2%), and herbal products (47.2%) were the three most frequently used CAM products. Reasons for using CAM were reported as improving immune response (74.0%), followed by maintaining health (65.0%) and relieving stress and suffering from HIV/AIDS (64.2%).
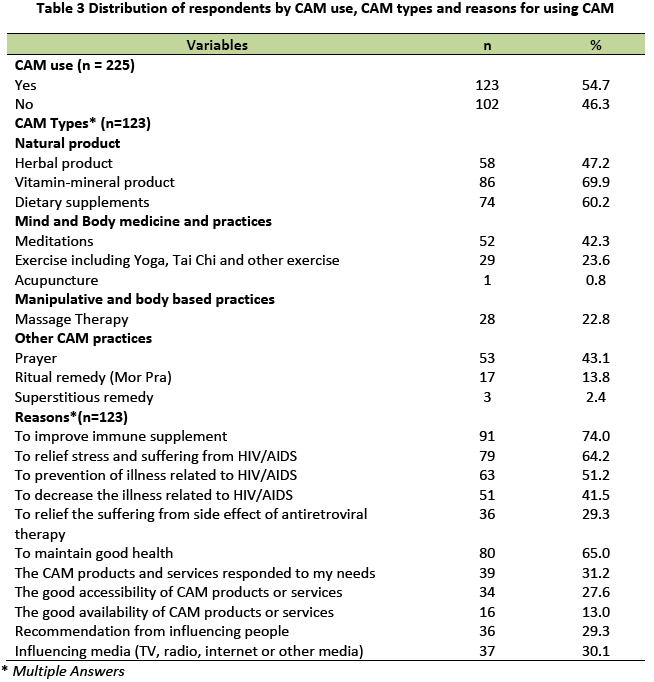
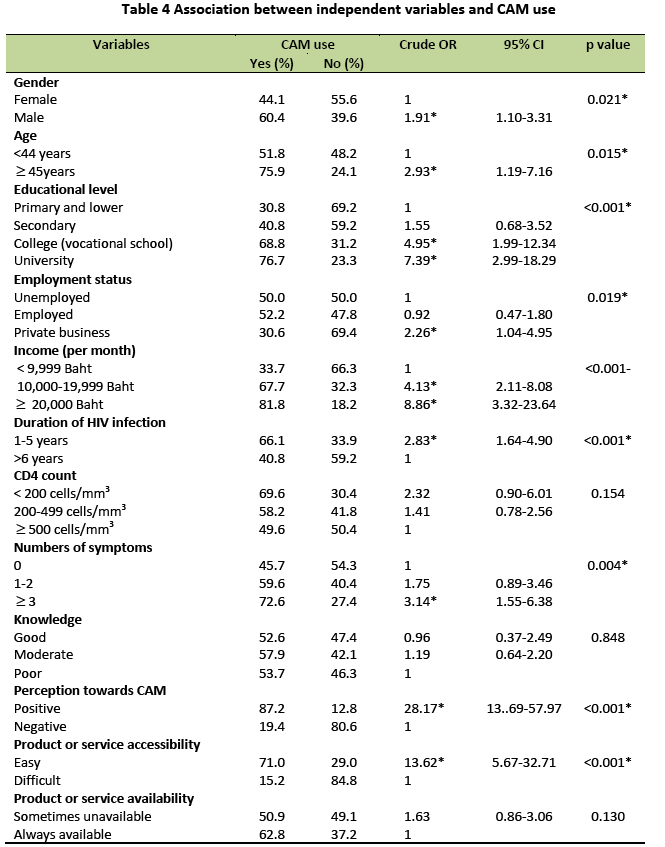
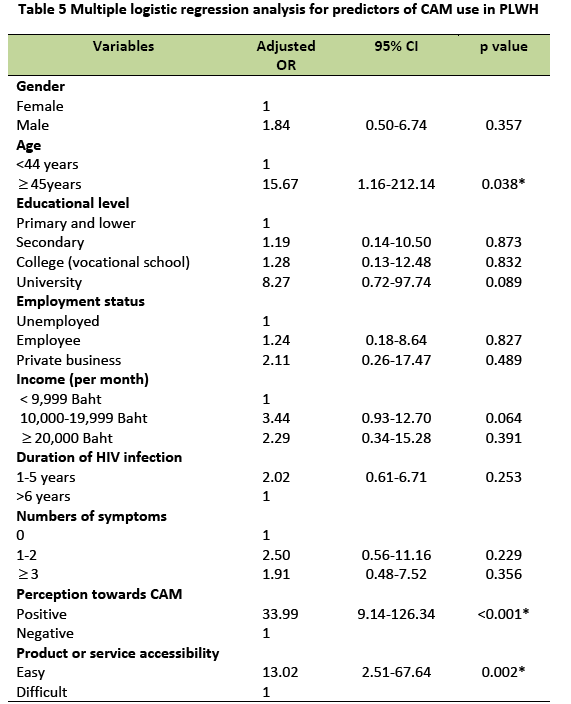
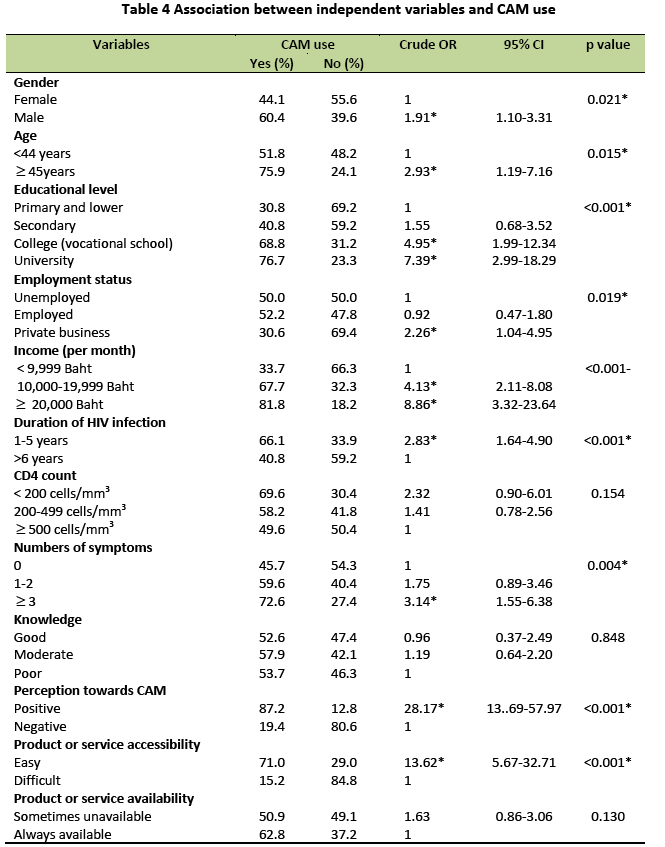
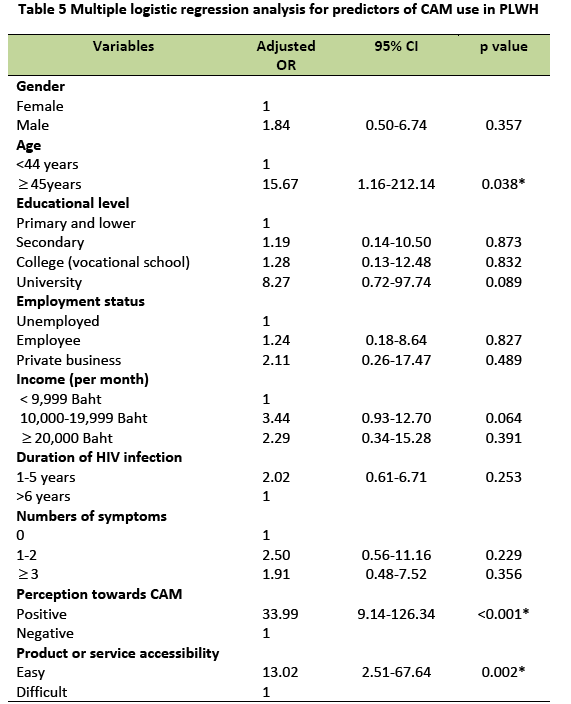
Table 4 shows that the use of CAM had a significant association with gender, age, educational level, employment status, income, duration of HIV infection, number of symptoms, perceptions, and product accessibility. Multiple logistic regression indicated that age, perceptions towards CAM, and product accessibility were significant predictors of the use of CAM among PLWH in Bangkok, Thailand, when adjusted for other factors (Table 5).
Discussion
This current study indicates that the prevalence of the use of CAM among PLWH was 54.7%. This prevalence was lower than that found by various Thai studies in the past [5,10]. This might be partly the result of a high degree of trust in conventional medical providers and deficiencies in the scientific database for the efficacy, safety and side effects of CAM. The national health care policy of free HIV/AIDS treatment and more varieties of ARV medicines might be another reason for the decrease in the use of CAM by PLWH [16]. However, the prevalence was still high and was consistent with a prevalence of 50-95% in previous studies worldwide [3-8,10]. The relevant findings were an increased desire on the part of PLWH for involvement in decisions regarding CAM, the positive perceptions towards CAM and influential external factors which lead to the high prevalence of the use of CAM among PLWH.
Perception was found to be the strongest predictor of CAM use when adjusted for other factors. PLWH who had positive perception were more likely to use CAM than those having negative perception. This was consistent with the findings in the previous study of Pelzer K et al., [4] which showed that perception was strongly associated to CAM use. In this study, most of PLWH had positive perceptions towards the use of CAM. However, most of PLWH had poor knowledge about CAM. They had a poor level of knowledge about the adverse effects including management of the risky situation. It is interesting that these PLWH respondents seemed unsure about how to manage their use of CAM in a proper way. They still lacked confidence in the management of health-related decisions. This is a consequence of Thais having inadequate knowledge, but positive perceptions towards the use of CAM. This may be because CAM plays a role in providing hope and optimism [2]., and two main reasons for the use of CAM among PLWH in Bangkok were to promote health and prevent illness by fulfilling the patient’s psychological demands. Another reason is to reduce the appearance of HIV-related symptoms. PLWH used CAM to increase their control over their illness and attempt to normalize their health status. This was similar to the results of many previous studies [9,12] which found that PLWH hope that CAM might reduce the side effects of ARV or strengthen the action of conventional medicine. Hence, the concept of multiple therapies is the best choice for treatment in the view of many PLWH.
Interestingly, there has been a change in the past belief that the use of CAM resulted from a belief in spiritual remedies [5] to the newer concept of trust in the scientific method of producing medicine. There is also a greater appreciation for ingestible natural health products. Ingestible natural health products might be easier for PLWH to buy and consume. This result was similar to results found in many previous studies. Natural health products (vitamins and minerals, dietary supplements and herbal products) were frequently used by those living with HIV [3,7,18].
Most sources of information reported PLWH using CAM because of information from HIV infected friends (50.22%), followed by family (45.33%) and some types of CAM use were inspired by health service providers (44.44%). In addition, some of them also sought CAM information from the mass media such as TV (44.44%), magazine (41.33%) and the Internet (38.22%) after being infected with HIV/AIDS. This finding of the various sources of information was consistent with the results of previous studies [10,19]. The group of HIV-infected friends was strongly influenced to the decision making of health care services and products. In Bangkok, many associations for HIV/AIDS have supported PLWH by providing many activities for their members. The PLWH have the chance to discuss their health status and health care products or services with one another. However, this may be problematic, as what is effective for one patient may not be for another, even one with the same symptoms. This is a significant issue for HIV/AIDS organizations to consider when attempting to provide correct information through appropriate HIV-infected psycho-social networks. Moreover, health professionals also influence CAM use. Finding the most beneficial therapy and obtaining higher patient’s satisfaction are based on good physician-patient communication [20].
This study had some limitations. The research design for this study was cross-sectional, using self-administered questionnaires, and relied on recall of PLWH covering the previous three months. Thus, recall bias in respondents’ memories may have occurred and in-depth information may not have been obtained. Demographically, the sample was composed of PLWH in HIV-associations and therefore may not represent the behaviors of all PLWH in Bangkok. Self-Selection bias may have occurred, as the respondents were PLWH who chose to participate in the study. Due to the ethical issues, the PLWH also had the right not to participate or not to answer in some question. Thus, a longitudinal study and a qualitative research should be conducted in order to get more accurate information about variations in CAM use as the disease progresses, and to get in-depth information. Moreover, the disclosure of CAM use among PLWH to health professionals, the health professionals’ views towards CAM use, the relationship between CAM use and ARV adherence of HIV/AIDS people are also deserving of future research.
Conclusion
In conclusion, the study reveals that PLWH had positive perception towards CAM, but they had inadequate knowledge. They had a poor level of knowledge about adverse effects of CAM, including management of risky situation. Therefore, PLWH should strive to learn more about CAM by conducting their own investigations to find how to use CAM appropriately. The advantages and disadvantages found in the information from both the media and peers should be taken into consideration. In addition, PLWH should disclose their use of CAM and discuss this use with health professionals by establishing two-way communication.
Acknowledgements
We would like to thank the coordinators of the Thai Red Cross Research Center, Mittrapap Hang Faa, Ya Fak, Namjai Poen Sai Sam, the Pozz Home Center and Samutsongkram HIV/AIDS association. We also thank Mr. William Martin of the Faculty of Liberal Arts, Mahidol University for his comments and suggestions about language and style.
2804
References
- World Health Organization. HIV/AIDS Fact sheet N 360 November 2011 [Online]; Available from: https://www.who.int/mediacentre/factsheets/fs360/en/index.html%2012%20January%202012 [Accessed 2011 Jan 20].
- Jennifer RJ. Patient education and wellness: a hand book for manual therapists. British: Elesvier Ltd.; 2010; 14-20.
- Hasan SS, See CK, Choong CL, Ahmed SI, Ahmadi K, Anwar M. Reasons, perceived efficacy, and factors associated with complementary and alternative medicine use among Malaysian patients with HIV/AIDS. The Journal of Alternative and Complementary Medicine 2010; 16(11). 1171-6. doi:10.1089/acm.2009.0657.
- Peltzer K, Preez N. F, Ramlagan S, Fomundam H. Use of traditional complementary and alternative medicine for HIV patients in KwaZulu-Natal, South Africa. BMC Public Health 2008; 8(255): 1-14. doi: 10.1186/1471-2458-8-255.
- Wiwanitkit V. The use of CAM by HIV-positive patients in Thailand. Complementary therapies in medicine 2003; 11. 39-41. doi:10.1016/50965-2299(02)00108-5.
- Bormann JE, Uphold CR, Maynard C. Predictors of complementary/alternative medicine sse and intensity of use among men with HIV infection from two geographic areas in the United States. Journal of the Assocociation of Nurses in Aids Care 2009; 20(6). 468-80. doi: 10.1016/j.jana.2009.03.008.
- Milan FB, Arnsten JH, Klein RS, Schoenbaum EE, Moskaleva G, Buono D, et al. Use of complementary and alternative medicine in inner-city persons with or at risk for HIV infection. AIDS Patient Care and STDS 2008; 22(10). 811-6. doi:10.1089/apc.2007.0159.
- Hoogbruin A. Complementary and alternative therapy (CAT) use and highly active antiretroviral therapy (HAART): Current evidence in the literature, 2000-2009. Journal of Clinical Nursing 2010; 20(7-8). 925-39. doi: 10.1111/j.1365-2702.2010.03322.x.
- Lui C, Yang Y, Gange ST, Weber K, Sharp GB, Wilson TE, et al. Disclosure of complementary and alternative medicine use to health care providers among HIV-infected women. AIDS Patient Care STDS 2009;23(11). 965-71. doi: 0.1089/apc.2009.0134.
- Pintobtang S. Complementary and alternative therapy using in hospitalized HIV/AIDS patients.[M.N.S. Thesis in Adult Nursing]. Bangkok: Faculty of Medicine Ramathibodi Hospital, Mahidol University; 2002.
- Littlewood RA, Vanable PA. Complementary and alternative medicine use among HIV-positive people: Research synthesis and implications for HIV care. AIDS Care 2008; 20(8). 1002-18. doi: 794151957 [pii]10.1080/09540120701767216.
- Chen W. T, Shiu C-S, Simoni J, Fredriksen-Goldsen K, Zhang F, Starks H, et al. Attitudes toward antiretroviral therapy and complementary and alternative medicine in Chinese HIV-infected patients. J Assoc Nurses AIDS Care 2009; 20(3). 203-17. doi: 10.1016/j.jana. 2008.12.004.
- Ladenheim D, Horn O, Werneke U, Phillpot M, Murungi A, Theobald N, et al. Potential health risks of complementary alternative medicines in HIV patients. British HIV Association HIV Med 2008 Apr 29; 9:653-9. doi: 10.1111/j.1468- 1293.2008.00610.x.
- Peltzer K, Preez N.F, Ramlagan S, Fomundam H, Anderson J. Traditional complementary and alternative medicine and antiretroviral treatment adherence among HIV patients in Kwazulu-Natal, South Africa. African Journal Traditional, complementary alternative medicine 2010;7(2):125-37.
- Sherrer P, Wongupparaj P. The situation of complementary alternative usage in health seeking behavior of Thais. Health Systems Research Institue and Alliances. 2009 [Online]; Available from: https://hdl.handle.net/123456789/2934 [Accessed 2011 Jan 20]
- The Thai Red Cross Society, The knowledge of HIV/AIDS. 3rd ed. Bangkok: Thai Red Cross Society; 2008. p.12.
- Bloom BS. Taxonomy of Educational Objectives: Classification of Educational Goals. Handbook 1: Cognitive Domain. New York: Longman, Green & Co.; 1956.
- Dhalla S, Chan KJ, Montaner JS, Hogg RS. Complementary and alternative medicine use in British Columbia: A survey of HIV positive people on antiretroviral therapy. Complementary Therapies in Clinical Practice 2006; 12(4). 242-8. doi: 10.1016/j.ctcp.2006.05.002.
- Leonard B, Huff H, Merryweather B, Lim A, Mills E. Knowledge of safety and herb-drug interactions amongst HIV+ individuals: a focus group study. The Canadian Journal of clinical pharmacology 2004; 11(2): 227-31.
- Michlig M, Ausfeld-Hafter B, Busato A. Patient satisfaction with primary care: A comparison between conventional care and traditional Chinese medicine. Complementary Therapies in Medicine 2007;16(6):350-8. doi:10.1016/ j.ctim.2007.12.001.